Introduction
Dens invaginatus (DI), also called dens in dente, is
a developmental malformation due to an invagination of the enamel
organ into the dental papilla during the morpho-differentiation
phase of tooth development (1,2). DI
can occur in both deciduous and permanent dentition but is more
common in permanent dentitions, with a prevalence of 0.04-10.00%
(3-5).
The maxillary lateral incisor is the most frequently involved tooth
for DI and there are also reports that DI occurred in canines and
posterior teeth (6-8).
DI may also uncommonly occur in supernumerary teeth (5). Several etiopathogenic theories have
been proposed to explain the development of this malformation:
Focal failure growth of the internal enamel epithelium engulfed by
surrounding continuous proliferating dental papilla cells is one of
the causes of DI (9). Oehlers
considered that during tooth development the enamel organ
distortion induces protrusion of the enamel organ into the dental
papilla, which may lead to invagination (10). In addition, external forces from
adjacent teeth, trauma, infection and genetic factors also are
considered as possible contributing factors (6,11).
According to the origin of invagination, the
anatomical disorder is classified into two categories: Coronal and
radicular DI (CDI and RDI, respectively) (10,12).
Oehlers proposed three types of CDI malformation (10): Type I, invagination is lined by
enamel and within the confines of the crown not extending beyond
the amelocemental junction; type II, invagination extends into the
root, beyond the cementoenamel junction and ends as a blind sac,
with or without communicating with the dental pulp and type III,
invagination extends to the root, forming an additional pseudo
apical or lateral foramen in the apical or periodontal area,
usually with no communication with the pulp. RDI occurs due to
invagination of Hertwig's sheath into the developing root. There
are two subtypes of RDI: Type I, invagination is cementum-lined and
related to an axial root groove; and type II, enamel-lined
invagination within the root (12).
Due to deep pits and structural defects, teeth with
DI are more susceptible to caries, pulpitis, pulp necrosis,
periapical lesion and even periodontal diseases (13-16).
The complex structure increases the difficulty of diagnosis and
treatment of DI. The radiographical imaging of DI often shows a
radiolucent invagination surrounded by a radiopaque area (enamel)
in the tooth crown or extending into the root (1). Although two-dimensional (2-D)
radiographs are routinely used to diagnose DI, treatment of
complicated cases requires three-dimensional (3-D) radiographical
imaging, such as cone-beam computed tomography (CBCT). CBCT is a
well-established 3-D imaging technique that has several
superiorities over 2-D radiographs, including superior diagnostic
ability in detection of DI and assessment of its type (8,17).
In addition, CBCT provides more accurate images of periapical
lesions than periapical or panoramic radiographs (18). Therefore, CBCT instead of 2D
radiographs can assist in the diagnosis and treatment of DI.
The principle underlying treatment for DI should be
maintaining the pulp vitality and preserving tooth structure using
minimally invasive methods (8).
Various treatment options, including prophylactic filling, root
canal treatment, the combination of endodontic and surgical
treatment, intentional replantation, extraction, and pulp
revascularization, are used according to the morphology of the
involved tooth and severity of infection (19-21).
The present study aimed to report a series of cases highlighting
variations in DI treatment.
Case report
Ethics approval
The present study was approved by the Ethics
Committee of Liaocheng People's Hospital (Shandong, China; approval
no. LC2020146). The treatment procedures, risks and benefits were
informed to the patient and each patient signed written informed
consent for publication of their data/images.
Case series
Of five cases with DI, one was CDI (type I), two
were CDI (type II) and two were RDI (type II). The inclusion
criteria were as follows: Root canal treatment RCT was performed in
treating CDI (type I) invagination removal combined with RCT for
CDI (type II) with pulpitis and periapical lesion; conventional RCT
with intentional replantation was used for the treatment of RDI;
periapical surgery or intentional replantation was used for the
cases with pulpitis and periapical lesion, which were not cured
after RCT; intentional replantation combining with RCT, seal the
invagination or root resection and back filling for RDI.
Case 1
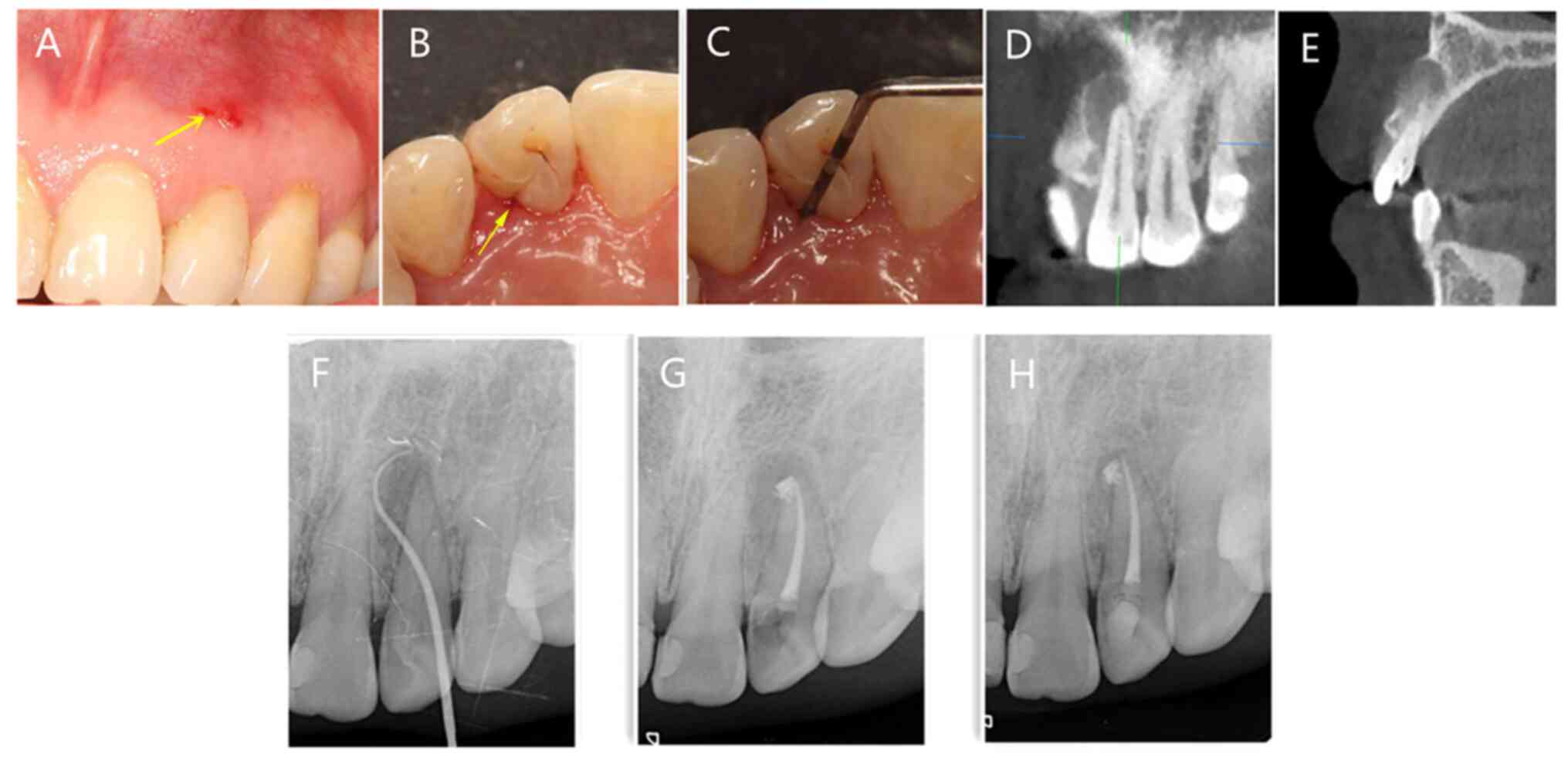
A 40-year-old female patient sought treatment in the
Department of Endodontics of Liaocheng People's Hospital
(Liaocheng, China) in March 2019 for slight sensitivity to
palpation and recurrent sinus on the upper left anterior region.
The patient reported swelling history in the upper lip from early
February 2019. Intraoral examination revealed a small crown on
tooth 22, a palatal groove and a DI with normal periodontal
attachment on the distal gingival margin; no caries or color
alteration was observed (Fig.
1A-C). Thermal and electrical pulp testing revealed no pulp
vitality. Periapical radiography revealed a well-circumscribed
radiolucent area at the apex of tooth 22 (Fig. 1F). CBCT (KaVo Dental) scans were
used to reveal the image of the tooth with the parameters as
follows: Patient position, upright; tube current, 8 mA; focus, 0.5
mm; grayscale, 14 bt; and scan time, 20 sec. CBCT scan demonstrated
that the invagination was limited within the amelocemental junction
and the root was not involved (Fig.
1D and E). The patient was
diagnosed with CDI (type I), necrotic pulp and chronic apical
periodontitis. As the invagination was limited within the
amelocemental junction and the root was not involved, conventional
RCT was performed (Fig. 1G). The
6-month follow-up showed the tooth was asymptomatic and the
radiolucent area was decreased in radiograph examination (Fig. 1H).
Case 2
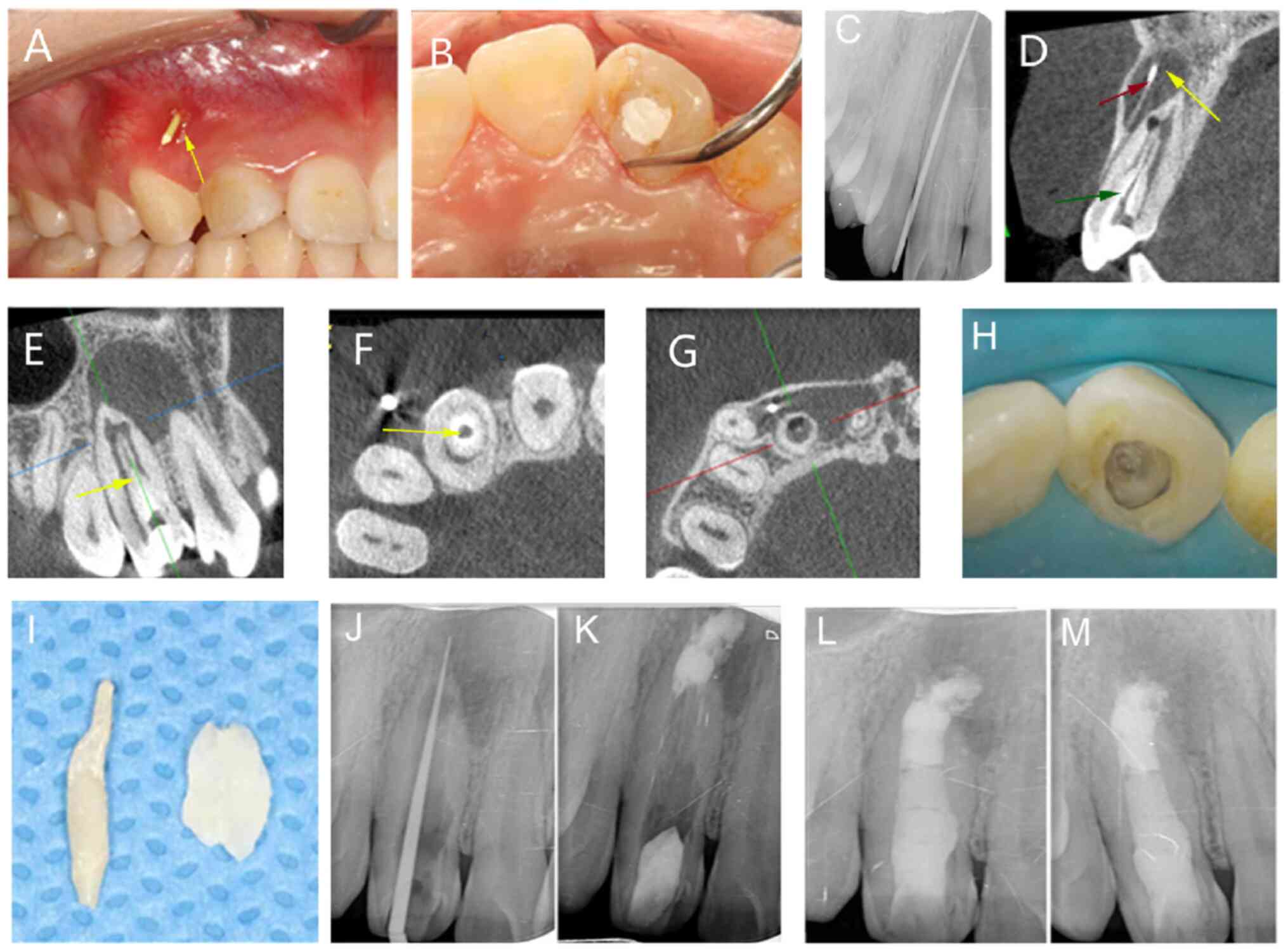
A 21-year-old female patient, visiting the
Department of Endodontics of Liaocheng People's Hospital in June
2021, complained of pus discharge from the upper right anterior
region for 6 months. Intraoral examination revealed a sinus with a
red and swollen fistula at the corresponding alveolar mucosa of the
periapical region of tooth 12, which had an unusually large crown
(Fig. 2A and B). Periapical radiography revealed an
abnormal root canal and a well-circumscribed radiolucent area at
the apex of tooth 12, suggesting a periapical lesion; probing with
a gutta percha point under X-ray demonstrated the fistula derived
from the periapical pathological lesion of the tooth 12 (Fig. 2C). CBCT scan indicated an identical
tooth-like structure extending beyond the cementoenamel junction
and reaching the pulpal space (Fig.
2D-G). The patient was diagnosed with CDI (type II) and chronic
apical periodontitis in tooth 12. As the invagination reached the
canal and the periapical tissue was affected, root canal treatment
was performed; the invaginated tissue was carefully removed using
an ultrasonic tip (model E3D; Guilin Woodpecker Medical Instrument
Co., Ltd.) under a dental operating microscope (Carl Zeiss GmbH)
(Fig. 2H-J); a 3-5 mm apical
barrier was created with iRoot BP Plus root repair material
(Innovative BioCeramix, Inc.); the pulp space was filled with a
gutta-percha (VDW Dental) using the continuous wave of condensation
technique (22) and then final
composite restoration was placed (Fig.
2K and L). After 6 months, the
sinus disappeared and bone healing was observed at the periapical
region of tooth 12 by periapical radiography (Fig. 2M).
Case 3
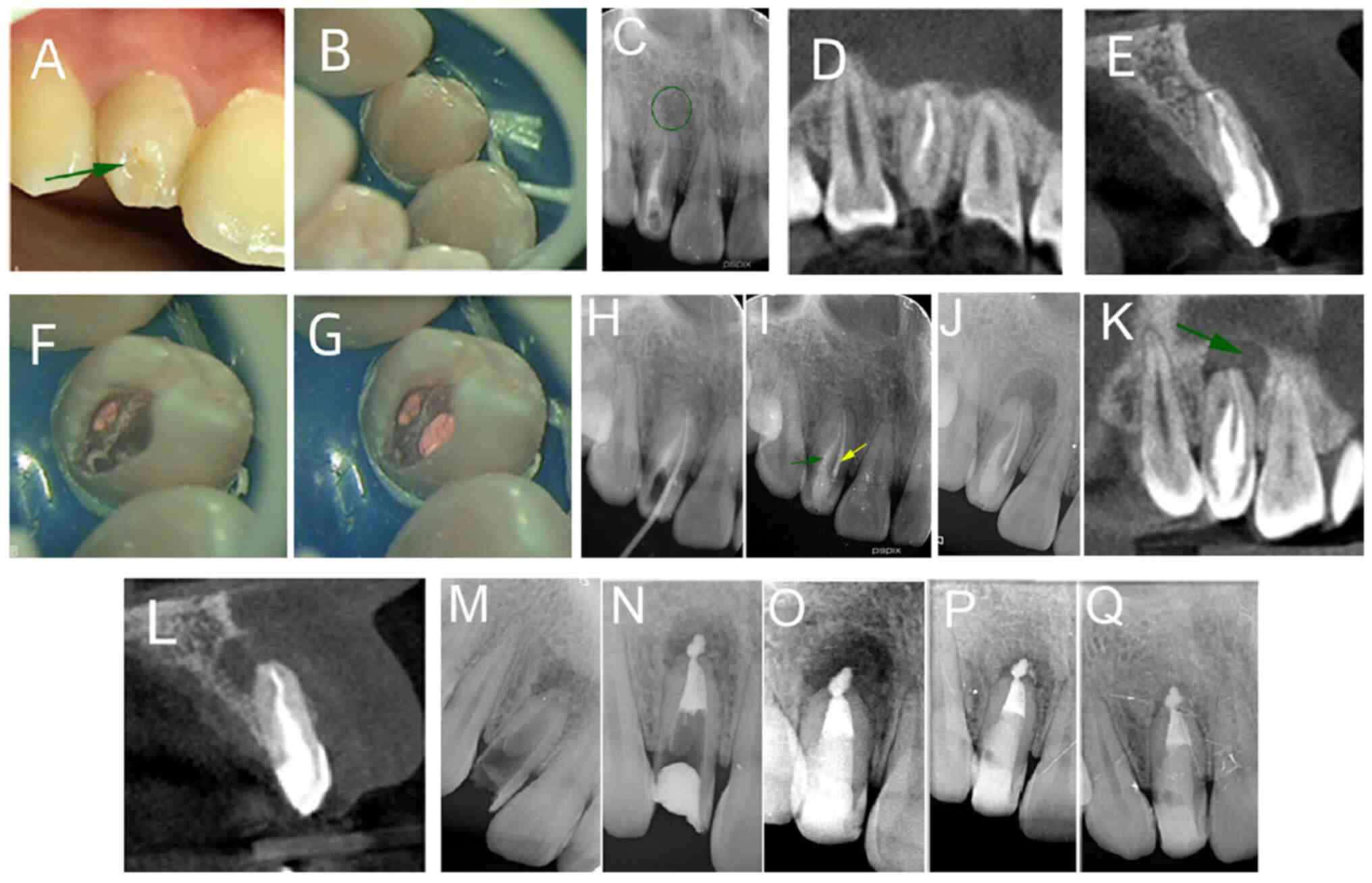
A 20-year-old female patient sought endodontic
treatment in the Department of Endodontics of Liaocheng People's
Hospital in December 2021 for the right upper lateral incisor. The
patient had undergone initial endodontic treatment on the incisor 5
years previously; after one year, the patient underwent root canal
retreatment to the main and invaginated canal of the tooth due to
residual pulpitis and DI (Fig.
3A-I). Here, the patient complained of recurrent mild pain,
tenderness to biting and touching mucosa near tooth 12 for 3 weeks.
Swelling in the infraorbital region was also reported ~1 month
previously. Intraoral examination revealed sinus tract in the
alveolar mucosa, proximal to the apical area of the tooth 12; there
was no discomfort following percussion, but mild sensitivity to
palpation. The radiograph showed that the main and the invaginated
canal were filled but there was an unclear view of the canal space
and variation in the distal side; in addition, there was a
well-circumscribed radiolucent area at the apex of the tooth
(Fig. 3J). CBCT indicated an
identical tooth-like structure in the root area close to the
cementoenamel junction (Fig. 3K
and L). The diagnosis was CDI
(type II) and chronic apical periodontitis. As the invagination
reached the canal and periapical tissue was affected due to the
unfilled main canal, an ultrasonic tip (E3D) was used to remove the
previous root filling material and invaginated tissue under the
dental operating microscope (Fig.
3M). iRoot BP was used to make an apical barrier, and the rest
of canal was restored with gutta-percha; two glass fiber-reinforced
posts (Nordic Glasix) were then placed into the root and the access
cavity was sealed with resin composite restoration (Fig. 3N and O). When followed up after 6 and 12
months, the patient was asymptomatic and radiograph examination
showed that the previous radiolucent area was decreased (Fig. 3P and Q).
Case 4
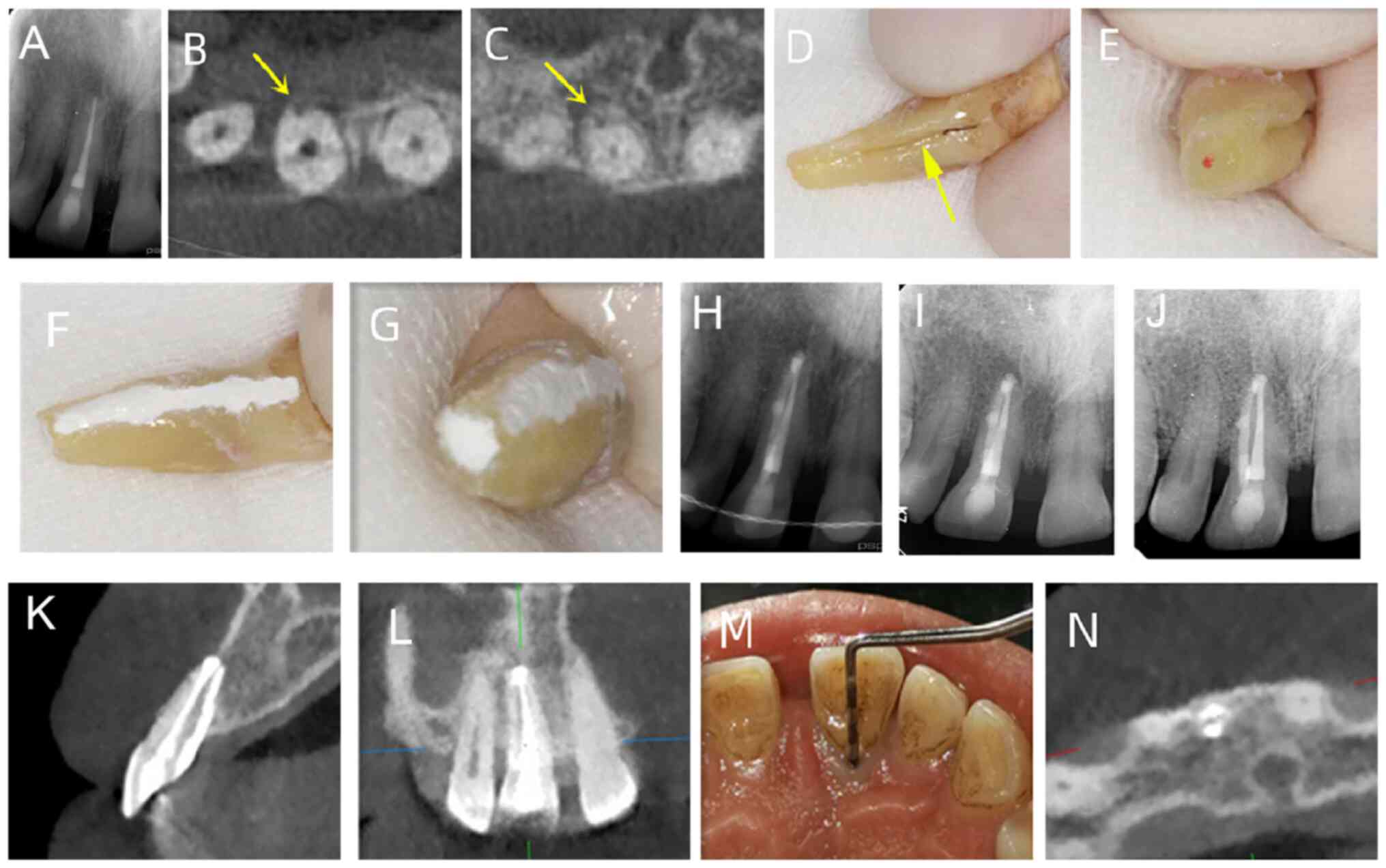
A 31-year-old female patient presented to the
Department of Endodontics of Liaocheng People's Hospital in
November 2020 with constant mild pain and tenderness to biting and
touching mucosa near tooth 12 for 1 month. From December 2019, the
patient underwent root canal treatment on the complaint tooth.
Following intraoral examination, a sinus tract was observed in the
alveolar mucosa, proximal to the apical area of tooth 12 (Fig. 4A); a palatal groove with ~5 mm
periodontal loss at the groove site was observed (Fig. 4B). Radiography showed an extra
canal beside the main one, a large periapical radiolucent lesion
and bone resorption related to the main root (Fig. 4C). The CBCT scan showed
invagination extending from the crown into the apex of the root
(pseudo canal), with no evident communication with the main canal
(Fig. 4D-G). The patient was
diagnosed with RDI (type II) and chronic apical periodontitis. The
aberrant anatomical structure hampered adequate sterilization and
obturation and conventional root canal treatment could not
eliminate the infected pulp tissue completely and seal the pseudo
canal tightly. The aim of the treatment for RDI is eradicating the
invagination and apical periodontitis; therefore, the patient
underwent conventional root canal treatment to the main root and
intentional replantation. Under a dental operating microscope, apex
of the extracted tooth was resected with high-speed handpiece for 3
mm and iRoot BP was placed to seal the retrograde cavity (Fig. 4H-K); the tooth was gently replanted
into the socket and fixed with composite resin splint (Fig. 4L). The 3-month follow-up radiograph
showed a reduction of the previous radiolucent area (Fig. 4M). A 1-year follow-up radiograph
was not collected as the patient was pregnant.
Case 5
A 54-year-old male patient was referred to the
Department of Endodontics of Liaocheng People's Hospital in
February 2021 for continuous sensitivity to palpation on the palate
side of tooth 11 for the past 3 years. The tooth had been treated
repeatedly with non-surgical root canal treatment during the past
12 months and received apical surgery 6 months ago. Intraoral
clinical examination revealed the tooth was filled with composite
restorative resin, and a radicular groove was detected in the
palatal face of the tooth extending from the cingulum to gingival
sulcus, with a nearly 10 mm probing depth. Periapical radiography
revealed a densely filled root canal and radiolucent area with an
opaque margin surrounding the apex of tooth 11 (Fig. 5A). CBCT indicated the
palatogingival groove extending from central fossa to the root apex
and the apical foramen being surrounded with a large periapical
radiolucent lesion (Fig. 5B and
C). The patient was diagnosed with
RDI (type II) and chronic apical periodontitis. The previous
treatment failure was caused by the aberrant anatomical structure
and the improper therapeutic strategy as conventional root canal
treatment cannot clean out the infected pulp tissue thoroughly and
seal the pseudo canal tightly. The patient underwent intentional
replantation and surgical treatment. Main root tip (~3 mm) was
resected and the root foramen was prepared by ultrasonic tips and
back-filled with iRoot BP (Fig.
5D-G); the tooth was replanted into its alveolar bone and fixed
by a wire and composite resin splint (Fig. 5H). At 6-month follow-up, the
patient was asymptomatic and radiograph examination showed a
reduction of the radiolucent area (Fig. 5I). At 24-month follow-up,
radiograph showed that the periapical radiolucent lesion
disappeared and the patient was asymptomatic (Fig. 5J-N).
Discussion
The clinical manifestation of DI can be a palatal
pit or groove, a barrel- or cone-shaped tooth, dilated crown or a
microdontic tooth (5). The deep
pit or groove of abnormal crown morphology, where saliva, food
remnants and bacteria are trapped, make DI teeth susceptible to
caries (23,24). If the enamel lining the surface of
the invagination is naturally absent or destroyed by caries,
bacteria and their products can diffuse to the pulp, leading to
pulpitis and periapical periodontitis (13,25).
Therefore, early and correct diagnosis of DI is especially
important to implement appropriate prevention or treatment
strategies for DI.
The complexity of DI is associated with its anatomy;
understanding the accurate anatomy is key to diagnose and treat DI.
Conventional radiological examinations, such as periapical and
panoramic radiograph, are routinely used for early diagnosis of DI.
However, these imaging techniques only show 2-D information and
cannot be used to depict the 3-D structure of the malformation;
misdiagnosis of the anomaly may lead to inappropriate treatment, as
in case 5. At present, 3-D imaging techniques in endodontics, such
as spiral CT and CBCT, are widely used in diagnosing and managing
DI (26,27). Due to its lower radiation dosage,
high efficiency and high resolution and accuracy, CBCT is a
preferable complementary examination to depict complicated root
canals of both CDI and RDI teeth, especially for type II and type
III (28). In case 4, CBCT
revealed a remnant root canal in the affected tooth, which was not
seen by periapical radiograph, leading to misdiagnosis and
treatment failure; many case reports reveal the superiority of CBCT
in detecting canal variations in DI (29,30).
A previous case report demonstrated that CBCT shows the accurate
location of the invagination and reveals no communication between
the invagination and the main root canal (31); in the aforementioned study,
according to the CBCT manifestation, conservative management,
endodontic treatment to invagination and untreated root canal with
a vital pulp was performed to allow the tooth to develop.
There are numerous reports about DI treatment
(32-35)
and several comprehensive treatments, such as combining surgical
and conservative endodontic management, have been suggested
(36); however, there is no
authoritative treatment standard being reported. Treatment of DI
depends on the type of invagination, complexity of root canal
anatomy, the pulp activity and the morphology of the apex.
Practitioners should select an appropriate therapeutic method or
design a regimen combining several methods according to the
individual condition. For CDI (type I) without pulp infection,
invagination sealing or filling is the first choice (32); however, Schmitz et al
(33) reported that even without
pulp infection, CDI (type I) should be treated with root canal. For
CDI with infected pulp or periapical inflammation but without
periodontal bone change, such as in case 1, conventional root canal
treatment is necessary. For CDI (type II) with infected pulp or a
periapical lesion, root canal treatment is necessary and thoroughly
eliminating infection in canal is key. Nasrabadi et al
(34) reported a type II DI
treated with root canal yielded favorable prognosis. There is a
controversy about whether the invaginated canal should be removed:
George et al (37) reported
a type II case in which, to avoid the decrease in root strength,
the main and the invaginated canal were filled separately without
removing the invagination. Subay and Kayatas (35) reported an immature type II DI
treated with apexification and filling both the root canal and the
invaginated canal; however, no sign of apex development appeared,
which was attributed to residual debris in invagination affected
cleaning and filling of the main root canal, resulting in poor
prognosis; therefore, removing the invagination thoroughly to
achieve sufficient canal cleaning is suggested, and this strategy
has become feasible through the application of microscopic and
ultrasonic techniques (38,39).
In cases 2 and 3, invaginations were removed completely with
ultrasonic techniques under a microscope, which facilitated
thorough debridement of the main canal. Apical barrier technique
provided complete apical sealing, resulting in good prognosis. The
root canal system of CDI (type III) is complex, so correct
assessment of the main pulp condition is key for treatment. If the
main pulp is healthy, to maintain the main canal pulp vitality,
only cleaning and filling the invaginated canal is suggested;
Heydari and Rahmani reported a case in which only the invaginated
canal was cleaned and filled; the periapical lesion resolved
completely and the tooth remained vital (40). If the main canal pulp is infected,
as reported by Agrawal et al (41), separate debriding and filling both
of the main and invaginated canal are needed. Other endodontists
suggest removing the extremely large anomalous invagination with
ultrasonic instruments and fusing the main canal and invaginated
canal as one space to benefit sterilization and sealing completely;
Martins et al (42)
reported a case of CDI (type III) in which dens were removed
regardless of whether pulp was infected and the main canal was
debrided and filled. If conservative treatment fails or the
invaginated canal cannot be cleaned and filled by traditional
methods, periapical surgery or intentional replantation is
recommended as an alternative to extraction (20,43).
Oliveira et al (44)
reported complex combined endodontic treatment of a type III DI in
a maxillary lateral incisor with extensive periapical lesion
affecting the buccal and palatine cortical bone treated with
endodontic and surgical treatment, including bioceramic sealer,
mineral trioxide aggregate (MTA) repair high plasticity and bone
graft. A retrospective study of ten cases of CDI (type III) with
apical periodontitis revealed survival rate of intentional
replantation was 80% (45). In
RDI, the lingual groove is a silent nidus for plaque formation,
contributes to coalescence between pulp and periodontal ligament
and leads to complicated combined periodontal-endodontic lesions.
Extraction has been the final resort in the past. Successful
treatment for RDI depends on both effective periodontal treatment
and resolution of associated localized periodontal defect, so
combined endodontic and periodontal treatment is suggested.
Periapical surgery combined with root amputation and sealing with
MTA and guided bone regeneration are suggested to restore the
original ridge volume in teeth without deep periodontal pockets
(46). Intentional replantation is
recommended because of its advantage in directly visualizing
length, depth, location of palatal grooves and debridement
infection thoroughly. Garrido et al (47) described a case of a maxillary
lateral incisor with deep palatogingival groove extending to the
root apex and severe periodontal destruction treated with
endodontic therapy and intentional replantation following
restoration with a self-etching flowable composite, resulting in
periodontal healing and notable healing of the periradicular
radiolucency. Tan et al (48) successfully treated a radicular
groove using a combination of endodontic therapy, intentional
replantation and root resection. For RDI cases with single-root,
intentional replantation with a 2-segment restoration method
(dividing the groove cavity into two parts at the cementoenamel
junction, then filling coronal part with flowable composite and
apical part with iRoot BP) is an optimal treatment to eliminate the
infection completely and promote periapical tissue regeneration
effectively (49). In cases 4 and
5, combined endodontic therapy, intentional replantation and root
resection with iRoot BP filling both the palatal groove and the
root apex was adopted, leading to good prognosis.
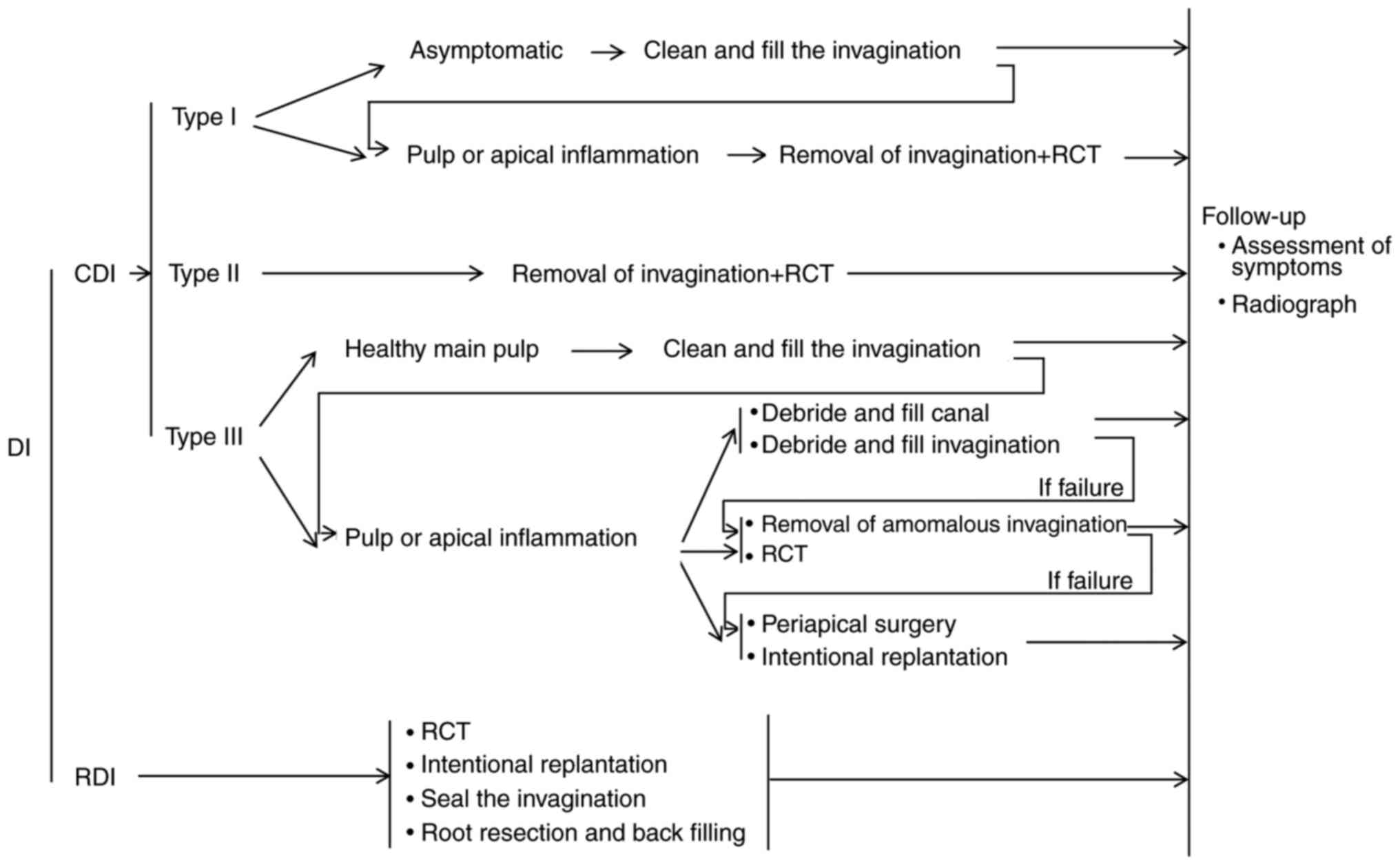
Strategy for DI treatment is shown in Fig. 6. The indicators for efficacy of DI
treatment in the Department of Endodontics of Liaocheng People's
Hospital include: i) No conscious symptoms, such as pain and
swelling; ii) no discomfort during chewing; iii) normal periapical
mucosal soft tissue without redness or abscess; iv) fistula
disappearance without tenderness and percussion; v) healthy gingiva
without redness, swelling or pus discharge and vi) radiographical
findings of intact tooth, tightly filled canal and periapical
lesions reduced or missed. In the present cases, lack of symptoms
and the aforementioned radiograph manifestations were considered
indicators for the efficacy of DI treatment, as previously reported
(16,30,50,51).
The complications of DI management methods are mainly secondary
pulpitis, periapical periodontitis and periodontal disease. When
complications occur, symptoms should be treated (for example, RCT
for pulpitis and periapical periodontitis). If a complication means
that the tooth cannot be saved, extraction along with a restoration
of the missing tooth is necessary.
Numerous types of congenital malformation can be
screened at an early stage; for example, cleft lip and palate can
be screened by genetic techniques or ultrasound inspection in the
embryonic development period (52,53).
Considering that DI is not a lethal or severely teratogenic
congenital malformation and is hard to screen during its
development, clinical therapy is more important than early
detection or prevention.
CBCT is an essential tool in assessing DI and
guiding treatment, especially in CDI (types II and III) and RDI
cases. Treatment should be based on the type of invagination,
complexity of root canal anatomy, level of pulp involvement,
morphology of apex and the periodontal status.
Acknowledgements
Not applicable.
Funding
Funding: The present study was supported by the Key Research and
Development Program of Liaocheng (grant no. 2022YDSF28).
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
RZ was responsible for conceptualization. CW and RZ
conceived the study and drafted the manuscript. DW and PL performed
treatments. RZ, LS and ZM collected and analyzed the data. CW and
LS supervised the study. CW, DW, PL, ZM and RZ reviewed and edited
the manuscript. ZM and RZ confirm the authenticity of all the raw
data. All authors have read and approved the final manuscript.
Ethics approval and consent to
participate
The present report was approved by the Ethics
Committee of Liaocheng People's Hospital (Shandong, China; approval
no. LC2020146).
Patient consent for publication
All patients involved in the present study provided
written informed consent for publication of their data and
images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Siqueira JF Jr, Rocas IN, Hernandez SR,
Brisson-Suárez K, Baasch AC, Pérez AR and Alves FRF: Dens
Invaginatus: Clinical implications and antimicrobial endodontic
treatment considerations. J Endod. 48:161–170. 2022.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Jimenez-Rubio A, Segura JJ, Jimenez-Planas
A and Llamas R: Multiple dens invaginatus affecting maxillary
lateral incisors and a supernumerary tooth. Endod Dent Traumatol.
13:196–198. 1997.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Gunduz K, Celenk P, Canger EM, Zengin Z
and Sumer P: A retrospective study of the prevalence and
characteristics of dens invaginatus in a sample of the Turkish
population. Med Oral Patol Oral Cir Bucal. 18:e27–e32.
2013.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Kirzioglu Z and Ceyhan D: The prevalence
of anterior teeth with dens invaginatus in the western
Mediterranean region of Turkey. Int Endod J. 42:727–734.
2009.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Zhu J, Wang X, Fang Y, Von den Hoff JW and
Meng L: An update on the diagnosis and treatment of dens
invaginatus. Aust Dent J. 62:261–275. 2017.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Gonzalez-Mancilla S, Montero-Miralles P,
Sauco-Marquez JJ, Areal-Quecuty V, Cabanillas-Balsera D and
Segura-Egea JJ: Prevalence of dens invaginatus assessed by CBCT:
Systematic review and meta-analysis. J Clin Exp Dent. 14:e959–e966.
2022.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Bansal AV, Bansal A, Kulkarni VK and Dhar
RS: Dens invaginatus in primary maxillary molar: A rare case report
and review of literature. Int J Clin Pediatr Dent. 5:139–141.
2012.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Yalcin TY, Bektas Kayhan K, Yilmaz A,
Goksel S, Ozcan I and Helvacioglu Yigit D: Prevalence,
classification and dental treatment requirements of dens
invaginatus by cone-beam computed tomography. PeerJ.
10(e14450)2022.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Segura JJ, Hattab F and Rios V: Maxillary
canine transpositions in two brothers and one sister: Associated
dental anomalies and genetic basis. ASDC J Dent Child. 69:54–58,
12. 2002.PubMed/NCBI
|
|
10
|
Oehlers FA: Dens invaginatus (dilated
composite odontome). I. Variations of the invagination process and
associated anterior crown forms. Oral Surg Oral Med Oral Pathol.
10:1204–1218 contd. 1957.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Alani A and Bishop K: Dens invaginatus.
Part 1: Classification, prevalence and aetiology. Int Endod J.
41:1123–1136. 2008.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Oehlers FA: The radicular variety of dens
invaginatus. Oral Surg Oral Med Oral Pathol. 11:1251–1260.
1958.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Cengiz SB, Korasli D, Ziraman F and Orhan
K: Non-surgical root canal treatment of Dens invaginatus: Reports
of three cases. Int Dent J. 56:17–21. 2006.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Arora S, Gill GS, Saquib SA, Saluja P,
Baba SM, Khateeb SU, Abdulla AM, Bavabeedu SS, Ali ABM and Elagib
MFA: Non-surgical management of dens invaginatus type IIIB in
maxillary lateral incisor with three root canals and 6-year
follow-up: A case report and review of literature. World J Clin
Cases. 10:12240–12246. 2022.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Kato H: Non-surgical endodontic treatment
for dens invaginatus type III using cone beam computed tomography
and dental operating microscope: A case report. Bull Tokyo Dent
Coll. 54:103–108. 2013.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Ghandi M and Jadidi S: Endodontic
management of type IIIb dens invaginatus in central incisor: A case
report. Clin Case Rep. 11(e7679)2023.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Mabrouk R, Berrezouga L and Frih N: The
Accuracy of CBCT in the detection of dens invaginatus in a Tunisian
population. Int J Dent. 2021(8826204)2021.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Leonardi Dutra K, Haas L, Porporatti AL,
Flores-Mir C, Nascimento Santos J, Mezzomo LA, Corrêa M and De Luca
Canto G: Diagnostic accuracy of cone-beam computed tomography and
conventional radiography on apical periodontitis: A systematic
review and meta-analysis. J Endod. 42:356–364. 2016.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Paula-Silva FW, Rocha CT, Flores DS,
Nelson-Filho P, Silva LA and Queiroz AM: Root canal treatment of an
immature dens invaginatus with apical periodontitis: A case report.
J Dent Child (Chic). 78:66–70. 2011.PubMed/NCBI
|
|
20
|
Zhang J, Li N, Li WL, Zheng XY and Li S:
Management of type IIIb dens invaginatus using a combination of
root canal treatment, intentional replantation, and surgical
therapy: A case report. World J Clin Cases. 10:6261–6268.
2022.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Yang J, Zhao Y, Qin M and Ge L: Pulp
revascularization of immature dens invaginatus with periapical
periodontitis. J Endod. 39:288–292. 2013.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Campello AF, Almeida BM, Franzoni MA,
Alves FRF, Marceliano-Alves MF, Rôças IN, Siqueira JF Jr and
Provenzano JC: Influence of solvent and a supplementary step with a
finishing instrument on filling material removal from canals
connected by an isthmus. Int Endod J. 52:716–724. 2019.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Yazdizadeh M, Sharifi M, Torabi Parizi A,
Alipour F, Ghasempuor M, Zanguei E and Yazdizadeh M: Dental
management of a pediatric patient with progressive familial
intrahepatic cholestasis having dental anomalies: A case report and
brief review of the literature. BMC Oral Health.
23(10)2023.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Chaturvedula BB, Muthukrishnan A,
Bhuvaraghan A, Sandler J and Thiruvenkatachari B: Dens invaginatus:
A review and orthodontic implications. Br Dent J. 230:345–350.
2021.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Ikemoto H: Bronchopulmonary aspergillosis:
Diagnostic and therapeutic considerations. Curr Top Med Mycol.
4:64–87. 1992.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Rozylo TK, Rozylo-Kalinowska I and Piskorz
M: Cone-beam computed tomography for assessment of dens invaginatus
in the Polish population. Oral Radiol. 34:136–142. 2018.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Reddy YP, Karpagavinayagam K and Subbarao
CV: Management of dens invaginatus diagnosed by spiral computed
tomography: A case report. J Endod. 34:1138–1142. 2008.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Teixido M, Abella F, Duran-Sindreu F,
Moscoso S and Roig M: The use of cone-beam computed tomography in
the preservation of pulp vitality in a maxillary canine with type 3
dens invaginatus and an associated periradicular lesion. J Endod.
40:1501–1504. 2014.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Vier-Pelisser FV, Pelisser A, Recuero LC,
So MV, Borba MG and Figueiredo JA: Use of cone beam computed
tomography in the diagnosis, planning and follow up of a type III
dens invaginatus case. Int Endod J. 45:198–208. 2012.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Azzahim L, Bassim N and Abdallaoui F: CBCT
evaluation and conservative management of a large periapical lesion
associated with dens invaginatus type II. Case Rep Dent.
2022(1529835)2022.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Patel S: The use of cone beam computed
tomography in the conservative management of dens invaginatus: A
case report. Int Endod J. 43:707–713. 2010.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Fayazi S, Bayat-Movahed S and White SN:
Rapid endodontic management of type II dens invaginatus using an
MTA plug: A case report. Spec Care Dentist. 33:96–100.
2013.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Schmitz MS, Montagner F, Flores CB, Morari
VH, Quesada GA and Gomes BP: Management of dens invaginatus type I
and open apex: Report of three cases. J Endod. 36:1079–1085.
2010.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Nasrabadi N, Naseri M, Khosraviani F and
Nematollahi Z: A successful non-surgical management of a type II
dens invaginatus with antimicrobial photodynamic therapy: A case
report. Iran Endod J. 18:59–62. 2023.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Subay RK and Kayatas M: Dens invaginatus
in an immature maxillary lateral incisor: A case report of complex
endodontic treatment. Oral Surg Oral Med Oral Pathol Oral Radiol
Endod. 102:e37–e41. 2006.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Ahmad S, Alam S, Andrabi SM and Kumar A:
Combined surgical and conservative endodontic management of
Oehler's type 3b dens invaginatus aided by guided tissue
regeneration. BMJ Case Rep. 16(e255546)2023.PubMed/NCBI View Article : Google Scholar
|
|
37
|
George R, Moule AJ and Walsh LJ: A rare
case of dens invaginatus in a mandibular canine. Aust Endod J.
36:83–86. 2010.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Sathorn C and Parashos P: Contemporary
treatment of class II dens invaginatus. Int Endod J. 40:308–316.
2007.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Kristoffersen O, Nag OH and Fristad I:
Dens invaginatus and treatment options based on a classification
system: Report of a type II invagination. Int Endod J. 41:702–709.
2008.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Heydari A and Rahmani M: Treatment of dens
invagination in a maxillary lateral incisor: A case report. Iran
Endod J. 10:207–209. 2015.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Agrawal PK, Wankhade J and Warhadpande M:
A rare case of type III dens invaginatus in a mandibular second
premolar and its nonsurgical endodontic management by using
cone-beam computed tomography: A case report. J Endod. 42:669–672.
2016.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Martins JNR, da Costa RP, Anderson C,
Quaresma SA, Corte-Real LSM and Monroe AD: Endodontic management of
dens invaginatus Type IIIb: Case series. Eur J Dent. 10:561–565.
2016.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Ozbas H, Subay RK and Ordulu M: Surgical
retreatment of an invaginated maxillary central incisor following
overfilled endodontic treatment: A case report. Eur J Dent.
4:324–328. 2010.PubMed/NCBI
|
|
44
|
Oliveira Fonseca F, Canal Vasconcellos B,
Martins Costa M, Ribeiro Sobrinho AP and Fonseca Tavares WL:
Combined endodontic and surgical therapy for resolution of type III
dens invaginatus. Iran Endod J. 15:117–123. 2020.PubMed/NCBI View Article : Google Scholar
|
|
45
|
Li N, Xu H, Kan C, Zhang J and Li S:
Retrospective study of Intentional replantation for type IIIb dens
invaginatus with periapical lesions. J Endod. 48:329–336.
2022.PubMed/NCBI View Article : Google Scholar
|
|
46
|
Giner-Lluesma T, Mico-Munoz P, Prada I,
Micó-Martínez P, Collado-Castellanos N, Manzano-Saiz A and
Albero-Monteagudo A: Role of cone-beam computed tomography (CBCT)
in diagnosis and treatment planning of two-rooted maxillary lateral
incisor with palatogingival groove. Case report. J Clin Exp Dent.
12:e704–e707. 2020.PubMed/NCBI View Article : Google Scholar
|
|
47
|
Garrido I, Abella F, Ordinola-Zapata R,
Duran-Sindreu F and Roig M: Combined endodontic therapy and
intentional replantation for the treatment of palatogingival
groove. J Endod. 42:324–328. 2016.PubMed/NCBI View Article : Google Scholar
|
|
48
|
Tan D, Li ST, Feng H, Wang ZC, Wen C and
Nie MH: Intentional replantation combined root resection therapy
for the treatment of type III radicular groove with two roots: A
case report. World J Clin Cases. 10:6991–6998. 2022.PubMed/NCBI View Article : Google Scholar
|
|
49
|
Yan H, Xu N, Wang H and Yu Q: Intentional
Replantation with a 2-segment restoration method to treat severe
palatogingival grooves in the maxillary lateral incisor: A report
of 3 cases. J Endod. 45:1543–1549. 2019.PubMed/NCBI View Article : Google Scholar
|
|
50
|
Cirakoglu NY and Cicek E: Nonsurgical
management of type II dens invaginatus with cone beam computed
tomography: A rare case. J Pak Med Assoc. 72:2559–2562.
2022.PubMed/NCBI View Article : Google Scholar
|
|
51
|
Kritika S, Bhandari SS, Benyocs G, Villa
Machado PA, Bishnoi N, Restrepo Restrepo FA, Karthikeyan K, Ataide
I and Mahalaxmi S: Demystifying dens invaginatus: Suggested
modification of the classification based on a comprehensive case
series. Eur Endod J. 7:73–80. 2022.PubMed/NCBI View Article : Google Scholar
|
|
52
|
Dabrowska J, Biedziak B, Szponar-Zurowska
A, Budner M, Jagodziński PP, Płoski R and Mostowska A:
Identification of novel susceptibility genes for non-syndromic
cleft lip with or without cleft palate using NGS-based multigene
panel testing. Mol Genet Genomics. 297:1315–1327. 2022.PubMed/NCBI View Article : Google Scholar
|
|
53
|
Liao M, Wang L, Shang N, Hu X, He B, Liu
X, Xiang G and Zhong W: Ultrasound measurements of fetal facial
profile markers and their associations with congenital
malformations during early pregnancy. BMC Pregnancy Childbirth.
23(772)2023.PubMed/NCBI View Article : Google Scholar
|