|
1
|
Singer M, Deutschman CS, Seymour CW,
Shankar-Hari M, Annane D, Bauer M, Bellomo R, Bernard GR, Chiche
JD, Coopersmith CM, et al: The third international consensus
definitions for sepsis and septic shock (Sepsis-3). JAMA.
315:801–810. 2016.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Yousuf F, Malik A, Saba A and Sheikh S:
Risk factors and compliance of surviving sepsis campaign: A
retrospective cohort study at tertiary care hospital. Pak J Med
Sci. 38:90–94. 2022.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Rudd KE, Johnson SC, Agesa KM, Shackelford
KA, Tsoi D, Kievlan DR, Colombara DV, Ikuta KS, Kissoon N, Finfer
S, et al: Global, regional, and national sepsis incidence and
mortality, 1990-2017: Analysis for the global burden of disease
study. Lancet. 395:200–211. 2020.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Lei S, Li X, Zhao H, Xie Y and Li J:
Prevalence of sepsis among adults in China: A systematic review and
meta-analysis. Front public Health. 10(977094)2022.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Shahsavarinia K, Moharramzadeh P, Arvanagi
RJ and Mahmoodpoor A: qSOFA score for prediction of sepsis outcome
in emergency department. Pak J Med Sci. 36:668–672. 2020.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Gorecki G, Cochior D, Moldovan C and Rusu
E: Molecular mechanisms in septic shock (Review). Exp Ther Med.
22(1161)2021.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Yoon SH, Choi B, Eun S, Bae GE, Koo CM and
Kim MK: Using the lactate-to-albumin ratio to predict mortality in
patients with sepsis or septic shock: A systematic review and
meta-analysis. Eur Rev Med Pharmacol Sci. 26:1743–1752.
2022.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Feng J, Wang L, Feng Y, Yu G, Zhou D and
Wang J: Serum levels of angiopoietin 2 mRNA in the mortality
outcome prediction of septic shock. Exp Ther Med.
23(362)2022.PubMed/NCBI View Article : Google Scholar
|
|
9
|
de Montmollin E, Aboab J, Mansart A and
Annane D: Bench-to-bedside review: Beta-adrenergic modulation in
sepsis. Crit Care. 13(230)2009.PubMed/NCBI View
Article : Google Scholar
|
|
10
|
Hartmann C, Radermacher P, Wepler M and
Nußbaum B: Non-hemodynamic effects of catecholamines. Shock.
48:390–400. 2017.PubMed/NCBI View Article : Google Scholar
|
|
11
|
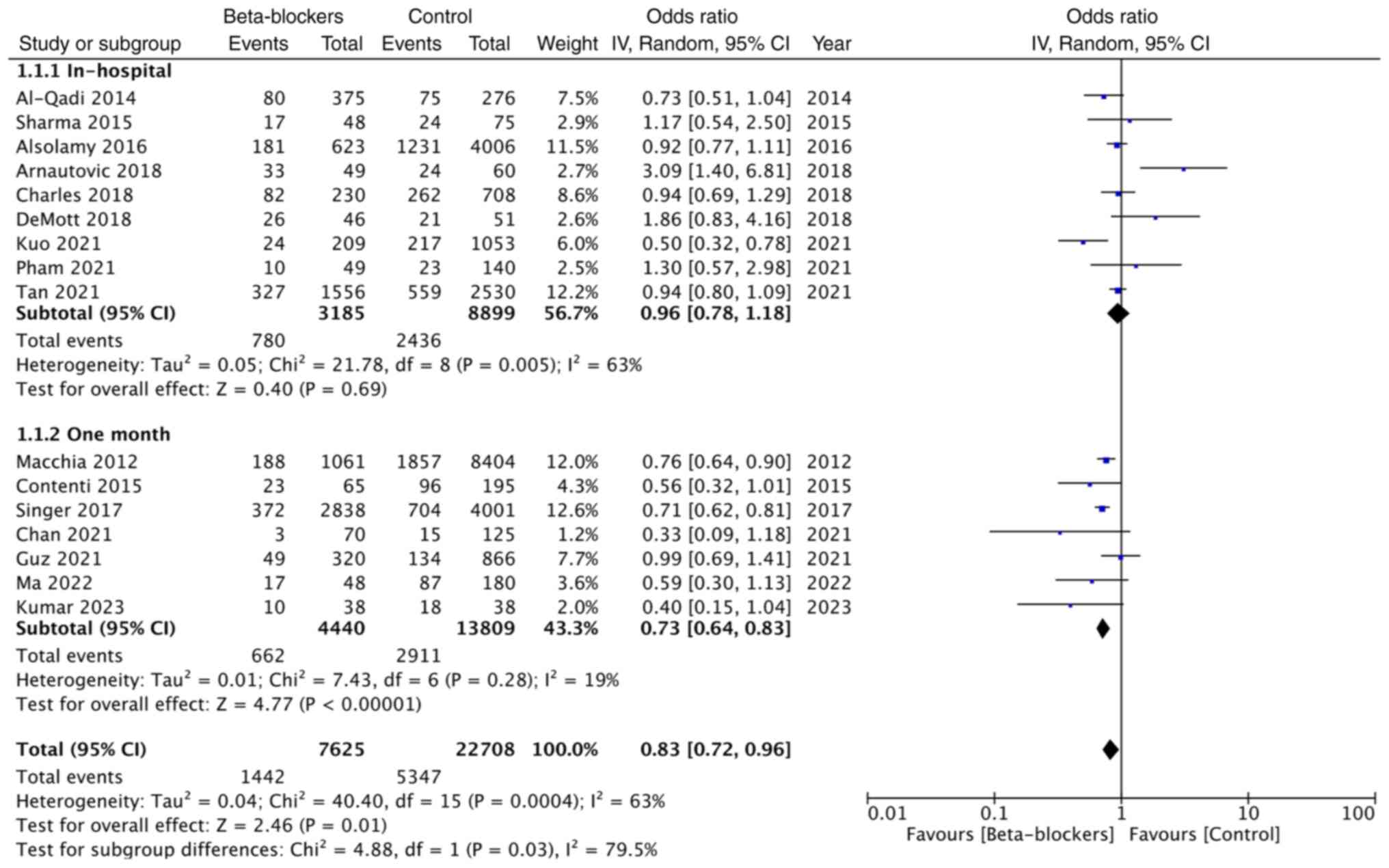
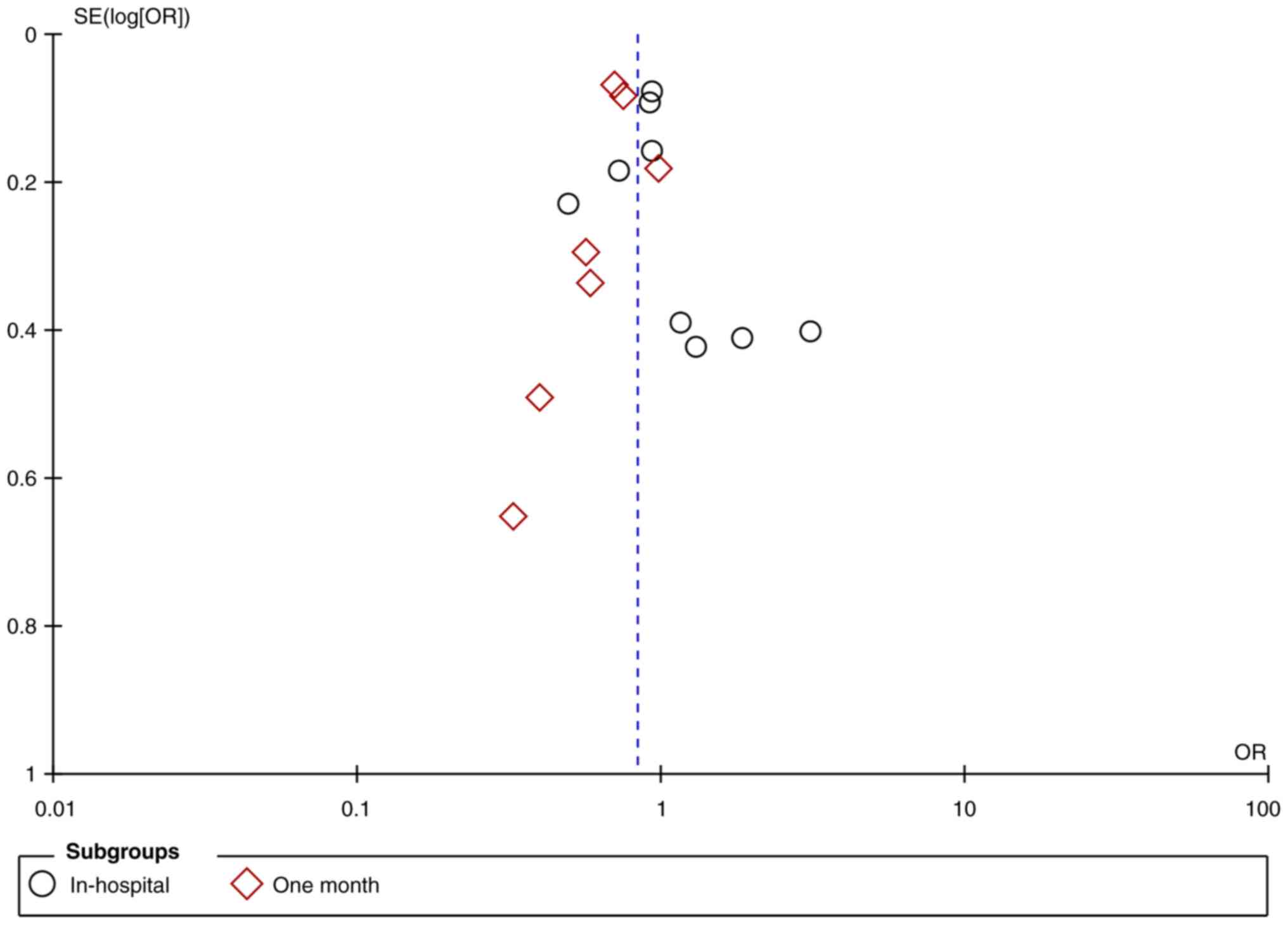
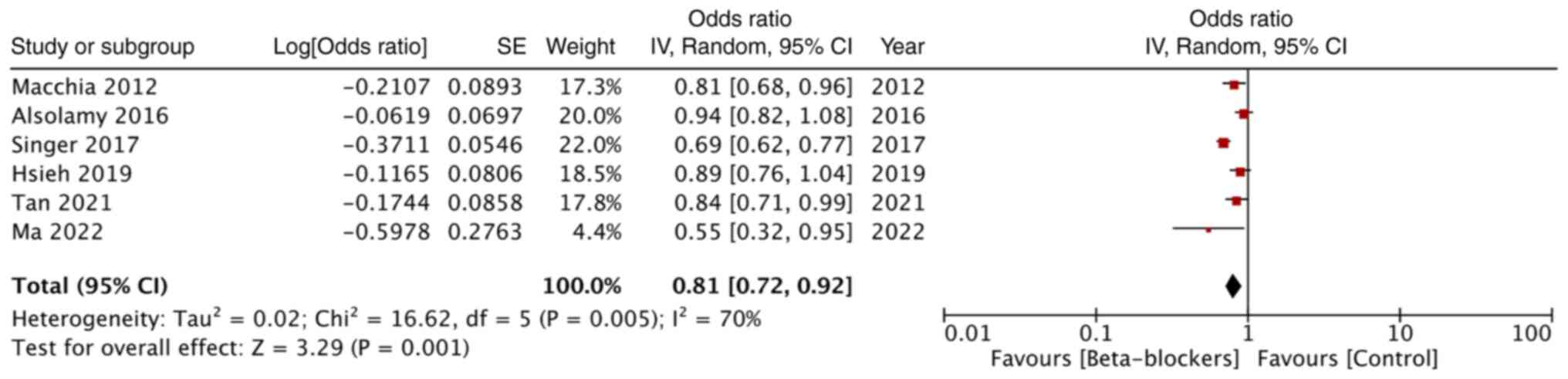
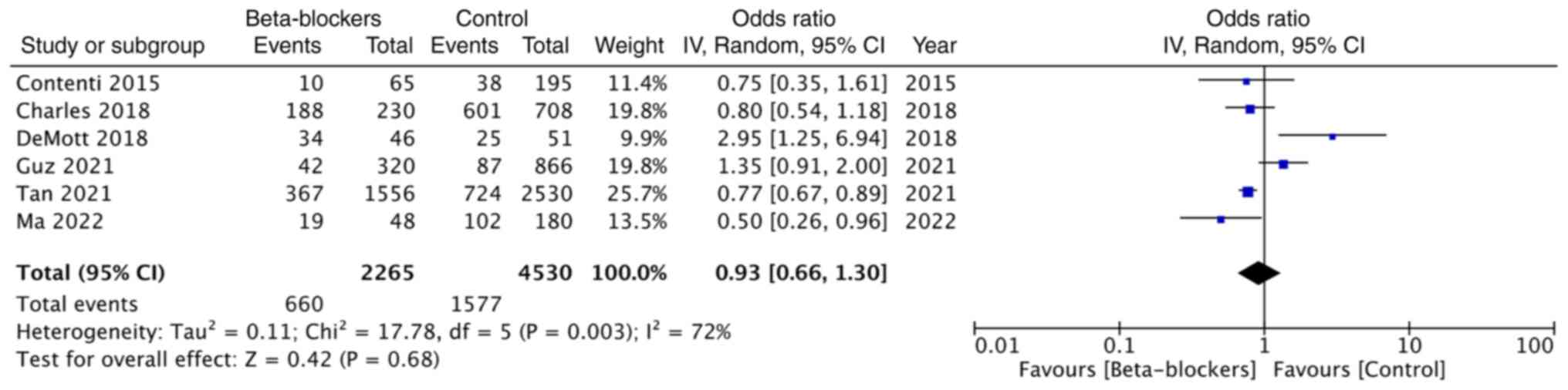
Hasegawa D, Sato R, Prasitlumkum N and
Nishida K: Effect of premorbid beta-blockers on mortality in
patients with sepsis: A systematic review and meta-analysis. J
Intensive Care Med. 37:908–916. 2022.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Singer M: Catecholamine treatment for
shock-equally good or bad? Lancet. 370:636–637. 2007.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Suzuki T, Suzuki Y, Okuda J, Kurazumi T,
Suhara T, Ueda T, Nagata H and Morisaki H: Sepsis-induced cardiac
dysfunction and β-adrenergic blockade therapy for sepsis. J
Intensive Care. 5(22)2017.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Morelli A, Ertmer C, Westphal M, Rehberg
S, Kampmeier T, Ligges S, Orecchioni A, D'Egidio A, D'Ippoliti F,
Raffone C, et al: Effect of heart rate control with esmolol on
hemodynamic and clinical outcomes in patients with septic shock: A
randomized clinical trial. JAMA. 310:1683–1691. 2013.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Hasegawa D, Sato R, Prasitlumkum N,
Nishida K, Takahashi K, Yatabe T and Nishida O: Effect of
ultrashort-acting β-blockers on mortality in patients with sepsis
with persistent tachycardia despite initial resuscitation: A
systematic review and meta-analysis of randomized controlled
trials. Chest. 159:2289–2300. 2021.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Arnautovic J, Mazhar A, Souther B,
Mikhijan G, Boura J and Huda N: Cardiovascular factors associated
with septic shock mortality risks. Spartan Med Res J.
3(6516)2018.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Sharma A, Vashisht R, Bauer S and Hanane
T: 1351: Effect of preadmission beta-blocker use on outcomes of
patients admitted with septic shock. Crit Care Med.
44(413)2016.
|
|
18
|
Kuo MJ, Chou RH, Lu YW, Guo JY, Tsai YL,
Wu CH, Huang PH and Lin SJ: Premorbid β1-selective (but not
non-selective) β-blocker exposure reduces intensive care unit
mortality among septic patients. J Intensive Care.
9(40)2021.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Tan K, Harazim M, Tang B, Mclean A and
Nalos M: The association between premorbid beta blocker exposure
and mortality in sepsis-a systematic review. Crit Care.
23(298)2019.PubMed/NCBI View Article : Google Scholar
|
|
20
|
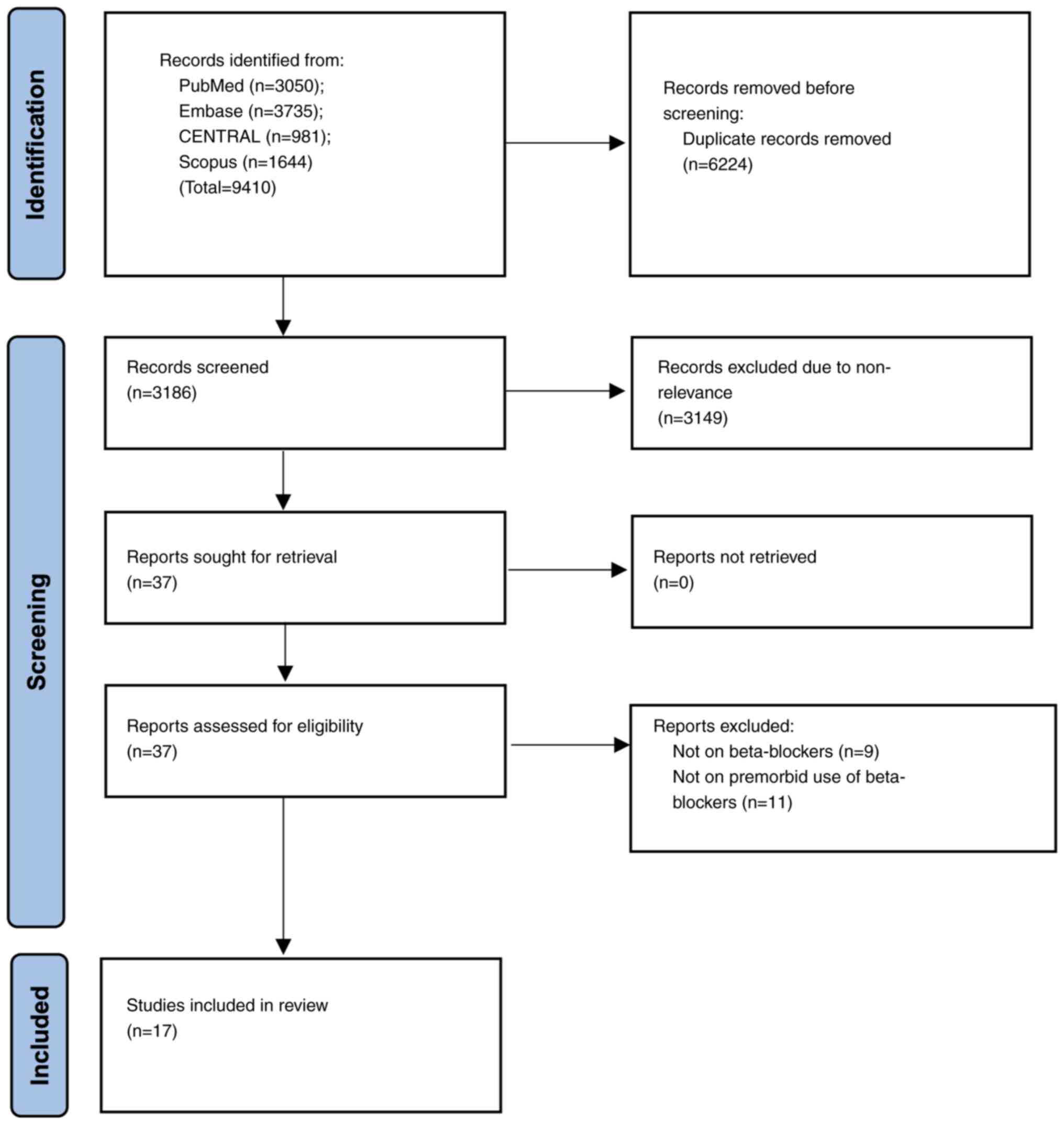
Page MJ, McKenzie JE, Bossuyt PM, Boutron
I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan
SE, et al: The PRISMA 2020 statement: An updated guideline for
reporting systematic reviews. Int J Surg. 88(105906)2021.PubMed/NCBI View
Article : Google Scholar
|
|
21
|
Wells G, Shea B, O'Connell D, Peterson J,
Welch V, Losos M and Tugwell P: The newcastle-ottawa scale (NOS)
for assessing the quality of nonrandomised studies in
meta-analyses.
|
|
22
|
DeMott JM, Patel G and Lat I: Effects of
chronic antihypertensives on vasopressor dosing in septic shock.
Ann Pharmacother. 52:40–47. 2018.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Hsieh MS, How CK, Hsieh VCR and Chen PC:
Preadmission antihypertensive drug use and sepsis outcome: Impact
of angiotensin-converting enzyme inhibitors (ACEIs) and angiotensin
receptor blockers (ARBs). Shock. 53:407–415. 2020.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Guz D, Buchritz S, Guz A, Ikan A, Babich
T, Daitch V, Gafter-Gvili A, Leibovici L and Avni T: β-Blockers,
tachycardia, and survival following sepsis: An observational cohort
study. Clin Infect Dis. 73:e921–e926. 2021.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Pham D, Ward H, Yong B, Raj JM, Awad M,
Harvey M, Doherty S and Cave G: Is lactate lower in septic patients
who are prescribed beta blockers? Retrospective cohort study of an
intensive care population. Emerg Med Australas. 33:82–87.
2021.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Tan K, Harazim M, Simpson A, Tan YC,
Gunawan G, Robledo KP, Whitehead C, Tang B, Mclean A and Nalos M:
Association between premorbid beta-blocker exposure and sepsis
outcomes-the beta-blockers in european and Australian/American
septic patients (BEAST) study. Crit Care Med. 49:1493–1503.
2021.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Ma Y, Ma J and Yang J: Association between
pre-existing long-term β-blocker therapy and the outcomes of
sepsis-associated coagulopathy: A retrospective study. Medicina
(Kaunas). 58(1843)2022.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Kumar S, Malviya D, Tripathi M, Rai S,
Nath SS, Tripathi SS and Mishra S: Exploring the impact of prior
beta-blocker and calcium channel blocker usage on clinical outcomes
in critically Ill patients with sepsis: An observational study.
Cureus. 15(e46169)2023.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Charles D, Jean-Francois L, Matthieu J,
Charpentier J, Cariou A and Chiche JD: Hemodynamic parameters of
septic shock patients treated with prior BB therapy. In:
Proceedings of Réanimation. Ann Intensive Care, p8, 2018.
|
|
30
|
Alsolamy S, Ghamdi G, Alswaidan L, Alharbi
S and Alenezi F: Association between previous prescription of
βblockers and mortality rate among septic patients: A retrospective
observational study. In: 36th International Symposium on Intensive
Care and Emergency Medicine. Crit Care, p20, 2016.
|
|
31
|
Al-Qadi M, O'Horo J, Thakur L, Kaur S,
Berrios R and Caples S: Long- term use of beta blockers is
protective in severe sepsis and septic shock. Am J Resp Crit Care
Med. 189(A6655)2014.
|
|
32
|
Macchia A, Romero M, Comignani PD, Mariani
J, D'Ettorre A, Prini N, Santopinto M and Tognoni G: Previous
prescription of β-blockers is associated with reduced mortality
among patients hospitalized in intensive care units for sepsis.
Crit Care Med. 40:2768–2772. 2012.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Contenti J, Occelli C, Corraze H, Lemoël F
and Levraut J: Long-term β-blocker therapy decreases blood lactate
concentration in severely septic patients. Crit Care Med.
43:2616–2622. 2015.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Singer KE, Collins CE, Flahive JM, Wyman
AS, Ayturk MD and Santry HP: Outpatient beta-blockers and survival
from sepsis: Results from a national cohort of Medicare
beneficiaries. Am J Surg. 214:577–582. 2017.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Chan JZW, Tan JH, Lather KS, Ng AJY, Ong
Z, Zou X, Chua MT and Kuan WS: Beta-blockers' effect on levels of
Lactate in patients with suspected sepsis-The BeLLa study. Am J
Emerg Med. 38:2574–2579. 2020.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Nakayama T, Yoshiike N and Yokoyama T:
Clinicians and epidemiologists view crude death rates differently.
BMJ. 318(395)1999.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Fleischmann C, Thomas-Rueddel DO, Hartmann
M, Hartog CS, Welte T, Heublein S, Dennler U and Reinhart K:
Hospital incidence and mortality rates of sepsis. Dtsch Arztebl
Int. 113:159–166. 2016.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Garg R, Tellapragada C, Shaw T, Eshwara
VK, Shanbhag V, Rao S, Virk HS, Varma M and Mukhopadhyay C:
Epidemiology of sepsis and risk factors for mortality in intensive
care unit: A hospital based prospective study in South India.
Infect Dis (Lond). 54:325–334. 2022.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Ren Y, Zhang L, Xu F, Han D, Zheng S,
Zhang F, Li L, Wang Z, Lyu J and Yin H: Risk factor analysis and
nomogram for predicting in-hospital mortality in ICU patients with
sepsis and lung infection. BMC Pulm Med. 22(17)2022.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Lee YR, Seth MS, Soney D and Dai H:
Benefits of beta-blockade in sepsis and septic shock: A systematic
review. Clin Drug Investig. 39:429–440. 2019.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Whitehouse T, Hossain A, Perkins GD,
Gordon AC, Bion J, Young D, McAuley D, Singer M, Lord J, Gates S,
et al: Landiolol and organ failure in patients with septic shock:
The STRESS-L randomized clinical trial. JAMA. 330:1641–1652.
2023.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Fuchs C, Wauschkuhn S, Scheer C, Vollmer
M, Meissner K, Kuhn SO, Hahnenkamp K, Morelli A, Gründling M and
Rehberg S: Continuing chronic beta-blockade in the acute phase of
severe sepsis and septic shock is associated with decreased
mortality rates up to 90 days. Br J Anaesth. 119:616–625.
2017.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Dünser MW and Hasibeder WR: Sympathetic
overstimulation during critical illness: Adverse effects of
adrenergic stress. J Intensive Care Med. 24:293–316.
2009.PubMed/NCBI View Article : Google Scholar
|
|
44
|
Annane D, Vignon P, Renault A, Bollaert
PE, Charpentier C, Martin C, Troché G, Ricard JD, Nitenberg G,
Papazian L, et al: Norepinephrine plus dobutamine versus
epinephrine alone for management of septic shock: A randomised
trial. Lancet. 370:676–684. 2007.PubMed/NCBI View Article : Google Scholar
|
|
45
|
Herndon DN, Hart DW, Wolf SE, Chinkes DL
and Wolfe RR: Reversal of catabolism by beta-blockade after severe
burns. N Engl J Med. 345:1223–1229. 2001.PubMed/NCBI View Article : Google Scholar
|