Introduction
Lung carcinoma is one of the most common malignant
tumors in China, with an incidence rate that ranks second in the
country; moreover, it has a mortality rate that ranks first
globally (1). Lung carcinoma is
classified into non-small-cell lung carcinoma (NSCLC) and
small-cell lung carcinoma (SCLC), of which SCLC accounts for ~15%
of lung carcinomas (2). SCLC is
characterized by a high proliferation rate, a tendency for early
metastasis and a poor prognosis (3). Most patients with SCLC have already
developed distal metastasis at the time of diagnosis. Intraocular
tumors can threaten the patient's vision and even life. Moreover,
symptoms of ocular metastatic carcinoma can be the same or similar
to symptoms of the primary tumor (4). Therefore, ocular metastatic carcinoma
is easily overlooked, making accurate diagnosis and treatment more
crucial. Case reports regarding eye metastasis in SCLC indicate
that right-sided eye metastasis is rare (5). The present study reported a case of
SCLC with right-sided eye metastasis. It gives a comprehensive
report of the patient's treatment process, in order to provide a
reference for the clinical diagnosis and treatment of ocular
metastatic carcinoma.
Case presentation
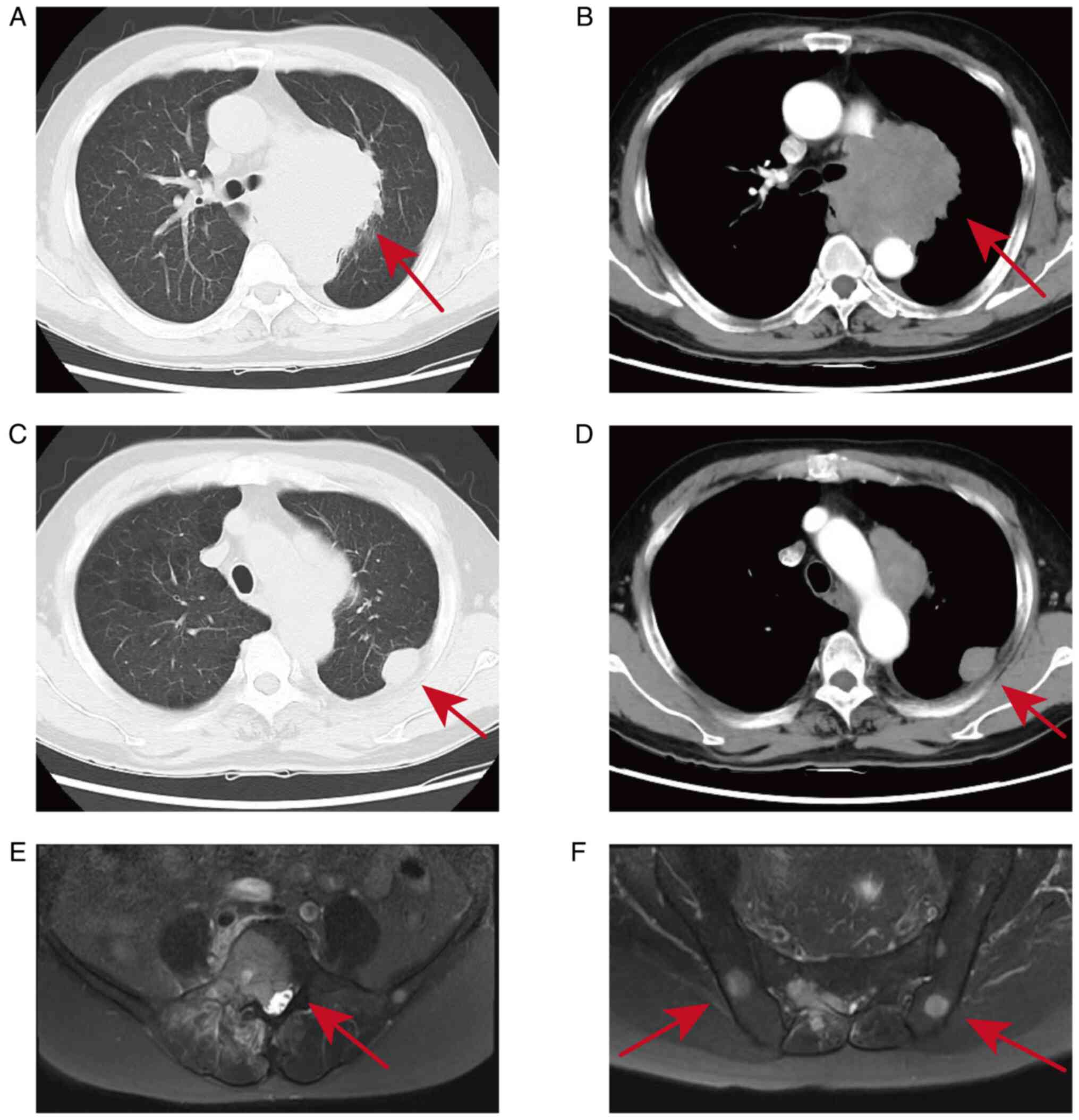
A 54-year-old male patient presented with right
flank pain and limited mobility of the right lower limb,
accompanied by numbness, which began in April 2023. In June 2023,
the patient was treated at Lu'an Hospital, which is affiliated with
Anhui University of Chinese medicine (Anhui, China). A lumbar
magnetic resonance imaging (MRI) scan indicated a high possibility
of bone metastasis (Fig. 1E and
F). A further contrast-enhanced
chest computed tomography (CT) revealed a malignant lesion at the
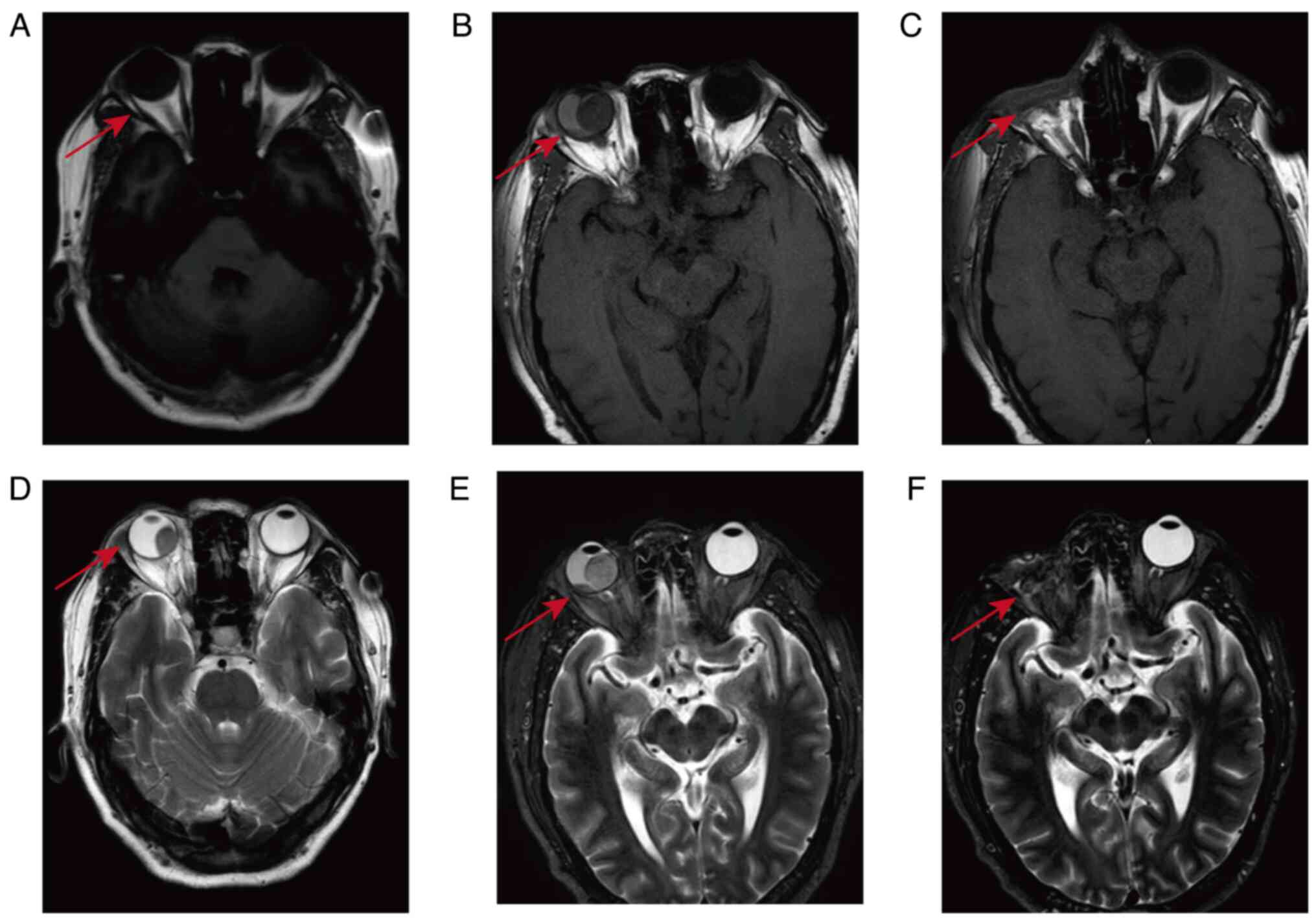
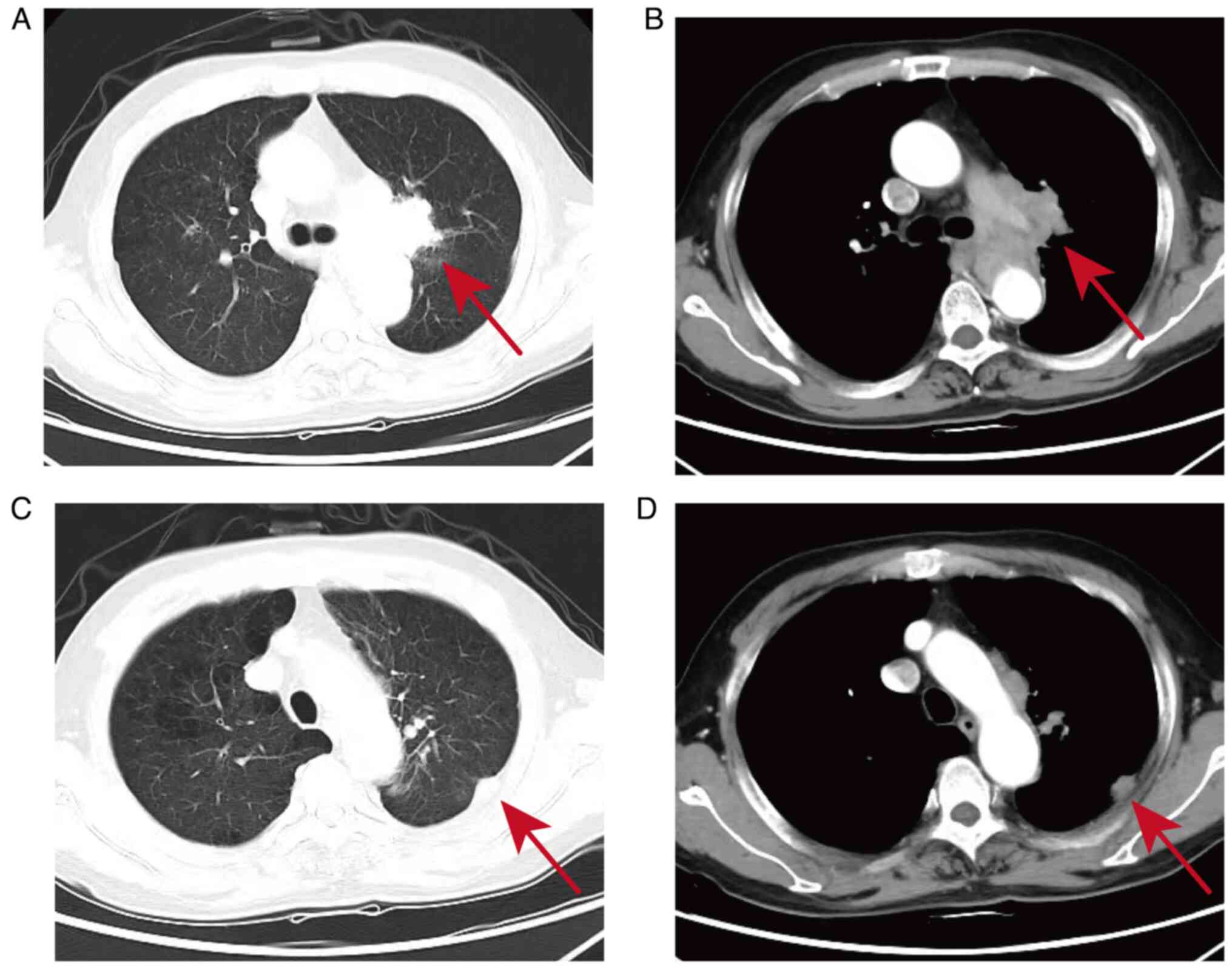
hilum of the left lung with pleural metastases (Fig. 1A and B). Cranial MRI suggested a possible
metastatic lesion in the right eye (Fig. 2A and D). The patient underwent a pulmonary
tissue biopsy and subsequent immunohistochemical staining.
The lung tissue was immersed in 4% neutral formalin
at 37˚C for 24 h. It was then dehydrated with different
concentrations of ethanol and finally embedded in paraffin. A 4 µm
tissue section adhering to the glass slide was baked in a 60˚C oven
for 1.5 h. Subsequently, an immunohistochemical experiment was
conducted using the Roche BenchMark XT fully automated
immunohistochemical instrument (Roche Diagnostics). Detailed
operational procedures were as follows: Heat dewaxing was performed
using EZ Prep (dehydrating solution, 1:10, lot number: K14102;
Roche Diagnostics). Then, CC1 (alkaline repair solution, pH
8.0-8.5, lot number: 77307801; Roche Diagnostics) was applied at
100˚C for a given period of time (depending on the type of
antibody), with an increase in heating time of 8 min and a cooling
time of 7 min. Blocking was performed using a UV Inhibitor
(hydrogen peroxide, lot number: K13635-K13800; Roche Diagnostics)
for 4 min. A primary antibody was added and the mixture incubated
for a specified period of time. The antibodies with an antigen
retrieval time of 36 min included: CD56 (rabbit monoclonal, cat.
no. IR040; incubation time: 36 min), CK5/6 (mouse monoclonal, lot
no. IM060; incubation time: 36 min), NapsinA (mouse monoclonal,
cat. number: IM198; incubation time: 40 min), Ki-67 (rabbit
monoclonal, lot number: IR098; incubation time: 40 min). The
antibodies with an antigen retrieval time of 64 min included: P40
(rabbit monoclonal, lot number: IR345; incubation time: 36 min),
TTF-1 (rabbit monoclonal, lot no. IR301; incubation time: 36 min),
CgA (mouse monoclonal, lot number: IM053; incubation time: 40 min),
LCA (mouse monoclonal, lot number: IM038; incubation time: 40 min)
(all antibodies were stock solutions from Abcam; temperature was
37˚C). The UV HRP-Multimer (the second antibody, comprising
HRP-labeled goat anti-mouse IgG, goat anti-mouse IgM and goat
anti-rabbit antibodies, ~55 µg/ml, lot number: K13635-K13799; Roche
Diagnostics) was added to the mixture and incubate for 8 min. UV
DAB (3,3'-diaminobenzidine reagent; lot number: K13635-K13802;
Roche Diagnostics) and UV H2O2 (phosphate
buffer solution containing 0.04% hydrogen peroxide, lot number:
K13635-K13803; Roche Diagnostics) were added and incubate for 8
min. UV Copper (an enhancer containing 5 g/l copper sulfate, lot
number: K13635-K13805; Roche Diagnostics) was added and incubate
for 4 min. Hematoxylin Ⅱ (lot number: K14384; Roche Diagnostics)
was added and incubated for 12 min. bluing reagent (lot number:
K12265; Roche Diagnostics) was added and incubated for 4 min. Upon
completion, The tissue sections on the slides were dehydrated,
mounted in a neutral resin and then imaged using an optical
microscope.
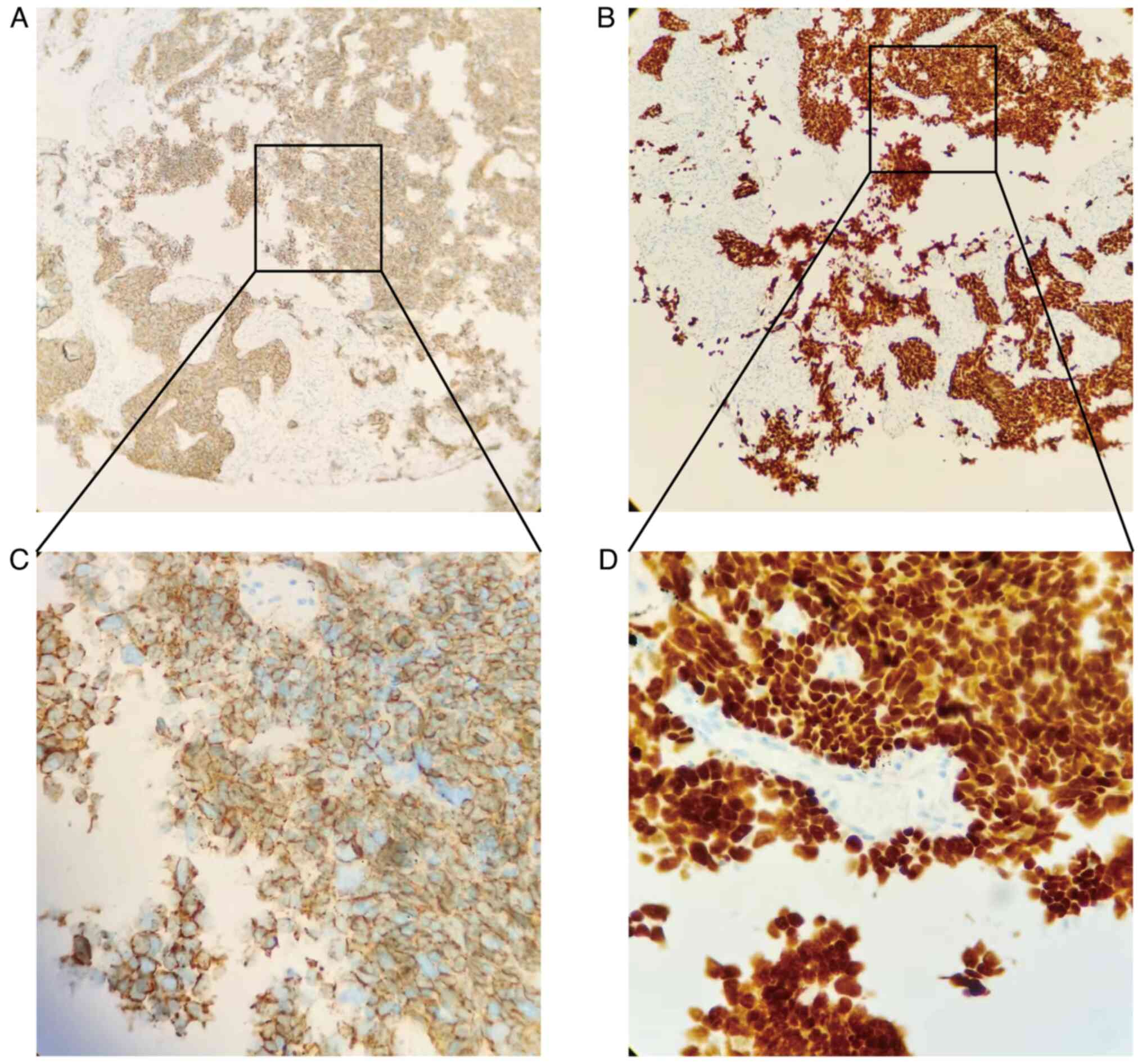
Based on the results of lung histopathology
(Fig. 3) and immunohistochemistry
(IHC; Fig. 4A-D) and after ruling
out other neuroendocrine tumors, the patient was diagnosed with
SCLC of the left lung, stage T4N1M1c, IVB. The patient did not have
a family history of hereditary diseases. The patient is divorced
and has one daughter. The patient has been smoking for >30
years.
Starting in June 2023, the patient was treated with
enverolumab and etoposide and cisplatin every three weeks as a
course of treatment: Enverolumab 400 mg subcutaneously on day 1;
Etoposide 120 mg intravenously on days 1-3; and Cisplatin 30 mg
intravenously on days 1-3. In July 2023, after one course of
treatment, the patient experienced decreased and blurred vision in
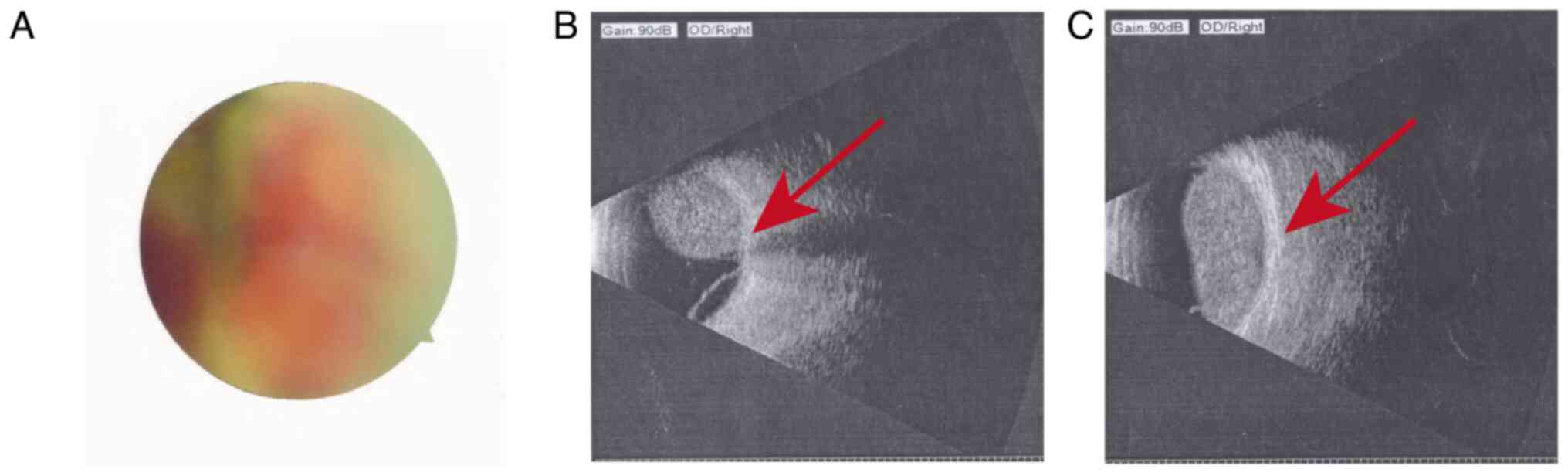
both eyes. The ophthalmological consultation indicated that the
intraocular pressure of both eyes was as follows: Right/left: 16/18
mmHg. Right fundus photography (Fig.
5A) and right eye ultrasound (Fig.
5B-C) showed a space-occupying lesion in the vitreous chamber
and retinal detachment in the right eye. The treatment plan
primarily focused on systemic therapy. In August 2023, after two
courses of treatment, the patient experienced pain in the right
eye. The ophthalmologic consultation indicated an intraocular
pressure of 32 mmHg in the right eye. The contrast-enhanced MRI of
the orbits showed abnormal enhancement signals and a detached state
of the retinal membrane on the right eyeball (Fig. 2B and E). At 4 days later, there was significant
conjunctival congestion in the right eye (Fig. 6A and B). Within a week, the patient reported
experiencing total blindness in the right eye and the oral
oxycodone dose was rapidly increased to 40 mg every 12 h (q12h).
Following consultations with a multiple disciplinary team (MDT), it
was decided not to opt for ocular radiation treatment due to the
absence of visual acuity in the right eye. Even if radiation
therapy proved to be effective, visual acuity could not be
restored. Later in August 2023, the patient underwent enucleation
of the right eyeball. This was performed at the 901 Hospital of the
People's Liberation Army of China, which is located in Hefei, Anhui
(China). The patient provided the hospital's postoperative
pathology and immunohistochemical results. Postoperative pathology
revealed a small-cell malignant tumor in the right eyeball
(Pathology Report Number: 2306821). When the patient's IHC results
were examined in combination with the medical history, there was a
tendency for pulmonary small-cell metastasis to the right eyeball.
The tumor measured 2x2x1.3 cm and invaded the retina and choroid,
but not the sclera. IHC (23-506) results were as follows: TTF-1(-),
P40(-), Syn(+), NapsinA(-), CD56(+) and CgA(-). The Ki-67 hotspot
area covered ~70%. The patient continued to be treated at Lu'an
Hospital (Anhui, China). The postoperative recovery of the eye was
good (Fig. 6C). After four courses
of treatment, a contrast-enhanced MRI of the orbits was performed
in September 2023. This showed the absence of the right eyeball,
with no metastatic lesions in the left eye (Fig. 2C and F). In October 2023, by the sixth course
of treatment, the contrast-enhanced chest CT showed that the hilar
and pleural metastatic lesions had reduced in size compared to June
(Fig. 7A-D). During the treatment
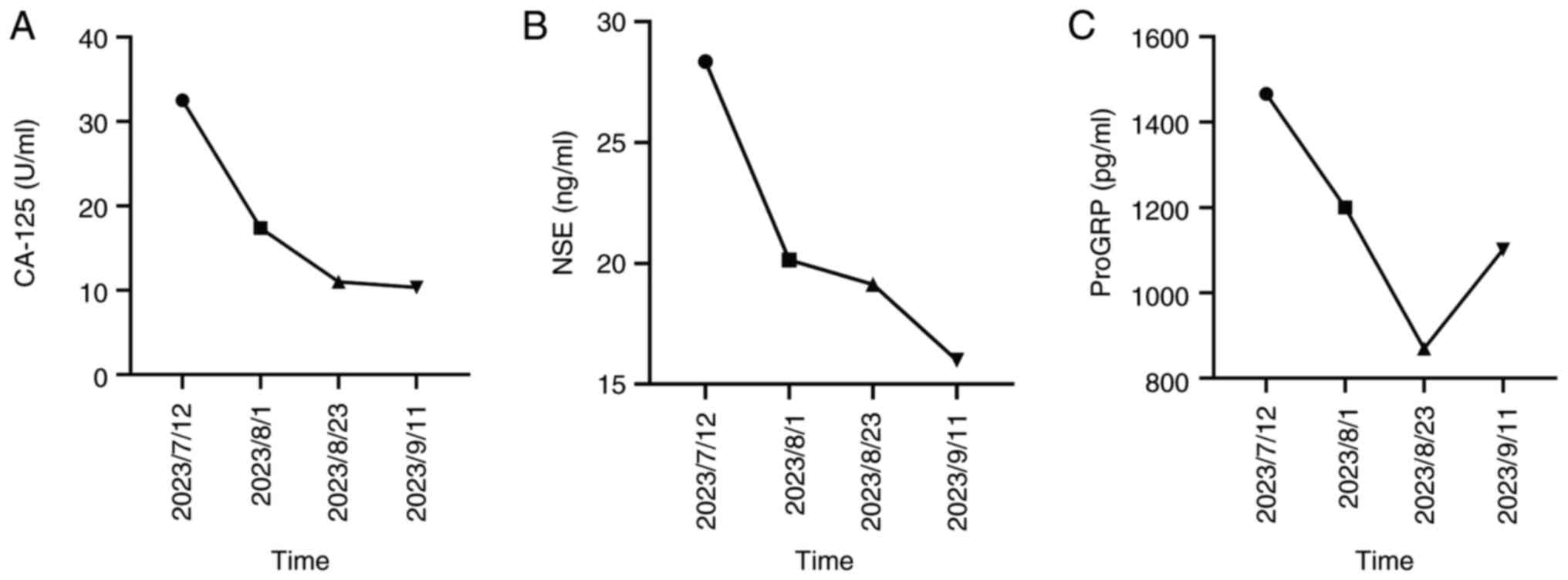
period, the levels of carbohydrate antigen 125 (CA-125),
neuron-specific enolase (NSE) and progastrin-releasing peptide
(ProGRP) decreased (Fig. 8). In
addition, the demonstrated vertebral metastases were treated with
radiotherapy (30 Gy/10 fractions). Currently, the condition of the
patient is stable, with ongoing oral administration of anlotinib
(12 mg qd). In addition, follow-up visits are continuing.
Discussion
SCLC is a high-grade neuroendocrine carcinoma
(6). It is an aggressive
smoking-related malignancy characterized by rapid growth and early
metastatic spread (7). Depending
on the extent of tissue involvement, SCLC is generally divided into
limited period and extensive stages (8). The extensive stage accounts for ~70%
of SCLC cases (9), with the most
common sites of metastasis being the brain, liver, or bone
(10). There are also reports of
ocular metastasis from SCLC (11).
Intraocular tumors are classified into primary and
metastatic tumors. Metastatic tumors in the eye can originate from
various tissues and organs throughout the body. The most common
primary tumor sites that lead to intraocular metastasis are the
breasts (40-47%) and lungs (21-29%) (12). Additionally, primary tumors in
other locations can also metastasize to the eye, such as the kidney
(13), stomach (14) and pancreas (15).
The eyes lack a lymphatic system, with most eye
metastatic tumors arising from hematogenous spread (16). Metastatic tumors in the eye mainly
occur in the uveal tissue due to its abundant blood supply and
multiple vascular connections, with the choroid being the most
frequent location (17).
Intraocular metastatic tumors are relatively rare (18). The ophthalmic artery branches at a
right angle to the internal carotid artery. This anatomical feature
increases the likelihood of tumor emboli in the bloodstream getting
lodged within the intracranial cavity due to the rapid blood flow.
Consequently, these emboli are less likely to enter the eye through
the ophthalmic artery. The incidence of intraocular metastases to
the left eye may be slightly higher, based on anatomical
characteristics (19). That is,
the bloodstream of the right eye must bypass the innominate artery
to travel upward, whereas the left common carotid artery can
directly ascend into the left eye.
The most common ocular symptoms of intraocular
metastasis are blurred vision and loss of vision (20). These often occur due to invasion of
the macular area or the area around the optic disc, leading to
subretinal exudation which causes retinal detachment. Other
symptoms include eye pain, floating objects in the vision, visual
field defects, abnormal eye position, proptosis, increased orbital
pressure, diplopia and restricted eye movement.
The ocular manifestations of metastatic tumors may
serve as the initial symptoms of the primary tumor (21-23).
Misdiagnosis or missed diagnosis of eye metastases may lead to
rapid deterioration of the condition. If detected late, it may
invade the contralateral optic nerve along the orbital floor,
leading to bilateral vision loss and potentially blindness
(24-26).
Within the clinical literature, there are cases of ocular
metastatic carcinomas misdiagnosed as secondary glaucoma, leading
to vision loss and the need for enucleation of the eyeball
(27). Therefore, for patients
suspected of having metastatic carcinoma in the eye, early
diagnosis is crucial. This can be achieved through a comprehensive
evaluation of the patient's signs and symptoms, as well as
necessary auxiliary examinations, to formulate an appropriate
treatment plan.
Clinical manifestations serve as the basis for the
early diagnosis of eye metastases. If a patient shows signs of
suspected malignant tumors in the eyes, an immediate examination
should be conducted to identify potential orbital metastases.
Diagnostic confirmation can be achieved through a comprehensive
array of modalities, including: funduscopy, ocular ultrasound,
optical coherence tomography (OCT), fundus fluorescence angiography
(FFA), indocyanine green angiography, CT, MRI and, when necessary,
histopathological examination via fine-needle aspiration biopsy
(FNAB) (28).
The treatment for intraocular metastatic tumors
primarily involves systemic and localized therapies (29). However, systemic treatment often
leads to secondary resistance. For eye metastases, local treatment
is recommended either concurrently or following systemic therapy
(30). Radiation therapy is the
primary localized treatment for eye metastases (31). Ocular radiation therapy can
eradicate localized tumors, control pain and improve vision.
Specifically, studies have indicated that in a group of 15 patients
(19 eyes) who underwent reflexotherapy, 11 out of 13 (84.6%) showed
improvement in vision and 14 out of 15 (93.3%) experienced partial
or complete remission (CR) of their ocular tumors (32). When the ocular metastatic carcinoma
causes severe pain or discomfort that cannot be alleviated by
medication or other conservative treatments and the eyeball loses
its normal function, enucleation of the eyeball may be
performed.
The use of enverolumab as a treatment was based on
the protocol provided by the Cancer Hospital, which is affiliated
with the Fudan University in Shanghai, China. After patient
consultation, the patient's family requested the use of this
protocol. According to the Chinese Society of Clinical Oncology
guidelines, enverolumab is not recommended as a first-line
treatment for extensive small cell lung carcinoma (ES-SCLC).
However, a review of relevant literature revealed clinical studies
on the use of a combination of enverolumab with
carboplatin/cisplatin and etoposide as a first-line treatment for
ES-SCLC (33). Therefore, the
hospital's recommendation was followed and this protocol was
accordingly implemented.
In the present case, the patient experienced a
sudden loss of vision and intense pain in the right eye within a
short period of time. Upon examination using funduscopy, ophthalmic
ultrasound, OCT and eye MRI, a metastatic lesion was suspected.
After MDT consultations, surgical extraction was chosen.
Postoperatively, the patient's pain and quality of life improved
markedly. Systemic treatment using immunotherapy combined with
chemotherapy resulted in a decrease in lung lesions. However,
eyeball extraction is a destructive procedure that should be
performed cautiously when multiple lines of evidence are
established. If possible, hospitals should conduct
multidisciplinary discussions. If the patient's eye pain is not
severe, local radiation therapy should be the first choice. Early
diagnosis and treatment of the ocular metastatic carcinoma can help
control tumor spread, preserve vision and improve the patient's
quality of life. When clinical symptoms suggest a suspected
malignant tumor in the eye, a comprehensive cancer investigation
should be conducted using funduscopy, ophthalmic ultrasound, OCT,
FFA, CT, MRI and FNAB. Timely and appropriate treatment should be
provided to preserve the patient's vision as much as possible and
manage the growth of intraocular tumors.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study are included
in the figures and/or tables of this article.
Authors' contributions
QS developed a clear treatment plan for patients
with SCLC. During the treatment WD collected detailed cases. MW
collated the patients' cases and pictures. PZ collected relevant
literature, wrote, translated and refined the manuscript. Finally,
all individuals checked the data and completed this article. PZ and
WD confirm the authenticity of all the raw data. All authors read
and approved the final manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
The patient's written consent has been obtained.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Huang J, Deng Y, Tin MS, Lok V, Ngai CH,
Zhang L, Lucero-Prisno DE III, Xu W, Zheng ZJ, Elcarte E, et al:
Distribution, risk factors, and temporal trends for lung cancer
incidence and mortality: A global analysis. Chest. 161:1101–1111.
2022.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Cozzi S, Bruni A, Ruggieri MP, Borghetti
P, Scotti V, Franceschini D, Fiore M, Taraborrelli M, Salvi F,
Galaverni M, et al: Thoracic radiotherapy in extensive disease
small cell lung cancer: Multicenter prospective observational
TRENDS study. Cancers (Basel). 15(434)2023.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Xie Q, Chu H, Yi J, Yu H, Gu T, Guan Y,
Liu X, Liang J, Li Y and Wang J: Identification of a prognostic
immune-related signature for small cell lung cancer. Cancer Med.
10:9115–9128. 2021.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Shamim S, Vidya S, Kabir S and Ghosh B:
Choroidal metastases as the initial presentation of lung cancer: A
rare scenario. Niger J Clin Pract. 20:905–909. 2017.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Sakellakis M, Peroukides S, Iconomou G and
Kalofonos H: Iris metastasis in a patient with small cell lung
cancer: A case report. Iran Red Crescent Med J.
18(e21522)2016.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Al Zreibi C, Gibault L, Fabre E and Le
Pimpec-Barthes F: Chirurgie du cancer pulmonaire à petites cellules
Surgery for small-cell lung cancer. Rev Mal Respir. 38:840–847.
2021.(In French).
|
|
7
|
Lally BE, Urbanic JJ, Blackstock AW,
Miller AA and Perry MC: Small cell lung cancer: Have we made any
progress over the last 25 years? Oncologist. 12:1096–1104.
2007.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Konala VM, Madhira BR, Ashraf S and
Graziano S: Use of immunotherapy in extensive-stage small cell lung
cancer. Oncology. 98:749–754. 2020.
|
|
9
|
Melosky B, Cheema PK, Brade A, McLeod D,
Liu G, Price PW, Jao K, Schellenberg DD, Juergens R, Leighl N and
Chu Q: Prolonging survival: The role of immune checkpoint
inhibitors in the treatment of extensive-stage small cell lung
cancer. Oncologist. 25:981–992. 2020.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Vicini G, Nicolosi C, Pieretti G and
Mazzini C: Large choroidal metastasis with exudative retinal
detachment as presenting manifestation of small cell lung cancer: A
case report. Respir Med Case Rep. 30(101074)2020.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Karunanithi S, Sharma P, Jain S, Mukherjee
A and Kumar R: Iris metastasis in a patient with small cell lung
cancer: Incidental detection with 18F-FDG PET/CT. Clin Nucl Med.
39:554–555. 2014.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Arepalli S, Kaliki S and Shields CL:
Choroidal metastases: Origin, features, and therapy. Indian J
Ophthalmol. 63:122–127. 2015.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Shome D, Honavar SG, Gupta P, Vemuganti GK
and Reddy PV: Metastasis to the eye and orbit from renal cell
carcinoma-a report of three cases and review of literature. Surv
Ophthalmol. 52:213–223. 2007.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Sitaula R, Shrestha GB, Paudel N and
Shrestha JK: Ocular and orbital metastases presenting as a first
sign of gastric adenocarcinoma. BMJ Case Rep.
2011(bcr1020114927)2011.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Singh A, Malik D, Singh S and Vyas VJ:
Choroidal metastasis in pancreatic adenocarcinoma. J Cancer Res
Ther. 18:263–265. 2022.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Cohen VM: Ocular metastases. Eye (Lond).
27:137–141. 2013.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Cennamo G, Montorio D, Carosielli M,
Romano MR and Cennamo G: Multimodal imaging in choroidal
metastasis. Ophthalmic Res. 64:411–416. 2021.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Funazo T, Morita K, Ikegami N, Konishi C,
Nakao S, Ariyasu R, Taki M, Nakagawa K, Hwang MH, Yoshimura C, et
al: Successful treatment with alectinib for choroidal metastasis in
anaplastic lymphoma kinase rearranged non-small cell lung cancer.
Intern Med. 56:2317–2320. 2017.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Ahmad SM and Esmaeli B: Metastatic tumors
of the orbit and ocular adnexa. Curr Opin Ophthalmol. 18:405–413.
2007.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Konstantinidis L and Damato B: Intraocular
metastases-a review. Asia Pac J Ophthalmol (Phila). 6:208–214.
2017.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Das SK, Sahoo TK, Parija S, Majumdar SKD
and Parida DK: Choroidal metastasis as initial presentation in
adenocarcinoma of lung: A case report. J Clin Diagn Res.
11:XD04–XD06. 2017.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Migaou A, Ben Saad A, Joobeur S, Ben
Abdeljelil N, Zina S, Cheikh Mhammed S, Rouatbi N and Fahem N:
Choroidal metastasis as the initial presentation of lung
adenocarcinoma: A case report. Respir Med Case Rep.
29(100992)2020.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Zhou Y, Sharifi A, Gupta P, Duong B,
Lahiji AP, He J and Lee WH: Vision loss as presenting symptom in
testicular cancer: A morbid case report. Case Rep Ophthalmol.
13:756–762. 2022.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Cun LP: MRI-based radiomics on prediction
of lymph-vascular space invasion in cervical cancer. Chin Med Sci
University, 2021.
|
|
25
|
Wu L, Yan J, Bai Y, Chen F, Zou X, Xu J,
Huang A, Hou L, Zhong Y, Jing Z, et al: An invasive zone in human
liver cancer identified by Stereo-seq promotes hepatocyte-tumor
cell crosstalk, local immunosuppression and tumor progression. Cell
Res. 33:585–603. 2023.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Zhou ZY, Wang Y, Long SY, et al: Research
progress on the pathogenesis of tumor-induced or infiltrative optic
neuropathy and traditional Chinese medicine etiology and
pathogenesis. China J Chinese Ophthalmol. 33:785–788. 2023.
|
|
27
|
Yang M, Wang W, Yan JH, Li XY, Zhou MW,
Huang WB and Zhang XL: Eye tumors misdiagnosed as glaucoma. Chin
Med J. 128:273–276. 2015.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Rishi P, Dhami A and Biswas J: Biopsy
techniques for intraocular tumors. Indian J Ophthalmol. 64:415–421.
2016.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Paul Chan RV and Young LH: Treatment
options for metastatic tumors to the choroid. Semin Ophthalmol.
20:207–216. 2009.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Thariat J, Boudin L, Loria O, Nguyen AM,
Kodjikian L and Mathis T: How to manage a patient with ocular
metastases? Biomedicines. 10(3044)2022.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Cho KR, Lee KM, Han G, Kang SW and Lee JI:
Gamma knife radiosurgery for cancer metastasized to the ocular
choroid. J Korean Neurosurg Soc. 61:60–65. 2018.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Chik JYK, Leung CWL and Wong KH:
Palliative radiation therapy for patients with orbital and ocular
metastases. Ann Palliat Med. 9:4458–4466. 2020.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Zhao L, Long L, Liang X, et al: Clinical
research progress of PD-L1 inhibitor envafolimab in the treatment
of advanced malignant tumor. Journal of Modern Oncology.
32:1154–1158. 2024.
|