|
1
|
Baron PL, Moore MP, Kinne DW, Candela FC,
Osborne MP and Petrek JA: Occult breast cancer presenting with
axillary metastases: Updated Management. Arch Surg. 125:210–214.
1990.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Sohn G, Son BH, Lee SJ, Kang EY, Jung SH,
Cho SH, Baek S, Lee YR, Kim HJ, Ko BS, et al: Treatment and
survival of patients with occult breast cancer with axillary lymph
node metastasis: A nationwide retrospective study. J Surg Oncol.
110:270–274. 2014.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Patel J, Nemoto T, Rosner D, Dao TL and
Pickren JW: Axillary lymph node metastasis from an occult breast
cancer. Cancer. 47:2923–2927. 1981.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Huang Y, Wu H and Luo Z: A retrospective
study of optimal surgical management for occult breast carcinoma:
Mastectomy or quadrantectomy? Medicine (Baltimore).
96(e9490)2017.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Yamaguchi H, Ishikawa M, Hatanaka K,
Uekusa T, Ishimaru M and Nagawa H: Occult breast cancer presenting
as axillary metastases. Breast. 15:259–262. 2006.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Abe S, Abe N, Noda M, Okano M, Tachibana
K, Yoshida S, Kiko Y, Hashimoto Y, Hatakeyama Y, Rokkaku Y and
Ohtake T: A Case of Occult Breast Cancer. Gan To Kagaku Ryoho.
44:1095–1097. 2017.PubMed/NCBI(In Japanese).
|
|
7
|
Walker GV, Smith GL, Perkins GH, Oh JL,
Woodward W, Yu TK, Hunt KK, Hoffman K, Strom EA and Buchholz TA:
Population-based analysis of occult primary breast cancer with
axillary lymph node metastasis. Cancer. 116:4000–4006.
2010.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Frattaroli FM, Carrara A, Conte AM and
Pappalardo G: Axillary metastasis as first symptom of occult breast
cancer: A case report. Tumori. 88:532–534. 2002.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Liu L, Zhang J, Chen M, Ren S, Liu H and
Zhang H: Anemia and thrombocytopenia as initial symptoms of occult
breast cancer with bone marrow metastasis: A case report. Medicine
(Baltimore). 96(e8529)2017.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Woo SM, Son BH, Lee JW, Kim HJ, Yu JH, Ko
BS, Sohn G, Lee YR, Kim H, Ahn SH and Baek SH: Survival outcomes of
different treatment methods for the ipsilateral breast of occult
breast cancer patients with axillary lymph node metastasis: A
single center experience. J Breast Cancer. 16:410–416.
2013.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Coleman C: Early detection and screening
for breast cancer. Semin Oncol Nurs. 33:141–155. 2017.PubMed/NCBI View Article : Google Scholar
|
|
12
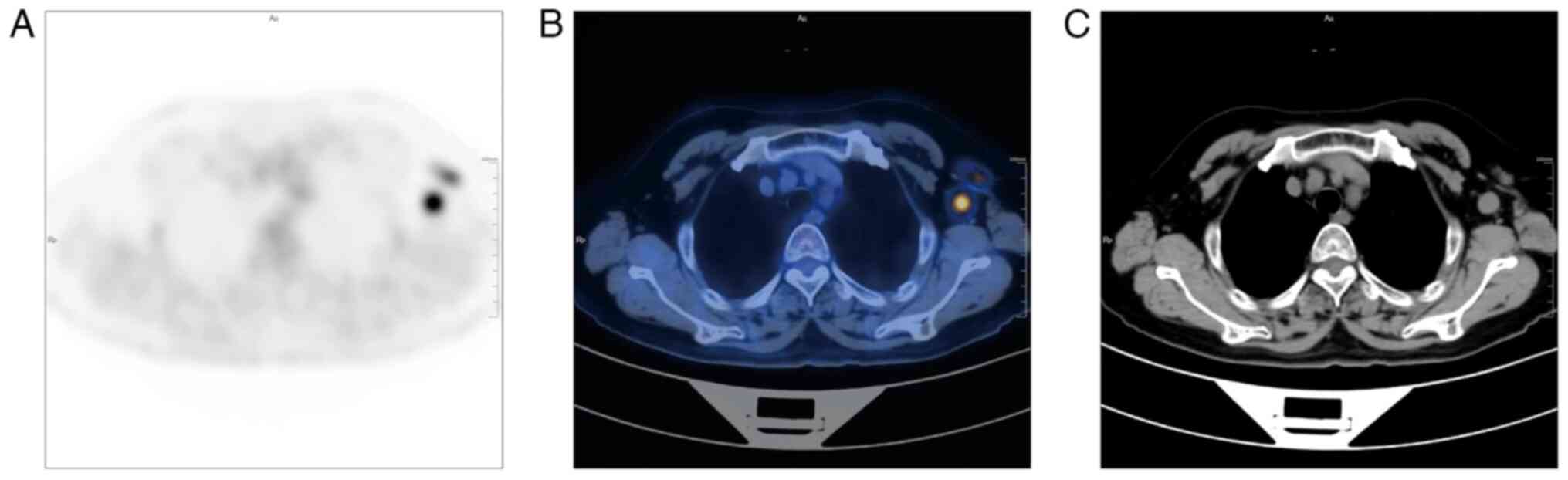
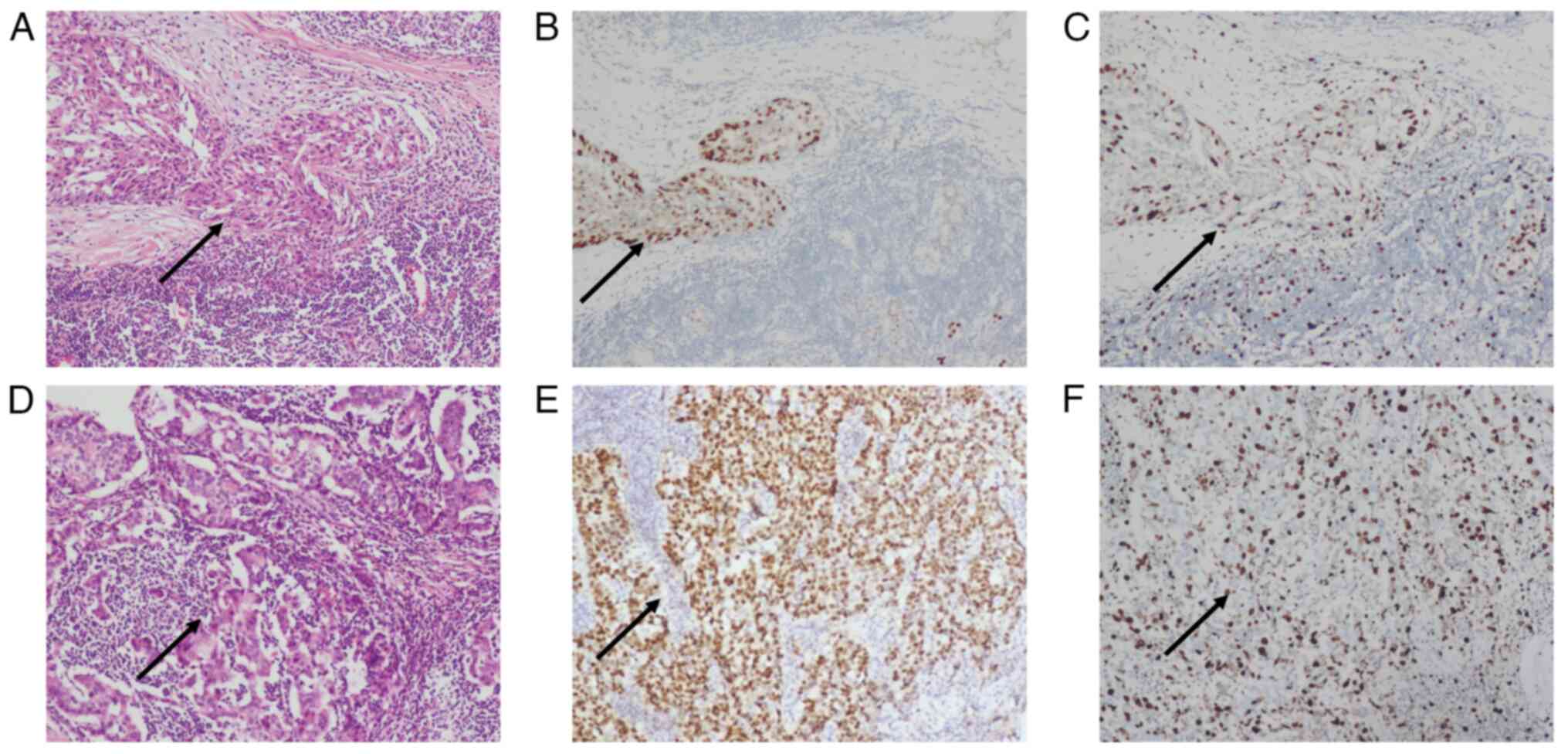
|
Anderson WF, Jatoi I and Devesa SS:
Assessing the impact of screening mammography: Breast cancer
incidence and mortality rates in Connecticut (1943-2002). Breast
Cancer Res Treat. 99:333–340. 2006.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Nguyen QD, Randall JW, Harmon TS, Robinson
AS, Cotes C, Lee AE, Mahon BH and Sadruddin S: Detection of a
mammographically occult breast cancer with a challenging clinical
history. Cureus. 10(e3594)2018.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Lee J and Nishikawa RM: Identifying women
with mammographically-occult breast cancer leveraging GAN-Simulated
Mammograms. IEEE Trans Med Imaging. 41:225–236. 2022.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Tartter PI, Weiss S, Ahmed S, Kamath S,
Hermann G and Drossman S: Mammographically occult breast cancers.
Breast J. 5:22–25. 1999.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Prasad SN and Houserkova D: The role of
various modalities in breast imaging. Biomed Pap Med Fac Univ
Palacky Olomouc Czech Repub. 151:209–218. 2007.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Planche K and Vinnicombe S: Breast imaging
in the new era. Cancer Imaging. 4:39–50. 2004.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Sánchez LR, Treviño LMT and Sánchez GE:
Fusion of Digital Mammography with High-Resolution Breast PET: An
Application to Breast Imaging. In: 2nd EAI International Conference
on Smart Technology. Torres-Guerrero F, Neira-Tovar L and
Bacca-Acosta J (eds). Springer International Publishing, Cham,
pp111-125, 2023.
|
|
19
|
Fiorica JV: Breast cancer screening,
mammography, and other modalities. Clin Obstet Gynecol. 59:688–709.
2016.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Rodriguez-Ruiz A, Lång K, Gubern-Merida A,
Broeders M, Gennaro G, Clauser P, Helbich TH, Chevalier M, Tan T,
Mertelmeier T, et al: Stand-Alone artificial intelligence for
breast cancer detection in mammography: Comparison with 101
radiologists. J Natl Cancer Inst. 111:916–922. 2019.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Groheux D, Espié M, Giacchetti S and
Hindié E: Performance of FDG PET/CT in the clinical management of
breast cancer. Radiology. 266:388–405. 2013.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Radan L, Ben-Haim S, Bar-Shalom R,
Guralnik L and Israel O: The role of FDG-PET/CT in suspected
recurrence of breast cancer. Cancer. 107:2545–2551. 2006.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Zangheri B, Messa C, Picchio M, Gianolli
L, Landoni C and Fazio F: PET/CT and breast cancer. Eur J Nucl Med
Mol Imaging. 31 (Suppl 1):S135–S142. 2004.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Gradishar WJ, Moran MS, Abraham J, Aft R,
Agnese D, Allison KH, Anderson B, Burstein HJ, Chew H, Dang C, et
al: Breast Cancer, Version 3.2022, NCCN Clinical Practice
Guidelines in Oncology. J Natl Compr Canc Netw. 20:691–722.
2022.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Zhao YF, Chen Z, Zhang Y, Zhou J, Chen JH,
Lee KE, Combs FJ, Parajuli R, Mehta RS, Wang M and Su MY: Diagnosis
of breast cancer using radiomics models built based on dynamic
contrast enhanced MRI combined with mammography. Front Oncol.
11(774248)2021.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Merson M, Andreola S, Galimberti V,
Bufalino R, Marchini S and Veronesi U: Breast carcinoma presenting
as axillary metastases without evidence of a primary tumor. Cancer.
70:504–508. 1992.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Varadarajan R, Edge SB, Yu J, Watroba N
and Janarthanan BR: Prognosis of occult breast carcinoma presenting
as isolated axillary nodal metastasis. Oncology. 71:456–459.
2006.PubMed/NCBI View Article : Google Scholar
|
|
28
|
He M, Tang LC, Yu KD, Cao AY, Shen ZZ,
Shao ZM and Di GH: Treatment outcomes and unfavorable prognostic
factors in patients with occult breast cancer. Eur J Surg Oncol.
38:1022–1028. 2012.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Khandelwal AK and Garguilo GA: Therapeutic
options for occult breast cancer: A survey of the American Society
of Breast Surgeons and review of the literature. Am J Surg.
190:609–613. 2005.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Halsted WS: I. The results of radical
operations for the cure of carcinoma of the breast. Ann Surg.
46:1–19. 1907.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Lloyd MS and Nash AG: ‘Occult’ breast
cancer. Ann R Coll Surg Engl. 83:420–424. 2001.PubMed/NCBI
|
|
32
|
Ofri A and Moore K: Occult breast cancer:
Where are we at? Breast. 54:211–215. 2020.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Wong YP, Tan GC, Muhammad R and Rajadurai
P: Occult primary breast carcinoma presented as an axillary mass: A
diagnostic challenge. Malays J Pathol. 42:151–155. 2020.PubMed/NCBI
|
|
34
|
Xu R, Li J, Zhang Y, Jing H and Zhu Y:
Male occult breast cancer with axillary lymph node metastasis as
the first manifestation: A case report and literature review.
Medicine (Baltimore). 96(e9312)2017.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Vlastos G, Jean ME, Mirza AN, Mirza NQ,
Kuerer HM, Ames FC, Hunt KK, Ross MI, Buchholz TA, Buzdar AU and
Singletary SE: Feasibility of breast preservation in the treatment
of occult primary carcinoma presenting with axillary metastases.
Ann Surg Oncol. 8:425–431. 2001.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Fayanju OM, Jeffe DB and Margenthaler JA:
Occult primary breast cancer at a comprehensive cancer center. J
Surg Res. 185:684–689. 2013.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Terada M, Adachi Y, Sawaki M, Hattori M,
Yoshimura A, Naomi G, Kotani H, Iwase M, Kataoka A, Onishi S, et
al: Occult breast cancer may originate from ectopic breast tissue
present in axillary lymph nodes. Breast Cancer Res Treat. 172:1–7.
2018.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Kadowaki M, Nagashima T, Sakata H,
Sakakibara M, Sangai T, Nakamura R, Fujimoto H, Arai M, Onai Y,
Nagai Y, et al: Ectopic breast tissue in axillary lymph node.
Breast Cancer. 14:425–428. 2007.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Edlow DW and Carter D: Heterotopic
epithelium in axillary lymph nodes: Report of a case and review of
the literature. Am J Clin Pathol. 59:666–673. 1973.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Turner DR and Millis RR: Breast tissue
inclusions in axillary lymph nodes. Histopathology. 4:631–636.
1980.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Maiorano E, Mazzarol GM, Pruneri G,
Mastropasqua MG, Zurrida S, Orvieto E and Viale G: Ectopic breast
tissue as a possible cause of false-positive axillary sentinel
lymph node biopsies. Am J Surg Pathol. 27:513–518. 2003.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Locopo N, Fanelli M and Gasparini G:
Clinical significance of angiogenic factors in breast cancer.
Breast Cancer Res Treat. 52:159–173. 1998.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Blanchard DK, Shetty PB, Hilsenbeck SG and
Elledge RM: Association of surgery with improved survival in stage
IV breast cancer patients. Ann Surg. 247:732–738. 2008.PubMed/NCBI View Article : Google Scholar
|
|
44
|
Olson JA Jr, Morris EA, Van Zee KJ,
Linehan DC and Borgen PI: Magnetic resonance imaging facilitates
breast conservation for occult breast cancer. Ann Surg Oncol.
7:411–415. 2000.PubMed/NCBI View Article : Google Scholar
|
|
45
|
Sanuki JI, Uchida Y, Uematsu T, Yamada Y
and Kasami M: Axillary mass suspected to be occult breast
carcinoma: A case study of skipped axillary lymph node metastasis
from endometrial carcinoma in which core-needle biopsy was useful
for diagnosis. Breast Cancer. 16:72–76. 2009.PubMed/NCBI View Article : Google Scholar
|
|
46
|
Hulka CA, Smith BL, Sgroi DC, Tan L,
Edmister WB, Semple JP, Campbell T, Kopans DB, Brady TJ and
Weisskoff RM: Benign and malignant breast lesions: Differentiation
with echo-planar MR imaging. Radiology. 197:33–38. 1995.PubMed/NCBI View Article : Google Scholar
|
|
47
|
Bhatia SK, Saclarides TJ, Witt TR, Bonomi
PD, Anderson KM and Economou SG: Hormone receptor studies in
axillary metastases from occult breast cancers. Cancer.
59:1170–1172. 1987.PubMed/NCBI View Article : Google Scholar
|
|
48
|
Poulakaki F: Occult Breast Cancer. In:
Breast Cancer Essentials. Rezai M, Kocdor MA and Canturk NZ (eds).
Springer International Publishing, Cham, pp667-674, 2021.
|
|
49
|
Van de Wouw AJ, Janssen-Heijnen ML,
Coebergh JW and Hillen HF: Epidemiology of unknown primary tumours;
incidence and population-based survival of 1285 patients in
Southeast Netherlands, 1984-1992. Eur J Cancer. 38:409–413.
2002.PubMed/NCBI View Article : Google Scholar
|
|
50
|
Randén M, Rutqvist LE and Johansson H:
Cancer patients without a known primary: Incidence and survival
trends in Sweden 1960-2007. Acta Oncol. 48:915–920. 2009.PubMed/NCBI View Article : Google Scholar
|
|
51
|
Hemminki K, Bevier M, Hemminki A and
Sundquist J: Survival in cancer of unknown primary site:
Population-based analysis by site and histology. Ann Oncol.
23:1854–1863. 2012.PubMed/NCBI View Article : Google Scholar
|
|
52
|
Pentheroudakis G, Lazaridis G and Pavlidis
N: Axillary nodal metastases from carcinoma of unknown primary
(CUPAx): A systematic review of published evidence. Breast Cancer
Res Treat. 119:1–11. 2010.PubMed/NCBI View Article : Google Scholar
|
|
53
|
Brewster DH, Lang J, Bhatti LA, Thomson CS
and Oien KA: Descriptive epidemiology of cancer of unknown primary
site in Scotland, 1961-2010. Cancer Epidemiol. 38:227–234.
2014.PubMed/NCBI View Article : Google Scholar
|
|
54
|
Binder C, Matthes KL, Korol D, Rohrmann S
and Moch H: Cancer of unknown primary-Epidemiological trends and
relevance of comprehensive genomic profiling. Cancer Med.
7:4814–4824. 2018.PubMed/NCBI View Article : Google Scholar
|
|
55
|
Krämer A, Hübner G, Schneeweiss A,
Folprecht G and Neben K: Carcinoma of unknown primary-an orphan
disease? Breast Care (Basel). 3:164–170. 2008.PubMed/NCBI View Article : Google Scholar
|
|
56
|
Barbieri E, Anghelone CAP, Gentile D, La
Raja C, Bottini A and Tinterri C: Metastases from occult breast
cancer: A case report of carcinoma of unknown primary Syndrome.
Case Rep Oncol. 13:1158–1163. 2020.PubMed/NCBI View Article : Google Scholar
|
|
57
|
Krämer A, Bochtler T, Pauli C, Baciarello
G, Delorme S, Hemminki K, Mileshkin L, Moch H, Oien K, Olivier T,
et al: Cancer of unknown primary: ESMO Clinical Practice Guideline
for diagnosis, treatment and follow-up. Ann Oncol. 34:228–246.
2023.PubMed/NCBI View Article : Google Scholar
|
|
58
|
Urban D, Rao A, Bressel M, Lawrence YR and
Mileshkin L: Cancer of unknown primary: A population-based analysis
of temporal change and socioeconomic disparities. Br J Cancer.
109:1318–1324. 2013.PubMed/NCBI View Article : Google Scholar
|
|
59
|
de Bresser J, de Vos B, van der Ent F and
Hulsewé K: Breast MRI in clinically and mammographically occult
breast cancer presenting with an axillary metastasis: A systematic
review. Eur J Surg Oncol. 36:114–119. 2010.PubMed/NCBI View Article : Google Scholar
|
|
60
|
Van Ooijen B, Bontenbal M, Henzen-Logmans
SC and Koper PC: Axillary nodal metastases from an occult primary
consistent with breast carcinoma. Br J Surg. 80:1299–1300.
1993.PubMed/NCBI View Article : Google Scholar
|
|
61
|
Hawes D, Neville AM and Cote RJ: Detection
of occult metastasis in patients with breast cancer. Semin Surg
Oncol. 20:312–318. 2001.PubMed/NCBI View Article : Google Scholar
|
|
62
|
Medina-Franco H and Urist MM: Occult
breast carcinoma presenting with axillary lymph node metastases.
Rev Invest Clin. 54:204–208. 2002.PubMed/NCBI
|
|
63
|
Owen HW, Dockerty MB and Gray HK: Occult
carcinoma of the breast. Surg Gynecol Obstet. 98:302–308.
1954.PubMed/NCBI
|
|
64
|
Chen YC, Chan CH, Lim YB, Yang SF, Yeh LT,
Wang YH, Chou MC and Yeh CB: Risk of breast cancer in women with
mastitis: A retrospective population-based cohort study. Medicina
(Kaunas). 56(372)2020.PubMed/NCBI View Article : Google Scholar
|
|
65
|
Ping J, Liu W, Chen Z and Li C: Lymph node
metastases in breast cancer: Mechanisms and molecular imaging. Clin
Imaging. 103(109985)2023.PubMed/NCBI View Article : Google Scholar
|
|
66
|
He M, Liu H and Jiang Y: A case report of
male occult breast cancer first manifesting as axillary lymph node
metastasis with part of metastatic mucinous carcinoma. Medicine
(Baltimore). 94(e1038)2015.PubMed/NCBI View Article : Google Scholar
|
|
67
|
Rosen PP and Kimmel M: Occult breast
carcinoma presenting with axillary lymph node metastases: A
follow-up study of 48 patients. Hum Pathol. 21:518–523.
1990.PubMed/NCBI View Article : Google Scholar
|
|
68
|
Hur SM, Cho DH, Lee SK, Choi MY, Bae SY,
Koo MY, Kim S, Nam SJ, Lee JE and Yang JH: Occult breast cancers
manifesting as axillary lymph node metastasis in men: A two-case
report. J Breast Cancer. 15:359–363. 2012.PubMed/NCBI View Article : Google Scholar
|
|
69
|
Matsuoka K, Ohsumi S, Takashima S, Saeki
T, Aogi K and Mandai K: Occult breast carcinoma presenting with
axillary lymph node metastases: Follow-up of eleven patients.
Breast Cancer. 10:330–334. 2003.PubMed/NCBI View Article : Google Scholar
|
|
70
|
Zheng H, Gu Y, Qin Y, Huang X, Yang J and
Yang GZ: Small Lesion Classification in Dynamic Contrast
Enhancement MRI for Breast Cancer Early Detection. In: Medical
Image Computing and Computer Assisted Intervention-MICCAI 2018. Vol
11071. Frangi AF, Schnabel JA, Davatzikos C, Alberola-López C and
Fichtinger G (eds). Springer International Publishing, Cham,
pp876-884, 2018.
|
|
71
|
Lei YM, Yin M, Yu MH, Yu J, Zeng SE, Lv
WZ, Li J, Ye HR, Cui XW and Dietrich CF: Artificial intelligence in
medical imaging of the breast. Front Oncol.
11(600557)2021.PubMed/NCBI View Article : Google Scholar
|
|
72
|
Uchida K, Yamashita A, Kawase K and Kamiya
K: Screening ultrasonography revealed 15% of mammographically
occult breast cancers. Breast Cancer. 15:165–168. 2008.PubMed/NCBI View Article : Google Scholar
|
|
73
|
Jacob D, Brombart JC, Muller C, Lefèbvre
C, Massa F and Depoerck A: Analysis of the results of 137
subclinical breast lesions excisions. Value of ultrasonography in
the early diagnosis of breast cancer. J Gynecol Obstet Biol Reprod
(Paris). 26:27–31. 1997.PubMed/NCBI(In French).
|
|
74
|
Asbeutah AM, AlMajran AA, Brindhaban A and
Asbeutah SA: Comparison of radiation doses between diagnostic
full-field digital mammography (FFDM) and digital breast
tomosynthesis (DBT): A clinical study. J Med Radiat Sci.
67:185–192. 2020.PubMed/NCBI View Article : Google Scholar
|
|
75
|
Gøtzsche PC and Jørgensen KJ: Screening
for breast cancer with mammography. Cochrane Database Syst Rev.
2013(CD001877)2013.PubMed/NCBI View Article : Google Scholar
|
|
76
|
Rodríguez-Ruiz A, Krupinski E, Mordang JJ,
Schilling K, Heywang-Köbrunner SH, Sechopoulos I and Mann RM:
Detection of breast cancer with mammography: Effect of an
artificial intelligence support system. Radiology. 290:305–314.
2019.PubMed/NCBI View Article : Google Scholar
|
|
77
|
McDonald ES, Hammersley JA, Chou SH,
Rahbar H, Scheel JR, Lee CI, Liu CL, Lehman CD and Partridge SC:
Performance of DWI as a Rapid unenhanced technique for detecting
mammographically occult breast cancer in elevated-risk women with
dense breasts. AJR Am J Roentgenol. 207:205–216. 2016.PubMed/NCBI View Article : Google Scholar
|
|
78
|
Theunissen CI, Rust EA, Edens MA, Bandel
C, Van't Ooster-van den Berg JG, Jager PL, Noorda EM and Francken
AB: Radioactive seed localization is the preferred technique in
nonpalpable breast cancer compared with wire-guided localization
and radioguided occult lesion localization. Nucl Med Commun.
38:396–401. 2017.PubMed/NCBI View Article : Google Scholar
|
|
79
|
Morris EA, Liberman L, Ballon DJ, Robson
M, Abramson AF, Heerdt A and Dershaw DD: MRI of Occult Breast
Carcinoma in a High-Risk Population. AJR Am J Roentgenol.
181:619–626. 2003.PubMed/NCBI View Article : Google Scholar
|
|
80
|
Buchanan CL, Morris EA, Dorn PL, Borgen PI
and Van Zee KJ: Utility of breast magnetic resonance imaging in
patients with occult primary breast cancer. Ann Surg Oncol.
12:1045–1053. 2005.PubMed/NCBI View Article : Google Scholar
|
|
81
|
Wecsler JS, Raghavendra A, Mack WJ,
Tripathy D, Yamashita M, Sheth P, Hovanessian-Larsen L, Sener SF,
Russell CA, McDonald H and Lang JE: Abstract P4-02-05: Predictors
of MRI detection of occult lesions in newly diagnosed breast
cancer. Cancer Res. 76 (Suppl 4)(P4-02-05)2016.
|
|
82
|
Zheng B, Hollingsworth AB, Tan MY, Stough
RG and Liu H: Abstract P4-02-06: Improving efficacy of applying
breast MRI to detect mammography-occult breast cancer. Cancer Res.
76 (Suppl 4)(P4-02-06)2016.
|
|
83
|
Amornsiripanitch N, Rahbar H, Kitsch AE,
Lam DL, Weitzel B and Partridge SC: Visibility of mammographically
occult breast cancer on diffusion-weighted MRI versus ultrasound.
Clin Imaging. 49:37–43. 2018.PubMed/NCBI View Article : Google Scholar
|
|
84
|
Gao Y, Bagadiya NR, Jardon ML, Heller SL,
Melsaether AN, Toth HB and Moy L: Outcomes of Preoperative
MRI-Guided needle localization of nonpalpable mammographically
occult breast lesions. AJR Am J Roentgenol. 207:676–684.
2016.PubMed/NCBI View Article : Google Scholar
|
|
85
|
Smith LF, Henry-Tillman R, Mancino AT,
Johnson A, Price Jones M, Westbrook KC, Harms S and Klimberg VS:
Magnetic resonance imaging-guided core needle biopsy and needle
localized excision of occult breast lesions. Am J Surg.
182:414–418. 2001.PubMed/NCBI View Article : Google Scholar
|
|
86
|
Ryu JK, Rhee SJ, Song JY, Cho SH and Jahng
GH: Characteristics of quantitative perfusion parameters on dynamic
contrast-enhanced MRI in mammographically occult breast cancer. J
Appl Clin Med Phys. 17:377–390. 2016.PubMed/NCBI View Article : Google Scholar
|
|
87
|
McCartan DP, Zabor EC, Morrow M, Van Zee
KJ and El-Tamer MB: Oncologic outcomes after treatment for MRI
occult breast cancer (pT0N+). Ann Surg Oncol. 24:3141–3147.
2017.PubMed/NCBI View Article : Google Scholar
|
|
88
|
Ramírez Huaranga MA, Salas Manzanedo V,
Huertas MP, Torres Sousa Y and Ramos Rodríguez CC: Lumbar pain as
the single manifestation of an occult breast cancer. Usefulness of
positron emission tomography. Reumatol Clin. 11:118–120.
2015.PubMed/NCBI View Article : Google Scholar
|
|
89
|
Takabatake D, Taira N, Aogi K, Ohsumi S,
Takashima S, Inoue T and Nishimura R: Two cases of occult breast
cancer in which PET-CT was helpful in identifying primary tumors.
Breast Cancer. 15:181–184. 2008.PubMed/NCBI View Article : Google Scholar
|
|
90
|
Brem RF, Ruda RC, Yang JL, Coffey CM and
Rapelyea JA: Breast-Specific γ-Imaging for the detection of
mammographically occult breast cancer in women at increased risk. J
Nucl Med. 57:678–684. 2016.PubMed/NCBI View Article : Google Scholar
|
|
91
|
Brem RF, Shahan C, Rapleyea JA, Donnelly
CA, Rechtman LR, Kidwell AB, Teal CB, McSwain A and Torrente J:
Detection of occult foci of breast cancer using breast-specific
gamma imaging in women with one mammographic or clinically
suspicious breast lesion. Acad Radiol. 17:735–743. 2010.PubMed/NCBI View Article : Google Scholar
|
|
92
|
Zand S and Abdolali A: Radioguided Occult
Lesion Localisation (ROLL) for Excision of Non-Palpable Breast
Lesions, a Personal Experience in a Patient with Multifocal Breast
Cancer. Arch Breast Cancer. 3:139–143. 2016.
|
|
93
|
Ong JSL, The J, Saunders C, Bourke AG,
Lizama C, Newton J, Phillips M and Taylor DB: Patient satisfaction
with Radioguided Occult Lesion Localisation using iodine-125 seeds
(‘ROLLIS’) versus conventional hookwire localisation. Eur J Surg
Oncol. 43:2261–2269. 2017.PubMed/NCBI View Article : Google Scholar
|
|
94
|
Li H, Liu Z, Yuan L, Fan K, Zhang Y, Cai W
and Lan X: Radionuclide-Based imaging of breast cancer: State of
the art. Cancers (Basel). 13(5459)2021.PubMed/NCBI View Article : Google Scholar
|
|
95
|
Altıparmak Güleç B and Yurt F: Treatment
with radiopharmaceuticals and radionuclides in breast cancer:
Current options. Eur J Breast Health. 17:214–219. 2021.PubMed/NCBI View Article : Google Scholar
|
|
96
|
Tolmachev V and Vorobyeva A: Radionuclides
in diagnostics and therapy of malignant tumors: New development.
Cancers (Basel). 14(297)2022.PubMed/NCBI View Article : Google Scholar
|
|
97
|
Amir E, Bedard PL, Ocaña A and Seruga B:
Benefits and harms of detecting clinically occult breast cancer. J
Natl Cancer Inst. 104:1542–1547. 2012.PubMed/NCBI View Article : Google Scholar
|
|
98
|
Health Commission Of The People's Republic
Of China N. National guidelines for diagnosis and treatment of
breast cancer 2022 in China (English version). Chin J Cancer Res.
34:151–175. 2022.PubMed/NCBI View Article : Google Scholar
|
|
99
|
Zhang S, Yu YH, Qu W, Zhang Y and Li J:
Diagnosis and treatment of accessory breast cancer in 11 patients.
Oncol Lett. 10:1783–1788. 2015.PubMed/NCBI View Article : Google Scholar
|
|
100
|
Pesapane F, Downey K, Rotili A, Cassano E
and Koh DM: Imaging diagnosis of metastatic breast cancer. Insights
Imaging. 11(79)2020.PubMed/NCBI View Article : Google Scholar
|
|
101
|
Feuerman L, Attie JN and Rosenberg B:
Carcinoma in axillary lymph nodes as an indicator of breast cancer.
Surg Gynecol Obstet. 114:5–8. 1962.PubMed/NCBI
|
|
102
|
Larsen RR, Sawyer KC, Sawyer RB and Torres
RC: Occult carcinoma of the breast. Am J Surg. 107:553–555.
1964.PubMed/NCBI View Article : Google Scholar
|
|
103
|
Osteen RT, Kopf G and Wilson RE: In
pursuit of the unknown primary. Am J Surg. 135:494–497.
1978.PubMed/NCBI View Article : Google Scholar
|
|
104
|
Chen QX, Wang XX, Lin PY, Zhang J, Li JJ,
Song CG and Shao ZM: The different outcomes between
breast-conserving surgery and mastectomy in triple-negative breast
cancer: A population-based study from the SEER 18 database.
Oncotarget. 8:4773–4780. 2017.PubMed/NCBI View Article : Google Scholar
|
|
105
|
Masinghe SP, Faluyi OO, Kerr GR and
Kunkler IH: Breast radiotherapy for occult breast cancer with
axillary nodal metastases-does it reduce the local recurrence rate
and increase overall survival? Clin Oncol (R Coll Radiol).
23:95–100. 2011.PubMed/NCBI View Article : Google Scholar
|
|
106
|
Macedo FI, Eid JJ, Flynn J, Jacobs MJ and
Mittal VK: Optimal surgical management for occult breast carcinoma:
A meta-analysis. Ann Surg Oncol. 23:1838–1844. 2016.PubMed/NCBI View Article : Google Scholar
|
|
107
|
Foroudi F and Tiver KW: Occult breast
carcinoma presenting as axillary metastases. Int J Radiat Oncol
Biol Phys. 47:143–147. 2000.PubMed/NCBI View Article : Google Scholar
|
|
108
|
Shannon C, Walsh G, Sapunar F, A'Hern R
and Smith I: Occult primary breast carcinoma presenting as axillary
lymphadenopathy. Breast. 11:414–418. 2002.PubMed/NCBI View Article : Google Scholar
|
|
109
|
Buisman FE, van Gelder L, Menke-Pluijmers
MB, Bisschops BH, Plaisier PW and Westenend PJ: Non-primary breast
malignancies: A single institution's experience of a diagnostic
challenge with important therapeutic consequences-a retrospective
study. World J Surg Oncol. 14(166)2016.PubMed/NCBI View Article : Google Scholar
|
|
110
|
Kemeny MM: Mastectomy: Is it necessary for
occult breast cancer? N Y State J Med. 92:516–517. 1992.PubMed/NCBI
|
|
111
|
Copeland EM and Mcbride CM: Axillary
metastases from unknown primary sites. Ann Surg. 178:21–27.
1973.PubMed/NCBI View Article : Google Scholar
|
|
112
|
Kim BH, Kwon J and Kim K: Evaluation of
the benefit of radiotherapy in patients with occult breast cancer:
A population-based analysis of the SEER database. Cancer Res Treat.
50:551–561. 2018.PubMed/NCBI View Article : Google Scholar
|
|
113
|
Rubovszky G, Kocsis J, Boér K,
Chilingirova N, Dank M, Kahán Z, Kaidarova D, Kövér E, Krakovská
BV, Máhr K, et al: Systemic treatment of breast cancer. 1st
Central-Eastern European professional consensus statement on breast
cancer. Pathol Oncol Res. 28(1610383)2022.PubMed/NCBI View Article : Google Scholar
|
|
114
|
Song MW, Ki SY, Lim HS, Lee HJ, Lee JS and
Yoon JH: Axillary metastasis from occult breast cancer and
synchronous contralateral breast cancer initially suspected to be
cancer with contralateral axillary metastasis: A case report. BMC
Womens Health. 21(418)2021.PubMed/NCBI View Article : Google Scholar
|
|
115
|
Wu SG, Zhang WW, Sun JY, Li FY, Lin HX,
Chen YX and He ZY: Comparable survival between additional
radiotherapy and local surgery in occult breast cancer after
axillary lymph node dissection: A population-based analysis. J
Cancer. 8:3849–3855. 2017.PubMed/NCBI View Article : Google Scholar
|
|
116
|
Neal L, Sookhan N and Reynolds C: Occult
breast carcinoma presenting as gastrointestinal metastases. Case
Rep Med. 2009(564756)2009.PubMed/NCBI View Article : Google Scholar
|
|
117
|
Ciulla A, Castronovo G, Tomasello G,
Maiorana AM, Russo L, Daniele E and Genova G: Gastric metastases
originating from occult breast lobular carcinoma: Diagnostic and
therapeutic problems. World J Surg Oncol. 6(78)2008.PubMed/NCBI View Article : Google Scholar
|
|
118
|
Khan I, Malik R, Khan A, Assad S, Zahid M,
Sohail MS, Yasin F and Qavi AH: Breast cancer metastases to the
gastrointestinal tract presenting with Anemia and intra-abdominal
bleed. Cureus. 9(e1429)2017.PubMed/NCBI View Article : Google Scholar
|
|
119
|
Rodrigues MV, Tercioti-Junior V, Lopes LR,
Coelho-Neto Jde S and Andreollo NA: Breast cancer metastasis in the
stomach: When the gastrectomy is indicated? Arq Bras Cir Dig.
29:86–89. 2016.PubMed/NCBI View Article : Google Scholar : (In English,
Portuguese).
|
|
120
|
Yang H, Li L, Zhang M, Zhang S, Xu S and
Ma X: Application of neoadjuvant chemotherapy in occult breast
cancer: Five case reports. Medicine (Baltimore).
96(e8200)2017.PubMed/NCBI View Article : Google Scholar
|
|
121
|
Asaoka M, Gandhi S, Ishikawa T and Takabe
K: Neoadjuvant chemotherapy for breast cancer: Past, present, and
future. Breast Cancer (Auckl). 14(1178223420980377)2020.PubMed/NCBI View Article : Google Scholar
|
|
122
|
Hessler LK, Molitoris JK, Rosenblatt PY,
Bellavance EC, Nichols EM, Tkaczuk KHR, Feigenberg SJ, Bentzen SM
and Kesmodel SB: Factors influencing management and outcome in
patients with occult breast cancer with axillary lymph node
involvement: Analysis of the National cancer database. Ann Surg
Oncol. 24:2907–2914. 2017.PubMed/NCBI View Article : Google Scholar
|
|
123
|
Gosset M, Hamy AS, Mallon P, Delomenie M,
Mouttet D, Pierga JY, Lae M, Fourquet A, Rouzier R, Reyal F and
Feron JG: Prognostic impact of time to ipsilateral breast tumor
recurrence after breast conserving surgery. PLoS One.
11(e0159888)2016.PubMed/NCBI View Article : Google Scholar
|
|
124
|
Liu YM, Ge JY, Chen YF, Liu T, Chen L, Liu
CC, Ma D, Chen YY, Cai YW, Xu YY, et al: Combined single-cell and
spatial transcriptomics reveal the metabolic evolvement of breast
cancer during early dissemination. Adv Sci (Weinh).
10(2205395)2023.PubMed/NCBI View Article : Google Scholar
|
|
125
|
Chagpar AB, Cicek AF and Harigopal M: Can
tumor biology predict occult multifocal disease in breast cancer
patients? Am Surg. 83:704–708. 2017.PubMed/NCBI
|
|
126
|
Merkkola-von Schantz PA, Jahkola TA,
Krogerus LA and Kauhanen SMC: Reduction mammaplasty in patients
with history of breast cancer: The incidence of occult cancer and
high-risk lesions. Breast. 35:157–161. 2017.PubMed/NCBI View Article : Google Scholar
|
|
127
|
Risk-reducing Salpingo-Oophorectomy in
Women at Higher Risk of Ovarian and Breast Cancer: A Single
Institution Prospective Series. AR 37, 2017.
|
|
128
|
Abe H, Naitoh H, Umeda T, Shiomi H, Tani
T, Kodama M and Okabe H: Occult breast cancer presenting axillary
nodal metastasis: A case report. Jpn J Clin Oncol. 30:185–187.
2000.PubMed/NCBI View Article : Google Scholar
|
|
129
|
Montagna E, Bagnardi V, Rotmensz N, Viale
G, Cancello G, Mazza M, Cardillo A, Ghisini R, Galimberti V,
Veronesi P, et al: Immunohistochemically defined subtypes and
outcome in occult breast carcinoma with axillary presentation.
Breast Cancer Res Treat. 129:867–875. 2011.PubMed/NCBI View Article : Google Scholar
|
|
130
|
Aydoğan F, Taşçı Y and Sagara Y: Phyllodes
Tumors of the Breast. In: Breast Disease. Aydiner A, İgci A and
Soran A (eds). Springer International Publishing, Cham, pp421-427,
2016.
|
|
131
|
Li L, Zhang D, Wen T, Wu Y, Lv D, Zhai J
and Ma F: Axillary lymph node dissection plus radiotherapy may be
an optimal strategy for patients with occult breast cancer. J
National Cancer Center. 2:198–204. 2022.PubMed/NCBI View Article : Google Scholar
|
|
132
|
Schwab FD, Burger H, Isenschmid M, Kuhn A,
Mueller MD and Günthert AR: Suspicious axillary lymph nodes in
patients with unremarkable imaging of the breast. Eur J Obstet
Gynecol Reprod Biol. 150:88–91. 2010.PubMed/NCBI View Article : Google Scholar
|
|
133
|
Shetty MK and Carpenter WS: Sonographic
evaluation of isolated abnormal axillary lymph nodes identified on
mammograms. J Ultrasound Med. 23:63–71. 2004.PubMed/NCBI View Article : Google Scholar
|
|
134
|
Christiansen P, Carstensen SL, Ejlertsen
B, Kroman N, Offersen B, Bodilsen A and Jensen MB: Breast
conserving surgery versus mastectomy: Overall and relative
survival-a population based study by the Danish Breast Cancer
Cooperative Group (DBCG). Acta Oncol. 57:19–25. 2018.PubMed/NCBI View Article : Google Scholar
|
|
135
|
de Boniface J, Szulkin R and Johansson
ALV: Survival after breast conservation vs mastectomy adjusted for
comorbidity and socioeconomic status: A Swedish National 6-year
follow-up of 48 986 women. JAMA Surg. 156:628–637. 2021.PubMed/NCBI View Article : Google Scholar
|
|
136
|
Keelan S, Flanagan M and Hill ADK:
Evolving trends in surgical management of breast cancer: An
analysis of 30 years of practice changing papers. Front Oncol.
11(622621)2021.PubMed/NCBI View Article : Google Scholar
|
|
137
|
Saha A, Mukhopadhyay M, Das C, Sarkar K,
Saha AK and Sarkar DK: FNAC Versus core needle biopsy: A
comparative study in evaluation of palpable breast lump. J Clin
Diagn Res. 10:EC05–EC08. 2016.PubMed/NCBI View Article : Google Scholar
|
|
138
|
Lieske B, Ravichandran D and Wright D:
Role of fine-needle aspiration cytology and core biopsy in the
preoperative diagnosis of screen-detected breast carcinoma. Br J
Cancer. 95:62–66. 2006.PubMed/NCBI View Article : Google Scholar
|
|
139
|
Willems SM, Van Deurzen CHM and Van Diest
PJ: Diagnosis of breast lesions: Fine-needle aspiration cytology or
core needle biopsy? A review. J Clin Pathol. 65:287–292.
2012.PubMed/NCBI View Article : Google Scholar
|
|
140
|
Calhoun BC and Collins LC: Predictive
markers in breast cancer: An update on ER and HER2 testing and
reporting. Semin Diagn Pathol. 32:362–369. 2015.PubMed/NCBI View Article : Google Scholar
|
|
141
|
Onitilo AA, Engel JM, Greenlee RT and
Mukesh BN: Breast cancer subtypes based on ER/PR and Her2
expression: Comparison of clinicopathologic features and survival.
Clin Med Res. 7:4–13. 2009.PubMed/NCBI View Article : Google Scholar
|
|
142
|
Wang R, Yang HX, Chen J, Huang JJ and Lv
Q: Best treatment options for occult breast cancer: A
meta-analysis. Front Oncol. 13(1051232)2023.PubMed/NCBI View Article : Google Scholar
|
|
143
|
Tsai C, Zhao B, Chan T and Blair SL:
Treatment for occult breast cancer: A propensity score analysis of
the National Cancer Database. Am J Surg. 220:153–160.
2020.PubMed/NCBI View Article : Google Scholar
|
|
144
|
Mariscotti G, Houssami N, Durando M,
Bergamasco L, Campanino PP, Ruggieri C, Regini E, Luparia A,
Bussone R, Sapino A, et al: Accuracy of mammography, digital breast
tomosynthesis, ultrasound and MR imaging in preoperative assessment
of breast cancer. Anticancer Res. 34:1219–1225. 2014.PubMed/NCBI
|
|
145
|
Kim WH, Chang JM, Moon HG, Yi A, Koo HR,
Gweon HM and Moon WK: Comparison of the diagnostic performance of
digital breast tomosynthesis and magnetic resonance imaging added
to digital mammography in women with known breast cancers. Eur
Radiol. 26:1556–1564. 2016.PubMed/NCBI View Article : Google Scholar
|
|
146
|
An YY, Kim SH and Kang BJ: Characteristic
features and usefulness of MRI in breast cancer in patients under
40 years old: Correlations with conventional imaging and prognostic
factors. Breast Cancer. 21:302–315. 2014.PubMed/NCBI View Article : Google Scholar
|
|
147
|
Van Goethem M, Tjalma W, Schelfout K,
Verslegers I, Biltjes I and Parizel P: Magnetic resonance imaging
in breast cancer. Eur J Surg Oncol. 32:901–910. 2006.PubMed/NCBI View Article : Google Scholar
|
|
148
|
Zeeshan M, Salam B, Khalid QSB, Alam S and
Sayani R: Diagnostic accuracy of digital mammography in the
detection of breast cancer. Cureus. 10(e2448)2018.PubMed/NCBI View Article : Google Scholar
|
|
149
|
Li H, Mendel KR, Lan L, Sheth D and Giger
ML: Digital mammography in breast cancer: Additive value of
radiomics of breast parenchyma. Radiology. 291:15–20.
2019.PubMed/NCBI View Article : Google Scholar
|
|
150
|
Seeram E: Full-Field Digital Mammography.
In: Digital Radiography. Springer Singapore, Singapore, pp111-123,
2019.
|
|
151
|
Jadvar H and Colletti PM: Competitive
advantage of PET/MRI. Eur J Radiol. 83:84–94. 2014.PubMed/NCBI View Article : Google Scholar
|
|
152
|
Koolen BB, Vidal-Sicart S, Benlloch
Baviera JM and Valdés Olmos RA: Evaluating heterogeneity of primary
tumor (18)F-FDG uptake in breast cancer with a dedicated breast PET
(MAMMI): A feasibility study based on correlation with PET/CT. Nucl
Med Commun. 35:446–452. 2014.PubMed/NCBI View Article : Google Scholar
|
|
153
|
Singh BK, Verma K and Thoke AS: Fuzzy
cluster based neural network classifier for classifying breast
tumors in ultrasound images. Exp Sys Appl. 66:114–123. 2016.
|
|
154
|
Gómez-Flores W and Ruiz-Ortega BA: New
fully automated method for segmentation of breast lesions on
ultrasound based on texture analysis. Ultrasound Med Biol.
42:1637–1650. 2016.PubMed/NCBI View Article : Google Scholar
|
|
155
|
Kozegar E, Soryani M, Behnam H, Salamati M
and Tan T: Breast cancer detection in automated 3D breast
ultrasound using iso-contours and cascaded RUSBoosts. Ultrasonics.
79:68–80. 2017.PubMed/NCBI View Article : Google Scholar
|
|
156
|
Mohammed MA, Al-Khateeb B, Rashid AN,
Ibrahim DA, Abd Ghani MK and Mostafa SA: Neural network and
multi-fractal dimension features for breast cancer classification
from ultrasound images. Comp Elect Eng. 70:871–882. 2018.
|
|
157
|
Moon WK, Chen IL, Yi A, Bae MS, Shin SU
and Chang RF: Computer-aided prediction model for axillary lymph
node metastasis in breast cancer using tumor morphological and
textural features on ultrasound. Comput Methods Programs Biomed.
162:129–137. 2018.PubMed/NCBI View Article : Google Scholar
|
|
158
|
Kim SA, Chang JM, Cho N, Yi A and Moon WK:
Characterization of breast lesions: Comparison of digital breast
tomosynthesis and ultrasonography. Korean J Radiol. 16:229–238.
2015.PubMed/NCBI View Article : Google Scholar
|
|
159
|
Cai SQ, Yan JX, Chen QS, Huang ML and Cai
DL: Significance and application of digital breast tomosynthesis
for the BI-RADS classification of breast cancer. Asian Pac J Cancer
Prev. 16:4109–4114. 2015.PubMed/NCBI View Article : Google Scholar
|
|
160
|
Nakashima K, Uematsu T, Itoh T, Takahashi
K, Nishimura S, Hayashi T and Sugino T: Comparison of visibility of
circumscribed masses on Digital Breast Tomosynthesis (DBT) and 2D
mammography: Are circumscribed masses better visualized and assured
of being benign on DBT? Eur Radiol. 27:570–577. 2017.PubMed/NCBI View Article : Google Scholar
|
|
161
|
Mercier J, Kwiatkowski F, Abrial C,
Boussion V, Dieu-de Fraissinette V, Marraoui W, Petitcolin-Bidet V
and Lemery S: The role of tomosynthesis in breast cancer staging in
75 patients. Diagn Interv Imaging. 96:27–35. 2015.PubMed/NCBI View Article : Google Scholar
|
|
162
|
Roganovic D, Djilas D, Vujnovic S, Pavic D
and Stojanov D: Breast MRI, digital mammography and breast
tomosynthesis: Comparison of three methods for early detection of
breast cancer. Bosn J Basic Med Sci. 15:64–68. 2015.PubMed/NCBI View Article : Google Scholar
|
|
163
|
Das BK, Biswal BM and Bhavaraju M: Role of
scintimammography in the diagnosis of breast cancer. Malays J Med
Sci. 13:52–57. 2006.PubMed/NCBI
|
|
164
|
Simanek M and Koranda P: SPECT/CT imaging
in breast cancer-current status and challenges. Biomed Pap Med Fac
Univ Palacky Olomouc Czech Repub. 160:474–483. 2016.PubMed/NCBI View Article : Google Scholar
|
|
165
|
Berrington de González A, Mahesh M, Kim
KP, Bhargavan M, Lewis R, Mettler F and Land C: Projected cancer
risks from computed tomographic scans performed in the United
States in 2007. Arch Intern Med. 169:2071–2077. 2009.PubMed/NCBI View Article : Google Scholar
|
|
166
|
Brem RF, Floerke AC, Rapelyea JA, Teal C,
Kelly T and Mathur V: Breast-specific gamma imaging as an adjunct
imaging modality for the diagnosis of breast cancer. Radiology.
247:651–657. 2008.PubMed/NCBI View Article : Google Scholar
|
|
167
|
Yoon HJ, Kim Y, Chang KT and Kim BS:
Prognostic value of semi-quantitative tumor uptake on Tc-99m
sestamibi breast-specific gamma imaging in invasive ductal breast
cancer. Ann Nucl Med. 29:553–560. 2015.PubMed/NCBI View Article : Google Scholar
|
|
168
|
Tan H, Zhang H, Yang W, Fu Y, Gu Y, Du M,
Cheng D and Shi H: Breast-specific gamma imaging with
Tc-99m-sestamibi in the diagnosis of breast cancer and its
semiquantitative index correlation with tumor biologic markers,
subtypes, and clinicopathologic characteristics. Nucl Med Commun.
37:792–799. 2016.PubMed/NCBI View Article : Google Scholar
|
|
169
|
Yu X, Hu G, Zhang Z, Qiu F, Shao X, Wang
X, Zhan H, Chen Y, Deng Y and Huang J: Retrospective and
comparative analysis of (99m)Tc-Sestamibi breast specific gamma
imaging versus mammography, ultrasound, and magnetic resonance
imaging for the detection of breast cancer in Chinese women. BMC
Cancer. 16(450)2016.PubMed/NCBI View Article : Google Scholar
|
|
170
|
Cho MJ, Yang JH, Yu YB, Park KS, Chung HW,
So Y, Choi N and Kim MY: Validity of breast-specific gamma imaging
for Breast Imaging Reporting and Data System 4 lesions on
mammography and/or ultrasound. Ann Surg Treat Res. 90:194–200.
2016.PubMed/NCBI View Article : Google Scholar
|