|
1
|
Killerby ME, Biggs HM, Midgley CM, Gerber
SI and Watson JT: Middle east respiratory syndrome coronavirus
transmission. Emerg Infect Dis. 26:191–198. 2020.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Murakami N, Hayden R, Hills T, Al-Samkari
H, Casey J, Del Sorbo L, Lawler PR, Sise ME and Leaf DE:
Therapeutic advances in COVID-19. Nat Rev Nephrol. 19:38–52.
2023.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Narayanan SA, Jamison DA Jr, Guarnieri JW,
Zaksas V, Topper M, Koutnik AP, Park J, Clark KB, Enguita FJ,
Leitão AL, et al: A comprehensive SARS-CoV-2 and COVID-19 review,
Part 2: Host extracellular to systemic effects of SARS-CoV-2
infection. Eur J Hum Genet. 32:10–20. 2024.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Tulimilli SV, Dallavalasa S, Basavaraju
CG, Kumar Rao V, Chikkahonnaiah P, Madhunapantula SV and Veeranna
RP: Variants of severe acute respiratory syndrome coronavirus 2
(SARS-CoV-2) and vaccine effectiveness. Vaccines (Basel).
10(1751)2022.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Watson OJ, Barnsley G, Toor J, Hogan AB,
Winskill P and Ghani AC: Global impact of the first year of
COVID-19 vaccination: A mathematical modelling study. Lancet Infect
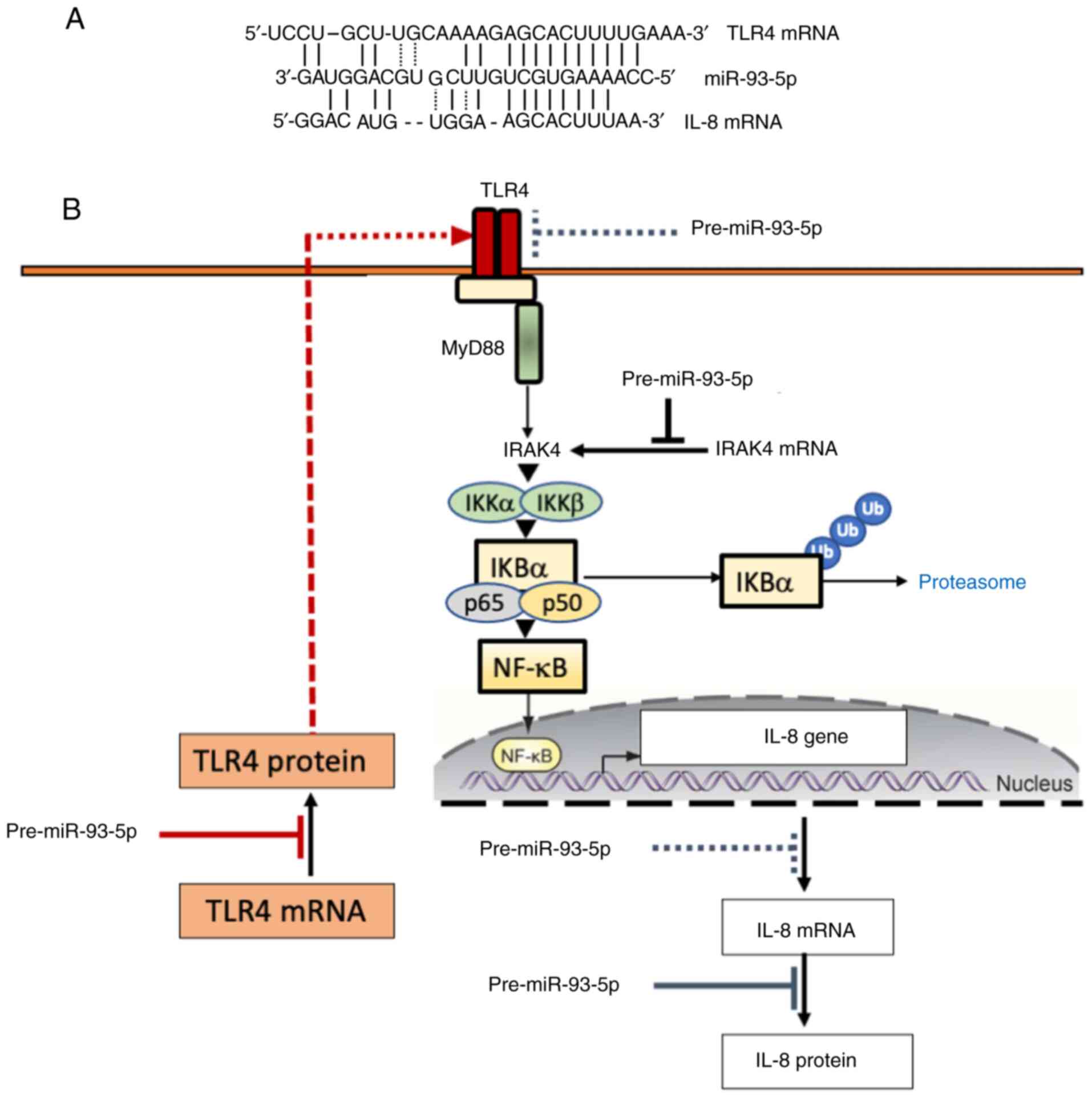
Dis. 22:1293–1302. 2022.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Walker PGT, Whittaker C, Watson OJ,
Baguelin M, Winskill P, Hamlet A, Djafaara BA, Cucunubá Z, Olivera
Mesa D, Green W, et al: The impact of COVID-19 and strategies for
mitigation and suppression in low- and middle-income countries.
Science. 369:413–422. 2020.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Villamagna AH, Gore SJ, Lewis JS and
Doggett JS: The need for antiviral drugs for pandemic coronaviruses
from a global health perspective. Front Med (Lausanne).
7(596587)2020.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Mikulska M, Sepulcri C, Dentone C, Magne
F, Balletto E, Baldi F, Labate L, Russo C, Mirabella M, Magnasco L,
et al: Triple combination therapy with 2 antivirals and monoclonal
antibodies for persistent or relapsed severe acute respiratory
syndrome coronavirus 2 infection in immunocompromised patients.
Clin Infect Dis. 77:280–286. 2023.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Meyerowitz EA and Li Y: Review: The
landscape of antiviral therapy for COVID-19 in the era of
widespread population immunity and omicron-lineage viruses. Clin
Infect Dis. 78:908–917. 2024.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Selickman J, Vrettou CS, Mentzelopoulos SD
and Marini JJ: COVID-19-related ARDS: Key mechanistic features and
treatments. J Clin Med. 11(4896)2022.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Silva MJA, Ribeiro LR, Gouveia MIM,
Marcelino BDR, Santos CSD, Lima KVB and Lima LNGC:
Hyperinflammatory response in COVID-19: A systematic review.
Viruses. 15(553)2023.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Conti P, Caraffa A, Gallenga CE, Ross R,
Kritas SK, Frydas I, Younes A and Ronconi G: Coronavirus-19
(SARS-CoV-2) induces acute severe lung inflammation via IL-1
causing cytokine storm in COVID-19: A promising inhibitory
strategy. J Biol Regul Homeost Agents. 34:1971–1975.
2020.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Zawawi A, Naser AY, Alwafi H and Minshawi
F: Profile of circulatory cytokines and chemokines in human
coronaviruses: A systematic review and meta-analysis. Front
Immunol. 12(666223)2021.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Altmann DM, Whettlock EM, Liu S,
Arachchillage DJ and Boyton RJ: The immunology of long COVID. Nat
Rev Immunol. 23:618–634. 2023.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Ghorra N, Popotas A, Besse-Hammer T,
Rogiers A, Corazza F and Nagant C: Cytokine profile in patients
with postacute sequelae of COVID-19. Viral Immunol. 37:346–354.
2024.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Song P, Li W, Xie J, Hou Y and You C:
Cytokine storm induced by SARS-CoV-2. Clin Chim Acta. 509:280–287.
2020.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Sefik E, Qu R, Junqueira C, Kaffe E, Mirza
H, Zhao J, Brewer JR, Han A, Steach HR, Israelow B, et al:
Inflammasome activation in infected macrophages drives COVID-19
pathology. Nature. 606:585–593. 2022.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Majidpoor J and Mortezaee K: Interleukin-6
in SARS-CoV-2 induced disease: Interactions and therapeutic
applications. Biomed Pharmacother. 145(112419)2022.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Santa Cruz A, Mendes-Frias A, Oliveira AI,
Dias L, Matos AR, Carvalho A, Capela C, Pedrosa J, Castro AG and
Silvestre R: Interleukin-6 is a biomarker for the development of
fatal severe acute respiratory syndrome coronavirus 2 pneumonia.
Front Immunol. 12(613422)2021.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Zizzo G, Tamburello A, Castelnovo L, Laria
A, Mumoli N, Faggioli PM, Stefani I and Mazzone A: Immunotherapy of
COVID-19: Inside and beyond IL-6 signalling. Front Immunol.
13(795315)2022.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Li L, Li J, Gao M, Fan H, Wang Y, Xu X,
Chen C, Liu J, Kim J, Aliyari R, et al: Interleukin-8 as a
biomarker for disease prognosis of coronavirus disease-2019
patients. Front Immunol. 11(602395)2021.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Yu Q, Zhou X, Kapini R, Arsecularatne A,
Song W, Li C, Liu Y, Ren J, Münch G, Liu J and Chang D: Cytokine
storm in COVID-19: Insight into pathological mechanisms and
therapeutic benefits of chinese herbal medicines. Medicines
(Basel). 11(14)2024.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Comarmond C, Drumez E, Labreuche J,
Hachulla E, Thomas T, Flipo RM, Seror R, Avouac J, Balandraud N,
Desbarbieux R, et al: COVID-19 presentation and outcomes in
patients with inflammatory rheumatic and musculoskeletal diseases
receiving IL6-receptor antagonists prior to SARS-CoV-2 infection. J
Transl Autoimmun. 6(100190)2023.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Ghosn L, Chaimani A, Evrenoglou T,
Davidson M, Graña C, Schmucker C, Bollig C, Henschke N, Sguassero
Y, Nejstgaard CH, et al: Interleukin-6 blocking agents for treating
COVID-19: A living systematic review. Cochrane Database Syst Rev.
3(CD013881)2021.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Pomponio G, Ferrarini A, Bonifazi M,
Moretti M, Salvi A, Giacometti A, Tavio M, Titolo G, Morbidoni L,
Frausini G, et al: Tocilizumab in COVID-19 interstitial pneumonia.
J Intern Med. 289:738–746. 2021.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Castelnovo L, Tamburello A, Lurati A,
Zaccara E, Marrazza MG, Olivetti M, Mumoli N, Mastroiacovo D,
Colombo D, Ricchiuti E, et al: Anti-IL6 treatment of serious
COVID-19 disease: A monocentric retrospective experience. Medicine
(Baltimore). 100(e23582)2021.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Tharmarajah E, Buazon A, Patel V, Hannah
JR, Adas M, Allen VB, Bechman K, Clarke BD, Nagra D, Norton S, et
al: IL-6 inhibition in the treatment of COVID-19: A meta-analysis
and meta-regression. J Infect. 82:178–185. 2021.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Segú-Vergés C, Artigas L, Coma M and Peck
RW: Artificial intelligence assessment of the potential of
tocilizumab along with corticosteroids therapy for the management
of COVID-19 evoked acute respiratory distress syndrome. PLoS One.
18(e0280677)2023.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Dominguez C, McCampbell KK, David JM and
Palena C: Neutralization of IL-8 decreases tumor PMN-MDSCs and
reduces mesenchymalization of claudin-low triple-negative breast
cancer. JCI Insight. 2(e9496)2017.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Piemonti L, Landoni G, Voza A, Puoti M,
Gentile I, Coppola N, Nava S, Mattei A, Marinangeli F, Marchetti G,
et al: Efficacy and safety of reparixin in patients with severe
COVID-19 pneumonia: A phase 3, randomized, double-blind
placebo-controlled study. Infect Dis Ther. 12:2437–2456.
2023.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Zarbock A, Allegretti M and Ley K:
Therapeutic inhibition of CXCR2 by Reparixin attenuates acute lung
injury in mice. Br J Pharmacol. 155:357–364. 2008.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Kaiser R, Leunig A, Pekayvaz K, Popp O,
Joppich M, Polewka V, Escaig R, Anjum A, Hoffknecht ML, Gold C, et
al: Self-sustaining IL-8 loops drive a prothrombotic neutrophil
phenotype in severe COVID-19. JCI Insight.
6(e150862)2021.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Shang R, Lee S, Senavirathne G and Lai EC:
microRNAs in action: Biogenesis, function and regulation. Nat Rev
Genet. 24:816–833. 2023.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Fazi and Nervi C: MicroRNA: Basic
mechanisms and transcriptional regulatory networks for cell fate
determination. Cardiovasc Res. 79:553–561. 2008.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Ivey KN and Srivastava D: microRNAs as
developmental regulators. Cold Spring Harb Perspect Biol.
7(a008144)2015.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Chaudhuri K and Chatterjee R: MicroRNA
detection and target prediction: Integration of computational and
experimental approaches. DNA Cell Biol. 26:321–337. 2007.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Doench JG and Sharp PA: Specificity of
microRNA target selection in translational repression. Genes Dev.
18:504–511. 2004.PubMed/NCBI View Article : Google Scholar
|
|
38
|
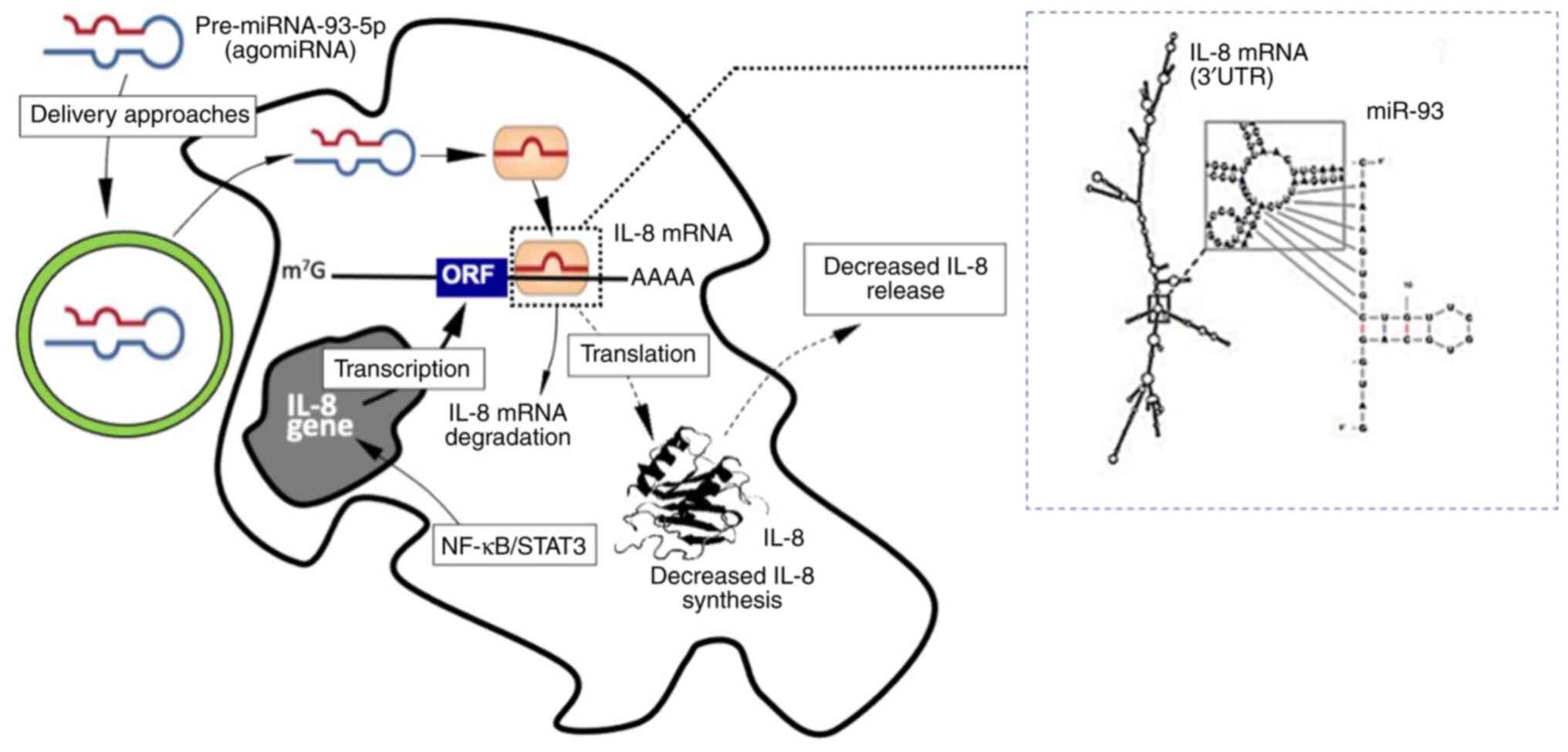
Gasparello J, Finotti A and Gambari R:
Tackling the COVID-19 ‘cytokine storm’ with microRNA mimics
directly targeting the 3'UTR of pro-inflammatory mRNAs. Med
Hypotheses. 146(110415)2021.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Fabbri E, Borgatti M, Montagner G, Bianchi
N, Finotti A, Lampronti I, Bezzerri V, Dechecchi MC, Cabrini G and
Gambari R: Expression of microRNA-93 and interleukin-8 during
pseudomonas aeruginosa-mediated induction of proinflammatory
responses. Am J Respir Cell Mol Biol. 50:1144–1155. 2014.PubMed/NCBI View Article : Google Scholar
|
|
40
|
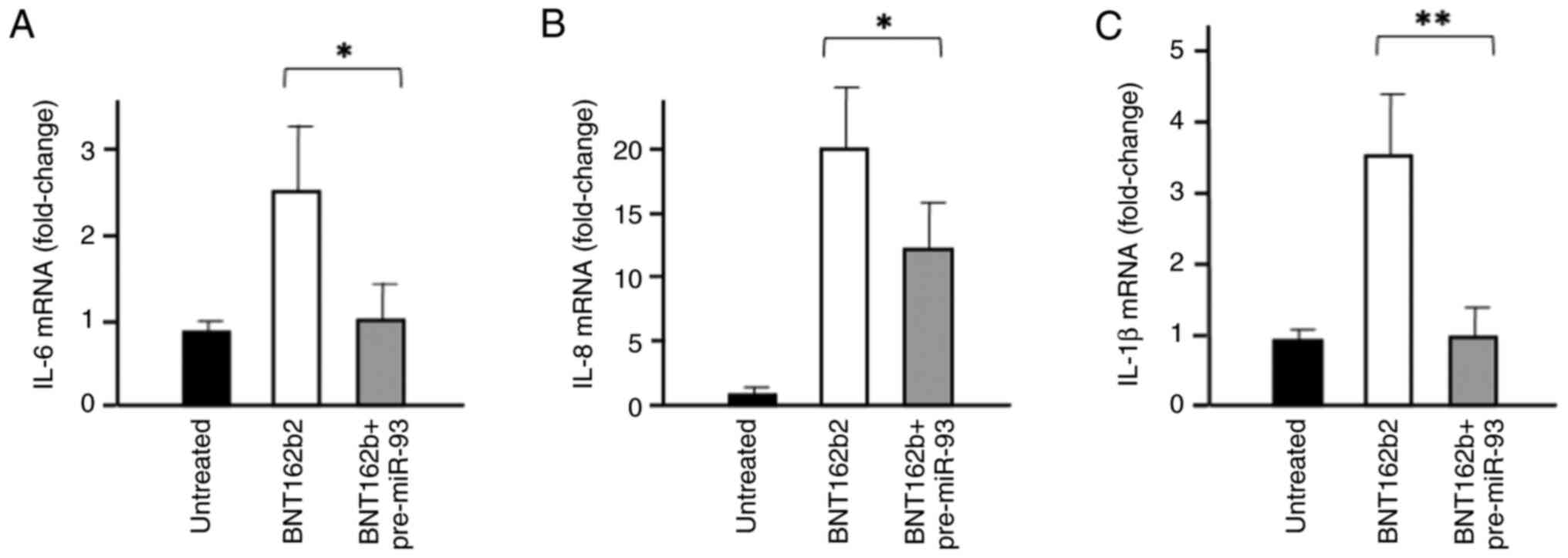
Gasparello J, d'Aversa E, Breveglieri G,
Borgatti M, Finotti A and Gambari R: In vitro induction of
interleukin-8 by SARS-CoV-2 spike protein is inhibited in bronchial
epithelial IB3-1 cells by a miR-93-5p agomiR. Int Immunopharmacol.
101(108201)2021.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Wu J, Ding J, Yang J, Guo X and Zheng Y:
MicroRNA roles in the nuclear factor kappa B signaling pathway in
cancer. Front Immunol. 9(546)2018.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Hanna J, Hossain G and Kocerha J: The
potential for microRNA therapeutics and clinical research. Front
Genet. 10(478)2019.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Momin MY, Gaddam RR, Kravitz M, Gupta A
and Vikram A: The challenges and opportunities in the development
of MicroRNA therapeutics: A multidisciplinary viewpoint. Cells.
10(3097)2021.PubMed/NCBI View Article : Google Scholar
|
|
44
|
Diener C, Keller A and Meese E: Emerging
concepts of miRNA therapeutics: From cells to clinic. Trends Genet.
38:613–626. 2022.PubMed/NCBI View Article : Google Scholar
|
|
45
|
Rupaimoole R and Slack FJ: MicroRNA
therapeutics: Towards a new era for the management of cancer and
other diseases. Nat Rev Drug Discov. 16:203–222. 2017.PubMed/NCBI View Article : Google Scholar
|
|
46
|
Lee EC, Valencia T, Allerson C, Schairer
A, Flaten A, Yheskel M, Kersjes K, Li J, Gatto S, Takhar M, et al:
Discovery and preclinical evaluation of anti-miR-17 oligonucleotide
RGLS4326 for the treatment of polycystic kidney disease. Nat
Commun. 10(4148)2019.PubMed/NCBI View Article : Google Scholar
|
|
47
|
Reid G, Kao SC, Pavlakis N, Brahmbhatt H,
MacDiarmid J, Clarke S, Boyer M and van Zandwijk N: Clinical
development of TargomiRs, a miRNA mimic-based treatment for
patients with recurrent thoracic cancer. Epigenomics. 8:1079–1085.
2016.PubMed/NCBI View Article : Google Scholar
|
|
48
|
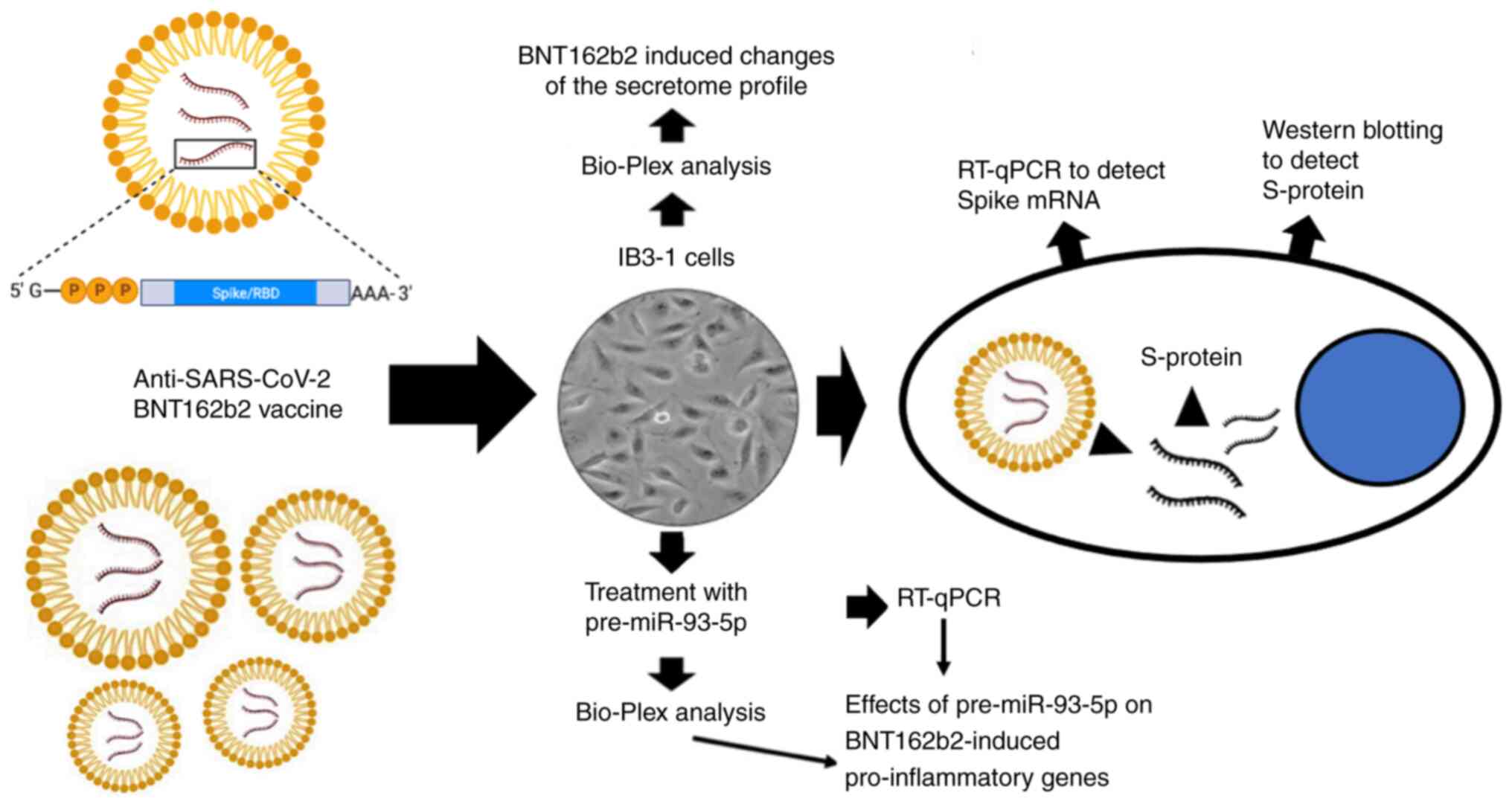
Zurlo M, Gasparello J, Verona M, Papi C,
Cosenza LC, Finotti A, Marzaro G and Gambari R: The anti-SARS-CoV-2
BNT162b2 vaccine suppresses mithramycin-induced erythroid
differentiation and expression of embryo-fetal globin genes in
human erythroleukemia K562 cells. Exp Cell Res.
433(113853)2023.PubMed/NCBI View Article : Google Scholar
|
|
49
|
Cosenza LC, Marzaro G, Zurlo M, Gasparello
J, Zuccato C, Finotti A and Gambari R: Inhibitory effects of
SARS-CoV-2 spike protein and BNT162b2 vaccine on
erythropoietin-induced globin gene expression in erythroid
precursor cells from patients with β-thalassemia. Exp Hematol.
129(104128)2024.PubMed/NCBI View Article : Google Scholar
|
|
50
|
Gasparello J, D'Aversa E, Papi C, Gambari
L, Grigolo B, Borgatti M, Finotti A and Gambari R: Sulforaphane
inhibits the expression of interleukin-6 and interleukin-8 induced
in bronchial epithelial IB3-1 cells by exposure to the SARS-CoV-2
spike protein. Phytomedicine. 87(153583)2021.PubMed/NCBI View Article : Google Scholar
|
|
51
|
Verbeke R, Hogan MJ, Loré K and Pardi N:
Innate immune mechanisms of mRNA vaccines. Immunity. 55:1993–2005.
2022.PubMed/NCBI View Article : Google Scholar
|
|
52
|
Sartorius R, Trovato M, Manco R, D'Apice L
and De Berardinis P: Exploiting viral sensing mediated by Toll-like
receptors to design innovative vaccines. NPJ Vaccines.
6(127)2021.PubMed/NCBI View Article : Google Scholar
|
|
53
|
Delehedde C, Even L, Midoux P, Pichon C
and Perche F: Intracellular routing and recognition of lipid-based
mRNA nanoparticles. Pharmaceutics. 13(945)2021.PubMed/NCBI View Article : Google Scholar
|
|
54
|
Dechecchi MC, Nicolis E, Norez C, Bezzerri
V, Borgatti M, Mancini I, Rizzotti P, Ribeiro CM, Gambari R, Becq F
and Cabrini G: Anti-inflammatory effect of miglustat in bronchial
epithelial cells. J Cyst Fibros. 7:555–565. 2008.PubMed/NCBI View Article : Google Scholar
|
|
55
|
Gambari R, Borgatti M, Lampronti I, Fabbri
E, Brognara E, Bianchi N, Piccagli L, Yuen MCW, Kan CW, Hau DKP, et
al: Corilagin is a potent inhibitor of NF-kappaB activity and
downregulates TNF-alpha induced expression of IL-8 gene in cystic
fibrosis IB3-1 cells. Int Immunopharmacol. 13:308–315.
2012.PubMed/NCBI View Article : Google Scholar
|
|
56
|
De Stefano D, Ungaro F, Giovino C,
Polimeno A, Quaglia F and Carnuccio R: Sustained inhibition of IL-6
and IL-8 expression by decoy ODN to NF-κB delivered through
respirable large porous particles in LPS-stimulated cystic fibrosis
bronchial cells. J Gene Med. 13:200–208. 2011.PubMed/NCBI View Article : Google Scholar
|
|
57
|
Gao H, Xiao D, Gao L and Li :
MicroRNA-93 contributes to the suppression of lung inflammatory
responses in LPS-induced acute lung injury in mice via the
TLR4/MyD88/NF-κB signaling pathway. Int J Mol Med. 46:561–570.
2020.PubMed/NCBI View Article : Google Scholar
|
|
58
|
Silva-Aguiar RP, Teixeira DE, Peruchetti
DB, Peres RAS, Alves SAS, Calil PT, Arruda LB, Costa LJ, Silva PL,
Schmaier AH, et al: Toll like receptor 4 mediates the inhibitory
effect of SARS-CoV-2 spike protein on proximal tubule albumin
endocytosis. Biochim Biophys Acta Mol Basis Dis.
1870(167155)2024.PubMed/NCBI View Article : Google Scholar
|
|
59
|
Chakraborty C, Mallick B, Bhattacharya M
and Byrareddy S: SARS-CoV-2 omicron spike shows strong binding
affinity and favourable interaction landscape with the TLR4/MD2
compared to other variants. J Genet Eng Biotechnol.
22(100347)2024.PubMed/NCBI View Article : Google Scholar
|
|
60
|
Fontes-Dantas FL, Fernandes GG, Gutman EG,
De Lima EV, Antonio LS, Hammerle MB, Mota-Araujo HP, Colodeti LC,
Araújo SMB, Froz GM, et al: SARS-CoV-2 spike protein induces
TLR4-mediated long-term cognitive dysfunction recapitulating
post-COVID-19 syndrome in mice. Cell Rep. 42(112189)2023.PubMed/NCBI View Article : Google Scholar
|
|
61
|
Choudhury A and Mukherjee S: In silico
studies on the comparative characterization of the interactions of
SARS-CoV-2 spike glycoprotein with ACE-2 receptor homologs and
human TLRs. J Med Virol. 92:2105–2113. 2020.PubMed/NCBI View Article : Google Scholar
|
|
62
|
Zhao Y, Kuang M, Li J, Zhu L, Jia Z, Guo
X, Hu Y, Kong J, Yin H, Wang X and You F: SARS-CoV-2 spike protein
interacts with and activates TLR41. Cell Res. 31:818–820.
2021.PubMed/NCBI View Article : Google Scholar
|
|
63
|
Patra R, Chandra Das N and Mukherjee S:
Targeting human TLRs to combat COVID-19: A solution? J Med Virol.
93:615–617. 2021.PubMed/NCBI View Article : Google Scholar
|
|
64
|
Das NC, Labala R, Patra R, Chattoraj A and
Mukherjee S: In silico identification of new anti-SARS-CoV-2 agents
from bioactive phytocompounds targeting the viral spike
glycoprotein and human TLR4. Lettr Drug Des Discov. 19:175–191.
2022.
|
|
65
|
Sahanic S, Hilbe R, Dünser C, Tymoszuk P,
Löffler-Ragg J, Rieder D, Trajanoski Z, Krogsdam A, Demetz E,
Yurchenko M, et al: SARS-CoV-2 activates the TLR4/MyD88 pathway in
human macrophages: A possible correlation with strong
pro-inflammatory responses in severe COVID-19. Heliyon.
9(e21893)2023.PubMed/NCBI View Article : Google Scholar
|
|
66
|
Nakazawa D, Takeda Y, Kanda M, Tomaru U,
Ogawa H, Kudo T, Shiratori-Aso S, Watanabe-Kusunoki K, Ueda Y,
Miyoshi A, et al: Inhibition of Toll-like receptor 4 and
Interleukin-1 receptor prevent SARS-CoV-2 mediated kidney injury.
Cell Death Discov. 9(293)2023.PubMed/NCBI View Article : Google Scholar
|
|
67
|
Asaba CN, Ekabe CJ, Ayuk HS, Gwanyama BN,
Bitazar R and Bukong TN: Interplay of TLR4 and SARS-CoV-2:
Unveiling the complex mechanisms of inflammation and severity in
COVID-19 infections. J Inflamm Res. 17:5077–5091. 2024.PubMed/NCBI View Article : Google Scholar
|
|
68
|
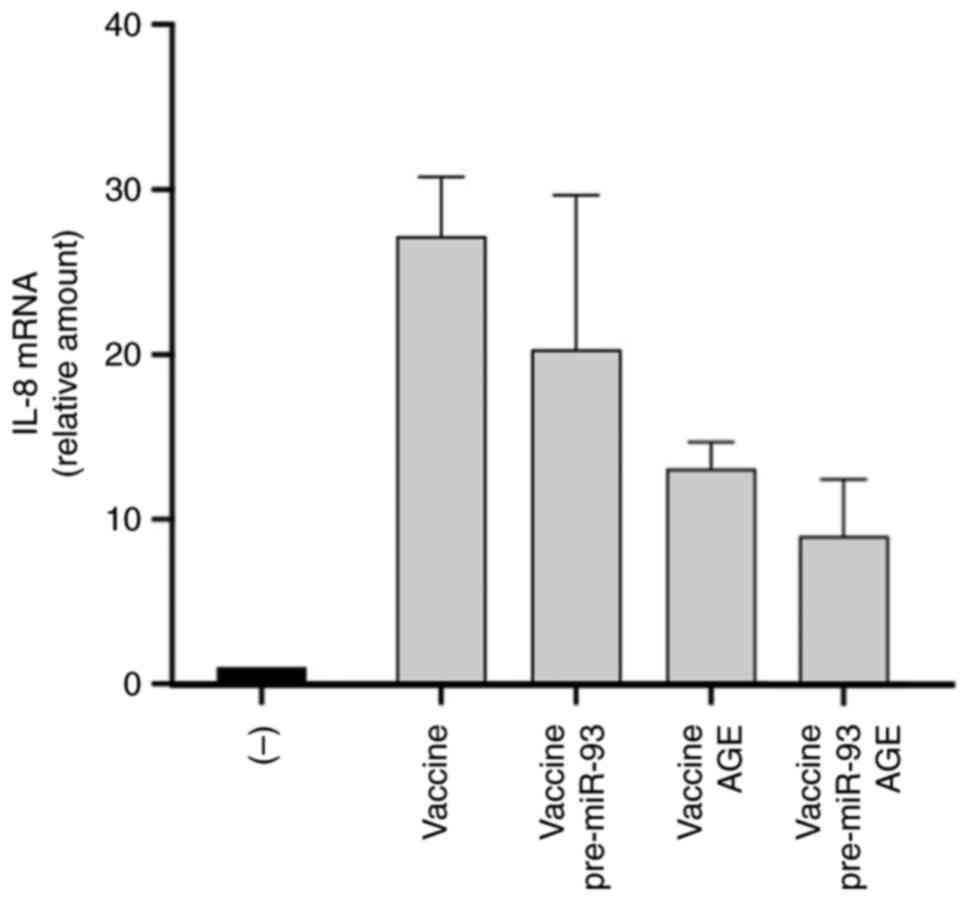
Gasparello J, Papi C, Marzaro G, Macone A,
Zurlo M, Finotti A, Agostinelli E and Gambari R: Aged garlic
extract (AGE) and its constituents S-allyl-cysteine (SAC) inhibit
the expression of pro-inflammatory genes induced in bronchial
epithelial IB3-1 cells by exposure to the SARS-CoV-2 spike protein
and the BNT162b2 vaccine. Molecules. 29(5938)2024.PubMed/NCBI View Article : Google Scholar
|
|
69
|
Gasparello J, Marzaro G, Papi C, Gentili
V, Rizzo R, Zurlo M, Scapoli C, Finotti A and Gambari R: Effects of
Sulforaphane on SARS-CoV-2 infection and NF-κB dependent expression
of genes involved in the COVID-19 ‘cytokine storm’. Int J Mol Med.
52(76)2023.PubMed/NCBI View Article : Google Scholar
|
|
70
|
Fertig TE, Chitoiu L, Marta DS, Ionescu
VS, Cismasiu VB, Radu E, Angheluta G, Dobre M, Serbanescu A,
Hinescu ME and Gherghiceanu M: Vaccine mRNA can be detected in
blood at 15 days post-vaccination. Biomedicines.
10(1538)2022.PubMed/NCBI View Article : Google Scholar
|
|
71
|
Zhou Q, Zhang L, Dong Y, Wang Y, Zhang B,
Zhou S, Huang Q, Wu T and Chen G: The role of SARS-CoV-2-mediated
NF-κB activation in COVID-19 patients. Hypertens Res. 47:375–384.
2024.PubMed/NCBI View Article : Google Scholar
|
|
72
|
Forsyth CB, Zhang L, Bhushan A, Swanson B,
Zhang L, Mamede JI, Voigt RM, Shaikh M, Engen PA and Keshavarzian
A: The SARS-CoV-2 S1 spike protein promotes MAPK and NF-κB
activation in human lung cells and inflammatory cytokine production
in human lung and intestinal epithelial cells. Microorganisms.
10(1996)2022.PubMed/NCBI View Article : Google Scholar
|
|
73
|
Zhang G and Ghosh S: Toll-like
receptor-mediated NF-kappaB activation: A phylogenetically
conserved paradigm in innate immunity. J Clin Invest. 107:13–19.
2001.PubMed/NCBI View Article : Google Scholar
|
|
74
|
Gargiulo S, Gamba P, Testa G, Rossin D,
Biasi F, Poli G and Leonarduzzi G: Relation between TLR4/NF-κB
signaling pathway activation by 27-hydroxycholesterol and
4-hydroxynonenal, and atherosclerotic plaque instability. Aging
Cell. 14:569–581. 2015.PubMed/NCBI View Article : Google Scholar
|
|
75
|
Muir A, Soong G, Sokol S, Reddy B, Gomez
MI, Van Heeckeren A and Prince A: Toll-like receptors in normal and
cystic fibrosis airway epithelial cells. Am J Respir Cell Mol Biol.
30:777–783. 2004.PubMed/NCBI View Article : Google Scholar
|
|
76
|
Greene CM, Carroll TP, Smith SGJ, Taggart
CC, Devaney J, Griffin S, O'neill SJ and McElvaney NG: TLR-induced
inflammation in cystic fibrosis and non-cystic fibrosis airway
epithelial cells. J Immunol. 174:1638–1646. 2005.PubMed/NCBI View Article : Google Scholar
|
|
77
|
Xu Y, Jin H, Yang X, Wang L, Su L, Liu K,
Gu Q and Xu X: MicroRNA-93 inhibits inflammatory cytokine
production in LPS-stimulated murine macrophages by targeting IRAK4.
FEBS Lett. 588:1692–1698. 2014.PubMed/NCBI View Article : Google Scholar
|
|
78
|
Tian F, Yuan C, Hu L and Shan S:
MicroRNA-93 inhibits inflammatory responses and cell apoptosis
after cerebral ischemia reperfusion by targeting interleukin-1
receptor-associated kinase 4. Exp Ther Med. 14:2903–2910.
2017.PubMed/NCBI View Article : Google Scholar
|
|
79
|
Wei L and Zhao D: M2 macrophage-derived
exosomal miR-145-5p protects against the
hypoxia/reoxygenation-induced pyroptosis of cardiomyocytes by
inhibiting TLR4 expression. Ann Transl Med. 10(1376)2022.PubMed/NCBI View Article : Google Scholar
|
|
80
|
Jin C, Wang A, Liu L, Wang G, Li G and Han
Z: miR-145-5p inhibits tumor occurrence and metastasis through the
NF-κB signaling pathway by targeting TLR4 in malignant melanoma. J
Cell Biochem. 120:11115–11126. 2019.PubMed/NCBI View Article : Google Scholar
|
|
81
|
Ma X, Becker Buscaglia LE, Barker JR and
Li Y: MicroRNAs in NF-kappaB signaling. J Mol Cell Biol. 3:159–166.
2011.PubMed/NCBI View Article : Google Scholar
|
|
82
|
Ghafouri-Fard S, Abak A, Fattahi F, Hussen
BM, Bahroudi Z, Shoorei H and Taheri M: . The interaction between
miRNAs/lncRNAs and nuclear factor-κB (NF-κB) in human disorders.
Biomed Pharmacother. 138(111519)2021.PubMed/NCBI View Article : Google Scholar
|