Introduction
Pancreatic cancer is one of the major causes of
cancer-related mortality worldwide, with a 5-year survival rate of
<5% (1,2). For patients with localized disease,
radical surgery may provide long-term benefits. However, even in
patients who undergo resection, the reported 5-year survival rate
remains low (7–24%) and the median survival is only ~1 year in most
patient series, indicating that surgery alone is generally
inadequate. Even following curative resection, patients with
pancreatic cancer are likely to experience a 50–80% local
recurrence rate and a 25–50% risk of developing distant metastases
(3). Adjuvant chemotherapy with
gemcitabine (GEM), the key drug used in the treatment of pancreatic
cancer, improves the survival of patients with resectable
pancreatic adenocarcinoma compared to resection alone (4), although to a limited extent.
However, 20–30% of patients are unable to receive
the designated therapy due to postoperative complications, delayed
surgical recovery and/or early disease recurrence (5,6). To
improve the therapeutic results of resected pancreatic cancer, it
is critical to optimize the postoperative management of liver
metastases, which frequently constitute the major determining
factor of prognosis.
An alternative treatment option that may be
beneficial in pancreatic cancer patients with liver metastases is
the hepatic arterial infusion (HAI) of chemotherapeutic agents.
This treatment option has been applied to patients with primary or
metastatic hepatic malignancies that are confined to the liver and
is soundly based on physiological and pharmacological factors.
First, liver metastases that grow >2–3 mm depend on the hepatic
artery for vascularization, whereas normal liver tissues are
perfused by the portal vein (7,8).
Second, HAI therapy allows drug delivery to hepatic metastases not
achievable by systemic administration, particularly of drugs with a
high systemic clearance rate (9).
Third, first-pass hepatic extraction of certain drugs results in
lower systemic concentrations and, thus, few systemic toxicities
(10). Phase I studies of HAI
chemotherapy with GEM in patients with liver malignancies have been
previously published (8–10). Moreover, results from our recent
pilot study suggest that HAI chemotherapy with GEM and
5-fluorouracil (5-FU) is safe and beneficial for the treatment of
postoperative metastatic tumors confined to the liver, even in
patients with poor general condition (11).
Over the past few years, we have expanded the number
of cases treated with HAI chemotherapy with GEM at our institution
to include cases with other metastases in addition to liver
metastases, by the addition of oral S-1 in lieu of 5-FU. S-1 is an
oral fluorinated pyrimidine compound developed by Taiho
Pharmaceutical Co., Ltd., (Tokyo, Japan). The administration of
oral S-1 is more convenient and simulates the effect of continuous
infusion of 5-FU. The safety and effectiveness of the combination
chemotherapy with GEM and S-1 for advanced pancreatic cancer were
reported by previous studies (12–14)
and a phase III (GEST) trial in Japanese patients demonstrated that
S-1 was not inferior to GEM (15).
In this study, we present the final results of the patients who
were treated with HAI with GEM plus 5-FU or HAI with GEM and oral
S-1.
Materials and methods
Patient eligibility
Seven patients with postoperative liver metastases
from pancreatic cancer underwent HAI with GEM between October, 2008
and September, 2010 at Kanazawa University Hospital (Kanazawa,
Japan). Patients with metastases confined to the liver following
curative (R0) resection of the pancreatic primary adenocarcinoma
underwent HAI with GEM plus 5-FU (GEM+5-FU group). However,
patients with metastases confined to the liver following
non-curative (R1 or R2) resection or cases that involved metastases
to other organs along with liver metastases that may dictate
prognosis, underwent HAI with GEM and oral S-1 administration
(GEM+S-1 group). Written informed consent was obtained from each
patient prior to enrollment in the study and the treatment was
undertaken with the approval of the local Medical Ethics
Committee.
The baseline characteristics of the patients are
listed in Table I. Five out of the
7 patients received GEM plus 5-FU treatment and 2 received GEM plus
S-1 treatment. The male:female ratio was 5:2. The median patient
age was 64.9 years (range, 60–71 years). The Eastern Cooperative
Oncology Group performance status score was 0 in all patients in
this study. Four patients had received preoperative chemotherapy
with GEM and oral S-1 and adjuvant chemotherapy with GEM had been
administered to 5 out of the 7 patients prior to the appearance of
liver metastases. The interval between surgery and the appearance
of liver metastases was 7 months (range, 3–11 months). The median
standard liver volume [SLV (ml) = 706.2 × body surface area (BSA) +
2.4] was 1.1 l (range, 9.0–1.3 l) (16).
 | Table IPatient characteristics. |
Table I
Patient characteristics.
| Case number | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
|---|
| Age (years) | 61 | 62 | 69 | 71 | 60 | 66 | 65 |
| Gender | F | M | M | M | F | M | M |
| Performance
status | 0 | 0 | 0 | 0 | 0 | 0 | 1 |
| Tumor location | H | H | BT | BT | BT | H | BT |
| Residual tumor | 0 | 0 | 0 | 0 | 0 | 0 | 1 |
| Preoperative
chemotherapy | + | + | − | − | − | + | + |
| Postoperative
chemotherapy | − | + | − | + | + | + | + |
| Interval between
operation and liver metastases (months) | 5 | 10 | 3 | 10 | 5 | 11 | 5 |
| Body surface area
(m2) | 1.6 | 1.7 | 1.8 | 1.5 | 1.3 | 1.7 | 1.5 |
| Standard liver volume
(l) | 1.1 | 1.2 | 1.3 | 1.1 | 0.9 | 1.2 | 1.1 |
| Other metastatic
lesion prior to HAI | − | − | − | − | − | P | − |
| Group | GEM+5-FU | GEM+5-FU | GEM+5-FU | GEM+5-FU | GEM+5-FU | GEM+S-1 | GEM+S-1 |
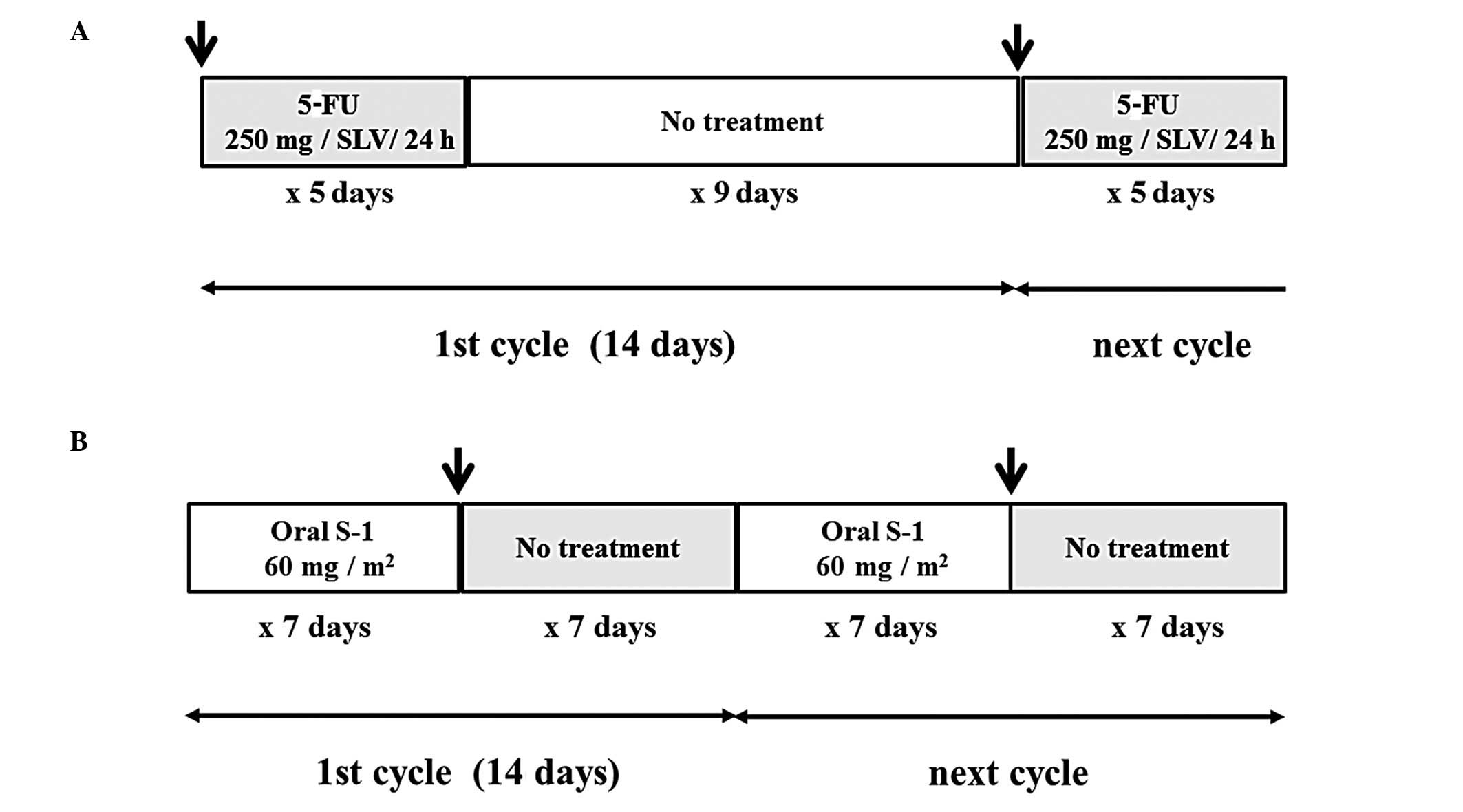
Catheter placement and treatment
regimen
An intrahepatic arterial catheter was percutaneously
implanted following hepatic arteriography via a right femoral
puncture to deliver chemotherapy. The catheter tip was placed in
the hepatic artery proper by a radiologist. The catheter was then
connected to a subcutaneous implantable port system, located in the
lower right abdominal area. In the GEM+5-FU group, an 800-mg/SLV
dose of GEM was dissolved in 50 ml of saline for administration
over a 30-min period using a bedside pump. Following GEM infusion,
a 250-mg/SLV dose of 5-FU dissolved in 50 ml of saline was infused
continuously over 24 h on days 1–5, comprising 1 cycle of therapy.
In case 1, only 400 mg of GEM was administered, due to the
development of leukocytopenia (17). Each treatment cycle was continued
biweekly on hospital days 1–6 (Fig.
1A). In the GEM+S-1 group, 60 mg/m2/day of S-1 was
administered for 7 consecutive days and an 800-mg/SLV dose of GEM
was administered on day 8 as in the GEM+5-FU group. Each treatment
cycle was continued biweekly in the outpatient clinic (Fig. 1B).
Assessment of response
Response to treatment was determined based on the
following measures: results of physical examination, complete blood
counts, biochemical tests and chest and abdominal radiography were
obtained prior to the initiation of each cycle. Serum CA 19-9 was
measured monthly and changes in this tumor marker were assessed
prior to and following 10 HAI cycles. Follow-up contrast-enhanced
computed tomography was performed upon completion of every 5
cycles, or more frequently for cases showing clinical
deterioration. The response rate was evaluated in accordance with
the Response Evaluation Criteria in Solid Tumors (RECIST) (18). A complete response (CR) was defined
as the disappearance of all evidence of disease and normalization
of tumor markers persisting for at least 2 weeks. A partial
response (PR) was defined as a >30% reduction on uni-dimensional
tumor measurements, without the appearance of any new lesions or
progression in any existing lesion. Progressive disease (PD) was
defined as any of the following: i) a 20% increase in the sum of
the products of all measurable lesions; ii) the appearance of any
new lesion; or iii) the reappearance of any lesion that had
previously disappeared. Stable disease (SD) was defined as a tumor
response that did not fulfill the criteria for CR, PR or PD.
In the GEM+5-FU group, HAI of 5-FU was terminated
after 10 cycles and administration of oral S-1 was initiated.
Patients in the two groups received GEM HAI and administration of
oral S-1 in the outpatient clinic for as long as possible, i.e.,
for as long as they exhibited no tumor regrowth or the appearance
of any new lesions and were free of HAI catheter-related problems.
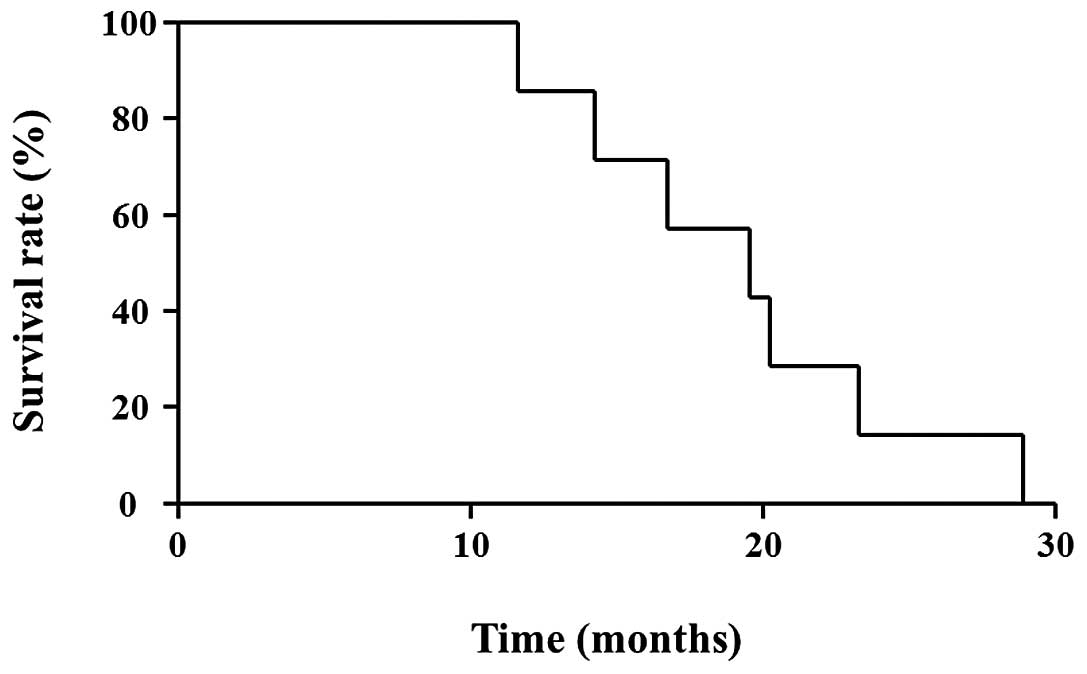
The median survival time (MST) was calculated from the initiation
of the study treatment until death and determined according to the
Kaplan-Meier method.
Results
In 6 out of the 7 cases, >10 cycles of HAI
chemotherapy were administered. In a single case (case 5), the HAI
catheter and subcutaneous implantable port system had to be removed
after eight cycles due to a problem with the tube. Based on RECIST,
PR was achieved in 2 out of the 7 cases and SD was achieved in 4
(response rate, 85.7%). CR was not achieved in any of the cases,
whereas PD was observed in 1 case. In 5 out of the 7 cases,
decreases in the serum tumor marker CA 19-9 levels were observed
after 10 cycles of HAI treatment. The median time to treatment
failure was 8 months (range, 0–17 months). The initial disease
progression factor was nodal and lung metastasis in 3 cases and
local recurrence plus peritoneal dissemination in 2. The overall
survival time from the initiation of the study treatment until
death was 17.4 months (range, 11–26 months) (Table II).
 | Table IITreatments and responses. |
Table II
Treatments and responses.
| Case number | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
|---|
| GEM administration
(cycles) | 13 | 40 | 23 | 10 | 8 | 15 | 12 |
| 5-FU administration
(cycles) | 10 | 10 | 10 | 10 | 6 | 0 | 0 |
| S-1 administration
(cycles) | 3 | 30 | 13 | 0 | 2 | 15 | 12 |
| Response | SD | PR | PR | PR | SD | SD | PD |
| TTF (months) | 15 | 17 | 7 | 8 | 3 | 6 | 0 |
| Other metastatic
lesion | L, N | N, P | Lg | L, Lg | N | P | Lg |
| Other
chemotherapy | Tx | Tx | Tx | Tx | Tx | Tx | Tx |
| Other therapy | RT | RT | − | − | − | − | − |
| Survival following
HAI (months) | 23 | 26 | 13 | 20 | 13 | 16 | 11 |
| Catheter
problems | + | + | − | + | + | + | + |
| CA19-9 prior to HAI
(U/ml) | 138 | 14 | 311 | 2,073 | 43,460 | 423 | 37 |
| CA19-9 following 10
HAI cycles (U/ml) | 33 | 65 | 221 | 811 | 32,200 | 34 | 1,060 |
Adverse events are listed in Table III. Grade 3 leukocytopenia was
observed in case 1; this patient was not able to receive adjuvant
systemic chemotherapy due to grade 2 leukocytopenia prior to HAI.
Leukocytopenia was also observed in 1 of the remaining 6 cases. The
patients were anemic; however, 5 out of the 7 patients had
developed anemia prior to HAI therapy. Grade 2 thrombocytopenia was
observed in 2 cases. Non-hematological events, such as nausea,
diarrhea, liver injury (AST/ALT increase), or neuropathy were not
observed. Of note, there were no life-threatening toxicities.
However, catheter-related complications (arterial thrombosis or
catheter dislocation) occurred in 6 cases (85.7%) and the HAI
catheter and subcutaneous implantable port system had to be removed
(Table II). All 7 patients
eventually succumbed to the primary disease. The MST was 22.4
months (Fig. 2).
 | Table IIITreatment toxicities (NCI-CTC
grade) |
Table III
Treatment toxicities (NCI-CTC
grade)
| Case number | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
|---|
| Anemia | 2a | 2a | 1 | 1a | 2a | 2a | 1 |
| Leukocytopenia | 3b | 0 | 0 | 0 | 0 | 2a | 0 |
|
Thrombocytopenia | 2a | 1 | 0 | 2 | 0 | 1a | 0 |
| Nausea | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Diarrhea | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Liver injury | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Neuropathy | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
Discussion
Pancreatic cancer is almost always fatal, with a
5-year survival rate of <5% (1,2).
Surgery remains the only curative option and usually consists of
radical pancreatic resection, including wide lymph node dissection
and complete removal of the extra-pancreatic nerve plexus of the
superior mesenteric artery or celiac axis (19,20).
Adjuvant chemotherapy improves the survival of patients with
resectable pancreatic adenocarcinoma compared to resection alone
(4), although to a limited extent.
However, 20–30% of patients are unable to receive the designated
therapy due to postoperative complications, delayed surgical
recovery and/or early disease recurrence (5,6). In
particular, the appearance of liver metastases early in the
postoperative period significantly contributes to a poor prognosis
in postoperative patients. For these patients, HAI chemotherapy,
which has less of an effect on the body as a whole, may provide an
effective treatment alternative to standard adjuvant
chemotherapy.
Arterial infusion chemotherapy with GEM and 5-FU has
been reported as a treatment for locally advanced pancreatic cancer
and liver metastases from pancreatic cancer (10,21,22).
Furthermore, in previous phase I studies, HAI chemotherapy with GEM
was well-tolerated up to 1,000 mg/m2 infused over 400
min (8,9).
According to the pharmacokinetics of GEM, when 1,000
mg/m2 of GEM is administered via intravenous infusion
over 30 min, the average maximum plasma concentrations reach
21,865±4,165 ng/ml by 15 min. The flow volume of the hepatic artery
proper is reportedly ~330 ml/min (11). When an 800-mg dose of GEM is
infused into the hepatic artery proper over a 30-min period, the
local plasma concentration in the liver reaches ~80,000 ng/ml by 30
min. Vogl et al(8) reported
that the maximum tolerated dose of HAI chemotherapy with GEM was
1,400 mg/m2. Conversely, the plasma concentration of
5-FU with a 250-mg infusion into the hepatic artery proper over a
24-h period was 0.5 μg/ml. This concentration is equal to that
obtained following administration of 30 mg/kg (1,350 mg in the
reported patient) of 5-FU over a 24-h period (23). In addition, Maruyama et
al(24) reported that when
1,000–1,500 mg of 5-FU was infused into the hepatic artery over a
period of 5 h, the maximum plasma concentration was 0.48 μg/ml on
average, without the development of any grade 3 adverse effects.
Super-selective HAI may deliver high doses of chemotherapeutic
agents into the tumor vessels, producing increased regional levels
with higher effectiveness and lower incidence/severity of systemic
side effects. In this study, the response rate was 85.7%, despite 6
out of the 7 cases having received systemic chemotherapy with GEM
prior to HAI. Moreover, no severe toxicity developed with this
therapy. These findings indicate that HAI chemotherapy is safe and
effective for the treatment of postoperative liver metastasis from
pancreatic carcinoma. The drawbacks of HAI chemotherapy include
problems with the catheter and the appearance of new lesions
outside the liver. In this study, 6 out of the 7 cases eventually
required removal of the HAI catheter and the subcutaneous
implantable port system due to problems with the tube, and new
lesions outside the liver appeared in all 7 patients. Even in the
GEM+5-FU group, we performed HAI with GEM plus oral S-1 therapy
after 10 cycles under the hypothesis of the appearance of
extra-hepatic metastases. Moreover, patients who did not undergo R0
surgery for primary lesions and patients suspected of having
extra-hepatic metastases were assigned to the GEM+S-1 group.
Although the safety of GEM plus S-1 therapy was
previously demonstrated in the GEST trial (15), the occurrence of adverse events was
greater in the phase I study of neoadjuvant chemotherapy (NAC) for
resectable pancreatic cancer performed in our department. In
addition, NAC with GEM plus S-1 was not well-tolerated (25). Nakahira et al(26) reported that pretreatment with S-1
enhances the GEM effects on pancreatic cancer xenografts. The
mechanism underlying these enhanced effects is considered to be
5-FU-induced upregulation of human equilibrative nucleoside
transporter 1, the major mediator of GEM cellular uptake. In our
trial, S-1 was administered for 14 consecutive days prior to GEM,
which may explain the greater number of adverse events observed in
our study. However, to maximize the effect of GEM, it is
recommended that S-1 be administered prior to GEM. By using a
combination of oral S-1 and HAI of GEM, effective amounts of the
two chemotherapeutic agents were reached in the liver and the
systemic side effects were reduced.
In conclusion, HAI chemotherapy is safe and
effective for the treatment for postoperative metastases from
pancreatic cancer confined to the liver. A clinical phase I trial
of HAI chemotherapy with GEM plus 5-FU or oral S-1 is currently
being undertaken, which includes the measurement of GEM
concentration in the peripheral blood of patients in order to
determine the optimal dose.
References
|
1
|
International Agency for Research on
Cancer, World Health Organization. Globocan 2008. World Health
Organization. Website. http://globocan.iarc.fr/.
Accessed October 1, 2010
|
|
2
|
Ishii H, Furuse J, Boku N, et al: Phase II
study of gemcitabine chemotherapy alone for locally advanced
pancreatic carcinoma: JCOG0506. Jpn J Clin Oncol. 40:573–579. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Evans DB, Abbruzzese JL and Willett CG:
Cancer of the pancreas. Cancer: Principles and Practice of
Oncology. De Vita VT, Hellman S and Rosenberg SA: 6th edition.
Lippincott Williams and Wilkins; Philadelphia: pp. 1126–1161.
2001
|
|
4
|
Oettle H, Post S, Neuhaus P, et al:
Adjuvant chemotherapy with gemcitabine vs. observation in patients
undergo curative-intent resection of pancreatic cancer: a
randomized controlled trial. JAMA. 297:267–277. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Aloia TA, Lee JE, Vauthey JN, et al:
Delayed recovery after pancreaticoduodenectomy: a major factor
impairing the delivery of adjuvant chemotherapy? J Am Coll Surg.
204:347–355. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Sandy H, Bruckner H, Cooperman A, Paradiso
J and Kiefer L: Survival advantage of combined chemoradiotherapy
compared with resection as the initial treatment of patients with
regional pancreatic carcinoma. An outcomes trial. Cancer.
89:314–327. 2000. View Article : Google Scholar
|
|
7
|
Ensminger WD, Rosowsky A and Raso V: A
clinical pharmacological evaluation of hepatic arterial infusions
of 5-fluoro-2-deoxyuridine and 5-fluoroufacil. Cancer Res.
38:3784–3792. 1978.PubMed/NCBI
|
|
8
|
Vogl TJ, Schwarz W, Eichler K, et al:
Hepatic intraarterial chemotherapy with gemcitabine in patients
with unresectable cholangiocarcinoma and liver metastases of
pancreatic cancer: a clinical study on maximum tolerable dose and
treatment efficacy. J Cancer Res Clin Oncol. 132:745–755. 2006.
View Article : Google Scholar
|
|
9
|
Tse AN, Wu N, Patel D, Haviland D and
Kemeny N: A phase I study of gemcitabine given via intrahepatic
pump for primary or metastatic hepatic malignancies. Cancer
Chemother Pharmacol. 64:935–944. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Van Riel JM, Peters GJ, Mammatas LH, et
al: A phase I and pharmacokinetic study of gemcitabine given by
24-h hepatic arterial infusion. Eur J Cancer. 45:2519–2527.
2009.PubMed/NCBI
|
|
11
|
Tajima H, Ohta T, Kitagawa H, et al: Pilot
study of hepatic arterial infusion chemotherapy with gemcitabine
and 5-fluorouracil for patients with postoperative liver metastases
from pancreatic cancer. Exp Therap Med. 2:265–269. 2011. View Article : Google Scholar
|
|
12
|
Nakamura K, Yamaguchi T, Ishihara T, et
al: Phase I trial of oral S-1 combined with gemcitabine in
metastatic pancreatic cancer. Br J Cancer. 92:2134–2139. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Ueno H, Okusaka T, Ikeda M, et al: A phase
I study of combination chemotherapy with gemcitabine and oral S-1
for advanced pancreatic cancer. Oncology. 69:421–427. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Nakamura K, Yamaguchi T, Ishihara T, et
al: Phase II trial of oral S-1 combined with gemcitabine in
metastatic pancreatic cancer. Br J Cancer. 94:1575–1579.
2006.PubMed/NCBI
|
|
15
|
Ueno H, Ioka T, Ikeda M, et al: Randomized
phase III study of gemcitabine plus S-1 (GS) versus S-1 alone, or
gemcitabine alone in patiens with locally advanced and metastatic
pancreatic cacer in Japan and Taiwan: GEST study. J Clin Oncol.
31:1640–1648. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Urata K, Kawasaki S, Matsunami T, et al:
Calculation of child and adult standard liver volume for liver
transplantation. Hepatology. 21:1317–1321. 1995.PubMed/NCBI
|
|
17
|
Tajima H, Ohta T, Kitagawa H, et al:
Hepatic arterial infusion chemotherapy for post-operative liver
metastases from pancreatic cancer in a patient with leukocytopenia:
a case report. Exp Therap Med. 1:987–990. 2010.PubMed/NCBI
|
|
18
|
Therasse P, Arbuck SG, Eisenhauer EA, et
al: New guidelines to evaluate the response to treatment in solid
tumors. European Organization for Research and Treatment of Cancer,
National Cancer Institute of the United States, National Cancer
Institute of Canada. J Natl Cancer Inst. 92:205–216. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Nagakawa T, Nagamori M, Futakami F, et al:
Result of extensive surgery for pancreatic carcinoma. Cancer.
77:640–645. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Noto M, Miwa K, Kitagawa H, et al:
Pancreas head carcinoma: frequency of invasion to soft tissue
adherent to the superior mesenteric artery. Am J Surg Pathol.
29:1056–1061. 2005.PubMed/NCBI
|
|
21
|
Homma H, Akiyama T, Mezawa S, et al:
Advanced pancreatic carcinoma showing a complete response to
arterial infusion chemotherapy. Int J Clin Oncol. 9:197–201. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Miyanishi K, Ishiwatari H, Hayashi T, et
al: A Phase I trial of arterial infusion chemotherapy with
gemcitabine and 5-fluorouracil for unresectable advanced pancreatic
cancer after vascular supply distribution via superselective
embolization. Jpn J Clin Oncol. 38:268–274. 2008. View Article : Google Scholar
|
|
23
|
Kikuchi K and Kanno H: Comparison for
blood levels and clinical effects between tablet and other dosage
forms of 5-fluorouracil (5-FU). Gan To Kagaku Ryoho. 6:559–565.
1979.(In Japanese).
|
|
24
|
Maruyama S, Ando M and Watayo T:
Concentration of 5-FU after hepatic artery infusion chemotherapy
for liver metastases of colorectal cancer. Gan To Kagaku Ryoho.
30:1635–1638. 2003.(In Japanese).
|
|
25
|
Tajima H, Kitagawa H, Tsukada T, et al: A
phase I study of neoadjuvant chemotherapy with gemcitabine plus
oral S-1 for resectable pancreatic cancer. Mol Clin Oncol.
1:768–772. 2013.PubMed/NCBI
|
|
26
|
Nakahira S, Nakamori S, Tsujie M, et al:
Pretratment with S-1, an oral derivative of 5-fluorouracil,
enhances gemcitabine effect in pancreatic cancer xenografts.
Anticancer Res. 28:179–186. 2008.PubMed/NCBI
|