Introduction
For patients with locoregionally advanced
nasopharyngeal carcinoma (NPC), radiotherapy, chemotherapy and even
targeted therapy are widely accepted treatment options. These
treatments, although they mostly achieve locoregional tumor
control, they may also be associated with complex post-treatment
changes, such as edema, loss of tissue planes, fibrosis, mucositis
and scarring, which may interfere with the detection of local
recurrence and the response to therapy. However, timely detection
is crucial for deciding whether treatment modification or
discontinuation is required.
Case report
This is a presentation of the case of a 51-year-old
nasopharyngeal carcinoma patient with cervical nodal metastases
(CNM). Following radiotherapy, chemotherapy and targeted therapy,
multislice spiral enhanced computed tomography (CT), enhanced
magnetic resonance imaging (MRI) and
18F-fluorodeoxyglucose (FDG) positron emission
tomography (PET)/CT of the neck were performed to compare the
extent of the CNM. The enhanced CT and MRI images were
unremarkable, whereas the 18F-FDG PET/CT images revealed
the exact recurrence or remission. This case demonstrated that
18F-FDG PET/CT exhibits a better sensitivity and
specificity for evaluating the response to combined treatment
compared to CT and/or MRI. Furthermore, 18F-FDG PET/CT
plays an important role in adjusting the clinical therapy regimen.
The patient had presented with epistaxis and diminished hearing for
2 years. Complete remission was achieved following radiotherapy (70
Gy in 35 fractions over 7 weeks) and 6 cycles of chemotherapy
(tegafur 1,000 mg on days 1–5 and cisplatin 25 mg/m2 on
days 1–3 following radiotherapy) (Fig.
1A). The patient developed locoregional recurrences in the
right cervical lymph nodes after 13 months. Enhanced CT,
18F-FDG PET/CT and aspiration biopsy of the cervical
lymph nodes were performed. The enhanced CT images revealed the
disappearance of the lateral pharyngeal fossa and the extended
lateral pharyngeal wall, as well as the increased right cervical
lymph nodes (Fig. 1B).
18F-FDG PET/CT revealed a focal increase of glucose
metabolism [standardized uptake value (SUV)max, 9.15] of the right
cervical lymph nodes, sized 1.5×1.2 cm, which lay behind the
carotid artery (Fig. 1C). Lymph node
metastasis was confirmed by aspiration biopsy (Fig. 1D). Subsequently, chemotherapy was
administered by intravenous infusion, liposomal paclitaxel 175
mg/m2 on day 1 and carboplatin 400 mg/m2 on
day 1 every 4 weeks for four cycles. Subsequently, enhanced CT and
MRI were performed to evaluate the response to chemotherapy with
paclitaxel liposome and carboplatin (Fig.
1E and F). However, the changes on the images were
unremarkable. 18F-FDG PET/CT showed the glucose
metabolism (SUVmax, 12.15) of the right cervical lymph nodes, sized
2.0×1.7 cm, which was increased compared to that during the
previous examination (Fig. 1G),
reflecting tumor progression (1).
Accordingly, the chemotherapeutic regimen was modified to
gemcitabine hydrochloride 1,000 mg/m2 on days 1 and 8
and oxaliplatin 135 mg/m2 on day 1. In addition,
targeted therapy with nimotuzumab 200 mg was administered by
intravenous infusion prior to chemotherapy. Enhanced CT and MRI
were employed following chemotherapy combined with targeted therapy
for two cycles (Fig. 1H and I). In a
similar manner, distinct changes were not identified by CT and MRI.
However, 18F-FDG PET/CT (Fig.
1J) showed a significantly decreased glucose metabolism
(SUVmax, 2.0) of the right cervical lymph nodes, suggesting disease
remission (2, 3).
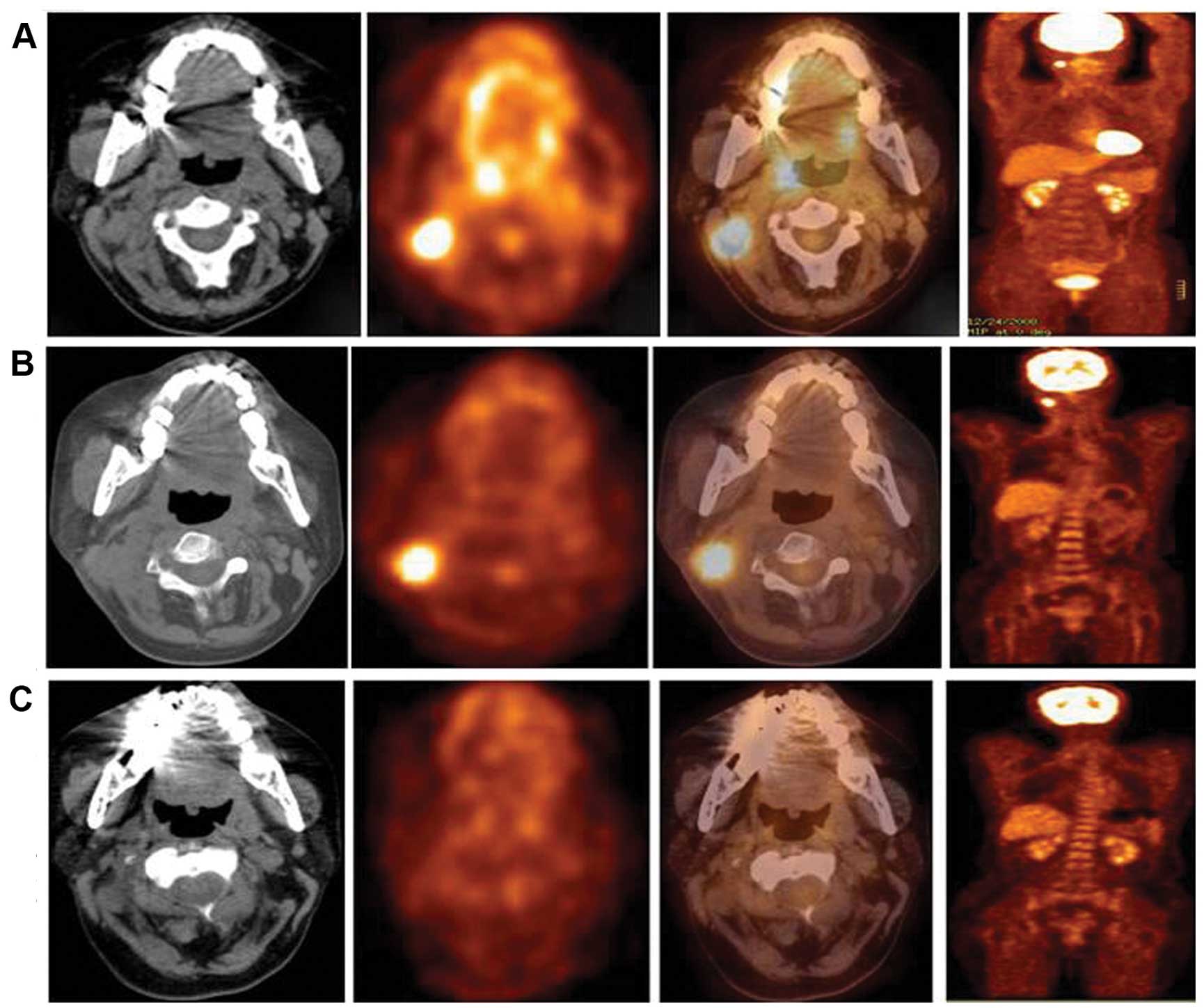
A comparison of the 18F-FDG PET/CT images
during the entire course of treatment is shown in Fig. 2. The 18F-FDG PET/CT images
prior to and following chemotherapy with liposomal paclitaxel and
carboplatin are shown in Fig. 2A and
B, respectively, whereas the 18F-FDG PET/CT image
following chemotherapy combined with targeted therapy is shown in
Fig. 2C.
Discussion
In the present case, local recurrence and the
response to treatment were difficult to evaluate on enhanced CT and
MRI, whereas 18F-FDG PET/CT is more likely to achieve an
accurate evaluation of the disease status. The causes are
following: CT and MRI are anatomical imaging modalities, which
analyze tumor tissues only on the basis of their morphological
appearance. Radiotherapy and chemotherapy may alter the normal
nasopharyngeal anatomy. Post-treatment-related edema, fibrosis,
inflammation and scarring are limiting factors in the diagnosis of
residual or recurrent NPC on CT and MRI (4–6). Not all
asymmetries of the nasopharyngeal mucosal outline, mass lesions and
abnormal enhancements or unusual signal changes in the CT or MRI
scans are signs of tumor recurrence (7). 18F-FDG PET/CT is a whole-body
imaging technique, capable of merging functional and morphological
information, which identifies viable tumors according to the higher
glycolytic rates exhibited by neoplasms compared to necrotic or
reactive tissue (8). Changes in
glucose metabolism are often evident before the appearance of a
physical change or symptom, which is crucial for the adjustment of
the therapeutic regimen. 18F-FDG PET/CT displays a high
sensitivity and a relatively high specificity in the evaluation of
recurrent NPC and the response to treatment (9, 10).
References
|
1
|
Nuñez RF, Yeung HW and Chisin R:
Fluorine-18 FDG positron emission tomography in advanced
nasopharyngeal carcinoma. Clin Nucl Med. 25:731–733. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Peng F, Rabkin G and Muzik O: Use of
2-deoxy-2-[F-18]-fluoro-D-glucose positron emission tomography to
monitor therapeutic response by rhabdomyosarcoma in children:
report of a retrospective case study. Clin Nucl Med. 31:394–397.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Klabbers BM, Lammertsma AA and Slotman BJ:
The value of positron emission tomography for monitoring response
to radiotherapy in head and neck cancer. Mol Imaging Biol.
5:257–270. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Mostafa E, Nasar MN, Rabie NA, et al:
Induction chemotherapy with paclitaxel and cisplatin, followed by
concomitant cisplatin and radiotherapy for the treatment of locally
advanced nasopharyngeal carcinoma. J Egypt Natl Canc Inst.
18:348–356. 2006.PubMed/NCBI
|
|
5
|
Kim YI, Han MH, Cha SH, et al:
Nasopharyngeal carcinoma: posttreatment changes of imaging
findings. Am J Otolaryngol. 24:224–230. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
King AD, Ma BB, Yau YY, et al: The impact
of 18F-FDG PET/CT on assessment of nasopharyngeal carcinoma at
diagnosis. Br J Radiol. 81:291–298. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
de Bondt RB, Nelemans PJ, Hofman PA, et
al: Detection of lymph node metastases in head and neck cancer: a
meta-analysis comparing US, USgFNAC, CT and MR imaging. Eur J
Radiol. 64:266–272. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Osmany S, Padhy AK and Ng DC: Detection of
thyroid metastases from nasopharyngeal carcinoma with F-18 FDG
PET/CT. Clin Nucl Med. 33:224–225. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Ong SC, Schöder H, Lee NY, et al: Clinical
utility of 18F-FDG PET/CT in assessing the neck after concurrent
chemoradiotherapy for locoregional advanced head and neck cancer. J
Nucl Med. 49:532–540. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Yao M, Smith RB, Hoffman HT, et al:
Clinical significance of postradiotherapy [18F]-fluorodeoxyglucose
positron emission tomography imaging in management of head-and-neck
cancer-a long-term outcome report. Int J Radiat Oncol Biol Phys.
74:9–14. 2009. View Article : Google Scholar : PubMed/NCBI
|