Introduction
Breast cancer is the most prevalent type of cancer
among women, affecting approximately one million women worldwide
(1). The development of breast cancer
is a complex, multistep process. Breast cancer is considered to be
a disease entity including different molecular subtypes with
distinct biological behavior profiles, which affect treatment
response and outcome. Accordingly, the biological classification of
breast tumors uses hormone receptor expression and human epidermal
growth factor receptor 2 (HER2) status with the aim to assess the
potential response to treatment. Luminal A tumors are associated
with the best prognosis among all breast cancer subtypes (2).
Over the last decade, the identification of small,
non-coding RNA molecules, namely the microRNAs (miRNAs), has
attracted considerable attention due to the accumulating evidence
regarding their relevant regulatory functions on cancer initiation,
proliferation and progression to a more aggressive phenotype. The
interactions between miRNAs and their target mRNAs, usually within
the 3′-untranslated region of the target genes, results in the
degradation and/or translational inhibition of these genes.
Approximately 1,000 miRNA genes are encoded in the human genome
(3) and a total of 1,600 precursors
and 2,042 mature miRNAs have been identified according to miRBase
(http://www.mirbase.org/cgi-bin/browse.pl?org=hsa).
miRNAs have great potential as biomarkers for cancer
detection due to their remarkable stability in the blood. Recent
data indicated that, in addition to their regulatory function,
miRNAs may play a predictive role in evaluating the response to
therapy (4,5). Several studies reported the use of
circulating miRNAs as biomarkers of disease and therapy response
and as diagnostic and prognostic markers in breast cancer (6). Studies investigating the expression of
miRNA molecules in breast cancer have revealed their significance
as potential markers in tumor classification (7,8). It has
even been suggested that circulating miRNAs may be specific
biomarkers for breast cancer screening (9).
The development of sensitive, non-invasive markers
in the blood circulation may facilitate early detection, monitoring
of tumor progression and treatment response in patients with breast
cancer. Free nucleic acids in the serum of cancer patients were
first reported in 1977 by Leon et al (10). For this reason, free nucleic acids and
oligonucleotides, such as miRNAs, have recently attracted attention
in the field of cancer research.
Recent studies indicated that miR-34a is one of the
key miRNA molecules with a tumor suppressor function, suggesting
that it may play a role in DNA damage repair through inducing cell
cycle arrest and apoptosis. The targets of miR-34 include cyclin
D1, cyclin-dependent kinase 6, E2F transcription factor 3 and myc
genes (11,12). miR-145 is another miRNA with tumor
suppressor function, playing a role in suppressing cancer cell
invasion and metastasis (13,14). miR-21 has been associated with an
oncogenic potential and poor outcome in cancer (15,16). It
has been suggested that miR-21 is directly involved in regulating
apoptosis in breast cancer cells (17–19).
miR-221 is another oncogenic miRNA, which is involved in the
induction of angiogenesis and resistance to tamoxifen (5,20). In
addition, upregulation of miR-10b has been reported in breast
cancer and has been correlated with invasion, metastatic capacity
and progression (21,22).
In this study, we analyzed the plasma levels of
breast cancer-associated miRNAs (miR-21, −145, −34a, −10b and −221)
during adjuvant chemotherapy in patients with luminal A breast
cancer, in order to identify miRNA molecules that are
differentially expressed in response to chemotherapy.
Patients and methods
Patients
A total of 52 patients with primary breast cancer
who were treated at the Oncology Institute, University of Istanbul
(Istanbul, Turkey), were included in the study. To ensure that all
the tumors exhibited the same biological characteristics, only
patients with luminal A tumors were included in the study. Patients
with stage I–III cancers were primarily treated with conservative
surgery or mastectomy. Tumor staging was performed according to the
American Joint Committee on Cancer TNM classification and the pTNM
was determined following pathological examination. Patients with
metastatic disease and other previous tumors were excluded from the
study. İmmunohistochemical screening for estrogen receptors,
progesterone receptors and HER2 status was performed on
formalin-fixed paraffin-embedded tissue samples. The serum samples
were obtained prior to the initiation and following completion of
the adjuvant chemotherapy. Data regarding patient demographics,
histology, receptor status, type of surgical treatment and adjuvant
therapy were obtained by reviewing the patients' medical records.
This study was approved by the local Ethics Committee of Istanbul
University.
RNA isolation
All sera were immediately stored at −80°C until RNA
isolation. Circulating RNA molecules were isolated from the sera
using the TriPure isolation reagent (Roche Diagnostics GmbH,
Mannheim, Germany). Briefly, a 200-µl sample was mixed with 800 µl
of TriPure reagent and the mixture was incubated at room
temperature for complete dissociation of the nucleoprotein
complexes. Following incubation, 0.2 ml chloroform was added to
each sample and incubated at room temperature for 15 min. Following
centrifugation at 12,000 × g for 15 min, the RNA phase was
transferred into Eppendorf tubes and 0.5 ml isopropanol was added.
The mixture was incubated at room temperature for 10 min and
centrifuged at 12,000 × g for 10 min. The supernatant was
discarded, the RNA-containing pellet was washed with 75% ethanol
and centrifuged at 7,500 × g for 5 min. The supernatant was
removed, air-dried and resuspended in RNAse-free water. The
RNA-containing sample was incubated at 55–60°C for 15 min and
stored in −80°C until usage.
Conversion of total RNA into
complementary DNA (cDNA)
cDNA was synthesized using the miScript Reverse
Transcription kit (Qiagen, Valencia, CA, USA) according to the
instructions of the manufacturer. cDNA synthesis was performed at
37°C for 60 min and the reaction was inactivated by incubation at
95°C for 5 min.
Quantitative polymerase chain reaction
(qPCR)
To quantitate the miRNA molecules, the miScript
Primer Assay (Qiagen) was used, which includes a universal primer
specific to the poly-A tail and a miRNA-specific primer. Selected
miRNA primers were obtained from the miScript Primer Assay, as
presented in Table I. SYBR®-Green
(Qiagen) was used as the fluorescent molecule. The amplified PCR
product had a size of ~80 bp. The miR-16 molecule was used as a
reference for normalization of the expression levels of the miR
panel. qPCR was performed using the LightCycler 480 (Roche
Diagnostics GmbH). The PCR program included a fast start step of 15
min at 95°C, followed by 45 cycles of amplification, with each
cycle consisting of denaturation at 94°C for 15 sec, annealing at
55°C for 30 sec and elongation at 70°C for 30 sec. A relative
quantification determined the ratio between the amount of target
miRNA and reference amplicon. Melting curve analyses were performed
to verify the specifity and identity of the PCR products.
 | Table I.List of microRNAs used in the
experiment. |
Table I.
List of microRNAs used in the
experiment.
| Assay name | Qiagen cat. no. | miRBase accession
no. |
|---|
| Hs_miR-145_1_1 | MS00003528 | MIMAT0000437 |
| Hs_miR-21_2 | MS00009079 | MIMAT0000076 |
miR-21 was detected in paired samples from 32
patients, while miR-145 was analyzed in paired samples from 49
patients. Under identical experimental conditions, the remaining
miRNAs exhibited very low levels and were detected only in a very
small number of samples; therefore, they were not included in the
statistical analyses.
Statistical analysis
We compared the plasma levels of miR-21 and miR-145
between the pre- and post-treatment samples of each patient. The
statistical analysis was performed using the Mann-Whitney U test.
P<0.05 was considered to indicate a statistically significant
difference. The association of miR-21 and miR-145 expression with
clinical stage was evaluated by the Wilcoxon signed-ranks test.
Results
Clinicopathological
characteristics
The main clinicopathological characteristics of the
patients in our series were as follows: The mean age was 47.7
years. Stage I was reported in 3 (5.8%), stage II in 33 (63.4%) and
stage III in 16 patients (30.8%). All the patients underwent
surgery: Conservative surgery was performed in 28 (53.8%) and
mastectomy was performed in 24 patients (46.1%). The hormone
receptor status was positive and the HER2 status was negative in
all the patients. Radiotherapy was delivered to 44 patients
(84.6%). Adjuvant chemotherapy was administered to all patients: A
total of 15 patients (28.9%) received anthracycline-based therapy,
1 patient (1.9%) received taxane-based therapy and 36 patients
(69.2%) received anthracycline and taxane-based regimens. Endocrine
therapy was administered to 51 of the 52 patients (98.0%) (Table II).
 | Table II.Characteristics of breast cancer
patients. |
Table II.
Characteristics of breast cancer
patients.
| Characteristics | Patient no. (%)
(n=52) |
|---|
| Age, years |
|
| Mean | 47.7 |
|
Median | 46 |
| Stage |
|
| I | 3 (5.8) |
| II | 33 (63.4) |
| III | 16 (30.8) |
| Surgery |
|
|
Conservative surgery | 28 (53.8) |
|
Mastectomy | 24 (46.2) |
| Radiotherapy
treatment | 44 (84.6) |
| Chemotherapy
treatment regimens |
|
|
Anthracycline-based | 15 (28.9) |
|
Taxane-based | 1 (1.9) |
|
Anthracyclin and
taxane-based | 36 (69.2) |
| Endocrine
therapy | 51 (98.0) |
Pre- and post-treatment plasma levels
of miR-21 and miR-145
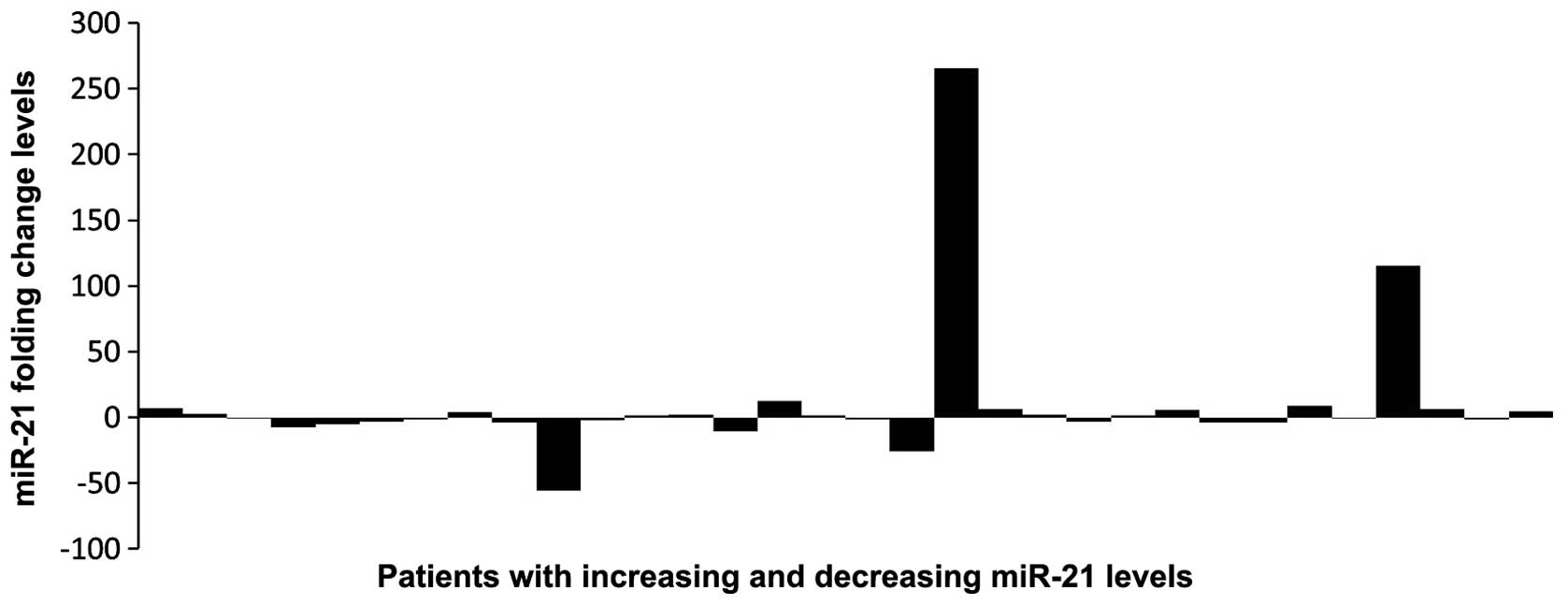
The plasma levels of miR-21 and miR-145 were
measured in matched pre- and post-treatment samples of the
patients. In the pre-treatment samples, the relative median levels
of miR-21 and miR-145 were 0.1 and 3.84, respectively, while in the
post-treatment samples the values were 0.12 and 3.08, respectively
(Figs. 1 and 2). The differences between pre- and
post-treatment samples were not statistically significant
(P>0.05). Following chemotherapy, the plasma levels of miR-21
increased in 17 and decreased in 15 patients, when compared with
pre-treatment levels. miR-145 expression was higher following
chemotherapy in 20 patients, while it declined in the remaining 29
patients (Figs. 3 and 4).
Plasma levels of miR-21 and miR-145
according to stage
We next compared miRNA levels according to clinical
stage. Significantly higher levels of miR-21 were observed in
post-treatment plasma samples from patients with stage III disease
(P=0.04). In this subgroup, we also observed a decrease in miR-145
expression, although the difference was not statistically
significant (P=0.06). In the evaluation of serum miRNA levels
according to stage, the decline in stage III patients was
significant compared with that in stage I+II patients (P=0.006)
(Table III).
 | Table III.Serum miR-21 and miR-145 levels
according to stage. |
Table III.
Serum miR-21 and miR-145 levels
according to stage.
|
| Stage I+II | Stage III |
|
|---|
|
|
|---|
| Variables | Median | Median | aP-value |
|---|
| miR-21 |
|
| 0.006 |
|
Pre-treatment | 0.105 | 0.007 |
|
|
Post-treatment | 0.092 | 0.381 |
|
|
bP-value | >0.05 | 0.04 |
|
| miR-145 |
|
| >0.05 |
|
Pre-treatment | 3.5 | 6.52 |
|
|
Post-treatment | 2.73 | 3.08 |
|
|
bP-value | >0.05 | >0.05 |
|
Discussion
miRNAs in the circulation may serve as biomarkers
for cancer detection. It remains unclear how tumor-associated
miRNAs enter the circulation. It has been suggested that tumor
miRNAs may be present in circulation as a consequence of tumor cell
death and lysis (23).
In this study, we evaluated pre- and post-treatment
plasma levels of five miRNAs (miR-21, −145, −34a, −10b and −221) in
patients with luminal A breast cancer undergoing adjuvant
chemotherapy. The miR-10b, −34a and-221 could not be analyzed, as
their serum levels were very low and several paired samples could
not be matched.
In unselected patients, we observed no significant
differences between pre- and post-treatment levels of miR-21 and
−145. However, in patients with initial stage III tumors, the
miR-21 plasma levels were found to be significantly increased
following treatment. This finding indicates that
chemotherapy-induced cancer cell apoptosis may contribute to
increased circulating levels of miR-21. Aberrant expression of
miR-21 in breast cancer has been previously reported (17–19,24).
miR-21 has been found to be highly expressed in breast tumors
compared with its expression in matched normal breast tissues,
suggesting that miR-21 may play a significant role in tumorigenesis
(25). A previous study on colorectal
cancer, which indicated that increased miR-21 expression may
represent a marker of poor prognosis, supports this finding
(26).
miR-145 is considered to act as a tumor suppressor
and has been shown to be downregulated in breast cancer. The
expression levels of mature miR-21 and mature miR-145 were found to
be higher in esophageal squamous cell carcinoma compared with those
in the normal epithelium (27).
Significantly reduced miR-145 expression was also reported in
atypical and anaplastic tumors compared with benign meningiomas
(28). In prostate cancer, miR-145, a
direct target of p53, represses bone metastasis and is involved in
regulating epithelial-to-mesenchymal transition (EMT) and cancer
cell stemness. Recent data suggest that loss of wild-type p53 may
promote bone metastasis of prostate cancer, at least partially
through repressing miR-145, promote EMT and stemness of cancer
cells (29). As stated above, we
would have expected increased miR-145 levels following
chemotherapy, but the miR-145 levels were in fact decreased.
To the best of our knowledge, this is the first
study investigating the plasma levels of miR-21 and miR-145 in pre-
and post-treatment breast cancer samples. Our results demonstrated
that miR-21 expression is significantly higher in post-treatment
plasma samples from patients with stage III tumors. These data
support the fact that chemotherapy-induced apoptosis may contribute
to increased circulating miRNA levels, including miR-21.
Acknowledgements
This study was supported by the Istanbul University
Research Fund (project no. 17143).
References
|
1
|
Jemal A, Siegel R, Xu J and Ward E: Cancer
statistics, 2010. CA Cancer J Clin. 60:277–300. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Chuthapisith S, Permsapaya W, Warnnissorn
M, Akewanlop C, Sirivatanauksorn V and Prasarttong Osoth P: Breast
cancer subtypes identified by the ER, PR and HER-2 status in Thai
women. Asian Pac J Cancer Prev. 13:459–462. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Fu SW, Chen L and Man YG: miRNA biomarkers
in breast cancer detection and management. J Cancer. 2:116–122.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Salter KH, Acharya CR, Walters KS, et al:
An intergrated approach to the prediction of chemotherapeutic
response in patients with breast cancer. PLoS One. 3:e19082008.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Miller TE, Ghoshal K, Ramaswamy B, Roy S,
Datta J, Shapiro CL, Jacob S and Majumder S: MicroRNA-221/222
confers tamoxifen resistance in breast cancer by targeting p27Kip1.
J Biol Chem. 283:29897–29903. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Cortez MA, Welsh JW and Calin GA:
Circulating microRNAs as noninvasive biomarkers in breast cancer.
Recent Results Cancer Res. 195:151–161. 2012.PubMed/NCBI
|
|
7
|
Yan LX, Huang XF, Shao Q, Huang MY, Deng
L, Wu QL, Zeng YX and Shao JY: MicroRNA miR-21 overexpression in
human breast cancer is associated with advanced clinical stage,
lymph node metastasis and patient poor prognosis. RNA.
14:2348–2360. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Chen J, Wang BC and Tang JH: Clinical
significance of microRNA-155 expression in human breast cancer. J
Surg Oncol. 106:260–266. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Ng EK, Li R, Shin VY, et al: Circulating
microRNAs as specific biomarkers for breast cancer detection. PLoS
One. 8:e531412013. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Leon SA, Shapiro B, Sklaroff DM and Yaros
MJ: Free DNA in the serum of cancer patients and the effect of
therapy. Cancer Res. 37:646–650. 1977.PubMed/NCBI
|
|
11
|
Sun F, Fu H, Liu Q, Tie Y, Zhu J, Xing R,
Sun Z and Zheng X: Downregulation of CCND1 and CDK6 by miR-34a
induces cell cycle arrest. FEBS Lett. 582:1564–1568. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Welch C, Chen Y and Stallings RL:
MicroRNA-34a functions as a potential tumor suppressor by inducing
apoptosis in neuroblastoma cells. Oncogene. 26:5017–5022. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Sachdeva M, Zhu S, Wu F, Wu H, Walia V,
Kumar S, Elble R, Watabe K and Mo YY: p53 represses c-Myc through
induction of the tumor suppressor miR-145. Proc Natl Acad Sci USA.
106:3207–3212. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Lei P, Xie J, Wang L, Yang X, Dai Z and Hu
Y: microRNA-145 inhibits osteosarcoma cell proliferation and
invasion by targeting ROCK1. Mol Med Rep. 10:155–160.
2014.PubMed/NCBI
|
|
15
|
Song B, Wang C, Liu J, Wang X, Lv L, Wei
L, Xie L, Zheng Y and Song X: MicroRNA-21 regulates breast cancer
invasion partly by targeting tissue inhibitor of metalloproteinase
3 expression. J Exp Clin Cancer Res. 29:292010. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Nair VS, Maeda LS and Ioannidis JP:
Clinical outcome prediction by microRNAs in human cancer: A
systematic review. J Natl Cancer Inst. 104:528–540. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Frankel LB, Christoffersen NR, Jacobsen A,
Lindow M, Krogh A and Lund AH: Programmed cell death 4 (PDCD4) is
an important functional target of the microRNA miR-21 in breast
cancer cells. J Biol Chem. 283:1026–1033. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Qi L, Bart J, Tan LP, Platteel I, Sluis T,
Huitema S, Harms G, Fu L, Hollema H and Berg A: Expression of
miR-21 and its targets (PTEN, PDCD4, TM1) in flat epithelial atypia
of the breast in relation to ductal carcinoma in situ and invasive
carcinoma. BMC Cancer. 9:1632009. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Zhu S, Wu H, Wu F, Nie D, Sheng S and Mo
YY: MicroRNA-21 targets tumor suppressor genes in invasion and
metastasis. Cell Res. 18:350–359. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Le Bot N: MicroRNAs in angiogenesis. Nat
Cell Biol. 14:3422012. View
Article : Google Scholar
|
|
21
|
Han X, Yan S, Weijie Z, Feng W, Liuxing W,
Mengquan L and Qingxia F: Critical role of miR-10b in transforming
growth factor-β1-induced epithelial-mesenchymal transition in
breast cancer. Cancer Gene Ther. 21:60–67. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Ma L, Teruya-Feldstein J and Weinberg RA:
Tumour invasion and metastasis initiated by microRNA-10b in breast
cancer. Nature. 449:682–688. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Heneghan HM, Miller N, Lowery AJ, Sweeney
KJ, Newell J and Kerin MJ: Circulating microRNAs as novel minimally
invasive biomarkers for breast cancer. Ann Surg. 251:499–505. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Iorio MV, Ferracin M, Liu CG, et al:
MicroRNA gene expression deregulation in human breast cancer.
Cancer Res. 65:7065–7070. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Si ML, Zhu S, Wu H, Lu Z, Wu F and Mo YY:
miR-21-mediated tumor growth. Oncogene. 26:2799–2803. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Shibuya H, Iinuma H, Shimada R, Horiuchi A
and Watanabe T: Clinicopathological and prognostic value of
microRNA-21 and microRNA-155 in colorectal cancer. Oncology.
79:313–320. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Akagi I, Miyashita M, Ishibashi O, Mishima
T, Kikuchi K, Makino H, Nomura T, Hagiwara N, Uchida E and Takizawa
T: Relationship between altered expression levels of MIR21, MIR143,
MIR145 and MIR205 and clinicopathologic features of esophageal
squamous cell carcinoma. Dis Esophagus. 24:523–530. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Kliese N, Gobrecht P, Pachow D, et al:
miRNA-145 is downregulated in atypical and anaplastic meningiomas
and negatively regulates motility and proliferation of meningioma
cells. Oncogene. 32:4712–4720. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Ren D, Wang M, Guo W, Zhao X, Tu X, Huang
S, Zou X and Peng X: Wild-type p53 suppresses the
epithelial-mesenchymal transition and stemness in PC-3 prostate
cancer cells by modulating miR-145. Int J Oncol. 42:1473–1481.
2013.PubMed/NCBI
|