Introduction
Recent progress in the treatment of malignant tumors
has improved patient survival. The improved prognosis, however, has
increased the number of patients with metastatic bone tumors.
Surgical and radiation therapy interventions to treat metastatic
bone tumors are complicated by a highly variable clinical course.
The precise roles of surgery and radiation therapy remain undefined
and cannot be resolved unless prognosis-related factors are
elucidated. Scoring systems may help physicians predict the
prognosis of patients with bone metastases and provide a practical
tool for clinicians to facilitate treatment selection.
In 2013, Ratasvuori et al (1) described a prognosis scoring system for
1,195 surgically-treated patients with skeletal metastases in the
extremities that was based on the Scandinavian Sarcoma Group (SSG)
Skeletal Metastasis Registry (SSG score); in 2005, Katagiri et
al (2) described a prognosis
scoring system based on the data from 350 surgically or
non-surgically treated patients with skeletal metastases (Katagiri
score); in 2005, Tokuhashi et al (3) described a prognosis scoring system that
was based on data from 164 patients with spinal metastases who were
surgically or non-surgically treated (Tokuhashi score); and in
2008, Mizumoto et al (4)
reported yet another prognosis scoring system based on data from
544 patients with spinal column metastases who had been treated
with radiotherapy (Mizumoto score).
For the present study, we collected data from all
patients with bone metastases who were treated at the Department of
Orthopaedic Surgery, Kagoshima University Hospital, which is the
only teaching hospital in Kagoshima province, Japan. Almost all
patients with metastatic bone tumors who reside in this area are
referred to our department. We evaluated the four reported scoring
systems in regard to our patient population to determine which was
the most suitable for our patients with bone metastases.
Patients and methods
Patients
A total of 6,539 cancer patients were registered in
the Kagoshima University cancer registry between 2007 and 2011; 209
patients had bone metastases. In this retrospective study, we
reviewed the medical records and images of 145 patients with
metastatic bone tumors who were referred to the Department of
Orthopaedic Surgery, Kagoshima University Hospital between 2007 and
2011 as previously reported (5). The
patients included 81 men and 64 women with a mean age of 65 years
(range, 29–87 years). The mean follow-up was 10 months. Two
well-trained radiologists reviewed all bone scans. The bone scan
results were compared with radiographs, computed tomography scans,
or magnetic resonance images, taking into account the patient's
clinical symptoms. Any positive findings were considered as bone
metastases.
We collected data on the age and gender of the
patient, the primary tumor, site(s) and number of metastases,
presence of other metastases, type of surgery, performance status
(2,6),
complications, previous chemotherapy, Frankel classification
(7) and presence of hypercalcemia
(>10 mg/dl). Overall survival was defined as the time interval
between the date the first skeletal metastasis was diagnosed and
the date of death, or the date when the patient was last known to
be alive. The study protocol was approved by the Ethics Committee
on Clinical Research at Kagoshima University Hospital.
Statistical analysis
Differences in the categorical variables between
each scoring system and the data from our hospital were analyzed by
the Fisher's exact or Mann-Whitney U test. Kaplan-Meier analysis
was performed to illustrate the time to death. The significance of
all Kaplan-Meier analyses were tested by log-rank analysis.
Statistical analyses were performed using Excel statistics 2012
(Social Survey Research Information Co., Ltd. Tokyo, Japan).
Results
Evaluation of prognosis by the SSG
survival scoring system
Data were collected from 145 patients with skeletal
metastases regarding prognosis, number of skeletal metastases,
presence of organ metastasis, primary lesion and Karnofsky score
(6) according to the SSG survival
scoring (1). The demographic data for
each prognostic factor from Kagoshima University and the SSG report
are summarized in Table IA. We
performed the Fisher's exact test to assess any significant
differences between the Kagoshima University and SSG data sets. All
the sets differed significantly with respect to the presence of
organ metastasis (P<0.01), primary tumor (breast, kidney,
thyroid, myeloma, or lymphoma vs. other cancers, P<0.01),
Karnofsky score (≥70 vs. <70, P<0.01) and number of skeletal
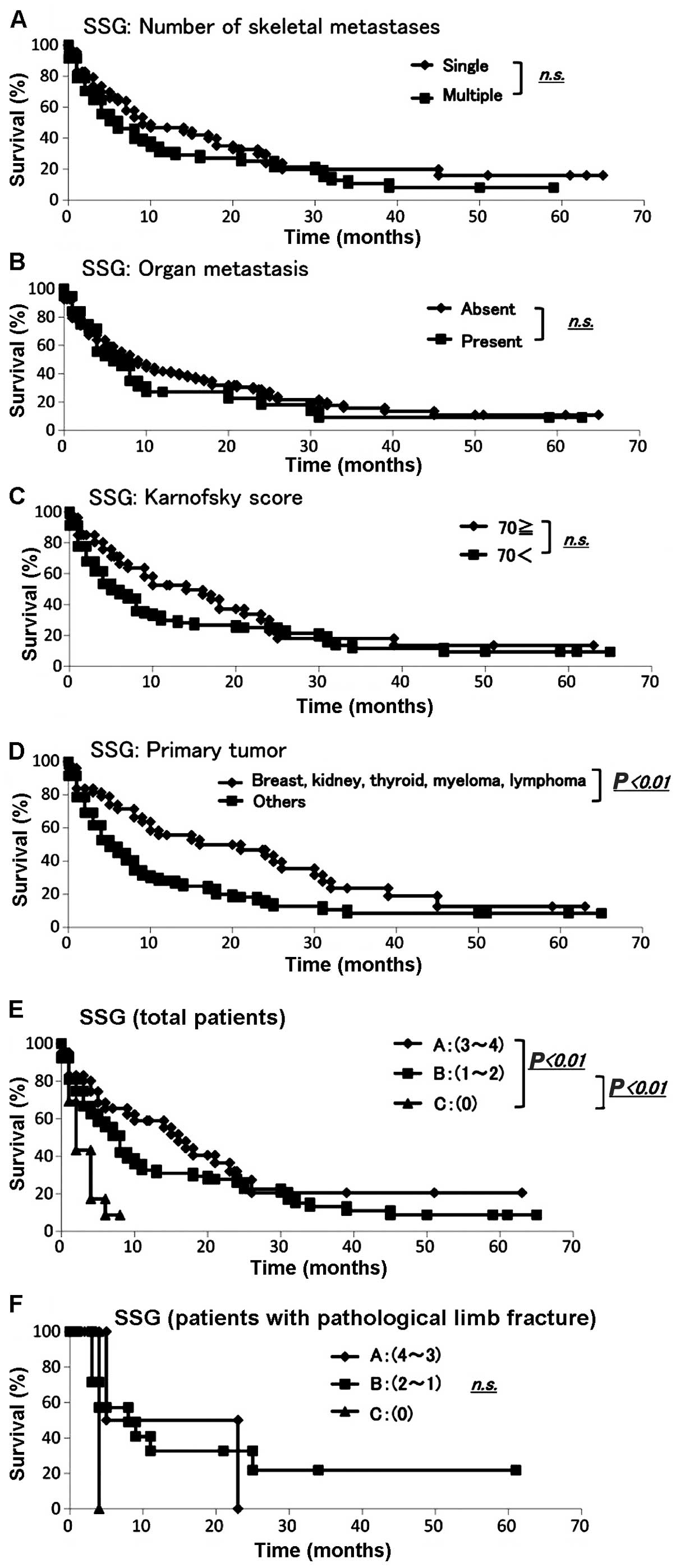
metastases (single or multiple, P<0.01) (Table IA). The Kaplan-Meier analysis and
log-rank analysis revealed that none of the other variables (apart
from the primary tumor) was a significant prognostic factor
(Fig. 1A–D).
 | Table I.Distribution and prognosis of patients
for each score of SSG survival scoring system. |
Table I.
Distribution and prognosis of patients
for each score of SSG survival scoring system.
| A, Distribution of
prognostic factors |
|
|
|
|
|---|
|
|---|
| Prognostic
factors |
| Kagoshima | SSG | P-valuea |
|---|
| Skeletal
metastasis |
|
|
| <0.01 |
|
Single |
| 65 | 146 |
|
|
Multiple |
| 80 | 505 |
|
| Organ metastasis |
|
|
| <0.01 |
|
Absent |
| 107 | 384 |
|
|
Present |
| 38 | 267 |
|
| Primary tumor |
|
|
| <0.01 |
| Breast,
kidney, thyroid, myeloma, lymphoma |
| 51 | 360 |
|
|
Other |
| 94 | 291 |
|
| Karnofsky score |
|
|
| <0.01 |
| ≥70 |
| 26 | 338 |
|
|
<70 |
| 119 | 313 |
|
| Impending
fracture |
| 122 | 156 | <0.01 |
| Pathological
fracture |
| 23 | 495 |
|
| SSG survival
score |
|
|
|
|
| Group A,
3–4 |
| 42 | N/A |
|
| Group B,
1–2 |
| 90 | N/A |
|
| Group C,
0 |
| 13 | N/A |
|
|
| B, SSG survival
scoring |
|
|
|
|
|
| Prognostic
factors | Points | Sum | Groups | Estimated survival
(months) |
|
| Skeletal
metastasis |
|
|
| >12 |
|
Single | 1 |
|
|
|
|
Multiple | 0 | 4 | A |
|
| Organ metastasis |
|
|
| 3–6 |
|
Absent | 1 | 3 |
|
|
|
Present | 0 | 2 | B |
|
| Breast, kidney,
thyroid, myeloma, lymphoma |
|
|
| <3 |
| Yes | 1 | 1 |
|
|
| No | 0 | 0 | C |
|
| Karnofsky score |
|
|
|
|
| ≥70 | 1 |
|
|
|
|
<70 | 0 |
|
|
|
|
| C, SSG scoring |
|
|
|
|
|
| Prognostic
score | Months | Survival rate
(%) | 95% CI |
|
| Group A, 3–4 | 3 | 80.2 | 0.69–0.93 |
|
| 6 | 65.5 | 0.50–0.81 |
|
| 12 | 59.0 | 0.43–0.75 |
|
| 24 | 27.4 | 0.10–0.44 |
| Group B, 1–2 | 3 | 66.7 | 0.56–0.77 |
|
| 6 | 55.5 | 0.44–0.67 |
|
| 12 | 32.6 | 0.21–0.44 |
|
| 24 | 26.0 | 0.15–0.37 |
| Group C, 0 | 3 | 43.3 | 0.15–0.71 |
|
| 6 |
8.7 | 0.00–0.25 |
The SSG survival scoring system was applied to the
validation set (Table IB) (1). The SSG scoring system divides patients
into groups A, B and C (Table IB).
The Kaplan-Meier analysis demonstrated that groups A and C and
groups B and C had significantly different prognoses (Fig. 1E). Among the patients in group A,
80.2% survived for 3 months and 59.0% survived for >12 months.
Among the patients in group B, 55.5% survived for >6 months.
Among the patients in group C, 43.3% survived for 3 months and 8.7%
for 6 months (Table IC). The SSG
survival scoring was based on the Scandinavian Skeletal Metastasis
Registry for patients with surgically treated, skeletal metastases
of the extremities.
The SSG survival scoring was then applied to the
data set for our patients who had been surgically treated for
skeletal metastases of the extremities. The demographic data for
the scoring groups from Kagoshima University are summarized in
Table II. The Kaplan-Meier analysis
and log-rank analysis demonstrated that there were no significant
differences in prognosis between groups (Fig. 1F).
 | Table II.Evaluation by the SSG survival
scoring system for patients with fracture operation. |
Table II.
Evaluation by the SSG survival
scoring system for patients with fracture operation.
|
| Patients with
fracture operation |
|---|
|
|
|
|---|
| Scoring,
points | Kagoshima | SSG |
|---|
| Group A, 3–4 | 42 | N/A |
| Group B, 1–2 | 90 | N/A |
| Group C, 0 | 13 | N/A |
Evaluation of prognosis by the
Katagiri score
We collected data from all 145 patients with
skeletal metastasis regarding prognosis, primary lesion, presence
of visceral and cerebral metastases, performance status (2), history of previous chemotherapy and
number of skeletal metastases according to the Katagiri score
(2). The demographic data for each
prognostic factor from Kagoshima University and Katagiri et
al (2) are summarized in Table IIIA. To determine whether there were
any significant differences between the Kagoshima University and
Katagiri score data sets, we performed the Fisher's exact or
Mann-Whitney U test. The sets significantly differed with respect
to the presence of visceral and cerebral metastasis, performance
status (4 and 3 vs. 2 and 1) and the number of skeletal metastases
(single or multiple) (all P-values <0.01). The sets did not
differ significantly with respect to the primary lesion or history
of previous chemotherapy (Table
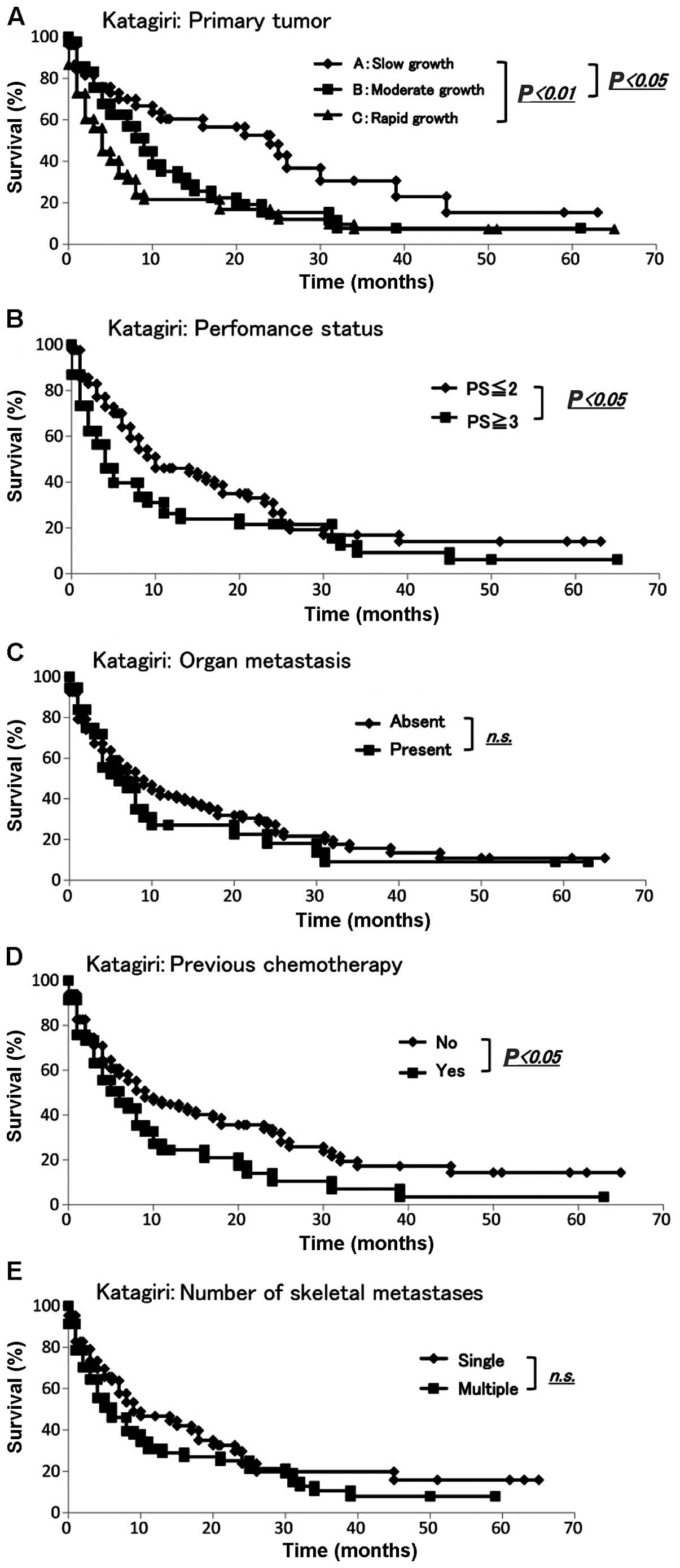
IIIA). The Kaplan-Meier and log-rank analyses revealed that
slow growth and moderate or rapid growth were significantly
different (P<0.05 and P<0.01, respectively) (Fig. 2A). Additionally, the Kaplan-Meier and
log-rank analyses demonstrated that performance status (≤2 vs. ≥3)
and history of previous chemotherapy exhibited significant
differences (P<0.05) (Fig. 2B and
D). None of the remaining variables was a significant
prognostic factor (Fig. 2C and
E).
 | Table III.Distribution of patients for each
score of the Katagiri scoring system. |
Table III.
Distribution of patients for each
score of the Katagiri scoring system.
| A, Proportion of
patients |
|
|
|
|---|
|
|---|
| Prognostic
factors | Kagoshima | Katagiri
(2005) | P-value |
|---|
| Primary
lesiona |
|
| 0.65b |
| Rapid
growth | 52 | 132 |
|
|
Moderate growth | 42 | 74 |
|
| Slow
growth | 51 | 144 |
|
| Visceral and
cerebral metastasis |
|
|
<0.01c |
|
Yes | 37 | 178 |
|
| No | 108 | 172 |
|
| Performance status
(ECOG) |
|
|
<0.01c |
| 3 or
4 | 61 | 219 |
|
| 1 or
2 | 84 | 131 |
|
| Previous
chemotherapy |
|
| 0.47c |
|
Yes | 46 | 108 |
|
| No | 99 | 241 |
|
| Skeletal
metastases |
|
|
<0.01c |
|
Multiple | 80 | 238 |
|
|
Single | 65 | 112 |
|
|
| B, Katagiri
scoring |
|
|
|
|
| Scoring | All patients
Kagoshima | All patients
Katagiri (2005) | P-value |
|
| 0–2 | 31 | 23 |
<0.01b |
| 3–5 | 54 | 67 |
|
| 6–8 | 60 | 156 |
|
|
| C, Katagiri
scoring |
|
|
|
|
| Prognostic
score | Months | Survival rate
(%) | 95% CI |
|
| 0–2 points | 3 | 78.0 | 0.66–0.90 |
|
| 6 | 69.7 | 0.56–0.84 |
|
| 12 | 66.5 | 0.52–0.81 |
|
| 24 | 38.2 | 0.20–0.57 |
| 3–5 points | 3 | 63.5 | 0.52–0.75 |
|
| 6 | 52.0 | 0.40–0.64 |
|
| 12 | 29.0 | 0.17–0.41 |
|
| 24 | 21.8 | 0.11–0.33 |
| 6–8 points | 3 | 64.5 | 0.45–0.84 |
|
| 6 | 29.8 | 0.10–0.49 |
|
| 12 | 13.2 | 0.00–0.29 |
|
| 24 | 6.61 | 0.00–0.19 |
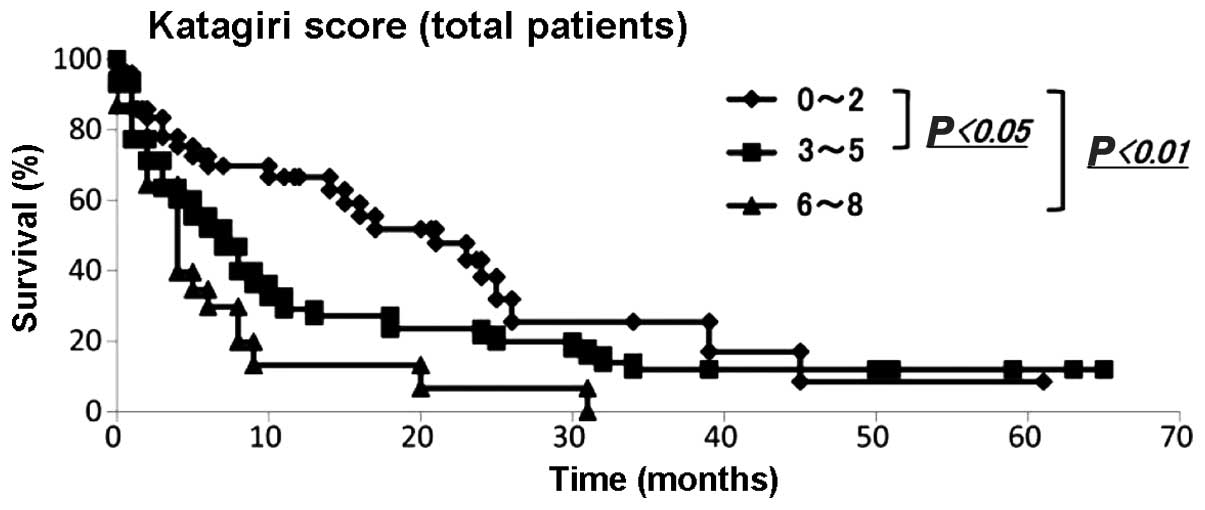
We then applied the Katagiri scoring system to our
data. The demographic data of each score from the Kagoshima
University and Katagiri et al (2) are summarized in Table IIIB. The Mann-Whitney U test
demonstrated that the distributions of each score were
statistically significant (P<0.01). The Kaplan-Meier and
log-rank analyses revealed that patients with 0–2 and 3–5 points
had significantly different prognoses from those with 0–2 and 6–8
points (P<0.05 and <0.01, respectively) (Fig. 3). Among the patients with 0–2 points,
78.0, 69.7, 66.5 and 38.2% survived for 3, 6, 12 and 24 months,
respectively. Among patients with 3–5 points, 63.5, 52.0, 29.0 and
21.8% survived for 3, 6, 12 and 24 months, respectively. Among
patients with 6–8 points, 64.5, 29.8, 13.2 and 6.6% survived for 3,
6, 12 and 24 months, respectively (Table IIIC).
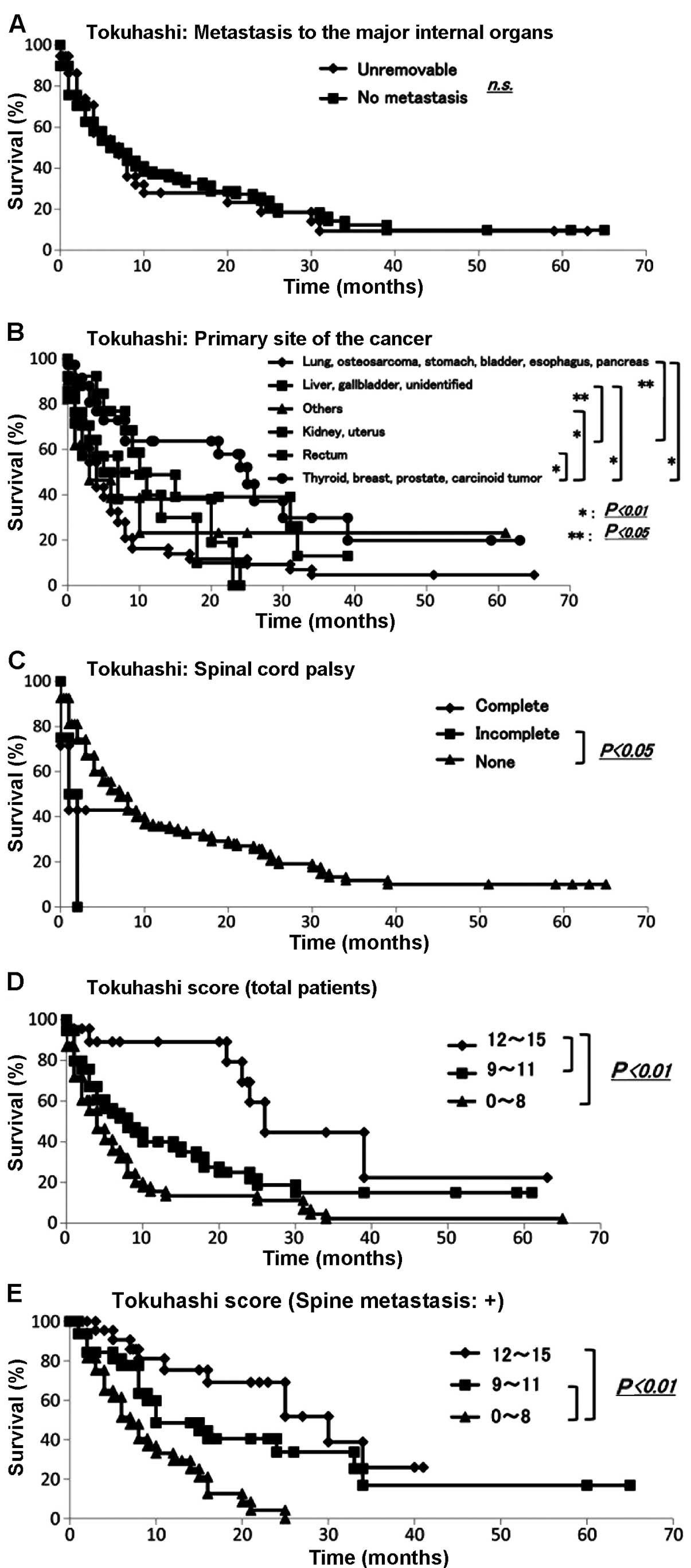
Evaluation of prognosis by the
Tokuhashi score
We collected data for all 145 skeletal metastasis
patients regarding prognosis, performance status (6), number of extraspinal bone metastases,
number of metastases in the vertebral body, presence or absence of
metastases to major internal organs, site of the primary lesion and
severity of palsy (7) according to
the Tokuhashi score (3). The
demographic data for each prognostic factor from Kagoshima
University are summarized in Table
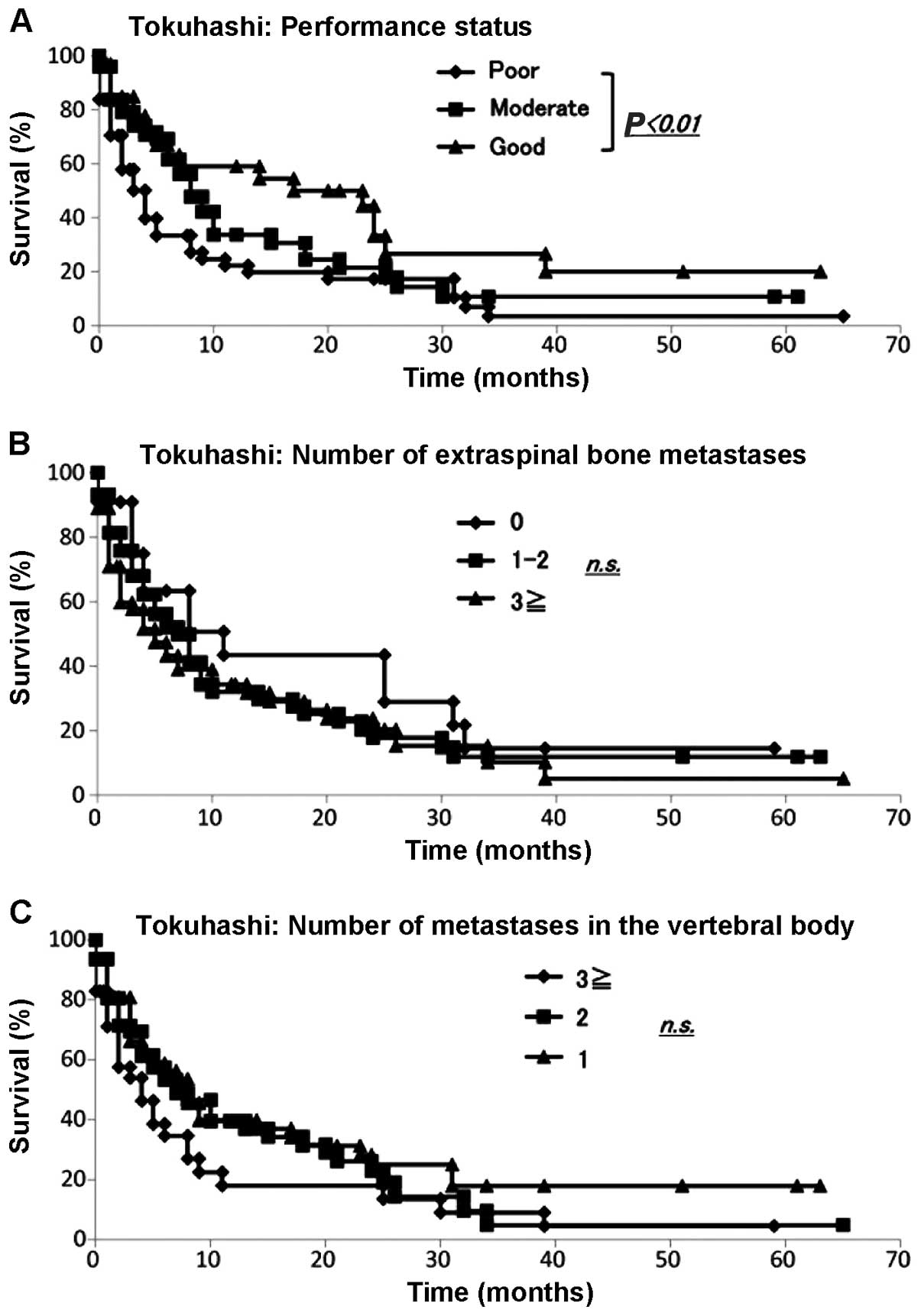
IV. The Kaplan-Meier and log-rank analyses demonstrated that
performance status (poor vs. good) (Fig.
4A), primary site of cancer (Fig.
5B) and palsy (incomplete vs. none) (Fig. 5C) exhibited significant differences
(P<0.05). No other variable was found to be a significant
prognostic factor (Fig. 4B and C;
Fig. 5A).
 | Table IV.Distribution of patients for each
score of the Tokuhashi scoring system. |
Table IV.
Distribution of patients for each
score of the Tokuhashi scoring system.
|
|
| Proportion of
patients |
|---|
|
|
|
|
|---|
| Prognostic
factors | All patients
Kagoshima | With spine
metastasis Tokuhashi (2005) | With spine
metastasis Kagoshima |
|---|
| Performance
status |
|
|
|
| Poor,
10–40% | 61 | N/A | 45 |
|
Moderate, 50–70% | 51 | N/A | 36 |
| Good,
80–100% | 33 | N/A | 17 |
| No. of extraspinal
bone metastases |
|
|
|
| ≥3 | 22 | N/A | 15 |
|
1–2 | 58 | N/A | 18 |
| 0 | 65 |
| 65 |
| No. of metastases
in the vertebral body |
|
|
|
| ≥3 | 36 | N/A | 36 |
| 2 | 17 | N/A | 17 |
| 1 | 45 | N/A | 45 |
| 0 | 47 | N/A | 0 |
| Metastases to the
major internal organs |
|
|
|
|
Unresectable | 36 | N/A | 28 |
|
Resectable |
0 | N/A | 0 |
| No
metastasis | 109 | N/A | 70 |
| Primary cancer
site |
|
|
|
| Lung,
osteosarcoma, stomach, bladder, esophagus, pancreas | 50 | N/A | 30 |
| Liver,
gallbladder, unidentified | 17 | N/A | 12 |
| Kidney,
uterus | 13 | N/A | 7 |
|
Rectum |
7 | N/A | 5 |
|
Thyroid, breast, prostate,
carcinoid | 37 | N/A | 29 |
|
Others | 21 | N/A | 15 |
| Palsy |
|
|
|
|
Complete, Frankel A and B |
7 | N/A | 7 |
|
Incomplete, Frankel C and
D |
4 | N/A | 4 |
| None,
Frankel E | 134 | N/A | 87 |
We then applied the Tokuhashi scoring system to the
data for all of our patients with metastases and to those with
metastases only to the spine (Table
VA). The results of score calculation of the total group and
the spinal metastasis group revealed significant differences for
both distributions compared with that of the Tokuhashi score
(P<0.01). The Kaplan-Meier and log-rank analyses demonstrated
that patients with scores of 12–15 and 9–11 and those with scores
of 12–15 and 0–8 had significantly different prognoses (P<0.01)
(Fig. 5D). Among the patients with
12–15 points, 84.4% survived for >12 months and 53.6% survived
for >24 months. Among the patients with 9–11 points, 67.8, 53.1,
34.5 and 18.2% survived for 3, 6, 12 and 24 months, respectively.
Among patients with 0–8 points, 58.9, 38.0, 18.9 and 16.5% survived
for 3, 6, 12 and 24 months, respectively (Table VB).
 | Table V.Evaluation of prognosis by the
Tokuhashi scoring system for patients with spine metastasis. |
Table V.
Evaluation of prognosis by the
Tokuhashi scoring system for patients with spine metastasis.
| A, Proportion of
patients |
|
|
|
|---|
|
|---|
| Scoring | All patients
Kagoshima |
| Patients with spine
metastasis Tokuhashi (2005)a |
|---|
| 12–15 points | 31 |
| 23 |
| 9–11 points | 54 |
| 67 |
| 0–8 points | 60 |
| 156 |
|
|
| Patients with spine
metastasis |
|
|
|
| Scoring | Kagoshima |
| Tokuhashi
(2005)a |
|
| 12–15 points | 25 |
| 23 |
| 9–11 points | 29 |
| 67 |
| 0–8 points | 44 |
| 156 |
|
| B, Tokuhashi
scoring |
|
|
|
|
| Prognostic
score | Months | Survival rate | 95% CI |
| 12–15 points | 3 | 88.8 | 0.77–1.00 |
|
| 6 | 88.8 | 0.77–1.00 |
|
| 12 | 84.4 | 0.77–1.00 |
|
| 24 | 53.6 | 0.30–0.77 |
| 9–11points | 3 | 67.8 | 0.55–0.81 |
|
| 6 | 53.1 | 0.38–0.68 |
|
| 12 | 34.5 | 0.20–0.49 |
|
| 24 | 18.2 | 0.06–0.31 |
| 0–8 points | 3 | 58.9 | 0.46–0.72 |
|
| 6 | 38.0 | 0.25–0.51 |
|
| 12 | 18.9 | 0.08–0.30 |
|
| 24 | 16.5 | 0.06–0.27 |
As the Tokuhashi score was originally based on the
prognoses of patients with metastatic spinal tumors, it was applied
to our patients who suffered from metastatic spine tumors. The
number of each group from Kagoshima University and Tokuhashi et
al (3) are summarized in Table VA. The Mann-Whitney U test revealed
that there was a statistically significant difference (P<0.05).
The Kaplan-Meier and log-rank analyses demonstrated that patients
with scores of 12–15 and 0–8 and those with scores of 9–11 and 0–8
had significantly different prognoses (P<0.01) (Fig. 5E).
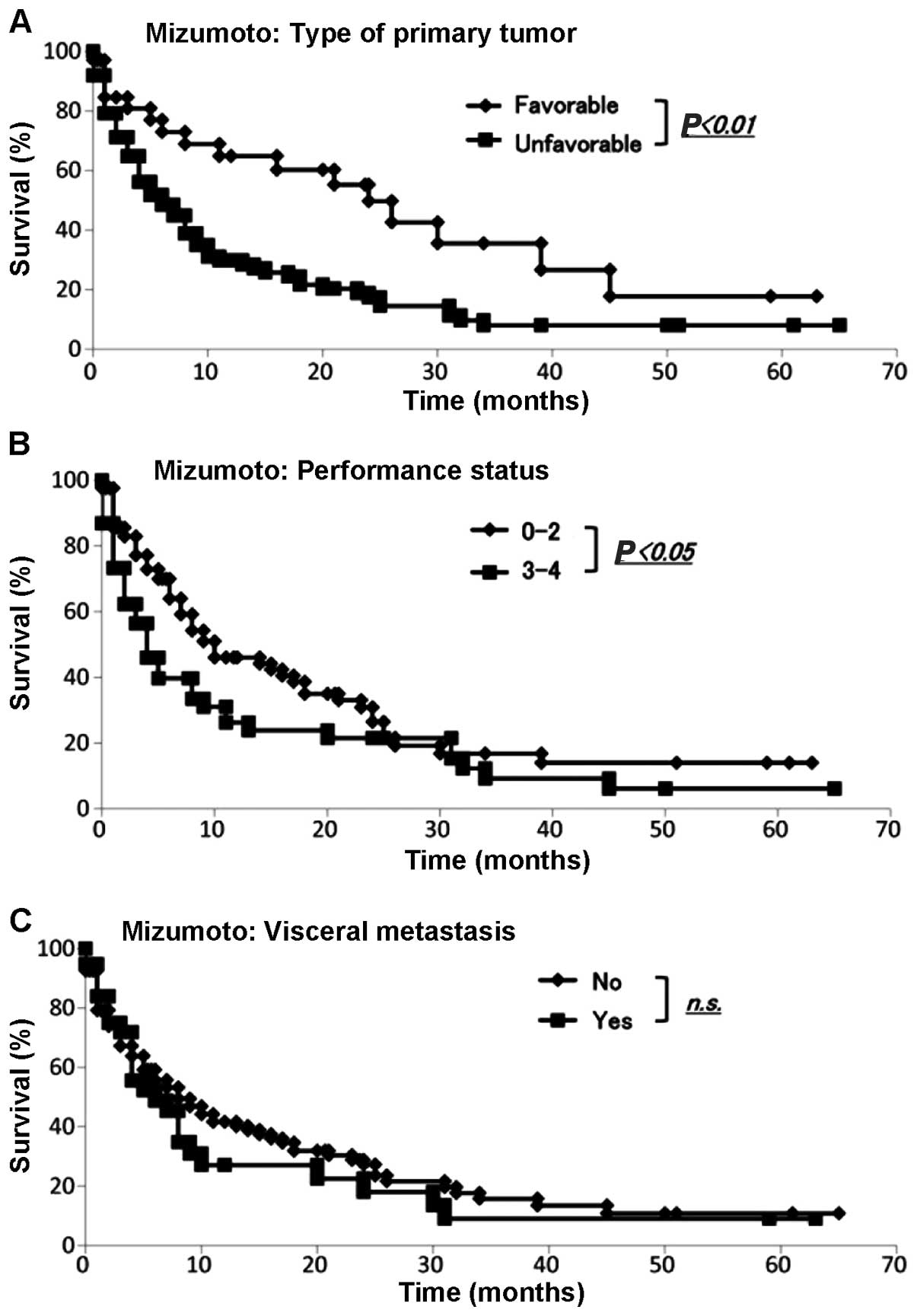
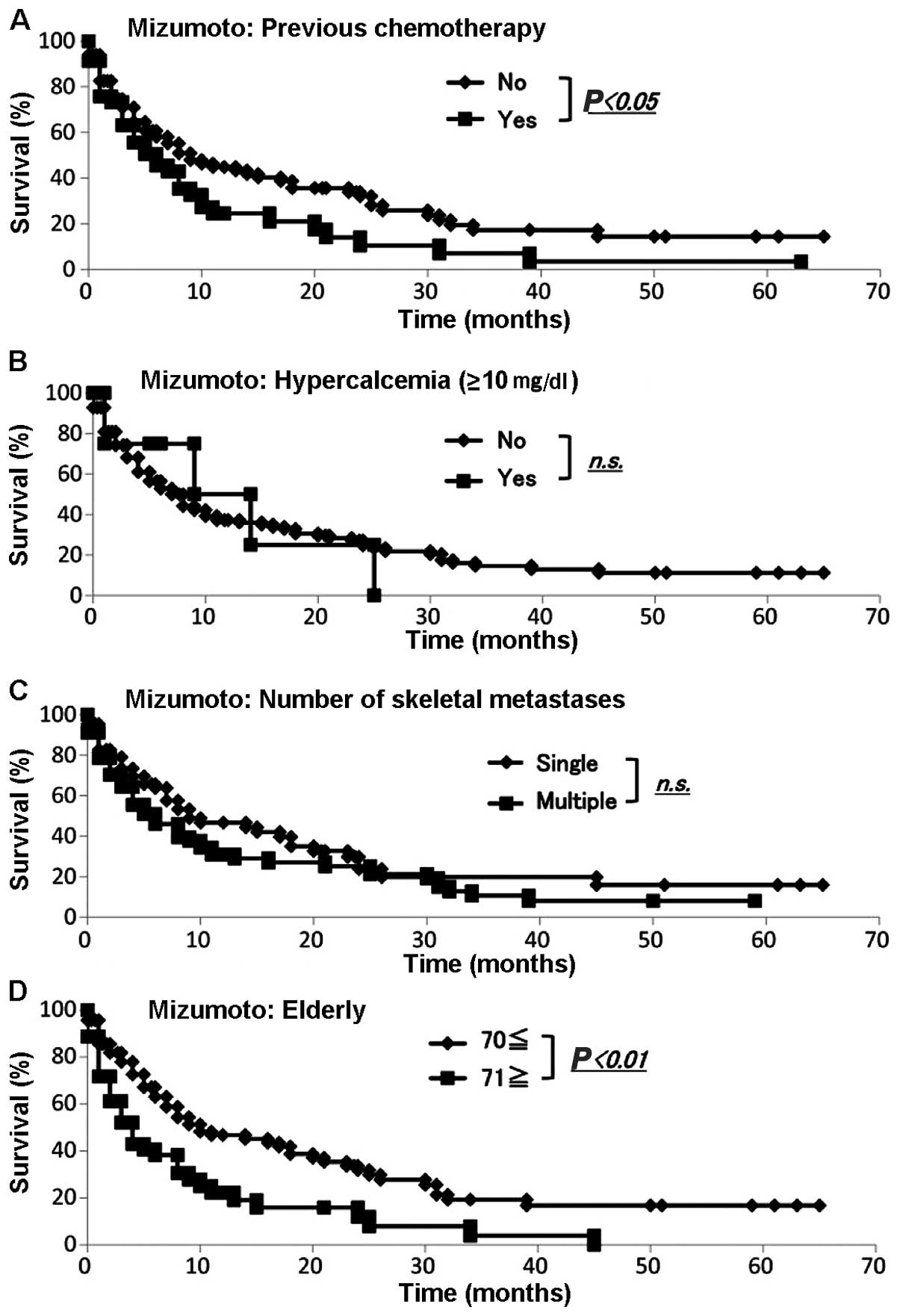
Evaluation of prognosis by the
Mizumoto score
We collected the data for all our 145 skeletal
metastasis patients regarding prognosis, type of primary lesion,
performance status, presence or absence of visceral metastases,
history of previous chemotherapy, presence or absence of
hypercalcemia (>10 mg/dl), number of bone metastases and age
(≥70 or <70 years) according to the Mizumoto scoring system
(4). The demographic data for each
prognostic factor from Kagoshima University and Mizumoto et
al (4) are summarized in Table VI. We performed the Fisher's exact
test to assess any significant differences between the Kagoshima
University and Mizumoto score data sets. The sets differed
significantly with respect to primary tumor type (P<0.05),
presence or absence of visceral metastasis, history of previous
chemotherapy, number of skeletal metastases (single or multiple)
and age ≥71 years (P<0.01). The sets did not differ
significantly with respect to performance status or total serum
calcium (>10 or ≤10 mg/dl) (Table
VI). The Kaplan-Meier and log-rank analyses revealed that
primary tumor type (favorable or unfavorable), performance status
(0–2 or 3–4) (Fig. 6A and B), history
of chemotherapy (yes or no) and age (<70 or ≥71 years) (Fig. 7A and D) exhibited significant
differences. By contrast, the Kaplan-Meier and log-rank analyses
demonstrated that the presence of visceral metastases (yes or no)
(Fig. 6C), total serum calcium
(>10 or ≤10 mg/dl) and number of skeletal metastases (single or
multiple) (Fig. 7B and C) were not
significantly different.
 | Table VI.Distribution of patients for each
score of the Mizumoto scoring system. |
Table VI.
Distribution of patients for each
score of the Mizumoto scoring system.
| Proportion of
patients | Kagoshima all
patients | Mizumoto (2008)
radiation | Fisher's exact
probability test | Kagoshima
radiation | Fisher's exact
probability test |
|---|
| Type of primary
tumor |
|
| <0.05 |
| <0.01 |
|
Favorable | 34 | 174 |
| 8 |
|
|
Unfavorable | 111 | 370 |
| 37 |
|
| Performance
status |
|
| 0.29 |
| 0.08 |
|
0–2 | 84 | 331 |
| 22 |
|
|
3–4 | 61 | 213 |
| 23 |
|
| Visceral
metastasis |
|
| <0.01 |
| <0.05 |
| No | 108 | 248 |
| 29 |
|
|
Yes | 37 | 296 |
| 16 |
|
| Previous
chemotherapy |
|
| <0.01 |
| <0.05 |
| No | 99 | 233 |
| 27 |
|
|
Yes | 46 | 311 |
| 18 |
|
| Total serum
calcium, mg/dl |
|
| 0.069 |
| <0.05 |
|
≤10 | 137 | 490 |
| 45 |
|
|
>10 |
8 | 54 |
| 0 |
|
| Multiple bone
metastases |
|
| <0.01 |
| <0.01 |
| No | 80 | 58 |
| 13 |
|
|
Yes | 65 | 486 |
| 32 |
|
| Age, years |
|
| <0.01 |
| 0.48 |
|
<70 | 92 | 402 |
| 34 |
|
|
≥71 | 53 | 142 |
| 11 |
|
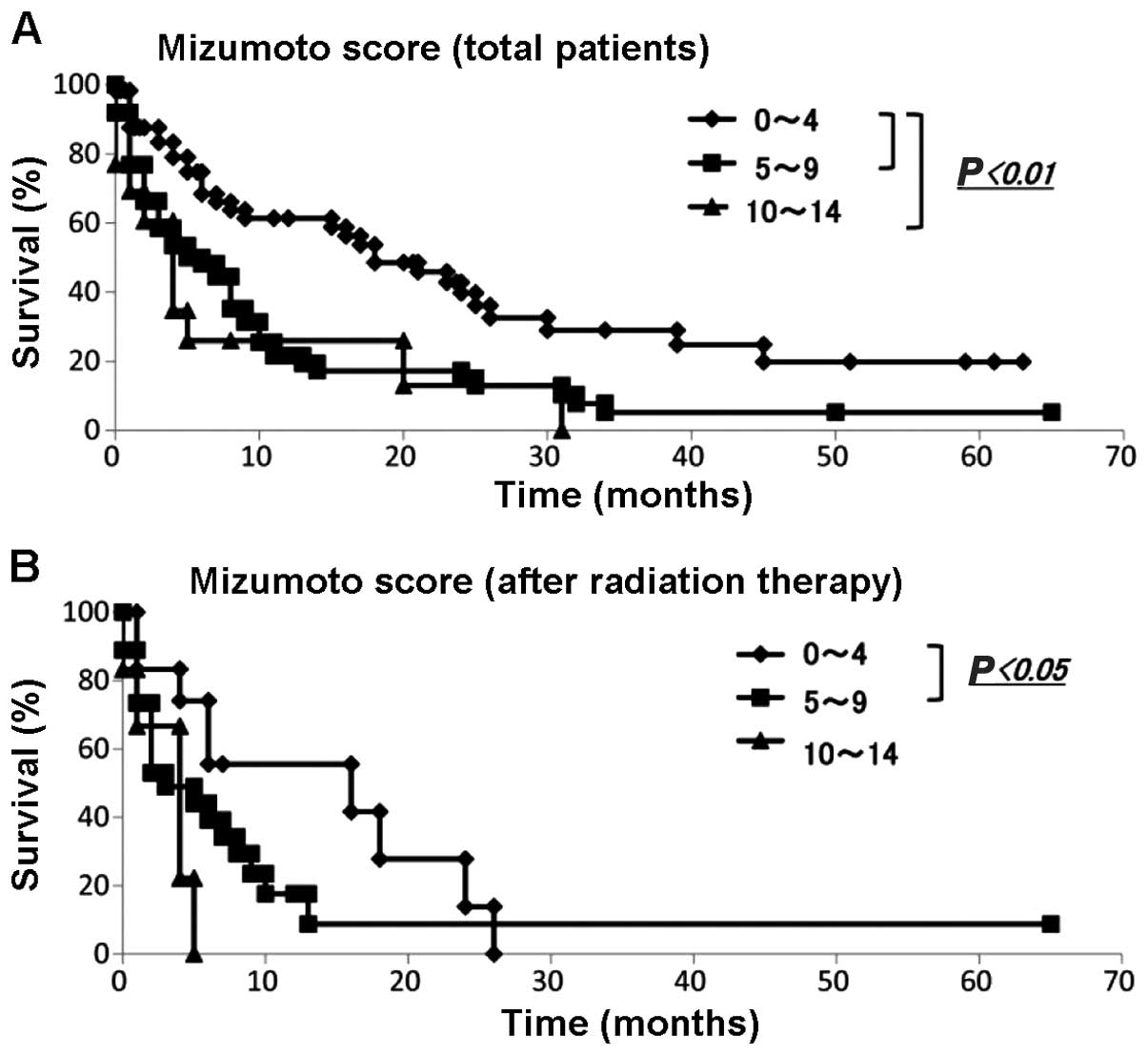
We applied the Mizumoto scoring system to the data
from our patients with metastatic bone tumors. The numbers of each
group from Kagoshima University and Mizumoto et al (4) are summarized in Table VIIA. The results of the scoring
calculation for all patients and for the spinal metastasis patients
exhibited significant differences in each distribution compared
with those of Mizumoto et al (4) (P<0.01). The Kaplan-Meier and log-rank
analyses demonstrated that patients with scores of 0–4 and 5–9 and
those with scores of 0–4 and 10–14 exhibited significantly
different prognoses (Fig. 8A). Among
the patients with 0–4 points, 83.3, 68.3, 61.3 and 39.8% survived
for 3, 6, 12 and 24 months, respectively. Among the patients with
5–9 points, 58.4, 48.1, 21.5 and 15.1% survived for 3, 6, 12 and 24
months, respectively. Among those with 10–14 points, 60.6, 26.0,
26.0 and 13.0% survived for 3, 6, 12 and 24 months, respectively
(Table VIIB).
 | Table VII.Evaluation of prognosis by the
Mizumoto survival scoring system. |
Table VII.
Evaluation of prognosis by the
Mizumoto survival scoring system.
| A, Mizumoto
score |
|
|
|
|---|
|
|---|
| Scoring | All patients
Kagoshima |
| All patients
Mizumoto (2008)a |
|---|
| 0–4 | 58 |
| 131 |
| 5–9 | 74 |
| 310 |
| 10–14 | 13 |
| 103 |
|
| Scoring | Radiation
Kagoshima |
| Radiation Mizumoto
(2008)a |
|
| 0–4 | 12 |
| 131 |
| 5–9 | 27 |
| 310 |
| 10–14 | 6 |
| 103 |
|
| B, Mizumoto
scoring |
|
|
|
|
| Prognostic
score | Months | Survival rate | 95% CI |
|
| 0–4 points | 3 | 83.3 | 0.73–0.93 |
|
| 6 | 68.3 | 0.55–0.81 |
|
| 12 | 61.3 | 0.47–0.75 |
|
| 24 | 39.8 | 0.25–0.55 |
| 5–9 points | 3 | 58.4 | 0.47–0.70 |
|
| 6 | 48.1 | 0.36–0.60 |
|
| 12 | 21.5 | 0.11–0.32 |
|
| 24 | 15.1 | 0.05–0.25 |
| 10–14 points | 3 | 60.6 | 0.33–0.88 |
|
| 6 | 26.0 | 0.01–0.51 |
|
| 12 | 26.0 | 0.01–0.51 |
|
| 24 | 13.0 | 0.00–0.35 |
The Mizumoto score was originally based on the
prognosis of patients with spinal metastases who underwent
radiotherapy; therefore, it was applied to our patients who
suffered from spinal metastases and had undergone radiotherapy. The
Mann-Whitney U test demonstrated that there were no statistical
differences (P<0.01) (Table
VIIA). The Kaplan-Meier and log-rank analyses revealed that
patients with scores between 0 and 4 and between 5 and 9 had
significantly different prognoses (P<0.05) (Fig. 8B).
Discussion
Using single-center data, we evaluated previously
reported prognostic scoring systems in patients with bone
metastases. It is difficult to determine which treatment should be
selected for patients with bone metastases: Curative surgery,
palliative surgery, or conservative treatment. A scoring system may
be useful in predicting the prognosis of patients with bone
metastases. Although scoring systems are based on statistical
evaluations of data obtained from a large number of patients, there
are several sampling biases.
The distributions of patients in each scoring group
were statistically different between the Kagoshima and Katagiri,
Tokuhashi and Mizumoto groups (P<0.01). The distributions of
patients for all prognostic factors were significantly different
between the SSG group and the Kagoshima group (1). The SSG patients comprised those whose
extremity skeletal metastases were treated surgically. The
distributions of patients for 5 of 7 prognostic factors were
significantly different between the Mizumoto and Kagoshima data
(4). The Mizumoto system included
data from patients whose metastatic bone tumors were treated by
radiation, whereas the Kagoshima data were from patients who had
skeletal metastases. These differences in collection criteria may
affect the differences in the group compositions. However, the
distributions of patients in 3 of 5 prognostic factors were
statistically different between the Katagiri and the Kagoshima
data, although these two data sets were based on patients who had
metastatic bone tumors (2).
Regional and hospital characteristics may also lead
to sampling biases. The Katagiri data were collected at Shizuoka
Cancer Center Hospital, which is one of the university hospitals in
Shizuoka province. Thus, a proportion of the Katagiri patients with
bone metastases may have been treated originally at other
university hospitals; some of these patients achieved remission and
others were referred to the Shizuoka Cancer Center Hospital. By
contrast, the Kagoshima data were collected at Kagoshima University
Hospital, which is the only university hospital in Kagoshima
province. Almost all Kagoshima province patients with metastatic
bone tumors are first referred to our department. In support of
these hypotheses, the Katagiri data include a higher number of
patients with visceral and cerebral metastases, lower performance
status and multiple skeletal metastases. These findings suggest
that differences in the background may affect the prediction of
prognosis determined by scoring systems.
The predictions of prognosis were substantially
different in each system's results and in our results for the good-
as well as the poor-prognosis groups. The 6-month survival rates
for the SSG and Kagoshima reports for group A using the SSG score
were 88.1 and 65.5%, respectively. The 6-month survival rates in
the Katagiri and Kagoshima patients with scores of 0–2 by the
Katagiri system were 97.9 and 69.7%, respectively. The 6-month
survival rates in the Tokuhashi and Kagoshima reports for patients
with 12–15 points by the Tokuhashi score were 100 and 88.8%,
respectively. The 6-month survival rates in the Mizumoto and
Kagoshima reports for patients with 10–14 points (group A) by the
Mizumoto score were 89.0 and 65.5%, respectively.
These differences suggest that it is crucial to
evaluate scoring systems to determine which is the most suitable
for each hospital. The Tokuhashi scoring system detected the
highest survival patient group at 6–12 months (12–15 points, 88.4%)
in the Kagoshima data. Patients with a life expectancy of >6
months may benefit from tumor excision and endoprosthetic
reconstruction (8). These findings
suggest that Tokuhashi scoring is the most appropriate scoring
system for identifying patients who should be explored for curative
surgical intervention at our hospital. By contrast, recovery from
surgery must be shorter than the prediction of survival. The
6-month survival rates of SSG and Kagoshima patients in group C
according to the SSG score were 14.3 and 8.7%, respectively. The
6-month survival rate in the Kagoshima data set among patients with
6–8 points by the Katagiri score was 29.8%. The 6-month survival
rates for the Tokuhashi and Kagoshima patients with 0–8 points by
the Tokuhashi score were 14.7 and 38.0%, respectively. The 6-month
survival rates for the Mizumoto and Kagoshima patients in group C
according to the Mizumoto score were 7.0 and 26.0%, respectively.
It is difficult to select curative surgical intervention in
patients with a life expectancy of <6 months (7,9). Our
findings suggest that SSG scoring is appropriate in our hospital
for identifying patients who are expected to live <6 months
(group C, 91.3%).
The type of primary lesion, performance status,
number of skeletal metastases, presence of organ metastasis,
history of previous chemotherapy, spinal cord palsy, hypercalcemia
and advanced age were proposed as prognostic factors by all four
scoring systems, although the cut-offs and the number of prognostic
factors assessed were different. Kaplan-Meier analysis demonstrated
that the type of primary lesion and performance status
statistically affected different prognoses in three of the four
scoring systems when calculated by the Kagoshima data. However, the
number of skeletal metastases and presence of organ metastases were
not statistically significantly different in any of the four
scoring systems when calculated by the Kagoshima data. Although we
were unable to identify the cause of the differences, these results
suggest that other sets of prognostic factors may be suitable as a
scoring system for individual hospitals that have multidisciplinary
care teams to treat metastatic bone tumors. In conclusion, prior to
predicting prognosis by a scoring system, it is crucial to select
the most suitable for the characteristics of each particular
hospital.
Acknowledgements
The authors would like to thank Hui Gao for the
excellent technical assistance and Edanz for English editing
services.
References
|
1
|
Ratasvuori M, Wedin R, Keller J, et al:
Insight opinion to surgically-treated metastatic bone disease:
Scandinavian Sarcoma Group Skeletal Metastasis Registry report of
1195 Operated Skeletal Metastasis Surg Oncol. 22:132–138.
2013.PubMed/NCBI
|
|
2
|
Katagiri H, Takahashi M, Wakai K, Sugiura
H, Kataoka T and Nakanishi K: Prognostic factors and a scoring
system for patients with skeletal metastasis. J Bone Joint Surg Br.
87:698–703. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Tokuhashi Y, Matsuzaki H, Oda H, Oshima M
and Ryu J: A revised scoring system for preoperative evaluation of
metastatic spine tumor prognosis. Spine. 30:2186–2191. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Mizumoto M, Harada H, Asakura H, et al:
Prognostic factors and a scoring system for survival after
radiotherapy for metastases to the spinal column: A review of 544
patients at Shizuoka Cancer Center Hospital. Cancer. 113:2816–2822.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Shimada H, Setoguchi T, Yokouchi M, et al:
Metastatic bone tumors: Analysis of factors affecting prognosis and
efficacy of CT and 18F-FDG PET-CT in identifying primary
lesions. Mol Clin Oncol. 5:875–881. 2014.
|
|
6
|
Oken MM, Creech RH, Tormey DC, et al:
Toxicity and response criteria of the Eastern Cooperative Oncology
Group. Am J Clin Oncol. 5:649–655. 1982. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Frankel HL, Hancock DO, Hyslop G, et al:
The value of postural reduction in the initial management of closed
injuries of the spine with paraplegia and tetraplegia. I.
Paraplegia. 7:179–192. 1969. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Quinn RH and Drenga J: Perioperative
morbidity and mortality after reconstruction for metastatic tumors
of the proximal femur and acetabulum. J Arthroplasty. 21:227–232.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Eastley N, Newey M and Ashford RU:
Skeletal metastases - the role of the orthopaedic and spinal
surgeon. Surg Oncol. 21:216–222. 2012. View Article : Google Scholar : PubMed/NCBI
|