Introduction
Toxic epidermal necrolysis (TEN) is a progressive
extensive skin disease that is potentially fatal. TEN is defined by
formation of bullae and skin sloughing, with purpuric spots
covering ≥30% of the body surface area, or skin sloughing and
bullae alone, involving 10% of the body surface area. The skin
manifestations are associated with a marked systemic inflammatory
response syndrome and major electrolyte disturbances, with a
mortality rate of >30% (1). TEN is
classically medication-induced. A skin biopsy is essential for
diagnosis and exclusion of other diseases masquerading as or
coexisting with TEN. We herein describe a case where skin biopsy in
a patient with classical TEN revealed a cutaneous T-cell lymphoma
complicated by TEN. To the best of our knowledge, very few cases of
TEN associated with cutaneous T-cell lymphoma have been reported to
date (2–4).
Case report
A 54-year-old African-American man with a past
medical history of psoriasis diagnosed 6 years prior, diabetes
mellitus, chronic pancreatitis, heart failure and hypertension,
presented to the emergency department for evaluation of fever
(101.7°F for 3 days) accompanied by chills, body aches, pruritus
and edema. The patient also reported recent prolonged sun exposure
and a progressive scaly rash on his face and neck that had first
appeared 3 weeks prior to presentation. The patient attributed his
skin rash to methotrexate (MTX) and denied any recent sick
contacts, chest pain, weight loss, vomiting, abdominal pain,
dysuria, cough or headaches.
The patient's home medications included MTX and
prednisone for psoriasis, insulin for diabetes, and lisinopril,
metoprolol and aspirin for hypertension and heart failure. All
medications were held on admission. In the emergency department,
the patient's vitals included an elevated oral temperature of
104.4°F, a heart rate of 168 beats/min, blood pressure 89/70 mmHg
and a glucose level of 138 mg/dl. On physical examination, the
patient was in moderate distress; his lungs were clear and the
cardiac sounds were normal, without any rubs or gallops, but he was
tachycardic. The abdomen was soft, with active bowel sounds. The
skin examination revealed a dry scaly rash on the upper and lower
extremities bilaterally. Erythema and pigmentation were observed on
the face, without blisters. Palpable lymph nodes were detected in
the bilateral inguinal areas. The laboratory test results revealed
leukocytosis (20,900 cells/mm3), but were otherwise
unremarkable.
The patient's chest X-ray was normal, but a computed
tomography (CT) scan of his chest, abdomen and pelvis revealed
bulky axillary lymphadenopathy and prominent mediastinal lymph
nodes, with extensive retroperitoneal, external iliac chain and
inguinal lymphadenopathy.
The patient was fluid-resuscitated; blood and urine
cultures were obtained, and a lumbar puncture was performed prior
to starting antibiotics, initially consisting of i.v. vancomycin
and cefepime for empiric treatment of sepsis from unknown source.
All the cultures were negative and the antibiotics were
de-escalated to clindamycin to cover for cellulitis. Despite the
negative cultures, the patient developed an altered mental status
and underwent a repeat head CT and lumbar puncture, which were
normal. At that time, antibiotic therapy was escalated again to
i.v. vancomycin, piperacillin/tazobactam and tobramycin for
refractory sepsis. The skin was biopsied and a bone marrow biopsy
was performed for thrombocytopenia and hemolysis, with an elevated
immature platelet count of 8.6%.
Five days later, the patient developed respiratory
failure, became tachypneic and tachycardic, with a significantly
increased work of breathing, requiring intubation and mechanical
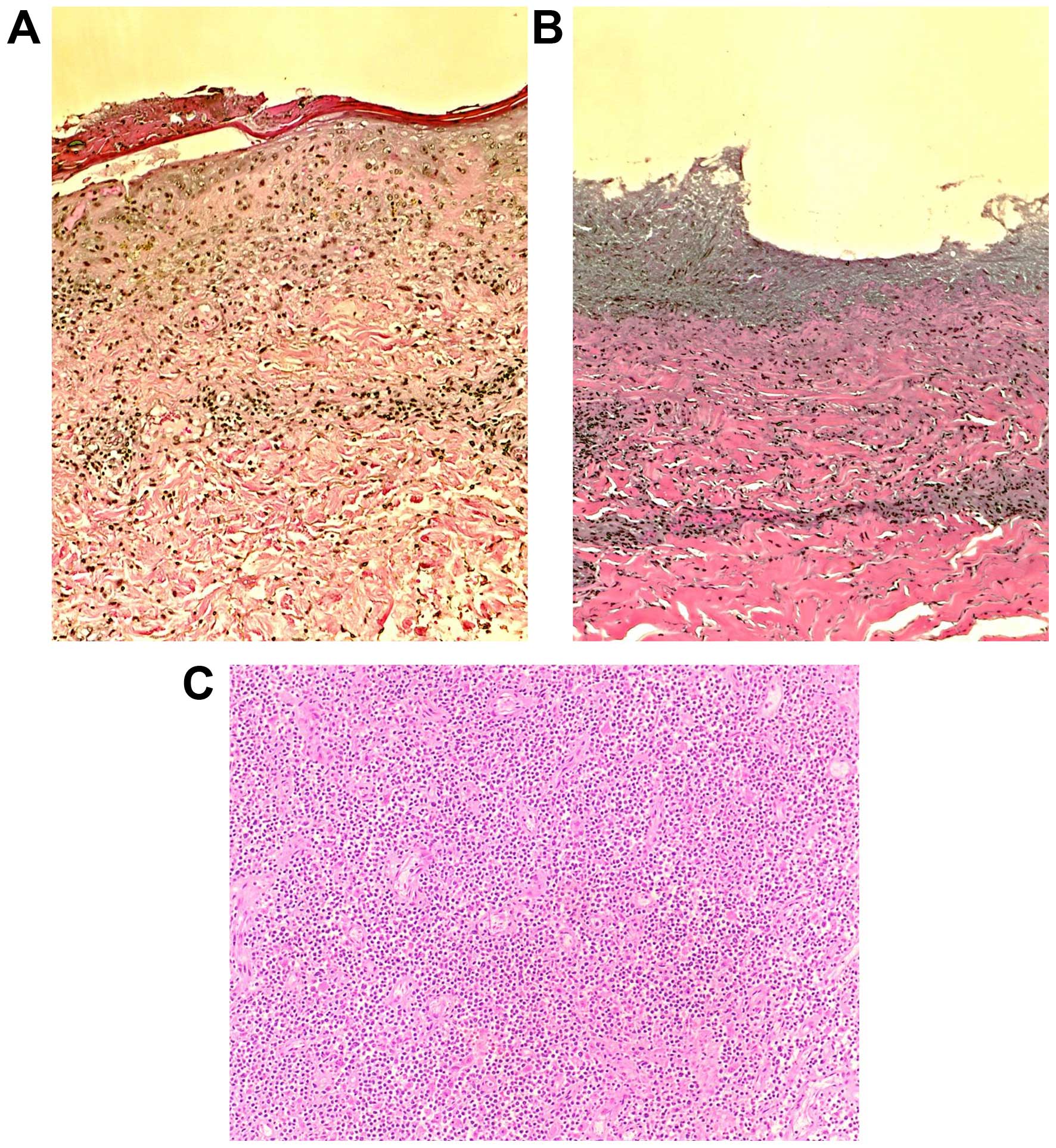
ventilation. The skin rash became more desquamative; Stevens-Johson
syndrome (SJS) was suspected and was attributed to MTX, which had
been held on admission. The clinical picture progressed rapidly to
TEN (Fig. 1).
Subsequently, the patient developed acute renal
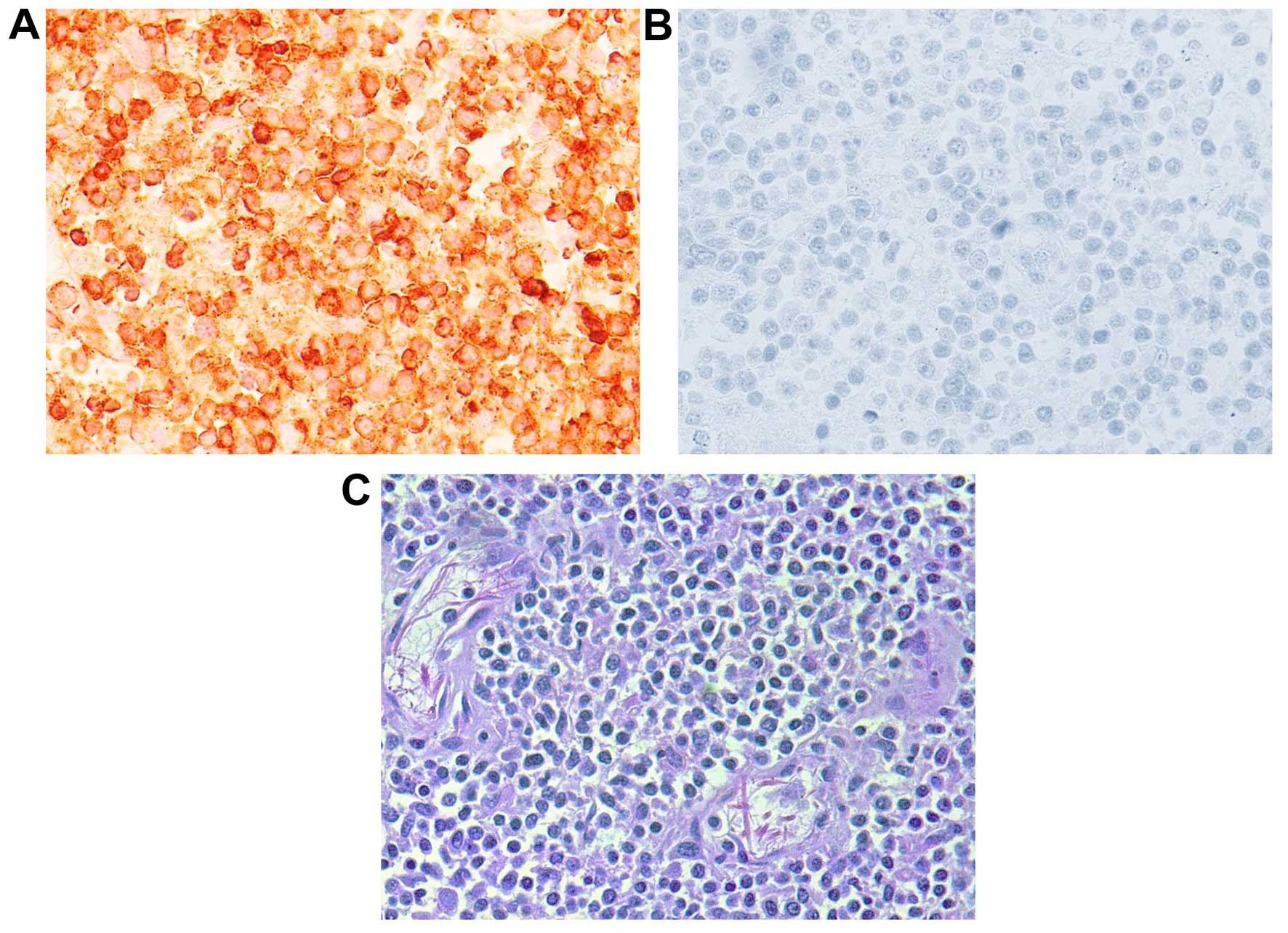
failure requiring hemodialysis. The prior skin biopsy was
interpreted as being consistent with T-cell cutaneous lymphoma
(Fig. 2). The peripheral blood smear
was negative for Sezary cells. Subsequent blood cultures grew
vancomycin-resistant enterococcus and candida at 15 days. The
antibiotics were changed to fluconazole, daptomycin and
meropenem.
The patient's skin rash progressively worsened and,
on hospital day 23, it progressed to TEN. Fluconazole was changed
to caspofungin, as it is associated with a lower incidence of TEN.
Lymph node core needle biopsy was performed, the results of which
were consistent with lymphoma (Fig.
3). Given the patient's clinical instability, he was not deemed
to be a candidate for chemotherapy. The rash progressively became
more extensive and the patient subsequently succumbed to his
condition.
Discussion
SJS and TEN have long been viewed as a continuum
with escalating severity, as the exfoliating pathology advances to
involve larger body areas. Between those rare entities, SJS is 3–5
times more common compared with TEN, and usually encountered in
women. Studies have shown that a dysregulated immune response,
genetics and drugs may be predisposing risk factors to developing
these two pathologies (5).
TEN is an entity frequently seen in the intensive
care unit (ICU) and it is usually drug-induced. Thus, this was the
initial impression when assessing the present case. Our patient was
on MTX for presumed psoriasis. MTX has been found to be associated
with TEN. However, the rash progressed from SJS to TEN despite
discontinuing MTX. Alternatively, SJS/TEN could have been
drug-induced, secondary to the antibiotics the patient received for
sepsis. When reviewing the literature, no TEN cases were reported
in association with daptomycin, only 4 with pippracillin-tazobactam
(6–9),
and 12 cases with fluconazole (10–17).
The fact that the patient presented with SJS
progressing to TEN despite discontinuing MTX and despite being on
antibiotics that have minimal association with TEN, makes the
association with cutaneous T-cell lymphoma more likely. Lymphoma
was confirmed by skin, bone marrow and lymph node biopsies that
solely revealed T-cell lymphoma. There have been several reported
cases of TEN in lymphoma patients with presentations similar to our
case.
While skin rashes in the ICU are frequently
encountered, it is important to perform skin biopsies, particularly
when the patient's status progressively deteriorates. It is also
important to rule out other causes of desquamating skin rashes,
such as human immunodeficiency virus, pemphigoid skin disorders,
drug-induced SJS and TEN and, rarely, cutaneous T-cell
lymphoma.
A witnessed informed consent for publication of this
case report was obtained from the patient's next of kin.
Glossary
Abbreviations
Abbreviations:
|
ICU
|
intensive care unit
|
|
CT
|
computed tomography
|
|
MTX
|
methotrexate
|
|
SJS
|
Stevens-Johnson syndrome
|
|
TEN
|
toxic epidermal necrolysis
|
References
|
1
|
Pereira FA, Mudgil AV and Rosmarin DM:
Toxic epidermal necrolysis. J Am Acad Dermatol. 56:181–200. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Schoeffler A, Levy E, Weinborn M, Cuny JF,
Schmutz JL, Barbaud A, Cribier B and Bursztejn AC: Stevens-Johnson
syndrome and Hodgkin's disease, A fortuitous association or
paraneoplastic syndrome? Ann Dermatol Venereol. 141:134–140.
2014.(In French). View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Jones B, Vun Y, Sabah M and Egan CA: Toxic
epidermal necrolysis secondary to angioimmunoblastic T-cell
lymphoma. Australas J Dermatol. 46:187–191. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Sadi AM, Toda T, Kiyuna M, Tamamoto T,
Ohshiro K and Shinzato R: An autopsy case of malignant lymphoma
with Lyell's syndrome. J Dermatol. 22:594–599. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Ellender RP, Peters CW, Albritton HL,
Garcia AJ and Kaye AD: Clinical considerations for epidermal
necrolysis. Ochsner J. 14:413–417. 2014.PubMed/NCBI
|
|
6
|
Bajaj P, Prematta MJ and Ghaffari G: A
sixty-five-year-old man with rash, fever, and generalized weakness.
Allergy Asthma Proc. 32:e1–e3. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Lam AI, Randhawa I and Klaustermeyer W:
Cephalosporin induced toxic epidermal necrolysis and subsequent
penicillin drug exanthem. Allergol Int. 57:281–284. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Craycraft ME, Arunakul VL and Humeniuk JM:
Probable vancomycin-associated toxic epidermal necrolysis.
Pharmacotherapy. 25:308–312. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Cheriyan S, Rosa RM and Patterson R:
Stevens-Johnson syndrome presenting as intravenous line sepsis.
Allergy Proc. 16:85–87. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Gussenhoven MJ, Haak A, Peereboom-Wynia JD
and van 't Wout JW: Stevens-Johnson syndrome after fluconazole.
Lancet. 338:1201991. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Islam S, Singer M and Kulhanjian JA: Toxic
epidermal necrolysis in a neonate receiving fluconazole. J
Perinatol. 34:792–794. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
George J, Sharma A, Dixit R, Chhabra N and
Sharma S: Toxic epidermal necrolysis caused by fluconazole in a
patient with human immunodeficiency virus infection. J Pharmacol
Pharmacother. 3:276–278. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Pasmatzi E, Monastirli A, Georgiou S,
Sgouros G and Tsambaos D: Short-term and low-dose oral fluconazole
treatment can cause Stevens-Johnson syndrome in HIV-negative
patients. J Drugs Dermatol. 10:13602011.PubMed/NCBI
|
|
14
|
Thiyanaratnam J, Cohen PR and Powell S:
Fluconazole-associated Stevens-Johnson syndrome. J Drugs Dermatol.
9:1272–1275. 2010.PubMed/NCBI
|
|
15
|
Monastirli A, Pasmatzi E, Vryzaki E,
Georgiou S and Tsambaos D: Fluconazole-induced Stevens-Johnson
syndrome in a HIV-negative patient. Acta Derm Venereol. 88:521–522.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Ofoma UR and Chapnick EK: Fluconazole
induced toxic epidermal necrolysis: A case report. Cases J.
2:90712009. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Craythorne E and Creamer D:
Stevens-Johnson syndrome due to prophylactic fluconazole in two
patients with liver failure. Clin Exp Dermatol. 34:e389–e390. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Azón-Masoliver A and Vilaplana J:
Fluconazole-induced toxic epidermal necrolysis in a patient with
human immunodeficiency virus infection. Dermatology. 187:268–269.
1993. View Article : Google Scholar : PubMed/NCBI
|