Introduction
Thyroid nodules have an incidence rate ranging
between 19 and 67% among different populations. Thyroid nodules are
the most commonly encountered tumors in the neck area, with
malignant nodules accounting for ~5–10% (1–3). It has
been reported that 1/3 of thyroid tumors are prone to lymph node
metastasis (4); therefore, early
diagnosis and timely treatment of thyroid nodules significantly
affect recovery and outcome. High-frequency ultrasonography (US) is
a priority imaging choice for identifying benign and malignant
thyroid nodules (5). With the
increased use of real-time shear wave elastography (SWE) and
contrast-enhanced ultrasonography (CEUS) in the diagnosis of
diseases of the liver, prostate, breast and other organs (6–8), their
combined use also provides a new approach to the diagnosis of
thyroid disease. The aim of the present study was to investigate
the value of the combined use of real-time (SWE) and CEUS in the
diagnosis of benign and malignant thyroid nodules.
Subjects and methods
Subjects
A retrospective analysis of 319 pathologically
confirmed thyroid nodules in 253 patients who underwent surgery
between March, 2014 and December, 2015 was conducted. All the
patients were subjected to two-dimensional US (2DUS), SWE and CEUS
imaging. A total of 86 male patients, aged 19–76 years [mean ±
standard deviation (SD), 44±13 years] were found to carry a total
of 116 nodules; 167 female patients, aged 18–78 years (mean ± SD,
43±11 years) were found to carry a total of 203 nodules. The mean ±
SD of the maximum diameters of the 319 nodules was 11.3±2.2 mm
(range, 3–67 mm), with a median of 12.5 mm.
The present study was conducted in accordance with
the Declaration of Helsinki and with approval of the Ethics
Committee of Ningbo First Hospital (Ningbo, China). Written
informed consent was obtained from all the participants.
Instruments and methods
2DUS
The patients underwent SWE performed using a linear
4–15 MHz transducer (Aixplorer, SuperSonic Imagine, Les Jardins de
la Duranne, France). 2DUS was used to determine thyroid nodule
location, size, internal echo, calcification, borders and pattern,
and to calculate the nodule diameter and longitudinal diameter
ratio (aspect ratio). Subsequently, the SWE mode was added. The
patients were asked to hold their breath when the probe was lightly
applied until the image stabilized. Three continuous measurements
of the lesion were then taken and averaged. The sampling frame
should be 2–3 times greater than the area of the lesion, with Q-BOX
covering the latter within a range of 0–180 kPa.
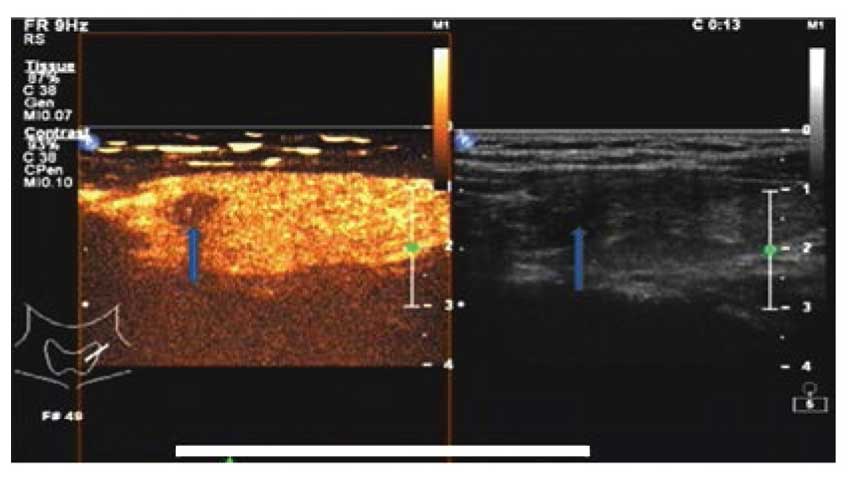
Ceus
The Philips iU22 Xmatrix ultrasonography diagnostic
apparatus with an L9-3 probe was used (Koninklijke Philips N.V.,
Amsterdam, The Netherlands). The instrument was equipped with UE
and CEUS analysis software. The patients were asked to lie in the
supine position. Prior to US, two-dimensional images and color
Doppler images of the thyroid nodules were collected. Subsequently,
intravenous access was established through an elbow vein. A total
of 25 mg SonoVue (Bracco Imaging S.p.A, Milan, Italy) was dissolved
in 5 ml 0.9% sodium chloride and was injected as an intravenous
bolus of 1.2 ml per subject via the antecubital vein, followed by 5
ml 0.9% sodium chloride. Under the US contrast mode the mechanical
index (MI) ranged between 0.05 and 0.06, and the focal point was
adjusted to the middle or the lower edge of the thyroid nodules. If
the nodule is small, the double-contrast mode maybe used to ensure
the probe is in parallel with the long axis of the thyroid gland as
much as possible. During the entire process, the patients were
asked to refrain from swallowing, and the probe was fixed to the
largest section of the nodule in order to ensure a continuous image
acquisition time of at least 2 min prior to storing all data and
collecting them for off-line analysis. Finally, off-line analysis
(Koninklijke Philips N.V., Amsterdam, The Netherlands) was used to
analyze the enhancement time of the lesion and its surrounding
tissue, as well as the enhancement characteristics of the lesion.
The former included access speed, peak time and subsidence speed,
whereas the latter included the access speed of the contrast agent
into the nodule, the distribution of the contrast agent following
access into the nodule, possible annular peripheral enhancement
around the nodule, and the degree of clearness of the nodule
boundaries.
Statistical analysis
SPSS 17.0 software (SPSS Inc., Chicago, IL, USA) was
used for statistical analysis. The indices of SWE were compared
with the t-test and the indices of CEUS were compared with
Kappa analysis. A receiver operating characteristic curve (ROC)
discriminating between benign and malignant thyroid nodules was
drawn according to Young's modulus for each thyroid nodule. The
optimal cut-off point was then determined, and the critical point
and area under the curve were calculated. Sensitivity, specificity
and accuracy of the SWE cut-off for the diagnosis of thyroid cancer
were also calculated. Differences between benign and malignant
thyroid nodules contrast modes were subjected to the χ2
test to identify the sensitivity, specificity and accuracy of CEUS
in discriminating malignant thyroid nodules. The sensitivity,
specificity and accuracy of 2DUS, SWE and the combined use of CEUS
and SWE in the diagnosis of thyroid nodules were compared and
tested using the χ2 difference test. P<0.05 was
considered to indicate statistically significant differences.
Results
Surgical histopathology
Of the 253 cases (319 nodules), the pathological
results showed a total of 136 malignant nodules. In terms of
pathological type, there were 107 papillary, 13 follicular, 11
medullary, 4 undifferentiated and 1 squamous cell carcinoma. The
pathological types of the 183 benign nodules included 135 cases of
nodular goiter, of which 9 exhibited calcifications, 3 coincided
with chronic lymphocytic thyroiditis, 4 exhibited follicular
dysplasia, 3 were adenomatous hyperplastic nodules, 5 exhibited
hemorrhage and 7 exhibited cystic degeneration; the remaining cases
included 38 adenomas, 7 cases of chronic lymphocytic thyroiditis
and 3 cases of subacute thyroiditis.
Diagnostic characteristics of benign
and malignant thyroid nodules using 2DUS
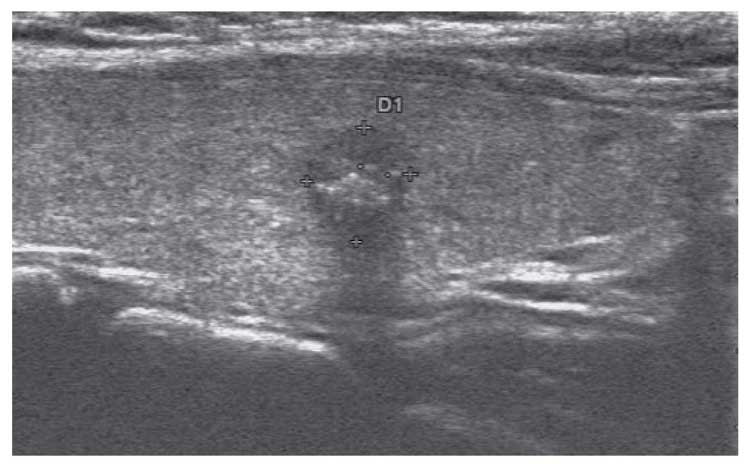
For the 253 cases (319 nodules), 2DUS was used to
evaluate benign and malignant thyroid nodules according to size,
internal echo, boundaries, shape and aspect ratio, and found that
nodule solidity, aspect ratio ≥1, calcification diameter <2 mm,
irregular shape and unclear boundaries exhibited statistically
significant differences between benign and malignant thyroid
nodules (P<0.05) (Tables I and
II; Fig.
1). Conventional US was associated with a sensitivity of 71.32%
(97/136), a specificity of 77.04% (141/183), a positive predictive
value of 69.78% (97/139), a negative predictive value of 78.33%
(141/180), an accuracy of 74.60% (238/319) and a misdiagnosis rate
of 25.4% (81/319) in the diagnosis of thyroid malignancy.
 | Table I.Characteristics of 253 cases (319
thyroid nodules) diagnosed by conventional ultrasonography. |
Table I.
Characteristics of 253 cases (319
thyroid nodules) diagnosed by conventional ultrasonography.
|
|
| Shape | Solidity | Aspect ratio |
|---|
|
|
|
|
|
|
|---|
| Group | Nodule no. | Regular | Irregular | Solid | Cystic-solid | ≥1 | <1 |
|---|
| Benign | 183 | 161 | 22 | 157 | 26 | 14 | 169 |
| Malignant | 136 | 37 | 99 | 103 | 33 | 121 | 15 |
| χ2 |
| 40.31 | 5.22 | 211.36 |
| P-value |
| 0.000 | 0.025 | 0.000 |
 | Table II.Characteristics of 253 cases (319
thyroid nodules) diagnosed by conventional ultrasonography. |
Table II.
Characteristics of 253 cases (319
thyroid nodules) diagnosed by conventional ultrasonography.
|
|
| Calcification
diameter | Boundary |
|---|
|
|
|
|
|
|---|
| Group | Nodule no. | <2 mm | >2 mm | Null | Clear | Unclear |
|---|
| Benign | 183 | 17 | 9 | 157 | 166 | 17 |
| Malignant | 136 | 35 | 4 | 97 | 35 | 101 |
| χ2 |
|
| 16.63 |
| 141.31 |
| P-value |
|
| 0.000 |
| 0.000 |
Diagnostic characteristics of benign
and malignant thyroid nodules using real-time SWE
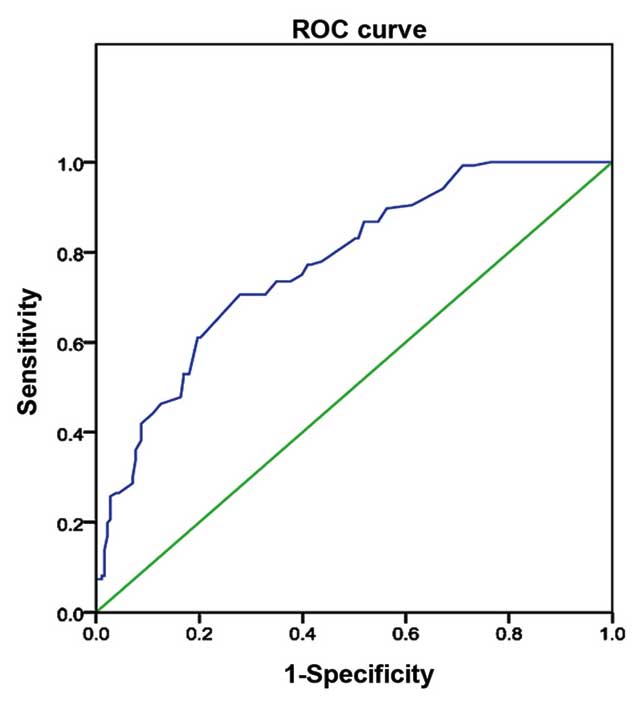
The mean elasticity ± SD of benign and malignant
thyroid nodular lesions was 49.34±23.22 and 17.99±19.55 kPa,
respectively. The paired t-test of independent measurement
of the same nodule by two well-trained sinologists exhibited a
significance of >0.05. The differences in the SWE value between
benign and malignant nodules were found to be statistically
significant (t=11.932, P=0.000). ROC curves were drawn for benign
and malignant thyroid nodules, in which the area under the curve
was 0.77 (95% confidence interval: 0.724–0.825) and the optimal
threshold was 27.65 kPa (Fig. 2). A
total of 144 thyroid nodules ≥27.65 kPa were diagnosed as
malignant, and 175 nodules <27.65 kPa were diagnosed as benign.
Compared with the pathological results, SWE exhibited a sensitivity
of 84.55% (115/136) and a specificity of 84.15% (154/183), a
positive predictive value of 79.86% (115/144), a negative
predictive value of 88.00% (154/175), an accuracy of 84.32%
(269/319) and a misdiagnosis rate of 15.68% (50/319) in the
diagnosis of malignant thyroid nodules.
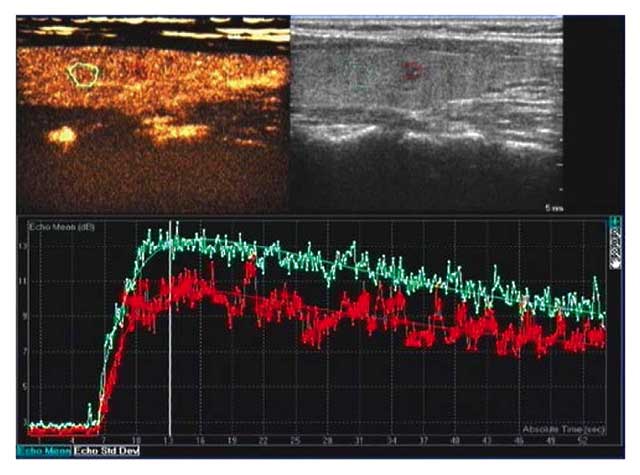
Diagnostic characteristics of benign
and malignant thyroid nodules using CEUS
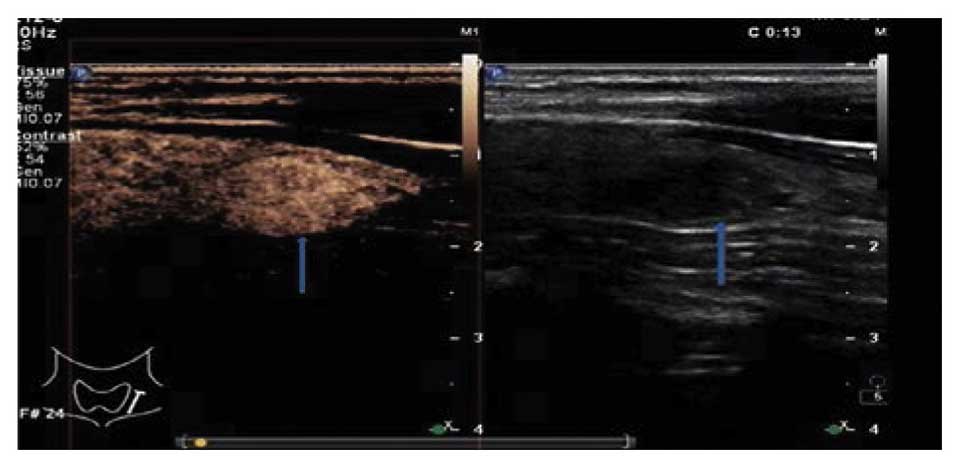
CEUS was used in the diagnosis of 176 benign nodules
that exhibited early high enhancement (later clearing compared with
the surrounding area) following injection of the contrast medium
(Fig. 4). Among these, 69 exhibited
circumferential annular enhancement (Fig. 5), 165 exhibited internal homogeneous
enhancement and 18 exhibited performance heterogeneous enhancement.
A time-intensity curve indicated that 129 nodules were fast-filled
and exhibited enhancement earlier compared with the surrounding
normal glandular tissue. In particular, 38 adenomas were more
highly visible, as their enhancement degree was higher compared
with that of the surrounding tissue and their clearing time was
slower compared with that of the remaining thyroid gland,
displaying classic ‘fast-in and slow-out’ and continued high
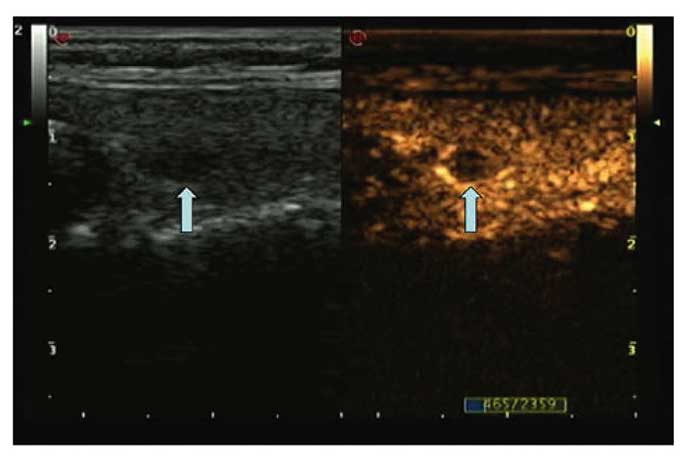
enhancement. A total of 143 thyroid nodules were diagnosed as
malignant, all of which exhibited early low enhancement (Figs. 6 and 7) and quick subsidence, and were filled
from the periphery towards the center, with uneven inner
enhancement and less clear boundaries on US. A comparison of
enhancement time phase and contrast agent distribution differences
between benign and malignant thyroid nodules revealed a
statistically significant difference (P<0.05) (Tables III and IV). CEUS was associated with a sensitivity
of 87.5% (119/136), a specificity of 86.33% (158/183), a positive
predictive value of 82.63% (119/144), a negative predictive value
of 90.28% (158/175), an accuracy of 86.83% (277/319) and a
misdiagnosis rate of 13.17% (42/319) in the diagnosis of benign and
malignant thyroid nodules.
 | Table III.Performance comparison of
contrast-enhanced ultrasound in the diagnosis of benign and
malignant thyroid nodules. |
Table III.
Performance comparison of
contrast-enhanced ultrasound in the diagnosis of benign and
malignant thyroid nodules.
|
|
| Access speed | Peak time | Subsidence speed |
|---|
|
|
|
|
|
|
|---|
| Group | Nodule no. | Fast | Synchronous | Slow | Earlier | Synchronous | Later | Fast | Synchronous | Slow |
|---|
| Benign | 183 | 129 | 54 | 0 | 68 | 96 | 19 | 22 | 82 | 79 |
| Malignant | 136 | 4 | 42 | 90 | 18 | 32 | 86 | 120 | 14 | 2 |
| χ2 |
|
| 206.44 |
|
| 98.99 |
|
| 182.64 |
|
| P-value |
|
| 0.000 |
|
| 0.000 |
|
| 0.000 |
|
 | Table IV.Comparison of internal and boundary
enhancement characteristics between benign and malignant thyroid
nodules. |
Table IV.
Comparison of internal and boundary
enhancement characteristics between benign and malignant thyroid
nodules.
|
|
| Access manner | Peak intensity | Evenness | Annular
enhancement | Boundary after
CEUS |
|---|
|
|
|
|
|
|
|
|
|---|
| Group | No. | Centripetal | Pervasive | Low | Equal | High | Yes | No | Yes | No | Clear | Unclear |
|---|
| Benign | 183 | 11 | 172 | 11 | 51 | 121 | 165 | 18 | 69 | 114 | 141 | 42 |
| Malignant | 136 | 89 | 47 | 99 | 23 | 14 | 23 | 113 | 123 | 13 | 23 | 113 |
| χ2 |
| 128.00 |
| 162.33 |
| 172.93 | 90.49 | 112.90 |
| P-value |
| 0.000 |
| 0.000 |
| 0.000 | 0.000 | 0.000 |
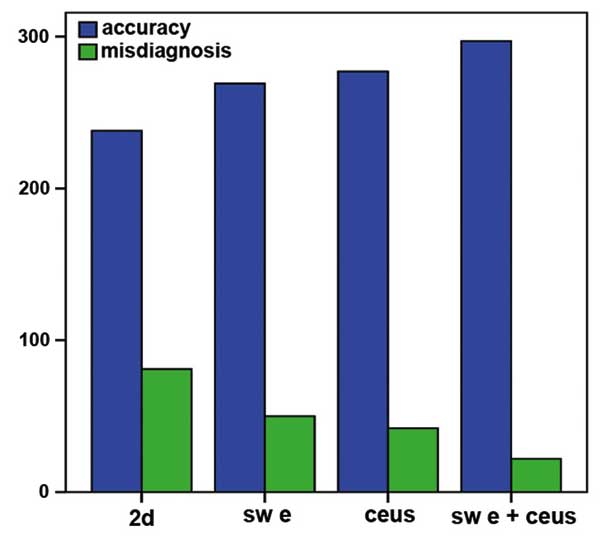
Performance comparison among 2DUS,
SWE, CEUS and their combined use in the diagnosis of benign and
malignant thyroid nodules (Table
IV)
When comparing 2DUS, SWE, CEUS and their combined
use, there were statistically significant differences in terms of
sensitivity, specificity and accuracy (χ2=9.220,15.310
and 40.296; P=0.000) in the diagnosis of malignant thyroid nodules;
however, there were no statistically significant differences in the
diagnosis of malignant thyroid nodules between SWE and CEUS in
terms of sensitivity, specificity or accuracy (χ2=0.737,
P=0.542). The combined use of SWE and CEUS exhibited statistically
significant differences compared with 2DUS, SWE or CEUS in terms of
sensitivity, specificity and accuracy (χ2=40.296, 12.264
and 6.939; P=0.000, 0.000 and 0.005, respectively) in the diagnosis
of malignant thyroid lesions. In addition, the combination of SWE
and CEUS was associated with a marked increase in accuracy and a
decrease in the misdiagnosis rate compared with 2DUS, SWE and CEUS
in the diagnosis of malignant thyroid nodules (Fig. 8).
Discussion
In recent years, as more individuals are subjected
to thyroid examination, the detection rate of thyroid nodules has
improved significantly, which is directly associated with surgical
decision-making. Conventional 2DUS detects thyroid nodules and
determines their nature through observation of their internal echo,
boundaries, shape, calcifications and growth manner (aspect ratio).
For example, malignant thyroid nodules are characterized by low
echogenicity, unclear boundaries, irregular shape, internal
calcification (particularly microcalcifications with a diameter of
<2 mm) and ‘vertical egg type’ growth with an aspect ratio of
≥1. Although 2DUS is able to discriminate between benign and
malignant thyroid nodules, its sensitivity of 71.32% (97/136),
specificity of 77.04% (141/183) and accuracy of 74.60% (238/319)
are relatively lower and more dependent on the examiner's
experience.
SWE is a type of elastography. By virtue of acoustic
radiation force impulse imaging and shear wave propagation, SWE
uses the probe to launch a series of pulse waves towards the region
of interest to display and quantify the hardness of tissues by
generating shear waves and measuring Young's modulus. The essence
of Young's modulus is the ratio of stress and strain, and its value
is proportional to the square of the shear wave speed. Within the
elastic limit of a target, the value is able to reflect tissue
elasticity. Therefore, this method has more advantages in terms of
objectivity and replicability, and has become a focus of research
(6–8). Normal thyroid tissues exhibit lower
hardness, which is subject to change when autoimmune or other
pathogenic processes alter the thyroid cells and tissues. As
thyroid tumors consist of more histological solid components but
less intercellular substance and have a tendency for pervasive
growth, they exhibit greater hardness and smaller elasticity upon
palpation, with a higher Young's modulus. This study demonstrated
that the Young's modulus of malignant nodules is higher compared
with that of benign nodules, and the difference was statistically
significant (t=11.932, P<0.05). Taking 29.52 kPa as the
threshold, those nodules with a value of ≥29.52 kPa were diagnosed
as malignant. SWE exhibited a sensitivity of 84.55% (115/136), a
specificity of 84.15% (154/183) and an accuracy of 84.32% (269/319)
in the diagnosis of malignant thyroid nodules, which was
significantly higher compared with that of 2DUS. This suggests that
real-time SWE technology is of great clinical value in the
diagnosis of benign and malignant thyroid nodules. However, this
technique is dependent upon the nodule, as well as the experience
of the examiner; therefore, some cases may be misdiagnosed.
CEUS has emerged as a major advance in the field of
medical US over the past decade. CEUS is a technology that enables
real-time observation of the status of the lesion and the blood
perfusion of its adjacent tissues through intravenous injection of
a US contrast agent under low mechanical index. CEUS has been
widely used in the examination of the liver, uterus, prostate and
other organs (9,10). With the upgrading of superficial
instrumentation and development of imaging techniques, clinical
applications of thyroid contrast US are also increasing (11–21). In
this study, the imaging of benign thyroid nodules shows that the
contrast agent enters the lesions and peaks earlier or
synchronically compared with the surrounding tissue, whereas its
subsidence occurs more slowly or synchronically compared with the
surrounding normal tissue. Furthermore, benign thyroid nodules
characteristically exhibit even internal echo, clear boundaries,
and annular, even and high enhancement (13–15,17,18); by
contrast, malignant nodules display ‘slow access and quick
subsidence’, early low enhancement (13–15,17–19),
non-homogeneous distribution of the contrast agent to the center
and the periphery, as well as unclear boundaries. Analysis of the
differences between benign and malignant nodules on contrast
imaging shows that they are mainly associated with the growth
pattern of the nodules.
Benign nodules, such as thyroid adenoma (22), mainly grow in an expansive manner,
gradually pushing the arteries and veins towards the periphery of
the tumor, with continuous growth of new capillaries as new
branches are needed. Therefore, the contrast agent reaches the
center of nodule slower compared with the normal surrounding
tissues. Likewise, the clearance of contrast agent is equally slow,
displaying a ‘fast-in and slow-out’ imaging pattern. With nodular
goiter and subacute thyroiditis (23), visible peripheral enhancement maybe
observed, as they are subject to repeated stimulation, which
renders the thyroid goitrous and its glands hyperplastic or
atrophic. Moreover, the interior of the gland in goiter and
subacute thyroiditis may suffer from necrosis due to a lack or
shortage of blood supply. While some cases only exhibit continued
low enhancement or no enhancement, the majority exhibit a tendency
of ‘fast in and slow-out’ enhancement, which poses a risk for
misdiagnosis.
The vascular structure of malignant nodules is very
complex and often dense at the periphery, but relatively sparse in
the central region, which explains why the blood supply of
malignant nodules exhibits centripetal enhancement. The invasive
growth of tumor tissue damages its surrounding tissue and new blood
vessels, causing thrombus formation, arteriovenous fistulas and
uneven distribution of blind-ended vessels. Larger malignant
nodules may develop internal bleeding and necrosis, with
coexistence of local abundance or shortage of blood supply. In
addition, the poor differentiation of vascular endothelial cells,
lack of muscle and nerve support, vascular dysfunction, continued
destruction of tumor cells, shortage of new blood vessels,
particularly lack of blood supply due to insufficient
neovascularization in smaller nodules, may lead to low enhancement
of the contrast agent (14–15,23).
CEUS has a sensitivity of 87.5% (119/136), a specificity of 86.33%
(158/183) and an accuracy of 86.83% (294/319) in the diagnosis of
benign and malignant thyroid nodules.
Although CEUS exhibits high sensitivity and
specificity, there remains a missed diagnosis rate of 12.5%
(17/136) and a misdiagnosis rate of 13.67% (25/183). Regarding the
17 missed cases, the present study found that the majority of
papillary thyroid tumors exhibit low enhancement and early low
enhancement, but there are certain cases of equal enhancement
(n=14) and high enhancement (n=3). Further pathological analysis
confirmed 9 papillary carcinomas, 5 medullary carcinomas and 3
follicular carcinomas. The missed diagnosis may be attributed to
the strong aggressiveness and rapid growth of the malignant part of
the thyroid, as is suggested by adequate internal blood supply on
contrast imaging. Of the 25 misdiagnosed cases of low-enhancing
nodules, 18 were nodular goiter, 3 were chronic lymphocytic
thyroiditis, 1 was a nodular goiter with degeneration (fibrosis,
collagenous changes, calcification and hemorrhage) and 3 were
subacute thyroiditis. Misdiagnosis is closely associated with the
enhancement mode and pathological changes of the thyroid nodules.
Benign thyroid nodules are prone to hemorrhage, cystic degeneration
and calcification, which may lead to pathological structural
changes. When examined by CEUS, they exhibit low enhancement, no
enhancement or local non-enhancement; thus, the enhancement pattern
may vary. However, CEUS has a good sensitivity in displaying
internal nodular hemorrhage, cystic degeneration and necrotic
areas.
Diagnosis using SWE and CEUS in the examination of
malignant thyroid nodules shows no statistically significant
difference in terms of sensitivity, specificity or accuracy.
Nevertheless, SWE may demonstrate the hardness of nodules, whereas
CEUS may illustrate blood supply, which adds information to the
two-dimensional image of the nodules and evidence regarding the
nature of the nodule. The combined use of SWE and CEUS was able to
significantly increase the sensitivity, specificity and accuracy of
diagnosis compared with 2DUS, SWE and CEUS (P<0.05), suggesting
that this combination enhances the credibility of the diagnosis of
malignant thyroid nodules.
In conclusion, compared with 2DUS, SWE and CEUS, the
combined use of the latter two exhibits higher sensitivity,
specificity and accuracy in the diagnosis of malignant thyroid
nodules and the differences are statistically significant. However,
two-dimensional inspection should not be omitted and, as the
combination significantly increases sensitivity, specificity and
accuracy in the diagnosis of malignant nodules, it maybe used as a
follow-up step for further diagnosis of suspicious nodules, as it
helps improve the reliability and reduce the rate of missed
diagnosis. In case of diagnostic inconsistencies between CEUS and
SWE, further fine-needle aspiration biopsy maybe applied to improve
diagnostic accuracy.
References
|
1
|
American Thyroid Association (ATA)
Guidelines Taskforce on Thyroid Nodules and Differentiated Thyroid
Cancer, ; Cooper DS, Doherty GM, Haugen BR, Kloos RT, Lee SL,
Mandel SJ, Mazzaferri EL, McIver B, Pacini F, et al: Revised
American thyroid association management guidelines for patients
with thyroid nodules and differentiated thyroid cancer. Thyroid.
19:1167–1214. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Pellegriti G, Frasca F, Regalbuto C,
Squatrito S and Vigneri R: Worldwide increasing incidence of
thyroid cancer: Update on epidemiology and risk factors. J Cancer
Epidemiol. 2013:9652122013.PubMed/NCBI
|
|
3
|
Henrichsen TL and Reading CC: Thyroid
ultrasonography. Part 2: Nodules. Radiol Clin North Am. 49:417–424.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Zeng RC, Zhang W, Gao EL, Cheng P, Huang
GL, Zhang XH and Li Q: Number of central lymph node metastasis for
predicting lateral lymph node metastasis in papillary thyroid
microcarcinoma. Head Neck. 36:101–106. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Sherman SI, Angelos P, Ball DW, Beenken
SW, Byrd D, Clark OH, Daniels GH, Dilawari RA, Ehya H, Farrar WB,
et al: Thyroid carcinoma. J Natl Compr Canc Netw. 3:404–457.
2005.PubMed/NCBI
|
|
6
|
Gweon HM, Youk JH, Son EJ and Kim JA:
Visually assessed colour overlay features in shear wave
elastography for breast masses: Quantification and diagnostic
performance. Eur Radiol. 23:658–663. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Ferraioli G, Tinelli C, Zicchetti M, Above
E, Poma G, Di Gregorio M and Filice C: Reproducibility of real-time
shear wave elastography in the evaluation of liver elasticity. Eur
J Radiol. 81:3102–3106. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Woo S, Kim SY, Cho JY and Kim SH: Shear
wave elastography for detection of prostate cancer: A preliminary
study. Korean J Radiol. 15:346–355. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Pop CM, Mihu D and Badea R: Role of
contrast-enhanced ultrasound (CEUS) in the diagnosis of endometrial
pathology. Clujul Med. 88:433–437. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Lin Q, Lv F, Luo Y, Song Q, Xu Q, Su Y,
Tang Y and Tang J: Contrast-enhanced ultrasound for evaluation of
renal trauma during acute hemorrhagic shock: A canine model. J Med
Ultrason (2001). 42:199–205. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Kim BK, Choi YS, Kwon HJ, Lee JS, Heo JJ,
Han YJ, Park YH and Kim JH: Relationship between patterns of
calcification in thyroid nodules and histopathologic findings.
Endocr J. 60:155–160. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Bartolotta TV, Midiri M, Galia M, Runza G,
Attard M, Savoia G, Lagalla R and Cardinale AE: Qualitative and
quantitative evaluation of solitary thyroid nodules with
contrast-enhanced ultrasonography: Initial results. Eur Radiol.
16:2234–2241. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Zhang B, Jiang YX, Liu JB, Yang M, Dai Q,
Zhu QL and Gao P: Utility of contrast-enhanced ultrasound for
evaluation of thyroid nodules. Thyroid. 20:51–57. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Ma JJ, Ding H, Xu BH, Xu C, Song LJ, Huang
BJ and Wang WP: Diagnostic performances of various gray-scale,
color Doppler, and contrast-enhanced ultrasonography fidings in
predicting malignant thyroid nodules. Thyroid. 24:355–363. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Cantisani V, Consorti F, Guerrisi A,
Guerrisi I, Ricci P, Di Segni M, Mancuso E, Scardella L, Milazzo F,
D'Ambrosio F and Antonaci A: Prospective comparative evaluation of
quantitative-elastosonography (Q-elastography) and
contrast-enhanced ultrasound for the evaluation of thyroid nodules:
Preliminary experience. Eur J Rsdiol. 82:1892–1898. 2013.
View Article : Google Scholar
|
|
16
|
Moon WJ, Jung SL, Lee JH, Na DG, Baek JH,
Lee YH, Kim J, Kim HS, Byun JS and Lee DH: Thyroid Study Group,
Korean Society of Neuro- and Head and Neck Radiology: Benign and
malignant thyroid nodules: US differentiation-multicenter
retrospective study. Radiology. 247:762–770. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Hong YR, Yan CX, Mo GQ, Luo ZY, Zhang Y,
Wang Y and Huang PT: Conventional US, elastopraphy, and contrast
enhanced US features of papillary thyroid microcarcinoma predict
cental compartment lymph node matastases. Sci Rep. 5:77482015.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Oyedeji F, Giampoli E, Ginat D and Dogra
V: The sonographic appearance of benign and malignant thyroid
diseases and their histopathology correlate:Demystifying the
thyroid nodule. Ultrasound Q. 29:161–178. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Li F and Luo H: Comparative study of
thyroid puncture biopsy guided by contrast-enhanced ultrasonography
and conventional ultrasonography. ExpTher Med. 5:1381–1384.
2013.
|
|
20
|
Giusti M, Orlandi D, Melle G, Massa B,
Silvestri E, Minuto F and Turtulici G: Is there a real diagnostic
impact of elastosonography and contrast-enhanced ultrasonography in
the management of thyroid nodules? J Zhejiang Univ Sci B.
14:195–206. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Nemec U, Nemec SF, Novotny C, Weber M,
Czerny C and Krestan CR: Quantitative evaluation of
contrast-enhanced ultrasonography after intravenous administration
of a microbubble contrast agent for differentiation of benign and
malignant thyroid nodules: Assessment of diagnostic accuracy. Eur
Radiol. 22:1357–1365. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Jiang J, Huang L, Zhang H, Ma W, Shang X,
Zhou Q, Gao Y, Yu S and Qi Y: Contrast-enhanced sonography of
thyroid nodules. J Clin Ultrasound. 43:153–156. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Friedrich-Rust M, Sperber A, Holzer K,
Diener J, Grünwald F, Badenhoop K, Weber S, Kriener S, Herrmann E,
Bechstein WO, et al: Real-time elastography and contrast-enhanced
ultrasound for the assessment of thyroid nodules. Exp Clin
Endocrinol Diabetes. 118:602–609. 2010. View Article : Google Scholar : PubMed/NCBI
|