Introduction
Gastric cancer with peritoneal metastases has a poor
prognosis (1). S-1 plus cisplatin is
widely administered for metastatic or unresectable gastric cancer
and is considered to be the standard first-line regimen in Japan
(2). Recently, intravenous (IV) and
intraperitoneal (IP) administration of paclitaxel (PTX) with S-1 is
showing promising results for gastric cancer with peritoneal
metastases (3). However, it remains
unclear whether conversion of unresectable gastric cancer to
resectable disease is possible with this combination chemotherapy.
We herein present a case of a successful conversion therapy using a
combination of systemic and IP chemotherapy, followed by ovarian
metastasectomy and primary tumor resection.
Case report
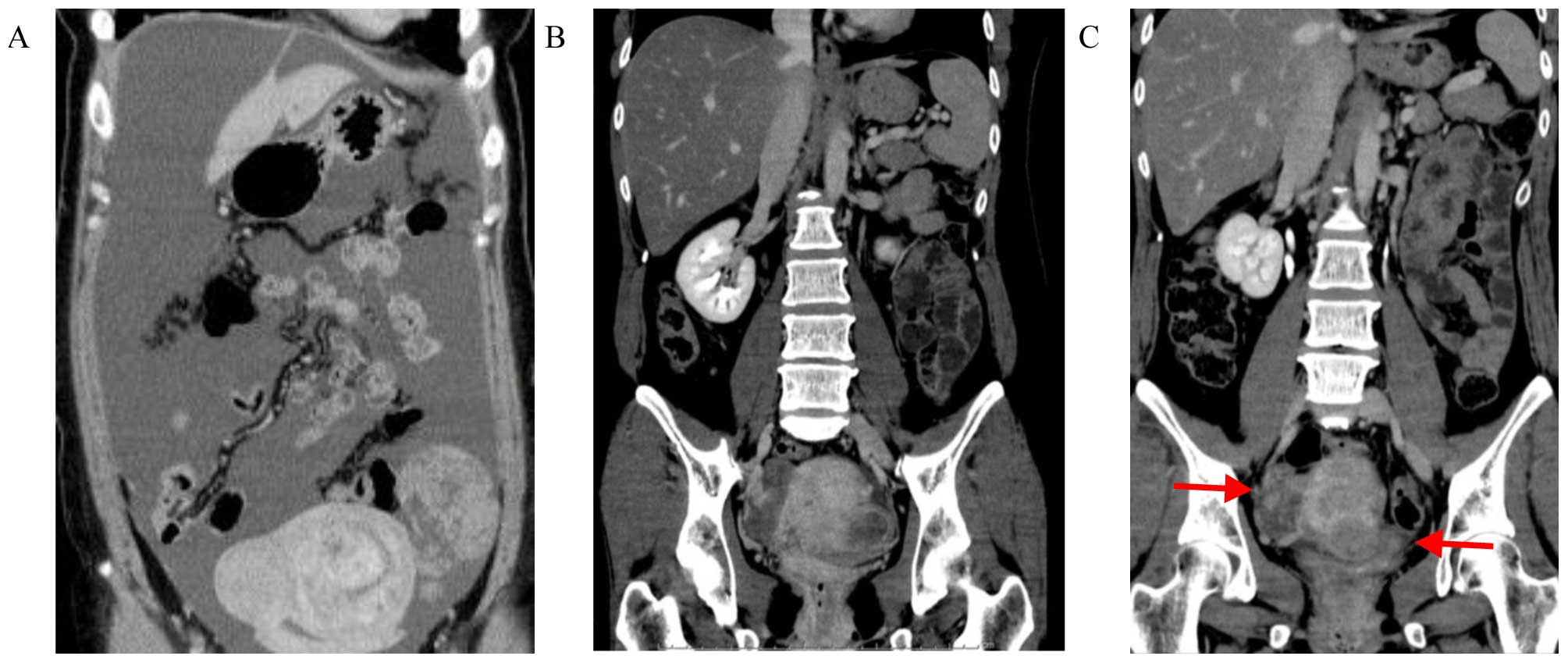
A 39-year old woman presented with abdominal
distention and pain. The patient was diagnosed with advanced
gastric cancer with pulmonary metastases, massive malignant ascites
and bilateral ovarian metastases (Fig.
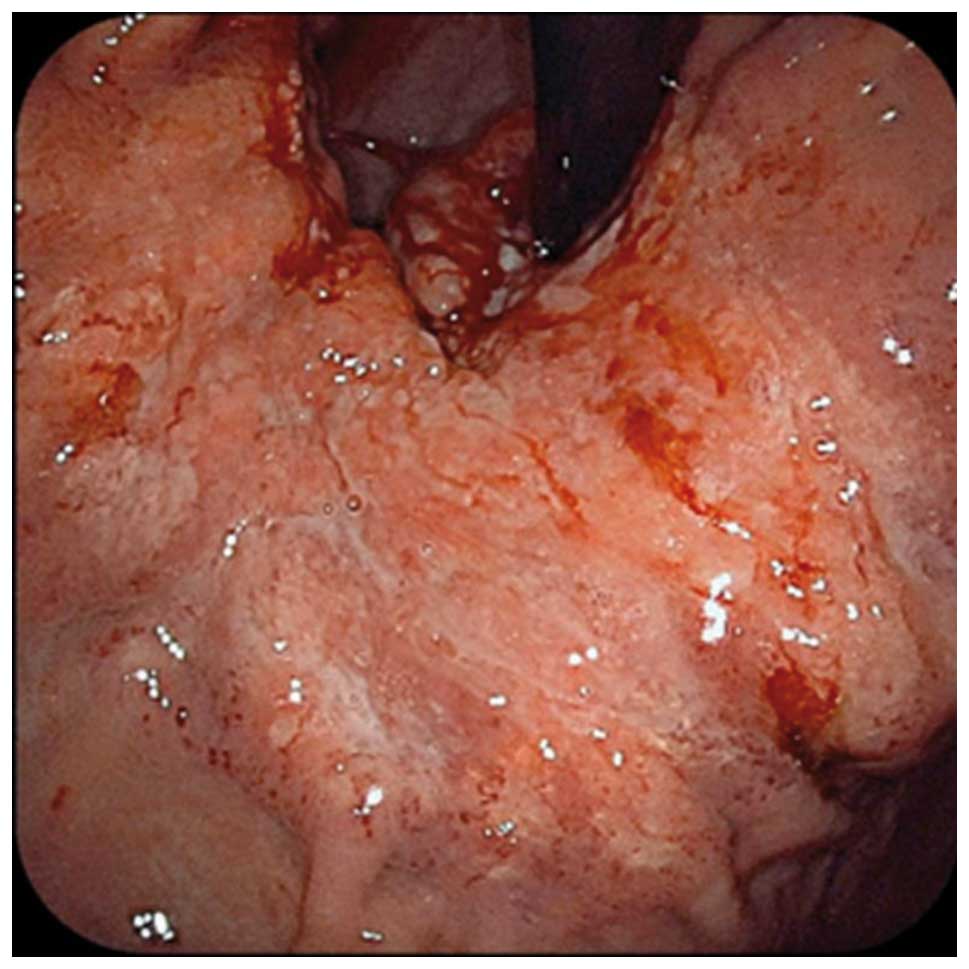
1A). Gastrointestinal endoscopy revealed a Borrmann type IV
tumor and the biopsy revealed poorly differentiated adenocarcinoma
overexpressing the human epidermal growth factor receptor 2 (HER-2)
protein (3+) (Fig. 2). Triweekly SPT
therapy was administered, which consisted of oral S-1, IV cisplatin
and IV trastuzumab (4). After 2
cycles of the therapy, computed tomography (CT) and
gastrointestinal endoscopy revealed disappearance of the malignant
ascites and complete response of the pulmonary metastases (Fig. 1B). After an additional 4 cycles of
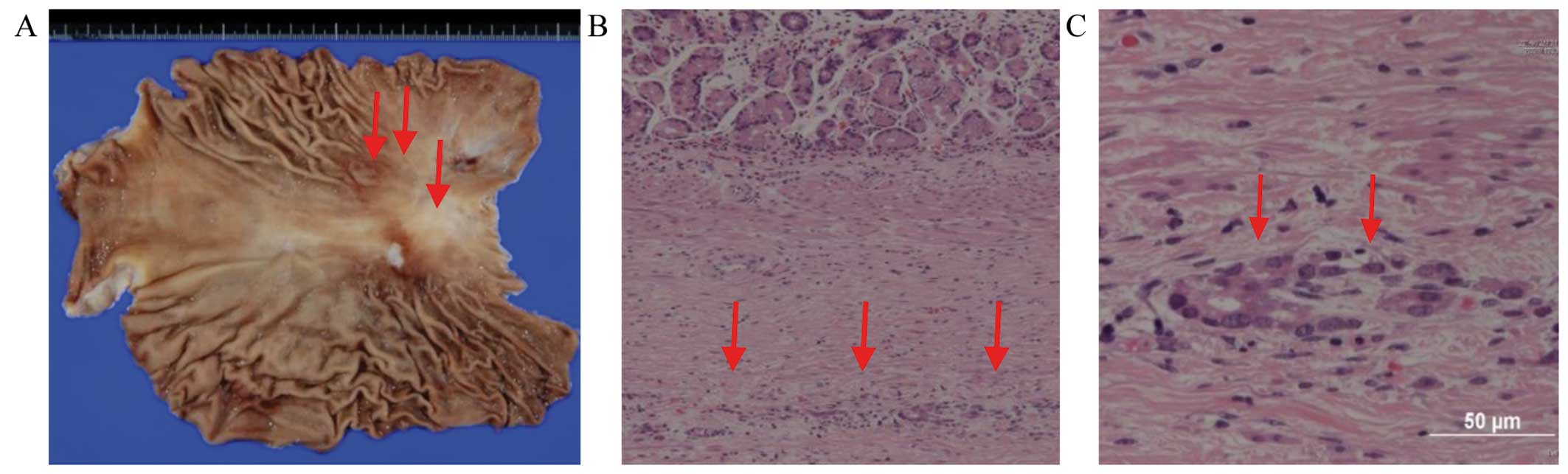
the SPT therapy, diagnostic laparoscopy was conducted. As residual
peritoneal metastases were found, a peritoneal access device was
implanted in the right lower abdomen wall and a catheter was placed
in the pelvic cavity (Fig. 3A).
Therapy was then switched to IV and IP PTX with S-1 and
trastuzumab. The regimen was as follows: S-1 80
mg/m2/day for 14 consecutive days followed by 7 days of
rest, IV PTX at 50 mg/m2 and IP PTX at 20
mg/m2 on days 1 and 8, and triweekly IV trastuzumab at
the standard dose on day 1. Gastrointestinal endoscopy and CT after
11 cycles of this combination chemotherapy confirmed no progression
of the primary lesion and metastatic disease (Fig. 1C). Secondary laparoscopy revealed
multiple white nodules without evidence of malignancy and
peritoneal lavage cytology was negative. Bilateral ovarian
metastasectomy was conducted in order to prevent ovarian torsion
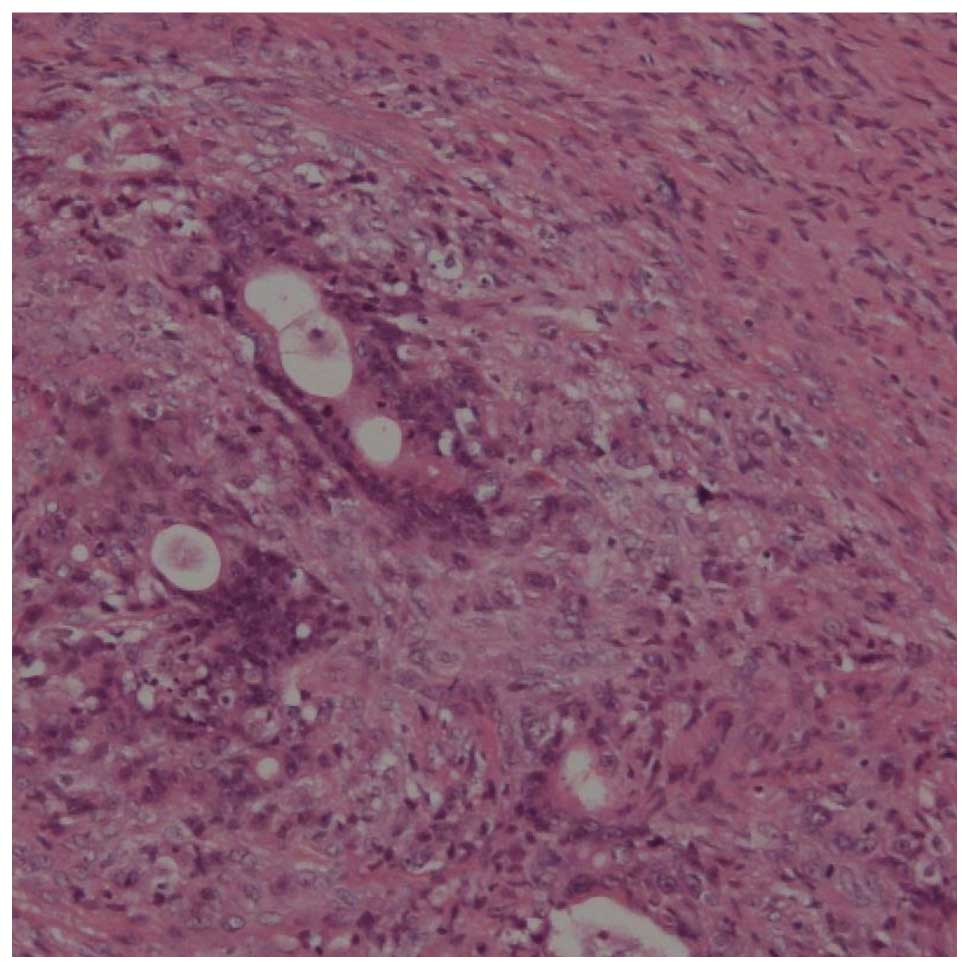
due to the extensive metastases. The pathological examination
revealed residual ovarian metastatic disease with overexpression of
the HER-2 protein (3+) (Fig. 4).
Following ovariectomy, 4 additional cycles of the systemic and IP
chemotherapy were administered. As no obvious non-curative factors
were identified, laparoscopic total gastrectomy was performed after
pathologically re-confirming disappearance of the peritoneal
metastases and negative peritoneal lavage cytology (Fig. 3B). The postoperative course was
uneventful.
The final diagnosis revealed minute residual tumor
cell nests at the primary site (stomach) with overexpression of
HER-2 (3+) (Fig. 5). The
pathological diagnosis was as follows: U, Less, ypType4, por2,
ypT2, sci, INFc, ly0, v0, ypN0 (0/41), pPM0 (12 mm), pDM0 (147 mm),
histological grade 2 according to the Third Edition of Japanese
Classification of Gastric Carcinoma (5). The patient continued the combination
chemotherapy with S-1 and IP PTX (changed from the original IV and
IP paclitaxel) with trastuzumab for 1 year after the gastrectomy,
suffering mild adverse effects, such as low-grade anorexia.
Chemotherapy was then discontinued according to the patient's
wishes, and the patient developed no recurrence for 16 months from
the gastrectomy and 33 months from diagnosis. However, 4 months
after discontinuing chemotherapy, isolated para-aortic lymph node
recurrence was detected.
Discussion
Based on this case, two important clinical issues
must be discussed: First, a satisfactory response to systemic and
IP chemotherapy may convert unresectable gastric cancer with
peritoneal metastases to resectable disease. Primary tumor
resection and ovarian metastasectomy may prolong patient survival
if the combination chemotherapy is sufficiently effective and there
are no unresectable metastases.
The disease responded well to systemic and IP
chemotherapy and was converted from unresectable to resectable. The
ability of IP PTX to maintain a high concentration for prolonged
periods of time contributed to the high antitumor effect against
peritoneal metastases, and the tumor responded well to the drug
combination of IV and IP PTX with S-1 and trastuzumab. A phase II
trial demonstrated that IV and IP PTX with S-1 were well-tolerated
and highly effective in gastric cancer patients with peritoneal
metastases (3). The 1-year overall
survival rate was 77%, and malignant ascites disappeared or was
reduced in 15 of 22 (68%) patients. PTX is an effective agent for
gastric cancer, with a relatively good response of diffuse-type
adenocarcinoma, which accounts for the majority of peritoneal
metastases of this disease (6). IP
administration of PTX was developed to reinforce the drug effect on
peritoneal metastases (7). This is
accomplished by allowing PTX to act directly on nodules at a high
concentration. When PTX is administered IP, it is absorbed slowly
due to its high molecular weight and lipophilic properties. IP PTX
is also considered to have a mild toxicity profile (7,8). IP
administration of PTX has been used together with systemic
chemotherapy for peritoneal metastases of ovarian cancer, where it
has demonstrated significant survival benefits (9). Additionally, S-1 is an oral 5-FU agent
that has been shown to be non-inferior to infusional 5-FU in terms
of overall survival in Japanese patients with metastatic gastric
cancer; furthermore, trastuzumab in combination with standard
cytotoxic chemotherapy for this disease improved overall survival
for patients with HER2-positive disease (10,11). The
tumor responded well to the combination of IV and IP PTX with S-1
and trastuzumab. This combination chemotherapy was able to convert
unresectable to resectable disease; however, its viability has not
been sufficiently confirmed. Conversion therapy was originally
well-established in colon cancer management (12); in gastric cancer, it was recently
considered beneficial in some cases with effective chemotherapy and
negative peritoneal washing cytology (13). If peritoneal metastases are
controlled well over a long time period, primary tumor resection
appears to prolong survival. In fact, almost all peritoneal
metastases in this case visibly disappeared with this combination
chemotherapy.
The second clinical issue is that primary tumor
resection and ovarian metastasectomy may prolong survival in
gastric cancer patients with peritoneal metastases if systemic and
IP chemotherapy is sufficiently effective without unresectable
metastases. Kitayama et al suggested criteria for primary tumor
resection with IV and IP PTX with S-1 in gastric cancer (14). The criteria are as follows: i) No
distant metastases except in the peritoneal area, including the
ovary; ii) negative peritoneal cytology; and iii) metastatic
nodules in the peritoneal cavity visibly reduced or controlled. Of
the 64 patients with severe peritoneal metastases and ascites,
gastrectomy was performed in 34 patients. The median survival time
of the gastrectomized patients was 26.4 months, whereas that of the
30 patients who did not undergo gastrectomy was 12.1 months. Other
retrospective studies demonstrated that gastrectomy and
metastasectomy, including ovariectomy, may improve survival
(15,16). Peng et al reported that gastrectomy
and absence of ascites were the two independent prognostic factors
associated with longer survival in gastric cancer (16). In addition, for colorectal cancer
with peritoneal metastases, the presence of ovarian metastases did
not affect prognosis in patients undergoing complete cytoreductive
surgery with IP chemotherapy (17).
Removing microscopic residual tumor is the expected effect of the
surgery. In a mouse model, IP PTX penetrates only 100–200 µm under
the surface of the disseminated tumor, and its effect against
massive metastases is limited (18,19).
Moreover, although IV and IP PTX with S-1 was highly effective,
grade 2 and 3 histological response was only obtained in 7 (21%)
and 1 (3%) patients, respectively (14). Surgical resection of extensive
residual disease is required to achieve a disease-free status, as
pathological complete response in gastric cancer is rare, even with
highly effective chemotherapy. If systemic and IP chemotherapy
effectively control peritoneal metastases over a long period of
time, primary tumor resection and ovarian metastasectomy appear to
prolong survival.
In summary, satisfactory response to IV and IP PTX
with S-1 and trastuzumab was able to convert unresectable gastric
cancer with peritoneal metastases to resectable disease, and
primary tumor resection with ovarian metastasectomy may also
prolong survival in such patients. This combination chemotherapy
has the potential to become a conversion therapy for gastric cancer
with peritoneal metastases, even if ascites and ovarian metastases
are extensive. As the optimal surgical procedure has not yet been
determined in such patients, further investigation is required to
determine the optimal treatment strategy for gastric cancer with
peritoneal metastases.
Acknowledgements
The authors would like to thank the patient for her
kind cooperation, and David Hochman for reviewing the language of
our article.
References
|
1
|
Sadeghi B, Arvieux C, Glehen O, Beaujard
AC, Rivoire M, Baulieux J, Fontaumard E, Brachet A, Caillot JL,
Faure JL, et al: Peritoneal carcinomatosis from non-gynecologic
malignancies: Results of the EVOCAPE 1 multicentric prospective
study. Cancer. 88:358–363. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Koizumi W, Narahara H, Hara T, Takagane A,
Akiya T, Takagi M, Miyashita K, Nishizaki T, Kobayashi O, Takiyama
W, et al: S-1 plus cisplatin versus S-1 alone for first-line
treatment of advanced gastric cancer (SPIRITS trial): A phase III
trial. Lancet Oncol. 9:215–221. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Yamaguchi H, Kitayama J, Ishigami H, Emoto
S, Yamashita H and Watanabe T: A phase 2 trial of intravenous and
intraperitoneal paclitaxel combined with S-1 for treatment of
gastric cancer with macroscopic peritoneal metastasis. Cancer.
119:3354–3358. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Kurokawa Y, Sugimoto N, Miwa H, Tsuda M,
Nishina S, Okuda H, Imamura H, Gamoh M, Sakai D, Shimokawa T, et
al: Phase II study of trastuzumab in combination with S-1 plus
cisplatin in HER2-positive gastric cancer (HERBIS-1). Br J Cancer.
110:1163–1168. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Japanese Gastric Cancer Association, .
Japanese classification of gastric carcinoma: 3rd English edition.
Gastric Cancer. 14:101–112. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Yamada Y, Shirao K, Ohtsu A, Boku N, Hyodo
I, Saitoh H, Miyata Y and Taguchi T: Phase II trial of paclitaxel
by three-hour infusion for advanced gastric cancer with short
premedication for prophylaxis against paclitaxel-associated
hypersensitivity reactions. Ann Oncol. 12:1133–1137. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Markman M, Rowinsky E, Hakes T, Reichman
B, Jones W, Lewis JL Jr, Rubin S, Curtin J, Barakat R, Phillips M,
et al: Phase I trial of intraperitoneal taxol: A Gynecoloic
Oncology Group study. J Clin Oncol. 10:1485–1491. 1992.PubMed/NCBI
|
|
8
|
Gelderblom H, Verweij J, van Zomeren DM,
Buijs D, Ouwens L, Nooter K, Stoter G and Sparreboom A: Influence
of Cremophor El on the bioavailability of intraperitoneal
paclitaxel. Clin Cancer Res. 8:1237–1241. 2002.PubMed/NCBI
|
|
9
|
Armstrong DK, Bundy B, Wenzel L, Huang HQ,
Baergen R, Lele S, Copeland LJ, Walker JL and Burger RA:
Gynecologic Oncology Group: Intraperitoneal cisplatin and
paclitaxel in ovarian cancer. N Engl J Med. 354:34–43. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Boku N, Yamamoto S, Fukuda H, Shirao K,
Doi T, Sawaki A, Koizumi W, Saito H, Yamaguchi K, Takiuchi H, et
al: Gastrointestinal Oncology Study Group of the Japan Clinical
Oncology Group: Fluorouracil versus combination of irinotecan plus
cisplatin versus S-1 in metastatic gastric cancer: A randomised
phase 3 study. Lancet Oncol. 10:1063–1069. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Bang YJ, Van Cutsem E, Feyereislova A,
Chung HC, Shen L, Sawaki A, Lordick F, Ohtsu A, Omuro Y, Satoh T,
et al: ToGA Trial Investigators: Trastuzumab in combination with
chemotherapy versus chemotherapy alone for treatment of
HER2-positive advanced gastric or gastro-oesophageal junction
cancer (ToGA): A phase 3, open-label, randomised controlled trial.
Lancet. 376:687–697. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Power DG and Kemeny NE: Chemotherapy for
the conversion of unresectable colorectal cancer liver metastases
to resection. Crit Rev Oncol Hematol. 79:251–264. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Yoshida K, Yamaguchi K, Okumura N,
Tanahashi T and Kodera Y: Is conversion therapy possible in stage
IV gastric cancer: The proposal of new biological categories of
classification. Gastric Cancer. 19:329–338. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Kitayama J, Ishigami H, Yamaguchi H,
Yamashita H, Emoto S, Kaisaki S and Watanabe T: Salvage gastrectomy
after intravenous and intraperitoneal paclitaxel (PTX)
administration with oral S-1 for peritoneal dissemination of
advanced gastric cancer with malignant ascites. Ann Surg Oncol.
21:539–546. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Kim KH, Lee KW, Baek SK, Chang HJ, Kim YJ,
Park DJ, Kim JH, Kim HH and Lee JS: Survival benefit of gastrectomy
± metastasectomy in patients with metastatic gastric cancer
receiving chemotherapy. Gastric Cancer. 14:130–138. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Peng W, Hua RX, Jiang R, Ren C, Jia YN, Li
J and Guo WJ: Surgical treatment for patients with Krukenberg tumor
of stomach origin: Clinical outcome and prognostic factors
analysis. PLoS One. 8:e682272013. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Eveno C, Goéré D, Dartigues P, Honoré C,
Dumont F, Tzanis D, Benhaim L, Malka D and Elias D: Ovarian
metastasis is associated with retroperitoneal lymph node relapses
in women treated for colorectal peritoneal carcinomatosis. Ann Surg
Oncol. 20:491–496. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Soma D, Kitayama J, Konno T, Ishihara K,
Yamada J, Kamei T, Ishigami H, Kaisaki S and Nagawa H:
Intraperitoneal administration of paclitaxel solubilized with
poly(2-methacryloxyethyl phosphorylcholine-co n-butyl methacrylate)
for peritoneal dissemination of gastric cancer. Cancer Sci.
100:1979–1985. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Kamei T, Kitayama J, Yamaguchi H, Soma D,
Emoto S, Konno T, Ishihara K, Ishigami H, Kaisaki S and Nagawa H:
Spatial distribution of intraperitoneally administrated paclitaxel
nanoparticles solubilized with poly (2-methacryloxyethyl
phosphorylcholine-co n-butyl methacrylate) in peritoneal metastatic
nodules. Cancer Sci. 102:200–205. 2011. View Article : Google Scholar : PubMed/NCBI
|