Introduction
Population aging has become a worldwide problem in
recent decades, and the increasing number of elderly patients has
resulted in an increase in the mean age of cancer patients.
Consequently, the number of operations performed on elderly
patients is increasing. In the Japanese population, the overall
incidence of hepatocellular carcinoma (HCC) has decreased due to
the decreasing incidence of hepatitis C virus (HCV), while the rate
of HCC in the absence of HCV, and of liver metastasis from colon
cancer, has increased (1–3). The average age of patients undergoing
hepatic resection has increased due to population aging (1). Several studies have reported on the
usefulness and safety of hepatic resection for elderly patients: No
differences in complications or prognosis were observed between
this population and younger patients (2,3). Only a
few studies have reported problems associated with hepatic
resection in elderly patients (4,5). In
addition, most reports on hepatic resection for elderly patients
have included patients aged 70–75 years as elderly patients, and
there have been few studies involving patients aged ≥80 years. The
present study sought to clarify whether hepatic resection is
feasible in older patients, including those >80 years of age,
and to consider whether it would be feasible to undertake
peri-operative management in elderly and young patients. The aim of
the present study was therefore to determine the
clinicopathological features, benefits and problems associated with
hepatic resection in patients aged ≥80 years.
Patients and methods
Patients
Between January 2006 and December 2013, 395 patients
with HCC underwent hepatic resection at the Department of Surgery
(Kansai Medical University, Osaka, Japan). The patients were
divided into two groups according to their age: Those <80 years
of age (n=351) and those ≥80 years of age (n=44). All patients
provided written informed consent prior to treatment and the study
was approved by the institutional review board of our hospital
(Kansai Medical University, Osaka, Japan).
Methods
The following pre-operative characteristics were
compared among the two age groups: Patient age; gender; presence of
diabetes, hypertension, alcohol abuse; presence of absence of HCV;
platelet count; prothrombin activity; levels of aspartate
aminotransferase, alanine aminotransferase, alkaline phosphatase,
gamma-glutamyl transpeptidase, albumin, total bilirubin, C-reactive
protein (CRP), cholinesterase, α-fetoprotein (AFP) and
des-gamma-carboxy prothrombin (DCP); indocyanine green retention
rate at 15 min (ICGR-15); and Child-Pugh classification. Tumor
characteristics, including the maximum tumor size, tumor number,
tumor stage and differentiation were compared between the two
groups. Furthermore, operative factors and complications, including
operative method, operation time, intraoperative bleeding,
allogeneic transfusion, portal vein tumor thrombosis, background
liver condition, post-hepatectomy liver failure (PHLF), bile
leakage, as well as the mortality rate were also compared between
the two groups.
Patients receiving subcutaneous insulin injections
and/or taking oral anti-diabetic drugs were classified as diabetic.
Patients taking anti-hypertensive drugs were classified as having
hypertension. Alcohol abuse was defined as the consumption of
>20 g per day of alcohol for at least 1 year. Patients with
hepatitis B and/or C were identified based on positivity for the
respective surface antigen, while patients negative for the two
were regarded as non-B non-C (NBNC). Hepatic resection included
trisegmentectomy, lobectomy, segmentectomy and subsegmentectomy,
while partial resection was performed when resectability was
limited. Tumor differentiation, presence of portal vein tumor
thrombus and background liver condition were determined based on
pathological findings. Background liver condition was classified as
liver cirrhosis with chronic hepatitis or normal liver. Liver
cirrhosis was defined as stage F4 according to the METAVIR
classification (6). The tumor stage
was determined according to the Tumor-Lymph Nodes-Metastasis (TNM)
classification (7) and PHLF
according to the guidelines of the International Study Group of
Liver Surgery (8). Bile leakage was
defined as continuous gross bile drainage lasting ≥3 days and
drain-fluid bilirubin levels as >3 times the serum bilirubin
levels or drain-fluid bilirubin levels of ≥5 mg/dl. Complications
were defined as grade II and higher according to the Cavien-Dindo
classification. Recurrence-free survival and cumulative survival
rates were compared between the groups. In addition, the
independent risk factors for survival in each group were
investigated. Albumin, cholinesterase and CRP levels were measured
1 day before surgery and 1, 3, 7, 30 and 90 days after surgery.
Improvements in these parameters were compared between the
groups.
Statistical analysis
The Mann-Whitney U-test was used to evaluate
continuous variables and the chi-square test was used to evaluate
numerical variables in the univariate analysis. Kaplan-Meier
analysis and the log-rank test were performed to examine cumulative
survival and recurrence-free survival rates. To examine prognostic
factors, each patient group was divided into two subgroups
according to the median of continuous variables; univariate
analysis with log-rank test was performed for these subgroups. Cox
regression analysis was used for multivariate analysis.
Multivariate analysis was performed for factors with P<0.05
according to univariate analysis. All analyses were performed with
JMP version 9.0.2 (SAS Institute, Cary, NC, USA). P<0.05 was
considered to indicate a statistically significant difference
between values.
Results
Patient characteristics
The patients' background characteristics are listed
in Table I. The mean patient age was
67.4±8.9 years in the younger group and 83.0±2.9 years in the older
group. There were no significant differences in the prevalence of
diabetes, hypertension or alcohol abuse between the groups.
However, there were significant differences in certain factors
associated with the etiology of HCC. The older group contained
significantly less cases with NBNC status than the younger group
(32 vs. 52%; P<0.01). Factors associated with background liver
function were similar between the groups, with the exception of
prothrombin activity (87.7±13.6% in the younger group vs.
91.8±11.5% in the older group; P=0.04). AFP levels, used as a tumor
marker, were similar in the two groups; however, DCP levels in the
younger group were higher compared with those in the older group
(P=0.03).
 | Table I.Patient background characteristics
according to age group. |
Table I.
Patient background characteristics
according to age group.
| Characteristic | Patients aged <80
years (n=351) | Patients aged ≥80
years (n=44) | P-value |
|---|
| Age (years) | 67.4±8.9 | 83.0±2.9 | <0.01 |
| Gender (male), n
(%) | 260 (74) | 29 (66) | 0.24 |
| BMI
(kg/m2) | 23.4±3.3 | 22.0±2.9 | 0.04 |
| Diabetes, n (%) | 102 (29) | 9 (20) | 0.23 |
| Hypertension, n
(%) | 142 (40) | 20 (45) | 0.52 |
| Alcohol abuse, n
(%) | 113 (32) | 8 (18) | 0.06 |
| Hepatitis B, n
(%) | 42 (12) | 1 (2) | 0.05 |
| Hepatitis C, n
(%) | 198 (56) | 20 (45) | 0.16 |
| NBNC, n (%) | 111 (32) | 23 (52) | <0.01 |
| Platelet count
(104/µl) | 17.3±8.4 | 18.8±7.8 | 0.15 |
| Prothrombin activity
(%) | 87.7±13.6 | 91.8±11.5 | 0.04 |
| AST (IU/l) | 42.6±25.7 | 41.5±22.1 | 0.91 |
| ALT (IU/l) | 39.8±31.7 | 32.5±24.6 | 0.06 |
| ALP (IU/l) | 324±199 | 342±185 | 0.21 |
| γ-GTP (IU/l) | 89±97 | 80±67 | 0.41 |
| Albumin (g/dl) | 3.8±0.5 | 3.7±0.4 | 0.45 |
| Total bilirubin
(mg/dl) | 0.7±0.3 | 0.6±0.2 | 0.06 |
| CRP (mg/dl) | 0.5±1.4 | 0.6±1.5 | 0.77 |
| Cholinesterase
(IU/l) | 226±75 | 212±59 | 0.24 |
| ICGR 15 (%) | 16.8±11.9 | 15.6±7.3 | 0.65 |
| Child-Pugh
classification (A/B) | 319/32 | 40/4 | 0.99 |
| AFP (ng/ml) | 2,998±15,724 | 7,793±41,815 | 0.94 |
| DCP (mAU/ml) | 4,606±14,908 | 6,585±17,309 | 0.03 |
| Cardiovascular
diseases, n (%) | 37 (11) | 6 (14) | 0.60 |
| Pulmonary diseases,
n (%) | 20 (6) | 6 (14) | 0.05 |
Tumor characteristics, operative
factors and complications
Table II shows tumor
and operative factors according to the age group. The maximum tumor
size was 4.7±4.4 cm in the younger group and 6.4±7.5 cm in the
older group (P=0.02). The rate of pathologically diagnosed liver
cirrhosis was significantly higher in the younger group than in the
older group (30 vs. 6%; P<0.01). In addition, the prevalence of
advanced-stage cancer according to the TNM classification staging
system was higher in the older group (P<0.01).
 | Table II.Tumor characteristics, operative
factors and complications according to age group. |
Table II.
Tumor characteristics, operative
factors and complications according to age group.
| Parameter | Patients aged
<80 years (n=351) | Patients aged ≥80
years (n=44) | P-value |
|---|
| Maximum tumor size
(cm) | 4.7±4.4 | 6.4±7.5 | 0.02 |
| Tumor number
(single/multiple) | 227/124 | 28/16 | 0.89 |
| Operative method
(anatomic/limited) | 160/191 | 19/25 | 0.76 |
| Operation time
(min) | 368±136 | 333±124 | 0.16 |
| Intraoperative
bleeding (ml) | 1,061±961 | 1,011±906 | 0.68 |
| Allogeneic
transfusion, n (%) | 78 (22) | 11 (25) | 0.67 |
| Differentiation
(poor), n (%) | 15 (4) | 2 (5) | 0.93 |
| Portal vein tumor
thrombosis, n (%) | 188 (54) | 30 (68) | 0.06 |
| Background liver
condition (cirrhosis), n (%) | 106 (30) | 3 (6) | <0.01 |
| Tumor stage (I,
II/III, IV) | 189/162 | 14/30 | <0.01 |
| PHLF, n (%) | 40 (11) | 5 (11) | 0.99 |
| Bile leakage, n
(%) | 10 (3) | 1 (2) | 0.82 |
| Complications,
other (≥Clavien II), n (%) | 75 (27) | 12 (27) | 0.37 |
| Mortality, n
(%) | 15 (4) | 1 (2) | 0.51 |
| Delirium, n
(%) | 51 (15) | 33 (75) | <0.01 |
The incidence of post-operative complications
without post-operative delirium was similar between the older and
younger groups, with PHLF occurring in 11%, bile leakage in 2 and
3%, and other complications occurring in 27% of each group.
Complications other than PHLF and bile leakage in the younger group
included refractory ascites in 31 patients (9%), surgical site
infection in 17 (5%), pneumonia in seven (2%), pleural effusion in
five (1%), methicillin-resistant Staphylococcus aureus
infection in four (1%), ileus in three (1%) and other complications
in eight patients (2%). By contrast, complications in the older
group included refractory ascites in six patients (14%), surgical
site infection in two patients (5%), pneumonia in two patients
(5%), pleural effusion in one patient (2%) and ileus in one patient
(1%). These complications were also similar between the two groups.
Furthermore, the post-operative delirium occurred at a rate of 75%
in the older group, and 15% in the younger group (P<0.01).
The mortality rate was 4% (15 patients) in the
younger group and 2% (1 patient) in the older group. This
difference was not statistically significant (P=0.51).
Outcome
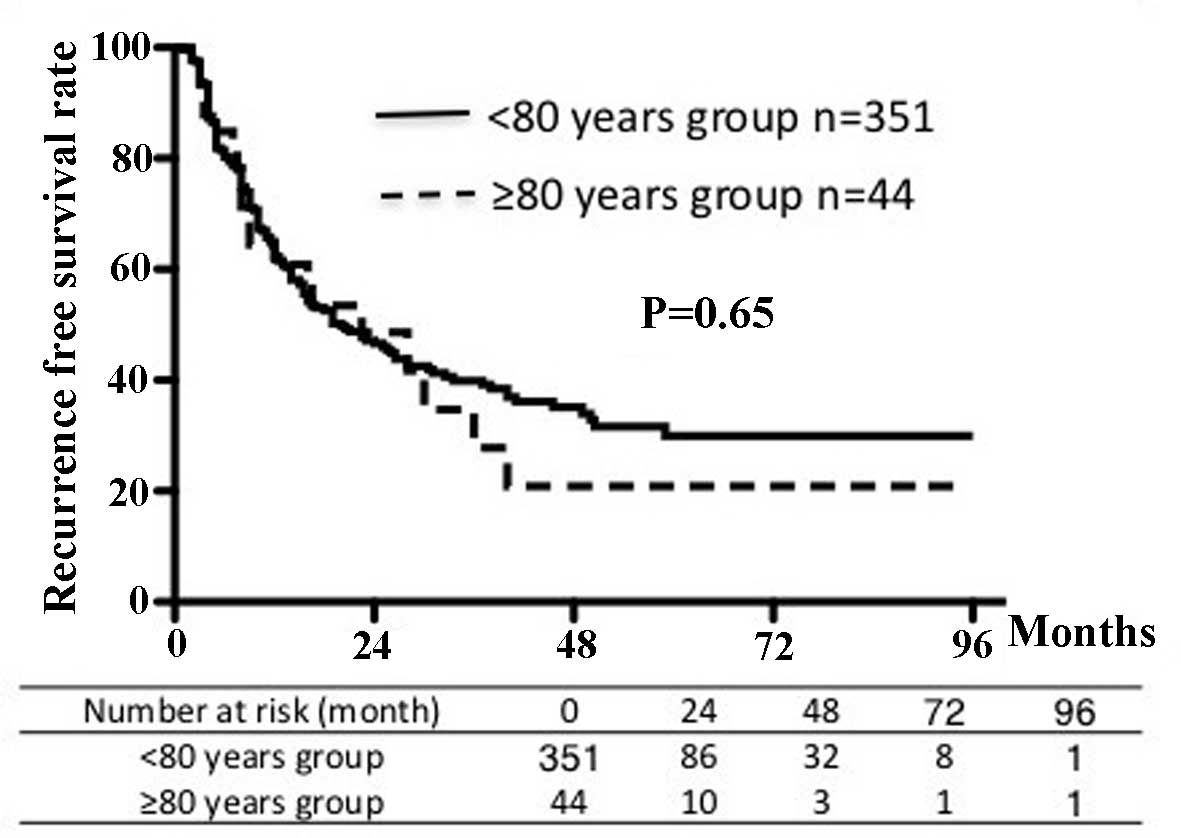
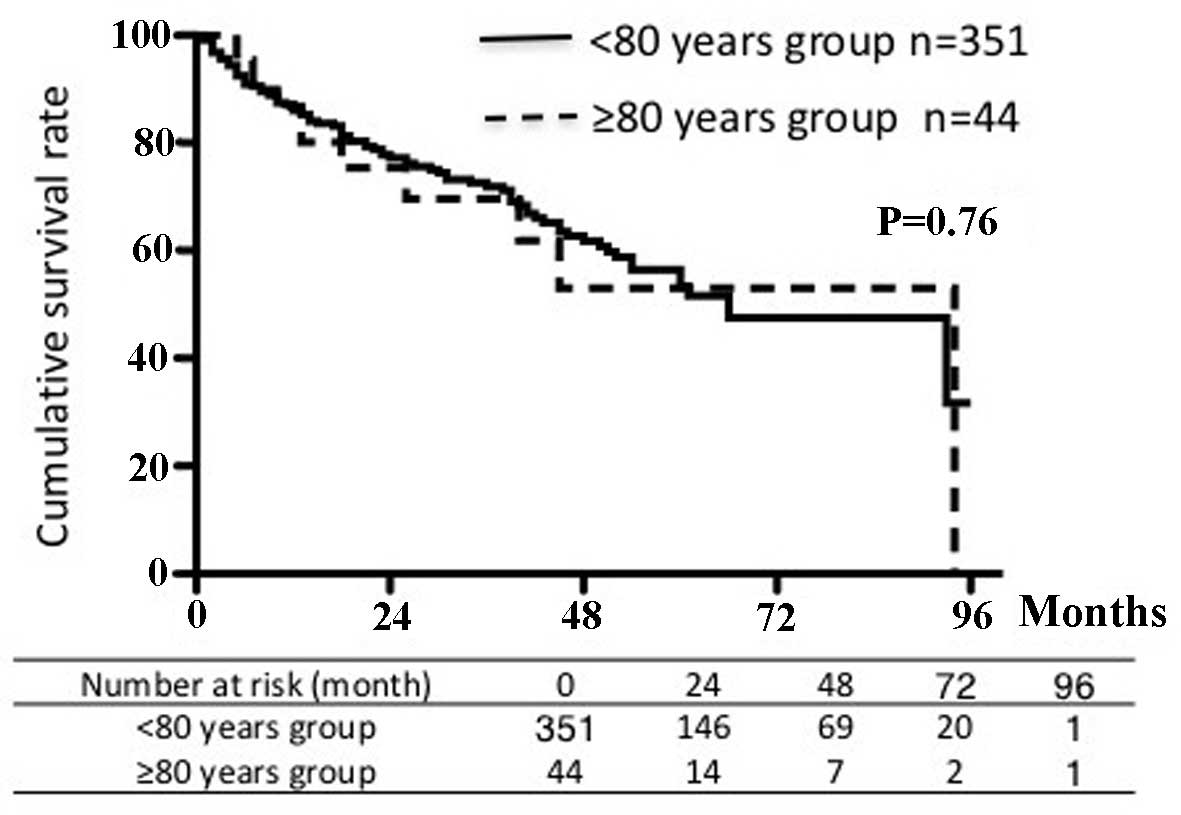
Figs. 1 and 2 show the recurrence-free survival and
cumulative survival rates for the two groups. The 5-year
recurrence-free survival rate was 29% in the younger group and 21%
in the older group. The 5-year cumulative survival rate was 53% in
each age group. There were no significant differences in survival
rates between the groups.
The independent risk factors for survival according
to age group are listed in Tables
III and IV. Among patients
<80 years of age, univariate analysis showed a significant
correlation between survival and prothrombin activity, total
bilirubin, albumin, AFP, DCP, ICGR-15, the number of tumors,
maximum tumor size, frequency of blood transfusion and
post-operative complications. According to multivariate analysis of
these factors, albumin levels, AFP and the number of tumors were
independent risk factors for survival in this age group. By
contrast, among patients ≥80 years of age, univariate analysis
revealed a significant association between survival and AFP, tumor
number and post-operative complications. The occurrence of
post-operative complications was the only independent risk factor
for survival in the older group according to multivariate analysis
(odds ratio, 4.30; 95% confidence interval, 1.49–13.25). By
contrast, the odds ratio in the younger group was 1.18.
 | Table III.Independent risk factors for
post-operative survival in patients aged <80 years. |
Table III.
Independent risk factors for
post-operative survival in patients aged <80 years.
|
| Univariate
analysis | Multivariate
analysis |
|---|
|
|
|
|
|---|
| Factor | P-value | Risk ratio | 95% CI | P-value |
|---|
| Age (years) | 0.13 |
|
|
|
|
≥67/<67 |
|
|
|
|
| Gender | 0.81 |
|
|
|
|
Male/female |
|
|
|
|
| Alcohol abuse | 0.46 |
|
|
|
|
Yes/no |
|
|
|
|
| Etiology | 0.99 |
|
|
|
|
NBNC/HCV and/or HBV |
|
|
|
|
| Platelet count
(104/µl) | 0.05 |
|
|
|
|
≥15/<15 |
|
|
|
|
| Prothrombin
activity (%) | 0.01 | 1.02 | 0.80–1.29 | 0.86 |
|
≥85/<85 |
|
|
|
|
| AST (IU/l) | 0.18 |
|
|
|
|
≥45/<45 |
|
|
|
|
| ALT (IU/l) | 0.50 |
|
|
|
|
≥45/<45 |
|
|
|
|
| Total bilirubin
(mg/dl) | <0.01 | 1.16 | 0.92–1.45 | 0.19 |
|
≥0.8/<0.8 |
|
|
|
|
| Albumin (g/dl) | <0.01 | 1.54 | 1.21–1.96 | <0.01 |
|
≥3.7/<3.7 |
|
|
|
|
| AFP (ng/ml) | <0.01 | 1.61 | 1.28–2.03 | <0.01 |
|
≥20/<20 |
|
|
|
|
| DCP (mAU/ml) | <0.01 | 1.24 | 0.96–1.59 | 0.08 |
|
≥100/<100 |
|
|
|
|
| ICGR-15 (%) | <0.01 | 1.15 | 0.89–1.50 | 0.26 |
|
≥17/<17 |
|
|
|
|
| Tumor number | <0.01 | 1.74 | 1.37–2.20 | <0.01 |
|
Single/multiple |
|
|
|
|
| Maximum tumor size
(cm) | <0.01 | 1.12 | 0.86–1.43 | 0.38 |
|
≥3/<3 |
|
|
|
|
| Blood
transfusion | <0.01 | 1.23 | 0.98–1.56 | 0.06 |
|
Yes/no |
|
|
|
|
| Post-operative
complications | <0.01 | 1.18 | 0.91–1.53 | 0.20 |
|
Yes/no |
|
|
|
|
 | Table IV.Independent risk factors for
post-operative survival in patients aged ≥80 years. |
Table IV.
Independent risk factors for
post-operative survival in patients aged ≥80 years.
|
| Univariate
analysis | Multivariate
analysis |
|---|
|
|
|
|
|---|
| Factor | P-value | Risk ratio | 95% CI | P-value |
|---|
| Age (years) | 0.72 |
|
≥83/<83 |
|
|
|
|
| Gender | 0.42 |
|
|
|
|
Male/female |
|
|
|
|
| Alcohol abuse | 0.07 |
|
|
|
|
Yes/no |
|
|
|
|
| Etiology | 0.93 |
|
|
|
|
NBNC/HCV and/or HBV |
|
|
|
|
| Platelet count
(104/µl) | 0.43 |
|
|
|
|
≥15/<15 |
|
|
|
|
| Prothrombin
activity (%) | 0.92 |
|
|
|
|
≥90/<90 |
|
|
|
|
| AST (IU/l) | 0.44 |
|
|
|
|
≥40/<40 |
|
|
|
|
| ALT (IU/l) | 0.20 |
|
|
|
|
≥40/<40 |
|
|
|
|
| Total bilirubin
(mg/dl) | 0.81 |
|
|
|
|
≥0.7/<0.7 |
|
|
|
|
| Albumin (g/dl) | 0.17 |
|
|
|
|
≥3.7/<3.7 |
|
|
|
|
| AFP (ng/ml) | 0.01 | 1.84 | 0.68–5.11 | 0.22 |
|
≥14/<14 |
|
|
|
|
| DCP (mAU/ml) | 0.59 |
|
|
|
|
≥200/<200 |
|
|
|
|
| ICGR15 (%) | 0.74 |
|
|
|
|
|
≥15/<15 |
|
|
|
|
| Tumor number | <0.01 | 2.17 | 0.74–5.98 | 0.14 |
|
Single/multiple |
|
|
|
|
| Maximum tumor size
(cm) | 0.27 |
|
|
|
|
≥4/<4 |
|
|
|
|
| Blood
transfusion | 0.85 |
|
|
|
|
Yes/no |
|
|
|
|
| Post-operative
complications | 0.02 | 4.30 | 1.49–13.25 | <0.01 |
|
Yes/no |
|
|
|
|
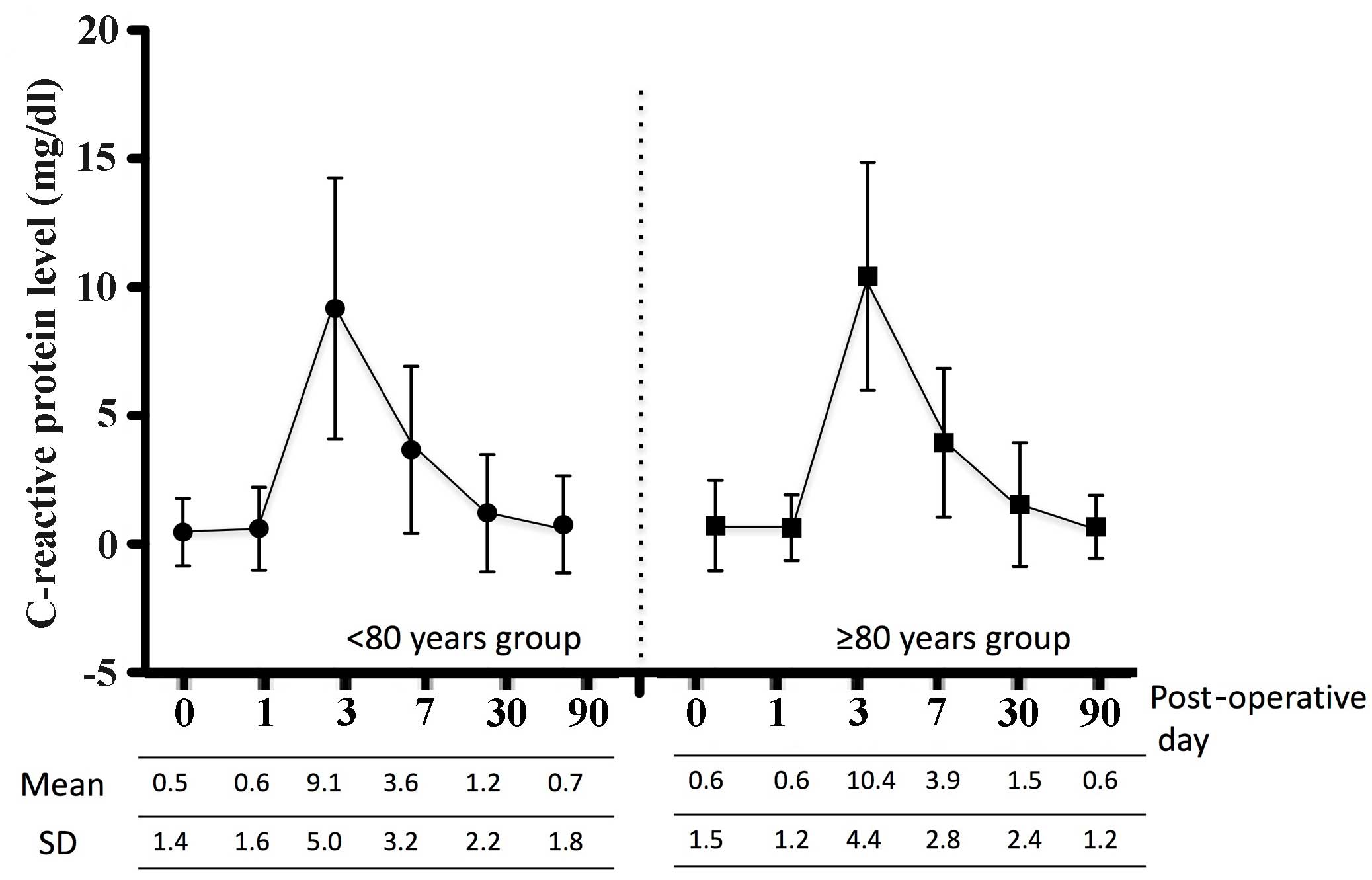
Nutrition and inflammation
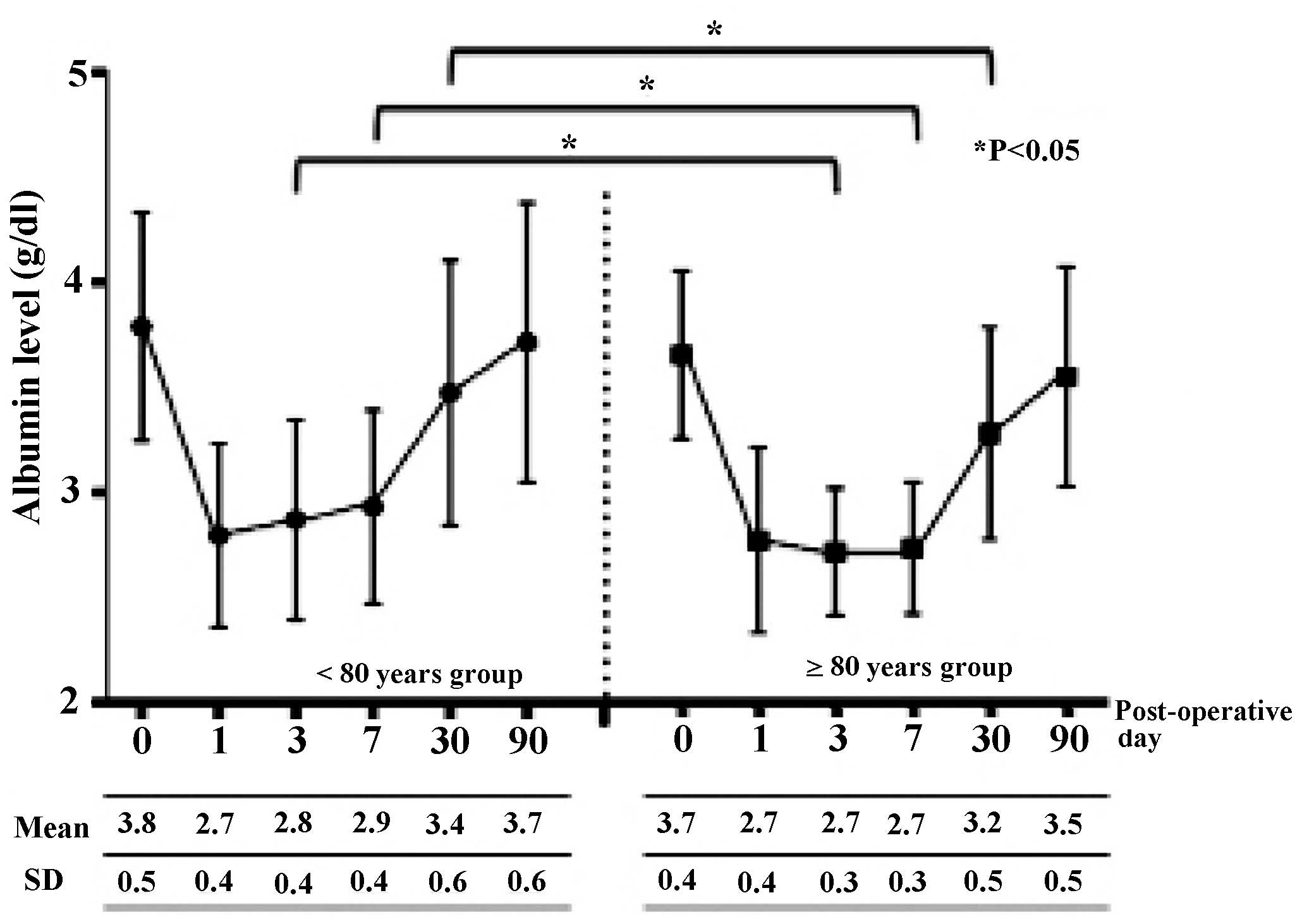
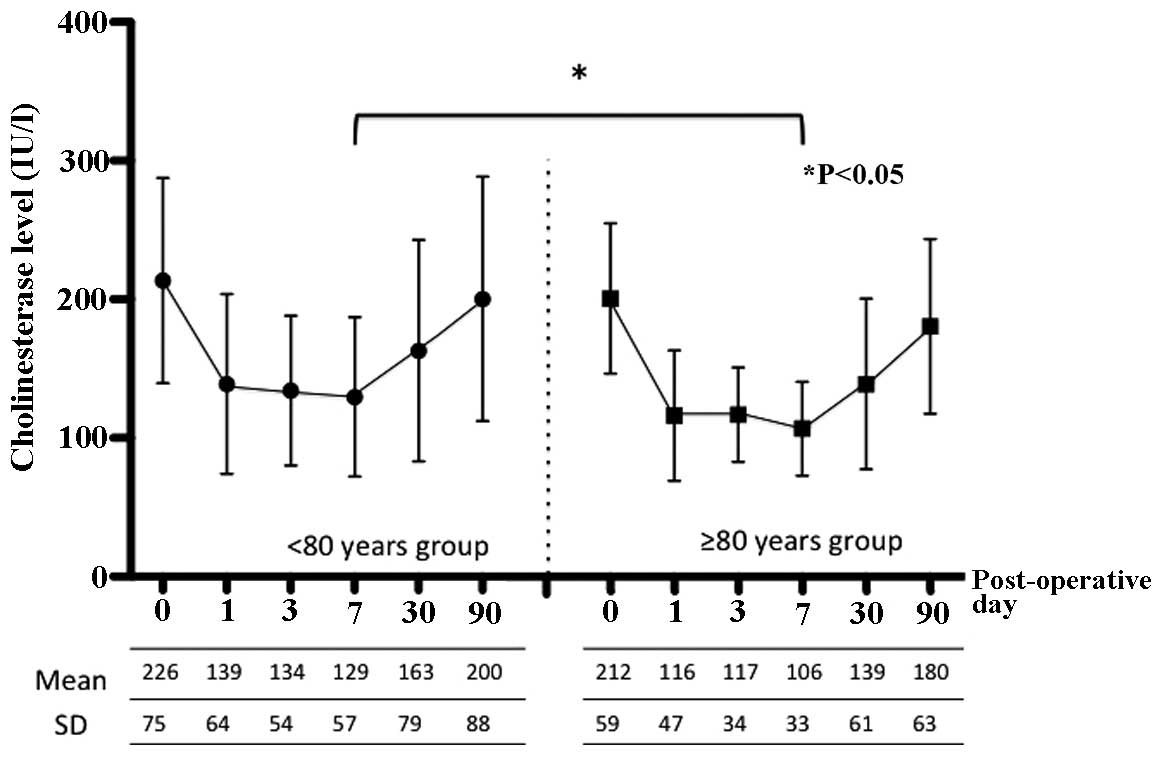
In addition, the present study assessed
peri-operative albumin, cholinesterase and CRP levels as indicators
of nutrition and inflammation. Figs.
3, 4 and 5 show the peri-operative changes in
albumin, cholinesterase and CRP levels, respectively. Albumin
levels prior to and at 1 day following surgery were similar between
the two groups. However, albumin levels were significantly lower in
the older group than in the younger group at 3, 7 and 30 days after
surgery. This finding indicated that improvement of albumin levels
was inferior in patients ≥80 years of age relative to those aged
<80 years. In addition, cholinesterase levels at 7 days after
surgery were significantly lower in the older group than in the
younger group. However, changes in CRP levels over time were
similar between the groups. These results indicated that, although
post-operative inflammation was similar between the two groups,
nutrition in patients aged ≥80 years improved more slowly compared
to younger patients.
Factors associated with post-operative
complications
Finally, the association of factors including
albumin levels with complications was assessed. Table V shows the association between
various parameters and the occurrence of post-operative
complications among patients ≥80 years of age. Patient background
characteristics, tumor characteristics and operative factors of
patients who experienced complications were compared with those of
patients without complications. Albumin levels were 3.5±0.4 g/dl in
the complications group vs. 3.8±0.4 g/dl in the group without
complications (P=0.02). In the complications group, ICGR-15 levels
(P=0.01), operation time (P=0.01) and the occurrence of
inter-operative bleeding (P<0.01) were significantly higher than
in the group without complications. In conclusion, low albumin
levels as well as increased ICGR-15 levels, operation time and
inter-operative bleeding were associated with post-operative
complications in patients aged ≥80 years. Moreover, an observation
of the present study was that the occurrence of post-operative
complications affected patient prognosis.
 | Table V.Univariate analysis of factors
according to the occurrence of complications in patients aged ≥80
years. |
Table V.
Univariate analysis of factors
according to the occurrence of complications in patients aged ≥80
years.
| Factor | Complication group
(≥80 years; n=12) | No complication
group (≥80 years; n=32) | P-value |
|---|
| Age (years) | 83.5±3.1 | 83.2±3.0 | 0.83 |
| Gender
(male/female) | 4/8 | 11/21 | 0.94 |
| Diabetes (n) | 3 (25%) | 6 (19%) | 0.64 |
| Hypertension
(n) | 5 (42%) | 15 (47%) | 0.16 |
| Alcohol abuse
(n) | 2 (17%) | 6 (19%) | 0.87 |
| Hepatitis C
(n) | 5 (42%) | 15 (47%) | 0.16 |
| NBNC (n) | 7 (58%) | 16 | 0.62 |
| Platelet count
(104/µl) | 17.5±5.2 | 19.3±9.0 | 0.74 |
| Prothrombin
activity (%) | 91.1±14.1 | 95.4±11.2 | 0.52 |
| AST (IU/l) | 42.9±21.5 | 45.1±24.1 | 0.92 |
| ALT (IU/l) | 31.8±20.9 | 34.4±27.4 | 0.92 |
| ALP (IU/l) | 437±248 | 36±212 | 0.47 |
| γ-GTP (IU/l) | 139±129 | 75±72 | 0.22 |
| Albumin (g/dl) | 3.5±0.4 | 3.8±0.4 | 0.02 |
| Total bilirubin
(mg/dl) | 0.7±0.2 | 0.6±0.2 | 0.48 |
| CRP (mg/dl) | 2.5±3.7 | 0.2±0.2 | 0.18 |
| Cholinesterase
(IU/l) | 208±60 | 217±70 | 0.91 |
| ICGR-15 (%) | 18.2±5.4 | 14.0±7.8 | 0.01 |
| AFP (ng/ml) | 3,235±5,999 | 296±1171 | 0.36 |
| DCP (mAU/ml) | 5,263±9,023 | 5,567±16,357 | 0.32 |
| Maximum tumor size
(cm) | 8.4±13.1 | 6.4±7.5 | 0.77 |
| Tumor number
(single/multiple) | 6/6 |
22/10 | 0.24 |
| Operative method
(anatomic/limited) | 4/8 | 15/17 | 0.41 |
| Operation time
(min) | 396±125 | 299±108 | 0.01 |
| Intraoperative
bleeding (ml) | 1,625±904 | 862±841 | <0.01 |
| Allogeneic
transfusion (n) | 5 (42%) | 6 (19%) | 0.10 |
Discussion
Population aging is one of the major problems
worldwide. According to the United Nations document, ‘World
Population Prospects, the 2012 Revision’, the proportion of people
aged >65 years in 2010 was 7.7%, and it is expected to increase
to 17.6% in 2060. It has been reported that elderly HCC patients
generally have good hepatic functional reserve and that treatment
methods involving ablation or transarterial embolization are
administered more frequently than hepatic resection in this age
group (9). In Japan, the mean age of
HCC patients has also increased over time (10,11), and
it has been reported that a considerable number of these patients
have cirrhosis and early-stage disease (12). The reported characteristics of
elderly HCC patients who undergo resection include a high
percentage of NBNC cases, lower albumin levels despite good hepatic
functional reserve, and a high prevalence of hypertension and
cardiovascular disease compared with younger patients (13,14).
The prevalence of cardiovascular disease was similar
between the groups of the present study. However, a significantly
greater percentage of patients in the older group had pulmonary
disease. Although the number of elderly people living independently
has increased, elderly people generally have more comorbid
disorders compared with younger people. However, the present study
found a similar prevalence of cardiovascular disease between the
groups. It is possible that for patients ≥80 years of age with
underlying cardiovascular diseases, other treatments, such as
radiofrequency ablation or transarterial embolization, were pursued
at a higher rate than for those <80 years of age. This
difference in treatment selection may also account for the similar
rates of post-operative complications between the groups of the
present study. However, a significantly higher percentage of
patients in the older group had post-operative delirium compared
with the younger group.
Major operations, such as those involving the
stomach, colon, rectum, pancreas and other organs, are generally
feasible in elderly patients (15).
Numerous studies have described the usefulness of hepatic resection
for elderly patients with HCC. Specifically, elderly and younger
patients were reported to have similar complication rates, duration
of hospitalization, prognoses and recurrence rates (16,17).
Surgery is reportedly safe even in cirrhosis patients (18), and the same post-operative management
approach can be used in elderly and younger patients (19). One reason for the safety of hepatic
resection is the use of improved surgical methods and drugs,
resulting in decreased post-operative mortality (20). However, elderly patients have a
higher pre-operative complication rate and are in a poorer overall
physical condition compared with younger patients, which should be
taken into account during peri-operative considerations, i.e., not
every peri-operative factor will be similar between younger and
elderly patients. For instance, a previous study reported more
post-operative complications in elderly patients vs. younger
patients undergoing gastrointestinal surgery (stomach, colon or
esophagus) (21). Particularly,
elderly patients with underlying cardiovascular conditions are
prone to be affected by a higher rate of complications (20).
The present study aimed to identify problems
associated with hepatic resection in elderly patients, differences
compared with younger patients and important points concerning
peri-operative management. It was revealed that post-operative
complications associated with blood loss, duration of surgery and
albumin levels affected the prognosis of elderly patients. Evidence
for a link between complications after hepatectomy and prognosis
for HCC patients has been provided (22). However, it remains to be fully
elucidated via which mechanisms post-operative morbidity influences
the long-term outcome of cancer patients. Major surgery causes a
systemic inflammatory response and immunosuppression (23), and post-operative morbidity may
exacerbate these conditions. It has been speculated the survival
and subsequent growth of tumor micrometastases is promoted by
prolonged systemic inflammation and immunosuppression associated
with post-operative morbidity. In the present study, blood loss,
the duration of surgery and albumin levels were associated with
post-operative complications, which in turn have been previously
reported to affect the prognosis (24,25).
Certain studies have concluded that liver resection
for HCC is feasible in patients >80 years of age, as their
short- and long-term outcome is similar to that of younger
patients. By contrast, other studies have reported problems among
older patients. One study reported that, although hepatic resection
is generally feasible in older patients, those with pre-operative
complications had more post-operative complications, particularly
patients >80 years of age (23).
Of note, one study found that the mortality rate among patients
>80 years of age was similar to that of younger patients, but
that patients >80 years of age had a lower incidence of liver-
and HCC-associated mortality, and a higher incidence of mortality
resulting from other causes (24).
The authors concluded that meticulous pre-operative assessment and
post-operative care are important in patients >80 years of
age.
The operation time, American Society of
Anesthesiologists (ASA) physical status classification, blood
transfusion and other factors have been reported to contribute to
post-operative morbidity (26,27). A
score based on age, presence of cardiovascular disease, pulmonary
disease and diabetes mellitus, as well as performance status and
the ASA score, can be used to predict post-operative morbidity
(28). In the present study, albumin
levels were a predictive factor for post-operative complications;
furthermore, post-operative improvement in the albumin levels among
elderly patients occurred more slowly compared with younger
patients. To the best of our knowledge, the present study was the
first to report the long-term changes in post-operative nutritional
status, including albumin levels, in younger vs. elderly patients.
One reason for the lower levels of improvement in the
post-hepatectomy albumin concentration in elderly patients may be
their decreased hepatic blood flow, as hepatic portal flow
decreases with age (29,30). Moreover, liver regeneration in
elderly patients is slower compared with that in younger patients
(31). Based on these findings,
operations should be performed carefully to avoid morbidity,
particularly in elderly patients. In addition, because low albumin
levels are associated with post-operative morbidity, peri-operative
nutritional care is important in elderly patients. The
branched-chain amino acid-to-tyrosine ratio, which is a marker of
nutritional status, is associated with post-operative complications
and administration of branched-chain amino acids reduces early HCC
recurrence (32,33). Therefore, it is important that
elderly patients are peri-operatively administered branched-chain
amino acids.
In conclusion, hepatic resection of HCC is feasible
in selected elderly patients without severe comorbidity. However,
the avoidance of post-operative complications is important, since
they adversely affect patient prognosis. As poor nutritional status
is one cause of post-operative complications, elderly patients
should receive appropriate peri-operative nutritional care. A
limitation of the present study was its single-center and
retrospective nature, and further research involving multi-center,
prospective studies is required.
Glossary
Abbreviations
Abbreviations:
|
HCC
|
hepatocellular carcinoma
|
|
HCV
|
hepatitis C virus
|
|
CRP
|
C-reactive protein
|
|
AFP
|
α-fetoprotein
|
|
DCP
|
des-gamma-carboxy prothrombin
|
|
ICGR-15
|
indocyanine green retention rate at 15
min
|
|
PHLF
|
post-hepatectomy liver failure
|
References
|
1
|
Suda T, Nagashima A, Takahashi S, Kanefuji
T, Kamimura K, Tamura Y, Takamura M, Igarashi M, Kawai H, Yamagiwa
S, et al: Active treatments are a rational approach for
hepatocellular carcinoma in elderly patients. World J
Gastroenterol. 19:3831–3840. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Fong Y, Brennan MF, Cohen AM, Heffernan N,
Freiman A and Blumgart LH: Liver resection in the elderly. Br J
Surg. 84:1386–1390. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Kaibori M, Matsui K, Ishizaki M, Saito T,
Kitade H, Matsui Y and Kwon AH: Hepatic resection for
hepatocellular carcinoma in the elderly. J Surg Oncol. 99:154–160.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Fortner JG and Lincer RM: Hepatic
resection in the elderly. Ann Surg. 211:141–145. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Mori S, Kita J, Shimizu T, Kato M, Shimoda
M and Kubota K: Outcome of hepatectomy for hepatocellular carcinoma
in elderly patients with portal hypertension. Int Surg. 99:153–160.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Intraobserver and interobserver variations
in liver biopsy interpretation in patients with chronic hepatitis
C. The French METAVIR Cooperative Study Group. Hepatology.
20:15–20. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Sobin LH and Fleming ID: TNM
Classification of Malignant Tumors, fifth edition (1997). Union
Internationale Contre le Cancer and the American Joint Committee on
Cancer. Cancer. 80:1803–1804. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Rahbari NN, Garden OJ, Padbury R,
Brooke-Smith M, Crawford M, Adam R, Koch M, Makuuchi M, Dematteo
RP, Christophi C, et al: Posthepatectomy liver failure: A
definition and grading by the International Study Group of Liver
Surgery (ISGLS). Surgery. 149:713–724. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Mirici-Cappa F, Gramenzi A, Santi V,
Zambruni A, Di Micoli A, Frigerio M, Maraldi F, Di Nolfo MA, Del
Poggio P, Benvegnù L, et al: Treatments for hepatocellular
carcinoma in elderly patients are as effective as in younger
patients: A 20-year multicentre experience. Gut. 59:387–396. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Ikai I, Itai Y, Okita K, Omata M, Kojiro
M, Kobayashi K, Nakanuma Y, Futagawa S, Makuuchi M and Yamaoka Y:
Report of the 15th follow-up survey of primary liver cancer.
Hepatol Res. 28:21–29. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Ikai I, Arii S, Okazaki M, Okita K, Omata
M, Kojiro M, Takayasu K, Nakanuma Y, Makuuchi M, Matsuyama Y, et
al: Report of the 17th Nationwide Follow-up Survey of Primary Liver
Cancer in Japan. Hepatol Res. 37:676–691. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Namieno T, Kawata A, Sato N, Kondo Y and
Uchino J: Age-related, different clinicopathologic features of
hepatocellular carcinoma patients. Ann Surg. 221:308–314. 1995.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Yamada S, Shimada M, Miyake H, Utsunomiya
T, Morine Y, Imura S, Ikemoto T, Mori H, Hanaoka J, Iwahashi S and
Saito Y: Outcome of hepatectomy in super-elderly patients with
hepatocellular carcinoma. Hepatol Res. 42:454–458. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Tsujita E, Utsunomiya T, Ohta M, Tagawa T,
Matsuyama A, Okazaki J, Yamamoto M, Tsutsui S and Ishida T: Outcome
of repeat hepatectomy in patients with hepatocellular carcinoma
aged 75 years and older. Surgery. 147:696–703. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Colapinto ND: Is age alone a
contraindication to major cancer surgery? Can J Surg. 28:323–326.
1985.PubMed/NCBI
|
|
16
|
Tsujita E, Utsunomiya T, Yamashita Y, Ohta
M, Tagawa T, Matsuyama A, Okazaki J, Yamamoto M, Tsutsui S and
Ishida T: Outcome of hepatectomy in hepatocellular carcinoma
patients aged 80 years and older. Hepatogastroenterology.
59:1553–1555. 2012.PubMed/NCBI
|
|
17
|
Nomura F, Ohnishi K, Honda M, Satomura Y,
Nakai T and Okuda K: Clinical features of hepatocellular carcinoma
in the elderly: a study of 91 patients older than 70 years. Br J
Cancer. 70:690–693. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Faber W, Stockmann M, Schirmer C,
Möllerarnd A, Denecke T, Bahra M, Klein F, Schott E, Neuhaus P and
Seehofer D: Significant impact of patient age on outcome after
liver resection for HCC in cirrhosis. Eur J Surg Oncol. 40:208–213.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Nagasue N, Chang YC, Takemoto Y, Taniura
H, Kohno H and Nakamura T: Liver resection in the aged (seventy
years or older) with hepatocellular carcinoma. Surgery.
113:148–154. 1993.PubMed/NCBI
|
|
20
|
Poon RT, Fan ST, Lo CM, Liu CL, Ngan H, Ng
IO and Wong J: Hepatocellular carcinoma in the elderly: results of
surgical and nonsurgical management. Am J Gastroenterol.
94:2460–2466. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Yanaga K, Kanematsu T, Takenaka K,
Matsumata T, Yoshida Y and Sugimachi K: Hepatic resection for
hepatocellular carcinoma in elderly patients. Am J Surg.
155:238–241. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Okamura Y, Takeda S, Fujii T, Sugimoto H,
Nomoto S and Nakao A: Prognostic significance of postoperative
complications after hepatectomy for hepatocellular carcinoma. J
Surg Oncol. 104:814–821. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Khuri SF, Henderson WG, DePalma RG, Mosca
C, Healey NA and Kumbhani DJ: Participants in the VA National
Surgical Quality Improvement Program. Determinants of long-term
survival after major surgery and the adverse effect of
postoperative complications. Ann Surg. 242:326–341; discussion
341–323. 2005.
|
|
24
|
Hirai T, Yamashita Y, Mukaida H, Kuwahara
M, Inoue H and Toge T: Poor prognosis in esophageal cancer patients
with postoperative complications. Surg Today. 28:576–579. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Mynster T, Christensen IJ, Moesgaard F and
Nielsen HJ: Effects of the combination of blood transfusion and
postoperative infectious complications on prognosis after surgery
for colorectal cancer. Danish RANX05 Colorectal Cancer Study Group.
Br J Surg. 87:1553–1562. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Ueno M, Hayami S, Tani M, Kawai M, Hirono
S and Yamaue H: Recent trends in hepatectomy for elderly patients
with hepatocellular carcinoma. Surg Today. 44:1651–1659. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Wang WL, Zhu Y, Cheng JW, Li MX, Xia JM,
Hao J, Yu L, Lv Y, Wu Z and Wang B: Major hepatectomy is safe for
hepatocellular carcinoma in elderly patients with cirrhosis. Eur J
Gastroenterol Hepatol. 26:444–451. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Ide T, Miyoshi A, Kitahara K and Noshiro
H: Prediction of postoperative complications in elderly patients
with hepatocellular carcinoma. J Surg Res. 185:614–619. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Zoli M, Iervese T, Abbati S, Bianchi GP,
Marchesini G and Pisi E: Portal blood velocity and flow in aging
man. Gerontology. 35:61–65. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Zoli M, Magalotti D, Bianchi G, Gueli C,
Orlandini C, Grimaldi M and Marchesini G: Total and functional
hepatic blood flow decrease in parallel with ageing. Age Ageing.
28:29–33. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Yamamoto K, Takenaka K, Matsumata T,
Shimada M, Itasaka H, Shirabe K and Sugimachi K: Right hepatic
lobectomy in elderly patients with hepatocellular carcinoma.
Hepatogastroenterology. 44:514–518. 1997.PubMed/NCBI
|
|
32
|
Mizuguchi T, Kawamoto M, Meguro M,
Nakamura Y, Harada K, Kukita K and Hirata K: Prognostic impact of
preoperative the branched-chain amino acid to the tyrosine ratio in
hepatocellular carcinoma patients after initial hepatectomy. J
Gastrointest Surg. 15:1433–1439. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Ichikawa K, Okabayashi T, Maeda H,
Namikawa T, Iiyama T, Sugimoto T, Kobayashi M, Mimura T and
Hanazaki K: Oral supplementation of branched-chain amino acids
reduces early recurrence after hepatic resection in patients with
hepatocellular carcinoma: a prospective study. Surg Today.
43:720–726. 2013. View Article : Google Scholar : PubMed/NCBI
|