Introduction
Benign tumors of the esophagus are rare, accounting
for <1% of all esophageal neoplasms. Leiomyomas are the most
common benign esophageal tumors, whereas hamartomas are the rarest
benign tumors (1). To the best of
our knowledge, there are only 12 cases of esophageal hamartoma
reported in the English literature to date, of which 8 were located
in the upper third and only 2 were in the lower third of the
esophagus no information regarding location was available for the
remaining 2 cases. One of the tumors was intramural, whereas in all
the remaining cases the tumors protruded into the lumen (2). However, esophageal chondroid hamartoma
has never been reported. We herein present an extremely rare case
of an adult patient presenting with an intramural chondroid
hamartoma located in the lower third of the esophagus and describe
the diagnosis and management of isolated esophageal chondroid
hamartomas.
Case report
A 33-year-old male patient was admitted to the
Department of Thoracic Surgery of the Harrison International Peace
Hospital (Hengshui, China) in August, 2013, with epigastric pain,
difficulty in swallowing and occasional vomiting after eating. The
symptoms were aggravated and the patient developed dysphagia,
occasionally experiencing acid reflux and heartburn within the last
2 months. Barium swallow examination revealed narrowing of the
lumen of the distal esophagus. Upper endoscopy revealed two
diverticulum-like lesions, measuring 0.3×0.3×0.3 and 0.3×0.3×0.3
cm, located on the right anterior wall of the esophagus at a
distance of ~38 cm from the incisors, and one diverticulum-like
lesion measuring 1.0×1.0×0.8 cm, located at 39–40 cm from the
incisors. A biopsy from the latter lesion revealed that the tissue
was lined by stratified squamous epithelium and the stroma was
infiltrated by chronic and acute inflammatory cells.
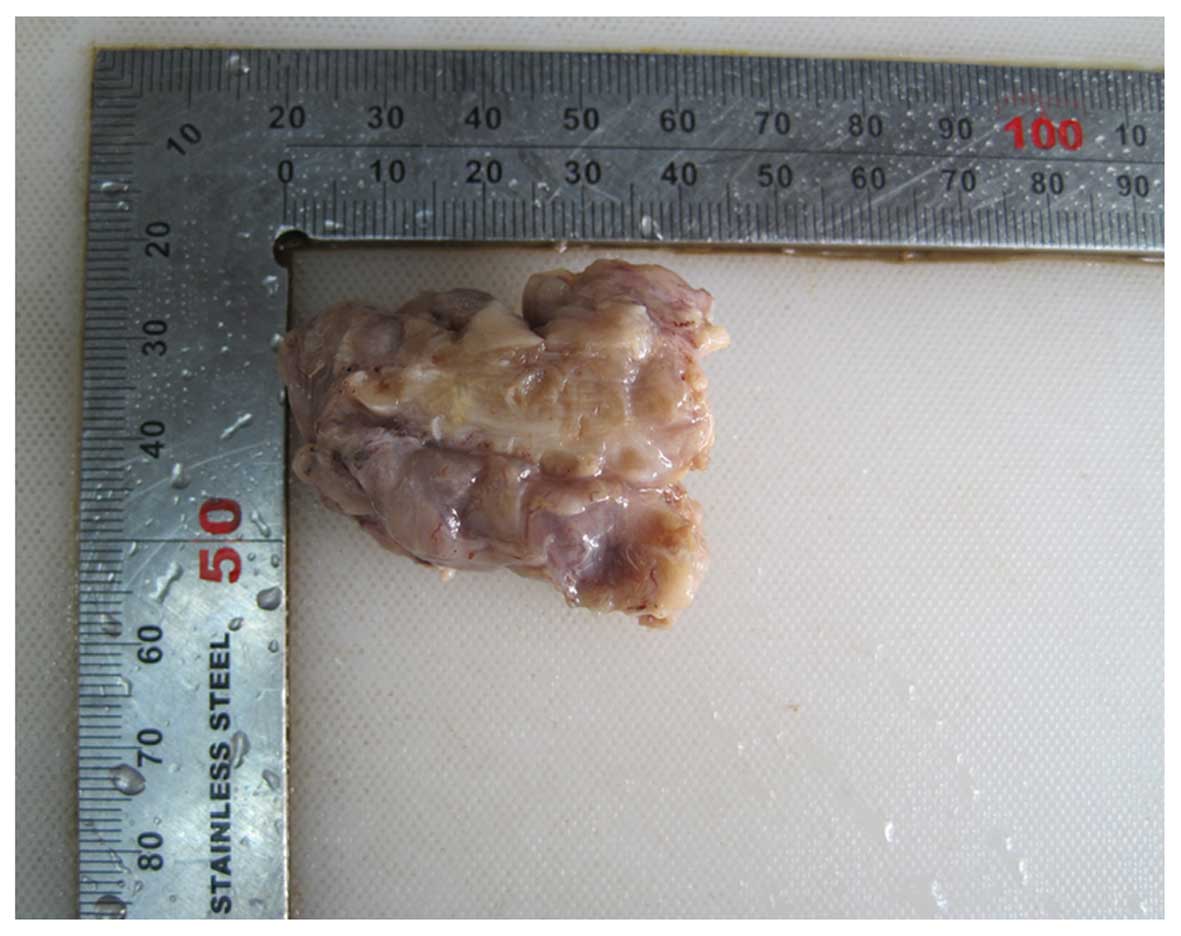
Intraoperatively, the affected segment of the distal
esophagus contained a mass measuring 2.0×2.0×2.0 cm located at 2.0
cm from the cardia. The mass tightly adhered to the esophageal
mucosa. On gross examination, the excised esophageal specimen
measured 3.5×3.0×1.5 cm and included a mass measuring 2.0×1.5×1.5
cm lying directly underneath the mucosa. On cross-section, the mass
was grayish-white and had a hard consistency (Fig. 1).
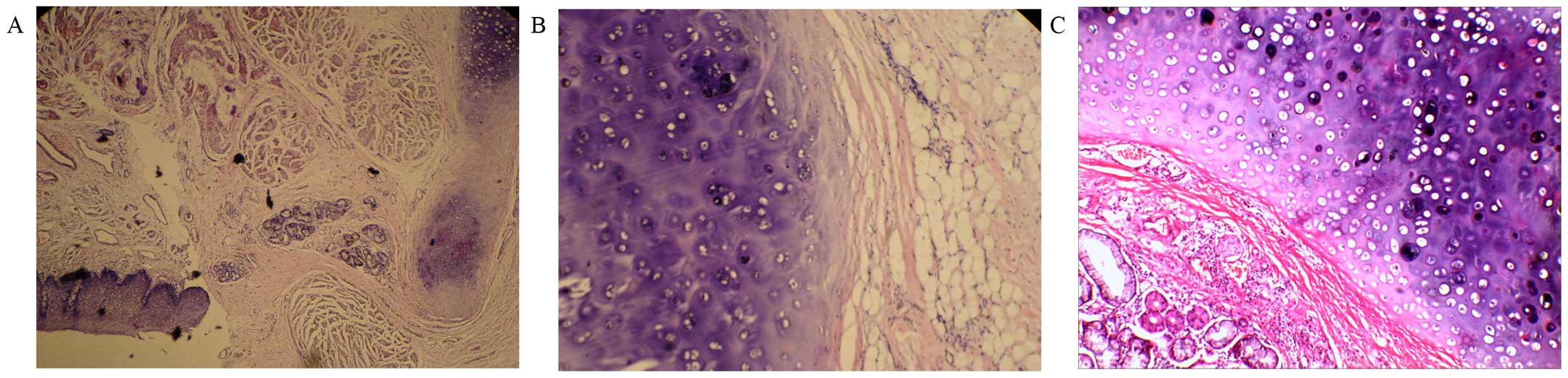
On microcopic examination, the mass was lined by
squamous epithelium and the stroma was mainly composed of chondroid
tissue (60%) admixed with adipose tissue (25%) and fibrous
connective tissue (15%) (Fig. 2).
The final histopathological diagnosis was lower esophageal
chondroid hamartoma. There was no recurrence of the tumor during 2
years of postoperative follow-up (last follow-up was in September,
2015).
Informed consent was obtained from the patient
regarding the publication of the case details and associated
images.
Discussion
Hamartoma is defined as a non-neoplastic, uni- or
multifocal developmental malformation, comprising a mixture of
cytologically normal mature cells and tissues which are indigenous
to the anatomic location, exhibiting a disorganized architectural
pattern with predominance of one of its components (3–6).
Hamartomas may occur in any organ, but are most commonly located in
the lungs (7), liver (8), pancreas (9) and spleen (10); however, they are rare in the
esophagus. The majority of the esophageal hamartomatous lesions
have been reported in pediatric patients (2), with a few cases reported in the adult
population, mostly among men.
Esophageal hamartomas are classified based on their
location in relation to the esophageal wall as intramural,
extramural or intraluminal (1). In
previously reported cases, the hamartoma was most commonly found in
the upper third of the esophagus and belonged to the category of
intraluminal lesions. In the present case, the tumor was located in
the lower third of the esophagus and was intramural. Smith et
al (11) reported a case in
which the tumor arose in the lower third of the esophagus and was
intramurally located; the patient was a 3.5-year-old female and the
tumor consisted of small mature lymphocytes, acidophilic
histiocytes, cartilage and bronchial-like mucous glands. In the
present case, however, the patient was a 33-year-old man and the
tumor mainly consisted of chondroid tissue admixed with adipose and
fibrous connective tissue. Following a review of the literature
(Table I), it is noteworthy that the
tumors arising in the upper third of the esophagus were all
intraluminal, whereas those in the lower third of the esophagus
were mostly intramural. Due to its rarity, there are no
epidemiological data regarding the occurrence of this type of tumor
in the esophagus.
 | Table I.Characteristics of cases with
esophageal hamartoma previously reported in the literature. |
Table I.
Characteristics of cases with
esophageal hamartoma previously reported in the literature.
| Study, year | Age
(years)/gender | Location | Microscopic
appearance | Refs. |
|---|
| Fuller, 1963 | 61/male | Upper
esophagus/intraluminal | Fibro-adipose
connective tissue admixed with mucous glands | (16) |
| Shah et al,
1975 | 60/male | Upper
esophagus/intraluminal | Adipose tissue,
glandular structures and cartilaginous tissue | (17) |
| Smith et al,
1976 | 3.5/female | Distal one third of
esophagus/intramural | Small mature
lymphocytes, acidophilic histiocytes, cartilage, bronchial-like
mucous glands | (11) |
| Kafai and Mirbod,
1977 | Child/male | NA | NA | (24) |
| Beckerman et
al, 1980 | Infant/male | Upper
esophagus/intraluminal | Skeletal muscle
fibres, fibrous connective tissue and hyaline cartilage | (18) |
| Venn et al,
1985 | 52/male | Upper
esophagus/intraluminal | Polypoid esophageal
hamartoma | (19) |
| Gupta et al,
1987 | 10/male | Upper end of
esophagus/intraluminal | Adipose tissue,
fibres of skeletal tissue, collagen tissue and moderate
vascularity | (20) |
| Saitoh et al,
1990 | 40/female | Upper
esophagus/intraluminal | Osseous,
cartilaginous, fibrous and adipose tissue and glandular
structures | (21) |
| Lakhkar et al,
1991 | 30/female | Upper
esophagus/intraluminal | Squamous epithelium,
hyperplastic and cystic glands with abundant well vascularized
stroma | (22) |
| Bernat et al,
1993 | NA | NA | NA | (25) |
| Halfhide et
al, 1995 | 41/male | Upper
esophagus/intraluminal | Fat cells, fibrous
tissue, atypical blood vessels and a large solitary island of bone
enclosed by periosteum | (23) |
| Wu et al,
2014 | 40/male | Distal one-third of
esophagus/intraluminal | NA | (2) |
| Present case | 33/male | Distal one-third of
esophagus/intramural | Cartilaginous tissue,
adipose tissue and fibrous connective tissue |
|
Hamartomas are pathologically subclassified
according to the relative abundance of a particular endogenous
tissue component, and the variants described include chondroid,
chondromesenchymal, angiomatous, lipomatous and leiomyomatous
hamartomas (12). A review of the
previously reported cases (Table I)
shows that the majority of the tumors comprise a mixture of adipose
tissue, skeletal muscle tissue and vascular components embedded in
connective tissue. However, the tumor in this case was mainly
composed of chondroid tissue admixed with adipose and fibrous
connective tissue. As the mesenchymal component in this lesion was
represented by chondroid cells, we recommend the term ‘chondroid
hamartoma’ to denote this unique characteristic of the tumor.
Although several chondroid hamartomas have been reported in the
lung and liver (13,14), to the best of our knowledge none have
been reported in the esophagus to date. Our findings add another
variant to the versatile phenotype of esophageal hamartoma.
There are no tumor markers or imaging
characteristics that allow a definitive preoperative diagnosis of
esophageal hamartoma, and the majority of the cases are diagnosed
following surgical resection or at autopsy. The diagnosis is based
entirely on histopathological evaluation. The differential
diagnosis includes choristoma and teratoma. Hamartoma is an
overgrowth of mature tissues that normally occur in an expected
area or organ, but with disorganization and often with one element
predominating (15). Choristoma is a
mass consisting of tissue that is histologically normal for an
organ or part of the body other than the one in which it is located
(15). Choristoma is considered to
consist of mass-forming, irregular and heterotopic tissue (15). Mature teratomas may have no mitoses
or a low mitotic index, they are mass-forming lesions and may
comprise heterologous elements, such as skeletal muscle, cartilage
or adipose tissu; however, teratomas are predominantly composed of
epidermal, dermal and adnexal structures along with keratin, rather
than cartilaginous elements. Thus, our case was ultimately
diagnosed as chondroid hamartoma.
Esophageal intramural hamartomas are associated with
non-specific, vague symptoms or are asymptomatic, presenting in
late childhood or adulthood. We hypothesize that the lack of
symptoms is the result of the significant compliance of the
esophagus. Symptoms may occur late during the course of the disease
as the result of the slow, gradual growth of these tumors, combined
with the indolent nature of these lesions, which is also common
among other benign tumors and may remain undetected for years
(1). The clinical and pathological
characteristics of 13 cases of esophageal hamartomas, including the
present case, are summarized in Table
I (additional full text for 2 cases was not available). The
median age of the patients was 31.3 years (range, infancy-61 years)
and the male:female ratio was 3:1. The clinical manifestations of
the esophageal hamartoma include dysphagia, mid chest/epigastric
pain, vomiting and weight loss. Our patient was admitted due to
epigastric pain, difficulty in swallowing and occasional vomiting
after eating. Upper endoscopy revealed three diverticulum-like
lesions and the patient underwent esophagotomy. Surgical resection
is the standard treatment for hamartomas, without reported
recurrences, and with a good prognosis. The procedure is usually
performed via esophagotomy or thoracotomy, whereas for some tumors
with thin pedicles, endoscopic excision may be the preferable
approach. In the previously reported cases, 9 of the patients
underwent esophagotomy (2,11,16–22) and
1 patient underwent snare coagulation (23). In the present case, we were able to
follow up the patient for 2 years, during which time there was no
evidence of tumor recurrence.
In conclusion, the esophageal tumor in the present
case was mainly composed of chondroid tissue and, in such cases,
chondroid hamartoma of the esophagus should be considered in the
differential diagnosis.
References
|
1
|
Choong CK and Meyers BF: Benign esophageal
tumors: Introduction, incidence, classification and clinical
features. Semin Thorac Cardiovasc Surg. 15:3–8. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Wu WM, Wang XD, Sun G, Qiang LH and Yang
YS: Adult asymptomatic hamartoma in the distal esophagus: A rare
case. Intern Med. 53:1945–1948. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Pilch BZ: Larynx and hypopharynxHead and
Neck Surgical Pathology. Lippincott Williams and Wilkins;
Philadelphia, PA: pp. 230–83. 2001
|
|
4
|
Barnes L: Surgical Pathology of the Head
and Neck. 2. 2nd. Marcel Dekker; New York, NY: pp. 1649–1672.
2001
|
|
5
|
Kumar V, Abbas AK and Aster JC: Robbins
Basic Pathology. 9th. Philadelphia, USA, Saunders: Elsevier; pp.
2572013
|
|
6
|
Allon I, Allon DM, Hirshberg A, Shlomi B,
Lifschitz-Mercer B and Kaplan I: Oral neurovascularhamartoma: A
lesion searching for a name. J Oral Pathol Med. 41:348–353. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Umashankar T, Devadas AK, Ravichandra G
and Yaranal PJ: Pulmonary hamartoma: Cytologicalstudy of a case and
literature review. J Cytol. 29:261–263. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Rosado E, Cabral P, Campo M and Tavares A:
Mesenchymal hamartoma of the liver-a case report and literature
review. J Radiol Case Rep. 7:35–43. 2013.PubMed/NCBI
|
|
9
|
Kawakami F, Shimizu M, Yamaguchi H, Hara
S, Matsumoto I, Ku Y and Itoh T: Multiple solid pancreatic
hamartomas: A case report and review of the literature. World J
Gastrointest Oncol. 4:202–206. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Basso SM, Sulfaro S, Marzano B, Fanti G,
Chiara GB and Lumachi F: Incidentally discovered asymptomatic
splenic hamartoma with rapidly expansive growth: A case report. In
Vivo. 26:1049–1052. 2012.PubMed/NCBI
|
|
11
|
Smith CW, Murray GF and Wilcox BR:
Intramural esophageal hamartoma. An unusual cause of progressive
stricture in a child. J Thorac Cardiovasc Surg. 72:315–318.
1976.PubMed/NCBI
|
|
12
|
Park SK, Jung H and Yang YI: Mesenchymal
hamartoma in nasopharynx: A case report. Auris Nasus Larynx.
35:437–439. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Fan M, Lin Y and Liu L: Multiple pulmonary
chondroid hamartoma. J Thorac Oncol. 9:11053–11054. 2014.
View Article : Google Scholar
|
|
14
|
Scheele J, Lemke J, Barth TF, Juchems M,
Wittau M, Kornmann M and Henne-Bruns D: Chondroid hamartoma of the
liver. GMS Interdiscip Plast Reconstr Surg DGPW. 17:Doc162014.
|
|
15
|
Dorland and Newman WA: Dorland's
illustrated medical dictionary. 32nd. Elsevier/Saunders;
Philadelphia: 2012
|
|
16
|
Fuller AP: Pedunculated hamartoma of the
oesophagus. J Laryngol Otol. 77:706–713. 1963. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Shah B, Unger L and Heimlich HJ:
Hamartomatous polyp of the esophagus. Arch Surg. 110:326–328. 1975.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Beckerman RC, Taussig LM, Froede RC,
Coulthard SW, Firor H and Tonkin I: Fibromuscular hamartoma of the
esophagus in an infant. Am J Dis Child. 134:153–155.
1980.PubMed/NCBI
|
|
19
|
Venn GE, DaCosta P and Goldstraw P: Giant
oesophageal hamartoma. Thorax. 40:684–685. 1985. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Gupta AK, Goyal VP, Hemani DD, Maheshwari
SK and Dubey MK: Pedunculated intraluminal oesophageal hamartoma. J
Laryngol Otol. 101:851–854. 1987. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Saitoh Y, Inomata Y, Tadaki N and Mimaki
S: Pedunculated intraluminal osteochrondromatous hamartoma of the
esophagus. J Otolaryngol. 19:339–342. 1990.PubMed/NCBI
|
|
22
|
Lakhkar BN, Ghosh MK, Shenoy PD and Patil
UD: Hamartoma-a benign intraluminal tumor of the oesophagus (a case
report). J Postgrad Med. 37:235–237, 236A-236B. 1991.PubMed/NCBI
|
|
23
|
Halfhide BC, Ginai AZ, Spoelstra HA, Dees
J and Vuzevski VD: Case report: A hamartoma presenting as a giant
oesophageal polyp. Br J Radiol. 68:85–88. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Kafai F and Mirbod P: Hamartoma of the
oesophagus. Br J Clin Pract. 31:154–156. 1977.PubMed/NCBI
|
|
25
|
Bernat M, Strutyńska-Karpinska M,
Lewandowski A, Blaszczuk J, Grabowski K and Czapla L: Benign
esophageal tumors. Wiad Lek. 46:24–27. 1993.(In Polish). PubMed/NCBI
|