Introduction
Progress in laparoscopic techniques and expertise,
in combination with technological advances, have led to a more
widespread performance of laparoscopic hepatic resections for
hepatocellular carcinoma (HCC) over the last 15 years. It is
accepted that laparoscopic liver resection (LLRs) is a safe
procedure, with acceptable morbidity and mortality for both minor
and major liver resections (LRs) (1). Cirrhotic patients constitute a
high-risk population, and present a major challenge for the
performance of minimally invasive LR due to difficulties in
parenchymal transection. Several studies have reported successful
application of laparoscopic hepatic resections in selected
cirrhotic patients, despite the presence of greater preoperative
comorbidities (2,3). In the present study, the case of a
morbidly obese, cirrhotic patient who was admitted to the General
Hospital Laiko for an HCC, and who successfully underwent a
laparoscopic segmental hepatic resection, is reported.
Case report
A 71 year-old morbidly obese male patient with
cirrhosis due to hepatitis B virus (HBV) infection and alcoholic
hepatitis was referred to our department at the General Hospital
Laiko with a hepatic mass identified on performing abdominal
ultrasound. The patient, who was routinely evaluated for chronic
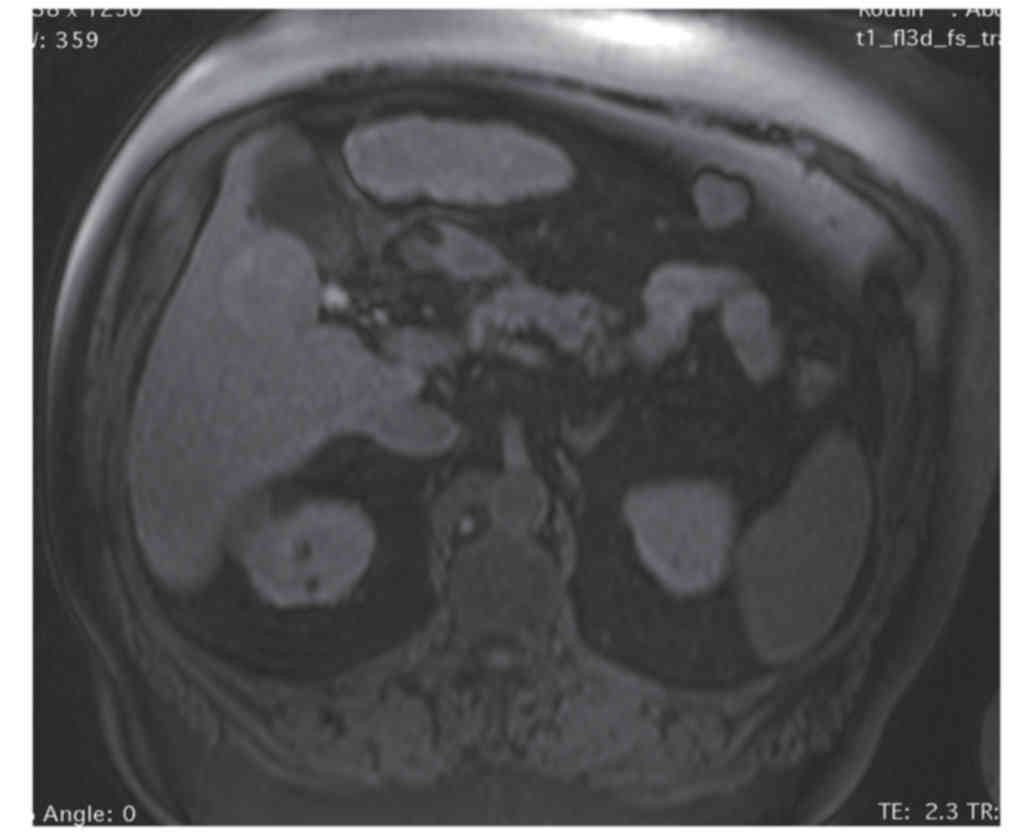
HBV infection, was asymptomatic. Abdominal computer tomography and
magnetic resonance imaging confirmed a mass in segments V–VI of the
liver (4.7×4.5×4.3 cm), highly suspicious for HCC (Fig. 1). The patient's past medical history
additionally included non-alcoholic steatohepatitis (NASH),
diabetes mellitus, arterial hypertension and myocardial infarction.
The patient's body mass index (BMI) was 45 kg/m2, the
American Society of Anesthesiologists' classification of
preoperative risk was 3, and the liver function was classified as
Child-Pugh class A (4,5). The patient's α-fetoprotein level was
5.5 ng/ml. He underwent laparoscopic resection of segments V–VI and
cholecystectomy. The operative time was 105 min. During the early
postoperative period, the patient developed a moderate renal and
hepatic failure that regressed gradually over the course of the
following next days, not necessitating any intervention, and was
classified as grade II according to the Dindo-Clavien
classification (6). The patient was
discharged on the eighth postoperative day. Histology and
immunohistochemistry [cytokeratin (CK) 7, CK19, epithelial membrane
antigen (EMA), α-fetoprotein (AFP), CEApol, glypican-3, CD10]
revealed a moderately differentiated HCC, with negative resection
margins (R0 resection), without vascular or lymphatic invasion
[stage pT1, according to the tumor-lymph nodes-metastasis (TNM)
staging system]. Two years postoperatively, the patient remains
disease-free and in excellent condition.
Discussion
Morbid obesity has a continually increasing
prevalence worldwide, and has been associated with worse
postoperative outcomes due to correlated co-morbidities, as well as
technical intraoperative difficulties. In the context of liver
disease, obesity is associated with various liver diseases,
including fatty liver disease and NASH. From the limited data
available, recent studies have shown that hepatic resections in
obese patients may be safely performed with no additional risk
compared with non-obese patients (7). Laparoscopic liver surgery in this
population presents a surgical challenge, and yet, since the BMI
has not been reported to negatively affect the postoperative
short-term outcomes in patients undergoing LLR, the laparoscopic
approach is not considered to be a contraindication for obese
patients (BMI, 32±2.0%) (8). A study
by Toriguchi et al (9)
underlined the benefits of LLR in obese patients, with a median BMI
of 26.8% (range 25–38.2%), reporting significantly lower
intraoperative blood loss and hospital stays compared with obese
patients operated on with open liver resection (9). A more recent study exploring the impact
of BMI on surgical outcomes in patients undergoing LLR (median BMI,
24.1±4.1%) compared with open LR (median BMI=23.1±3.9%)
demonstrates that LLR in obese patients may be performed as safely
as in non-obese patients, with the same risk of postoperative
complications and with, additionally, lower operation times and
levels of blood loss compared with non-obese patients (10). Furthermore, the study by Uchida et
al (10) also reported a marked
correlation of the BMI with operation time and blood loss in open
LR; however, no such correlation is demonstrated in LLR. It should
be noted that the results of these studies coming from Asian
patient populations (9,10) are to be interpreted with caution,
since patients are considered obese with a BMI of 25
kg/m2, or even 24 kg/m2, contrary to the
World Health Organization (WHO) standard of BMI of 30
kg/m2 (11,12). Such a phenomenon constitutes an
additional strength of our report, since there are actually only
limited published data on LLR for a morbidly obese patient, in our
case with a BMI of 45 kg/m2.
In conclusion, to the best of our knowledge, this is
the first case report on laparoscopic liver resection for such a
morbidly obese patient in the context of advanced liver
cirrhosis.
References
|
1
|
Nguyen KT, Gamblin TC and Geller DA: World
review of laparoscopic liver resection-2,804 patients. Ann Surg.
250:831–841. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Twaij A, Pucher PH, Sodergren MH, Gall T,
Darzi A and Jiao LR: Laparoscopic vs open approach to resection of
hepatocellular carcinoma in patients with known cirrhosis:
Systematic review and meta-analysis. World J Gastroenterol.
20:8274–8281. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Cheung TT, Dai WC, Tsang SH, Chan AC, Chok
KS, Chan SC and Lo CM: Pure laparoscopic hepatectomy versus open
hepatectomy for hepatocellular carcinoma in 110 patients with liver
cirrhosis: A propensity analysis at a single center. Ann Surg.
264:612–620. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
ASA Physical Classification System.
2016.http://www.asahq.orgAccessed June
2016.
|
|
5
|
Pugh RN, Murray-Lyon IM, Dawson JL,
Pietroni MC and Williams R: Transection of the oesophagus for
bleeding oesophageal varices. Br J Surg. 60:646–649. 1973.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Dindo D, Demartines N and Clavien PA:
Classification of surgical complications: A new proposal with
evaluation in a cohort of 6336 patients and results of a survey.
Ann Surg. 240:205–213. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Utsunomiya T, Okamoto M, Kameyama T,
Matsuyama A, Yamamoto M, Fujiwara M, Mori M, Aimitsu S and Ishida
T: Impact of obesity on the surgical outcome following repeat
hepatic resection in Japanese patients with recurrent
hepatocellular carcinoma. World J Gastroenterol. 14:1553–1558.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Nomi T, Fuks D, Ferraz JM, Kawaguchi Y,
Nakajima Y and Gayet B: Influence of body mass index on
postoperative outcomes after laparoscopic liver resection. Surg
Endosc. 29:3647–3654. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Toriguchi K, Hatano E, Sakurai T, Seo S,
Taura K and Uemoto S: Laparoscopic liver resection in obese
patients. World J Surg. 39:1210–1215. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Uchida H, Iwashita Y, Saga K, Takayama H,
Watanabe K, Endo Y, Yada K, Ohta M and Inomata M: Benefit of
laparoscopic liver resection in high body mass index patients.
World J Gastroenterol. 22:3015–3022. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Kanazawa M, Yoshiike N, Osaka T, Numba Y,
Zimmet P and Inoue S: Criteria and classification of obesity in
Japan and Asia-Oceania. World Rev Nutr Diet. 94:1–12. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Obesity: Preventing and managing the
global epidemic. Report of a WHO Consultation. World Health Organ
Tech Rep Ser. 894:i–xii, 1–253. 2000.PubMed/NCBI
|