Introduction
Mycobacterium tuberculosis (TB) infection remains a
challenge to human health (1,2). Although abdominal TB is uncommon, the
peritoneum is commonly involved in patients with abdominal TB
infection (3,4). Charoensak et al (4) reported that certain cases with
tuberculous peritonitis may mimic other diseases, which represents
a diagnostic challenge for clinicians.
A few cases with intraperitoneal tuberculous
abscesses have been previously reported, whereas diaphragmatic
tuberculous abscess (DTA) is particularly rare (4–6). The aim
of this case report was to gain some experience regarding the
computed tomography (CT) findings in this DTA case, which was
pathologically confirmed, with the hope that it will be
contributory to the comprehensive CT diagnosis of DTAs.
Case report
The present study was reviewed and approved by the
Institutional Review Board of The Affiliated Hospital of Weifang
Medical University. The patient provided written informed concent
was provided to the publication of this case.
A 22-year-old male patient presented with night
sweats, easy fatigability and obscure right upper abdominal pain
for 60 days. The clinical examination of the patient did not
identify an abdominal palpable mass, and there was no history of
lung TB.
Plain CT scanning of the chest was performed using
the GE Bright Speed 16-detector spiral CT scanner (GE Medical
Systems, Chicago, IL, USA) with the following parameters: 120 KV,
130 mAs and 5 mm slice width. Contrast-enhanced abdominal CT
scanning was performed using the Siemens Somatom Sensation Cardiac
64-slice spiral CT scanner (Siemens, Munich, Germany) with the
following parameters: 120 KV, 200–390 mAs and 5 mm slice width. The
patient received intravenous Ultravist (300 mgI/ml; Bayer Schering
Pharma AG, Berlin, Germany) administered as a bolus, at an
injection rate of 3.0 ml/sec. Oral contrast material (water) was
administered.
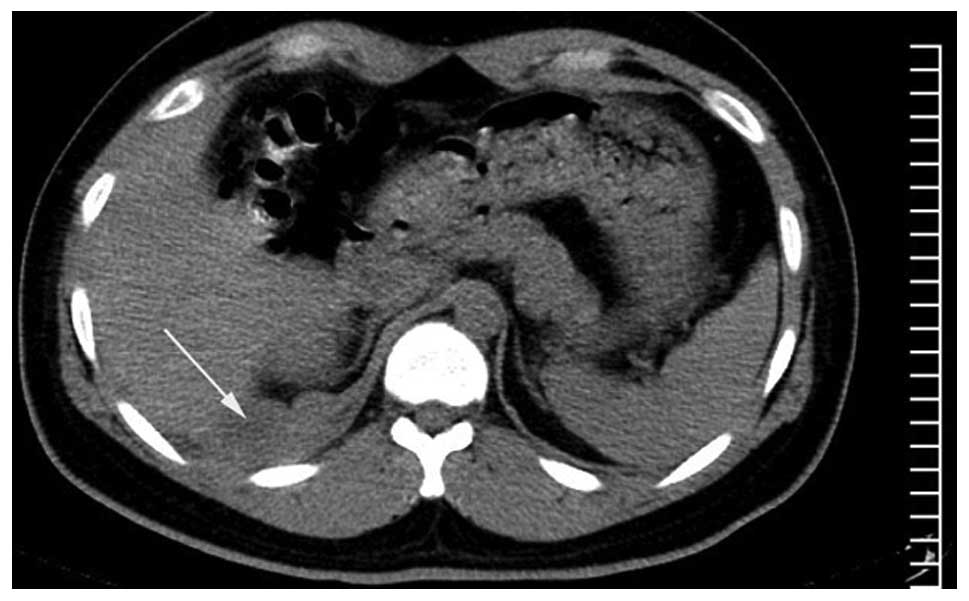
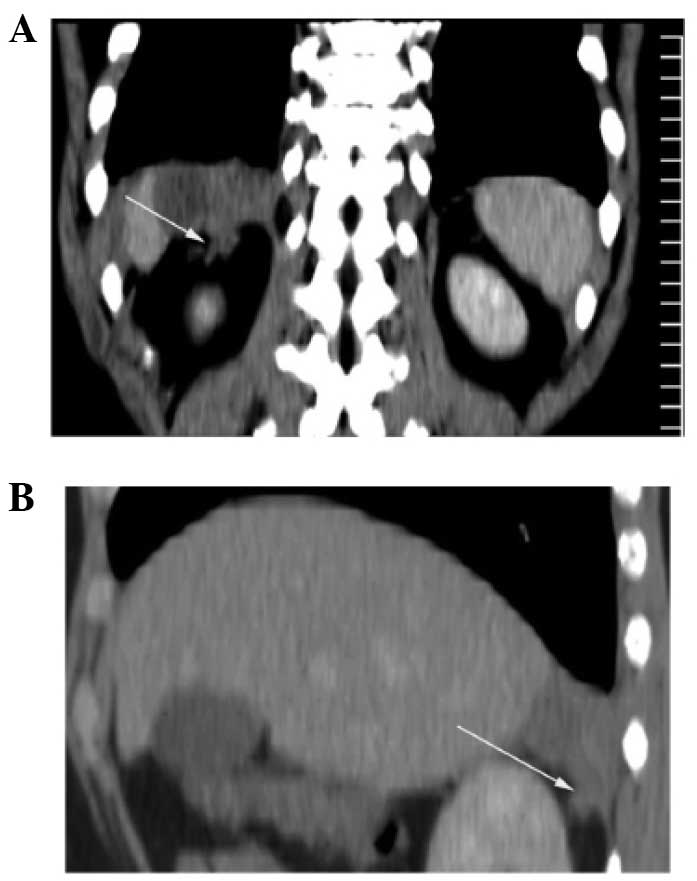
The CT images revealed a hypodense diaphragmatic
mass, sized 6.0×4.5×3.5 cm, pushing on the parenchyma of the liver.
The shape of the mass resembled an irregular double convex lens
based on the right side of the diaphragm. The wall of the mass
exhibited irregular thickening with enhancement. Gas collection or
calcification were not detected within the mass (Figs. 1–3). The
right side of the diaphragm was discontinuous. The right
retroperitoneal space and the adjacent pleura were invaded, with
marginally increased thickness of the subpleural fatty tissue
(Fig. 4). No enlarged lymph nodes
were detected in the mediastinum, root of the mesentery or upper
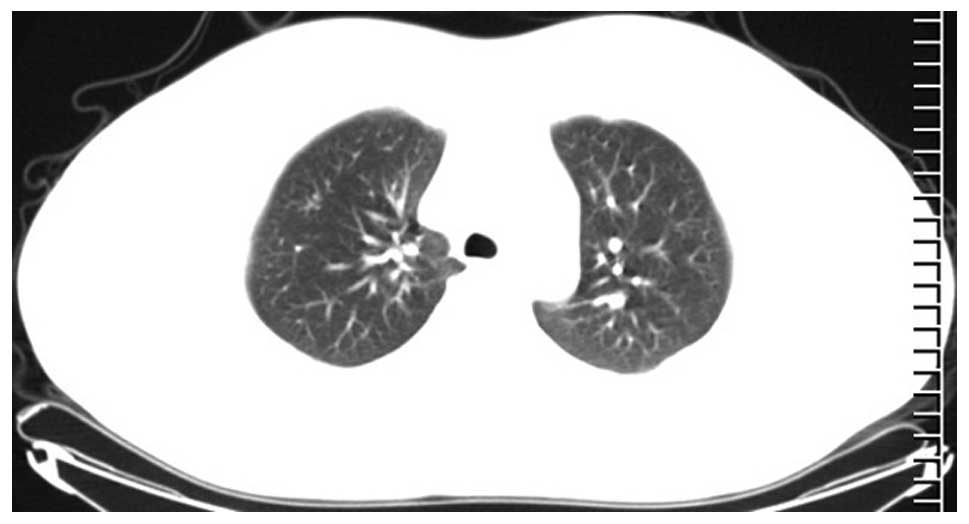
para-aortic region. No tuberculous lesion was detected on the
bilateral lung fields (Fig. 5).
Surgery was performed. The mass involved the right
side of the diaphragm and adhered to the liver. The small and large
bowel were normal. The pathological diagnosis was that of caseous
TB. After being treated with anti-tuberculosis drugs, the patient
fully recovered and was discharged from hospital.
Discussion
Tuberculous lesions are associated with a variable
spectrum of medical imaging manifestations, and they may mimic
other diseases (6–9). It is important to familiarize with the
CT manifestations of tuberculous lesions to ensure accurate CT
diagnosis.
Abdominal TB commonly spreads or disseminates by the
following routes: i) Intestinal TB spreading to the lymph nodes;
ii) hematogenous dissemination; and iii) direct extension of
adjacent tuberculous lesions (8).
Only a small proportion of patients with abdominal TB also suffer
from pulmonary TB (7). It has been
reported that multifocal TB may occur secondary to
lympho-hematogenous dissemination after the initial infection
(10). In our patient, the adjacent
pleura and retroperitoneal space were invaded, whereas no enlarged
lymph nodes or other tuberculous lesions were detected. This
indicates that the spreading route of this case of DTA may be
hematogenous dissemination.
The reasons for the rarity of skeletal muscle TB may
be as follows: i) High levels of lactic acid; ii) not enough
reticuloendothelial tissue; iii) not enough lymphatic tissue; and
iv) rich blood supply (11,12). Thus, the abovementioned reasons may
help to explain the rarity of the DTA.
In the present study, the wall of the DTA was
irregularly thickened with permanent enhancement, which was similar
to the cases reported in the literature (6). The right retroperitoneal space displayed
fibrous strands neighboring the mass, which also conformed to
inflammatory changes. In this case, the shape of the abscess
(irregular double convex lens), the simultaneous involvement of the
pleural cavity and retroperitoneal space with a discontinuous
diaphragm on CT images may help with the localization and
diagnosis.
Differential diagnosis
Most inflammations of the diaphragm result from
direct extension from adjacent lesions (13), whereas lung cancer may directly invade
the diaphragm (14). In this case, no
lesions were detected within the lung field.
Malignant pleural mesothelioma may involve the
diaphragm, and trans-diaphragmatic extension may be detected on CT
examination (15). A rind-like
pleura, with a thickness of >10 mm is crucial for the diagnosis
of malignant pleural mesothelioma (16). Increased thickness of the subpleural
fatty tissue was the sign for the diagnosis of benign pleural
lesion on CT images (16). In the
present case, the subpleural fatty tissue adjacent to the
diaphragmatic mass was thicker compared with that of the
contralateral side, which conformed to the diagnosis of a benign
pleural lesion.
It may be difficult to distinguish diaphragmatic
from abdominal tumors, particularly in the case of tumors arising
from the right side of the diaphragm (17). In the present case, no abnormal signs
were detected within the liver parenchyma and peritoneum.
Primary tumors of the diaphragm are rare, and the
most common benign lesions are diaphragmatic cysts (18). The CT density of the diaphragmatic
mesothelial cyst is similar to that of water, and the margin is
well-defined without enhancement (19), which was different from the findings
in this case.
In summary, DTA, despite its rarity, should be
suspected in patients with a diaphragmatic hypodense mass
exhibiting enhanced thick wall, even in the absence of enlarged
lymph nodes on CT images.
References
|
1
|
Lee WK, Van Tonder F, Tartaglia CJ, Dagia
C, Cazzato RL, Duddalwar VA and Chang SD: CT appearances of
abdominal tuberculosis. Clin Radiol. 67:596–604. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
LoBue PA, Enarson DA and Thoen TC:
Tuberculosis in humans and its epidemiology, diagnosis and
treatment in the United States. Int J Tuberc Lung Dis.
14:1226–1232. 2010.PubMed/NCBI
|
|
3
|
Khan R, Abid S, Jafri W, Abbas Z, Hameed K
and Ahmad Z: Diagnostic dilemma of abdominal tuberculosis in
non-HIV patients: An ongoing challenge for physicians. World J
Gastroenterol. 12:6371–6375. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Charoensak A, Nantavithya P and
Apisarnthanarak P: Abdominal CT findings to distinguish between
tuberculous peritonitis and peritoneal carcinomatosis. J Med Assoc
Thai. 95:1449–1456. 2012.PubMed/NCBI
|
|
5
|
Dong P, Chen JJ, Wang XZ and Wang YQ:
Intraperitoneal tuberculous abscess: Computed tomography features.
World J Radiol. 7:286–293. 2015.PubMed/NCBI
|
|
6
|
Dong P, Wang B and Sun YQ: Tuberculous
abscess in the hepatoduodenal ligament: Evaluation with
contrast-enhanced computed tomography. World J Gastroenterol.
14:2284–2287. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Akhan O and Pringot J: Imaging of
abdominal tuberculosis. Eur Radiol. 12:312–323. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Yang ZG, Min PQ, Sone S, He ZY, Liao ZY,
Zhou XP, Yang GQ and Silverman PM: Tuberculosis versus lymphomas in
the abdominal lymph nodes: Evaluation with contrast-enhanced CT.
AJR Am J Roentgenol. 172:619–623. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Yang GY, Zhao D, Zhang WZ, Meng J, Li J,
Li XH and Wan HF: Role of ultrasound evaluation for the diagnosis
and monitoring of thyroid tuberculosis: A case report and review of
the literature. Oncol Lett. 9:227–230. 2015.PubMed/NCBI
|
|
10
|
Al-Tawfiq JA: Multifocal systemic
tuberculosis: The many faces of an old nemesis. Med Sci Monit.
13:CS56–CS60. 2007.PubMed/NCBI
|
|
11
|
Chewoolkar V, Bichile L and Patel H:
Pyomyositis with multifocal osteomyelitis - an uncommon
presentation of skeletal tuberculosis. J Assoc Physicians India.
57:7062009.PubMed/NCBI
|
|
12
|
Neogi DS, Bandekar SM and Chawla L:
Skeletal muscle tuberculosis simultaneously involving multiple
sites. J Pediatr Orthop B. 22:167–169. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Ye Y, Yang Z, Li H, Deng W, Li Y and Guo
Y: MDCT features and anatomic-pathology in right thoracic-abdominal
junctional region diseases. Sheng Wu Yi Xue Gong Cheng Xue Za Zhi.
28:255–259. 2011.(In Chinese). PubMed/NCBI
|
|
14
|
Yokoi K, Tsuchiya R, Mori T, Nagai K,
Furukawa T, Fujimura S, Nakagawa K and Ichinose Y: Results of
surgical treatment of lung cancer involving the diaphragm. J Thorac
Cardiovasc Surg. 120:799–805. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Nickell LT Jr, Lichtenberger JP III,
Khorashadi L, Abbott GF and Carter BW: Multimodality imaging for
characterization, classification and staging of malignant pleural
mesothelioma. Radiographics. 34:1692–1706. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Metintas M, Ucgun I, Elbek O, Erginel S,
Metintas S, Kolsuz M, Harmanci E, Alatas F, Hillerdal G, Ozkan R
and Kaya T: Computed tomography features in malignant pleural
mesothelioma and other commonly seen pleural diseases. Eur J
Radiol. 41:1–9. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Asahi Y, Kamiyama T, Nakanishi K, Yokoo H,
Tahara M, Usui A, Funakoshi T, Sato M, Sasaki A, Matsuno Y, et al:
Chondroma of the diaphragm mimicking a giant liver tumor with
calcification: Report of a case. Surg Today. 44:2361–2365. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Kim MP and Hofstetter WL: Tumors of the
diaphragm. Thorac Surg Clin. 19:521–529. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Esparza Estaún J, González Alfageme A and
Sáenz Bañuelos J: Radiological appearance of diaphragmatic
mesothelial cysts. Pediatr Radiol. 33:855–858. 2003. View Article : Google Scholar : PubMed/NCBI
|