Introduction
Hashimoto's thyroiditis is autoimmune thyroid
disease in children. The most principal locations of pediatric
thyroid disease is in iodine-sufficient areas worldwide (1). At the time of diagnosis, thyroid
function of children and adolescent with Hashimoto's thyroiditis
may significantly vary in the different pediatric reports, ranging
from euthyroidism to overt hypothyroidism or occasionally,
hyperthyroidism (2–7). Epidemiological data showed that thyroid
cancer frequently occurs in the context of one of the most common
autoimmune thyroid diseases, Hashimoto's thyroiditis (8). The possible association between
Hashimoto's thyroiditis (HT) and papillary thyroid carcinoma (PTC)
remains controversial. The association between HT and PTC is also
supported by the observation that rearrangements of the rearranged
during transfection (RET) oncogene is frequently detected in PTC
(9).
Case report
A 15-year-old adolescent girl was admitted to a
local hospital and a left neck mass (~1.0×1.5 cm2) was
found one year ago. The mass was not accompanied by pain, itching,
chills, fever and cough; however, the girl did experienced weight
loss, heat intolerance and sweating. The patient had taken Chinese
herbal medicine, however this had no effect. She visited a local
hospital for treatment 9 months ago. Physical examination revealed
the painless left goiter ~1.5×1.5 cm2, without vascular
murmur. Laboratory examination results revealed normal thyroid
function, anti-thyroglobulin antibody (TG-Ab) of 52.35% (<30%)
and anti-thyroid microsomal antibody (TM-Ab) of 37.01% (<20%).
The neck ultrasound examination revealed no thyroid lesions. It was
diagnosed as Hashimoto's thyroiditis. After 3 months of
observation, the neck mass had grown. The neck ultrasound
examination revealed that a left lobe of the thyroid exhibited
multiple solid hypoechoic nodules and calcification to the left
neck lymph nodes. The right thyroid lobe and isthmus were normal. A
lymph node biopsy revealed carcinoembryonic antigen (CA)125, 173.52
U/ml (0–35) and left neck metastasis were observed in papillary
thyroid carcinoma. Possible diagnoses were: i) Left cervical lymph
node metastatic papillary adenocarcinoma; ii) left thyroid cancer;
iii) Hashimoto's thyroiditis. Surgery was performed and the total
left thyroid lobe and most of the right lobe were resected.
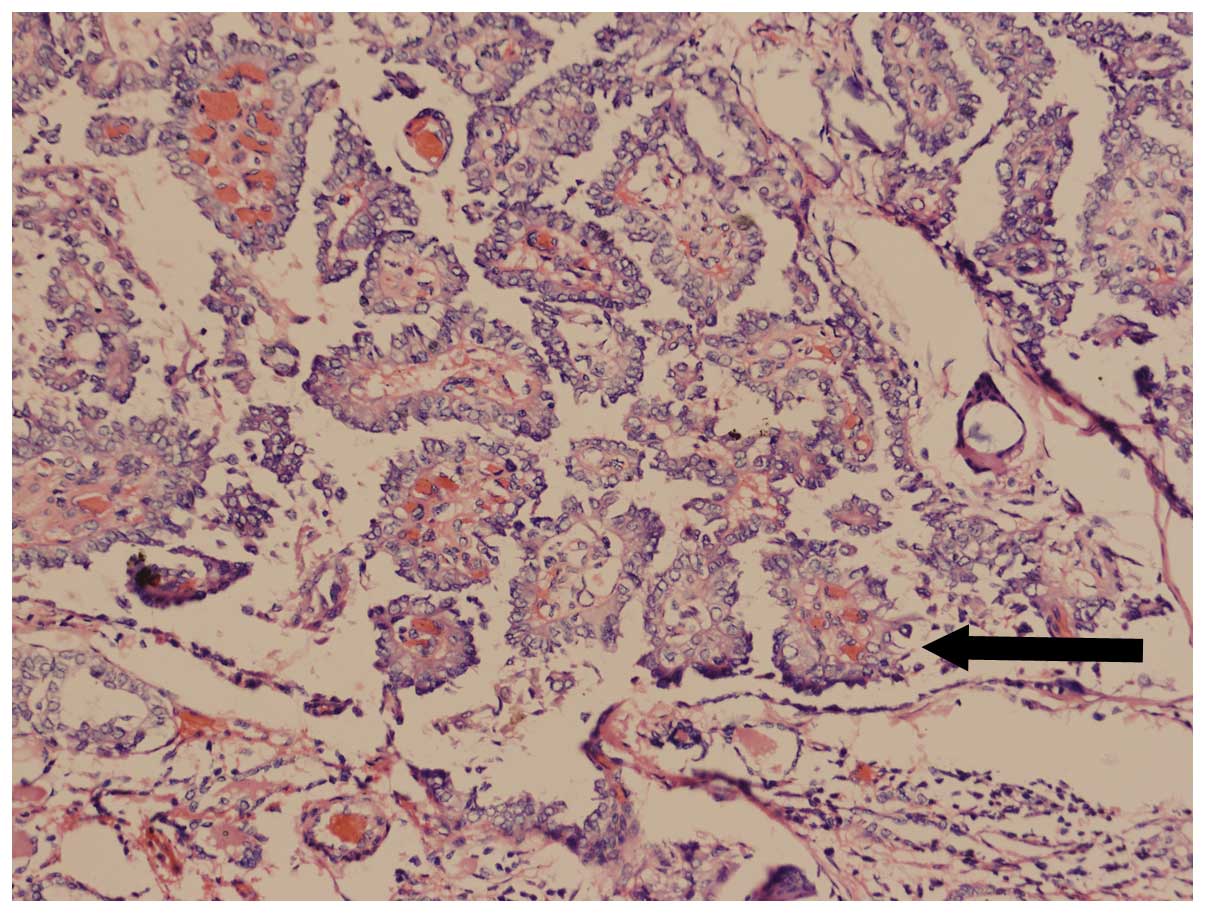
Pathological examination indicated that the patient was suffering
from papillary thyroid carcinoma (Figs.
1 and 2), with cervical lymph
node metastasis. Following chemotherapy and appropriate symptomatic
treatment, the patient recovered well.
Discussion
Hashimoto's thyroiditis, also termed chronic
lymphocytic thyroiditis, an autoimmune disease, is the most common
cause of hypothyroidism in children and adolescents. Previous
histological investigations demonstrated that lymphocyte
infiltration accompanied lymphoid follicles. In recent years, as a
result of the popularity of TM-Ab and TG-Ab, more cases are being
identified. It has been shown that ~1% of school children are
diagnosed with Hashimoto's thyroiditis. It is common children
between 6 and 16-years-old, particularly 10–11 year-old and those
in the peak of puberty. Females are more likely to have this
disease comapred with males, the ratio being ~4–9:1. Hashimoto's
thyroiditis develops slowly and is normally only diagnosed when the
patient visits the hospital due to of thyroid goiter. Generally, no
symptoms are exhibited, and only 8% suffer from hyperthyroidism and
~8% of patients finally get hypothyroidism. Therefore, symptoms are
associated with the disease duration and thyroid functionality.
Thyroid cancer accounts for ~1% of all cancer cases.
Papillary adenocarcinoma is widely distributed among all ages, from
children <10-years-old to centenarians (10). Childhood thyroid carcinoma reveals an
increasing trend. The Beijing Children's Hospital (Beijing, China)
pathologically confirmed 10 thyroid cancer cases (0.7% in 1,379
malignancies). Other reports indicated that these cases occur in
~3.7–5% children <15-years-old. Thyroid cancer is common in
10–14-year-olds, particularly girls. The ratio between male to
female is 1:2-3. More reported Hashimoto's thyroiditis merger
thyroid cancer cases are identified in adults, where as very few
cases are reported in children. Japan reported only one case in a
child in 2003 (11), and no child
cases have been reported in China.
Hashimoto's thyroiditis with thyroid cancer
pathogenesis remains unclear. Many hypotheses exist as to why
Hasimoto's thyroiditis occurs. It is possible that Hashimoto's
thyroiditis is thyroid chronic inflammation, which causes the
thyroid gland structural damage and affects thyroid hormone
production negative feedback to stimulate thyroid-stimulating
hormone (TSH) secretion. Long-term high levels of TSH stimulation
in the goiter may stimulate thyroid cancer (12). It is also possible that the patient
with Hashimoto's thyroiditis has organ-specific suppressor T
lymphocyte dysfunction, which reduces the role of local immune
surveillance and leads to the occurrence of thyroid cancer.
Molecular biology investigations also found that p53, B-cell
lymphoma-2 and RET genes are closely associated with the incidence
of thyroid cancer (13,14), providing another possibly explanation.
Hashimoto's thyroiditis is often accompanied with a large number of
lymphoid tissue cell infiltration and lymphoid follicles. Chronic
antigenic stimulation may cause neoplastic hyperplasia of thyroid
follicular, and thus malignant transformation. Finally, high iodine
intake significantly increased the risk of thyroid cancer. This
also increased the incidences of Hashimoto's thyroiditis, which may
easily lead to iodine and thyroid epithelial cell injury, and
immune dysfunction.
As a result of the complexity of the clinical
manifestations of Hashimoto's thyroiditis, it can be expressed as
not only hyperthyroidism or hypothyroidism, but also normal thyroid
function. Notably, the most common cases exhibit hypothyroidism.
Long-term treatment, and for children with thyroid cancer, early
diagnosis, is particularly difficult. In the present case, the
diagnosis of Hashimoto's thyroiditis is primarily based on the
clinical manifestations, TG-Ab and TM-Ab. The only diagnostic
imaging ultrasound was negative (data not shown). The patient did
not undergo fine needle aspiration cytology diagnosis of the
disease. Therefore, this child may be exhibiting one of two
situations: i) Hashimoto's thyroiditis, which develops into thyroid
cancer later; ii) thyroid cancer, with Hashimoto's thyroiditis
being diagnosed at the early stages. The present study hypothesized
that in either case, the clinical diagnosis of thyroid disease
provide a warning for the early diagnosis of Hashimoto's
thyroiditis. Following treatment or regular observation, if no
significant improvement is observed, the emergence of nodules
evident in children can be an alert to the possibility of the
coexistence of tumor nature. To improve the diagnosis accuracy,
besides detailed examination, the necessary laboratory
examinations, including ultrasound, computed tomography and other
imaging methods, must be performed. Ultrasound-guided fine needle
aspiration cytology prior to surgery can assist with identifying
the disease (15).
Acknowledgements
The present study was supported by a grant from
Chengdu Science and Technology Bureau project of China (no.
2014-HM01-00052-SF).
Glossary
Abbreviations
Abbreviations:
|
TG-Ab
|
anti-thyroglobulin antibody
|
|
TM-Ab
|
anti-thyroid microsomal antibody
|
|
CA125
|
carcinoembryonic antigen 125
|
References
|
1
|
Wasniewska M, Vigone MC, Cappa M, Aversa
T, Rubino M and De Luca F: Study Group for Thyroid diseases of
Italian Society for Pediatric Endocrinology: Acute suppurative
thyroiditis in childhood: relative frequency among thyroid
inflammatory diseases. J Endocrinol Invest. 30:346–347. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Zak T, Noczyńska A, Wasikowa R,
Zaleska-Dorobisz U and Golenko A: Chronic autoimmune thyroid
disease in children and adolescents in the years 1999–2004 in Lower
Silesia, Poland. Hormones. 4:45–48. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Gopalakrishnan S, Chugh PK, Chhillar M,
Ambardar VK, Sahoo M and Sankar R: Goitrous autoimmune thyroiditis
in a pediatric population: a longitudinal study. Pediatrics.
122:e670–e674. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Demirbilek H, Kandemir N, Gonc EN, Ozon A
and Alikasifoglu A: Assessment of thyroid function during the long
course of Hashimoto's thyroiditis in children and adolescents. Clin
Endocrinol. 71:451–454. 2009. View Article : Google Scholar
|
|
5
|
Skarpa V, Kappaousta E, Tertipi A,
Anyfandakis K, Vakaki M, Dolianiti M, Fotinou A and Papathanasiou
A: Epidemiological characteristics of children with autoimmune
thyroid disease. Hormones. 10:207–214. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Özen S, Berk Ö, Şimşek DG and Darcan S:
Clinical course of Hashimoto's thyroiditis and effects of
levothyroxine therapy on the clinical course of the disease in
children and adolescents. J Clin Res Pediatr Endocrinol. 3:192–197.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
De Luca F, Santucci S, Corica D, Pitrolo
E, Romeo M and Aversa T: Hashimoto's thyroiditis in childhood:
presentation modes and evolution over time. Italian Journal of
Pediatrics. 39:82013. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Guarino V, Castellone MD, Avilla E and
Melillo RM: Thyroid cancer and inflammation. Molecular and Cellular
Endocrinology. 321:94–102. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Mechler C, Bounacer A, Suarez H, Saint FM,
Magois C, Aillet G and Gaulier A: Papillary thyroid carcinoma: 6
cases from 2 families with associated lymphocytic thyroiditis
harbouring RET/PTC rearrangements. Br J Cancer. 85:1831–1837. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Repplinger D, Bargren A, Zhang YW, Adler
JT, Haymart M and Chen H: Is Hashimoto's thyroiditis a risk factor
for papillary thyroid cancer? J Surg Res. 150:49–52. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Yagasaki H, Inukai T, Uno K, Akahane K,
Nemoto A, Takahashi K, Sato H, Goi K, Mouri N, Takano K, et al:
Development of severe aplastic anemia in a girl with Hashimoto's
thyroiditis and papillary thyroid carcinoma. Rinsho Ketsueki.
44:328–333. 2003.(In Japanese). PubMed/NCBI
|
|
12
|
Fiore E, Rago T, Latrofa F, Provenzale MA,
Piaggi P, Delitala A, Scutari M, Basolo F, Di Coscio G, Grasso L,
et al: Hashimoto's thyroiditis is associated with papillary thyroid
carcinoma: Role of TSH and of treatment with L-thyroxine. Endocr
Relat Cancer. 18:429–437. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Burstein DE, Nagi C, Wang BY and Unger P:
Immunohistochemical detection of p53 homolog p63 in solid cell
nests, papillary thyroid carcinoma and hashimoto's thyroiditis: A
stem cell hypothesis of papillary carcinoma oncogenesis. Hum
Pathol. 35:465–473. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Kang DY, Kim KH, Kim JM, Kim SH, Kim JY,
Baik HW and Kim YS: High prevalence of RET, RAS and ERK expression
in Hashimoto's thyroiditis and in papillary thyroid carcinoma in
the Korean population. Thyroid. 17:1031–1038. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Haberal AN, Toru S, Ozen O, Arat Z and
Bilezikçi B: Diagnostic pitfalls in the evaluation of fine needle
aspiration cytology of the thyroid: Correlation with histopathology
in 260 cases. Cytopathology. 20:103–108. 2009. View Article : Google Scholar : PubMed/NCBI
|