Introduction
Lung cancer is the leading cause of cancer-related
mortality worldwide (1). Brain
metastasis (BM) is a common secondary localization of the disease
in lung cancer patients, encountered in ~7.4% of non-small-cell
lung cancer (NSCLC) cases at diagnosis (2), and 25–30% of the cases over the course
of the disease (3). The prognosis of
NSCLC with BM is poor and the mortality is high (4,5). The most
common treatment for these patients is radiation therapy (6,7); however,
the therapeutic options are limited in an emergency setting, as
well as for end-stage patients. In this report, we present the case
of a NSCLC patient with BM who received epidermal growth factor
receptor-tyrosine kinase inhibitor (EGFR-TKI) therapy, with quick
regression of the symptoms. The present case suggests that EGFR-TKI
therapy may be effective for late-stage NSCLC patients, or in an
emergency setting.
Case report
On, November 19, 2013, a 74-year-old female patient
was admitted to the Respiratory Department of The Second Affiliated
Hospital of Zhejiang University School of Medicine (Hangzhou,
China) complaining of persistent cough and progressive dyspnea. The
patient had already undergone a lung computed tomography (CT) scan
at a local hospital, which revealed a mass in the lower lobe of the
left lung, combined with left pleural effusion and mediastinal
lymph node enlargement. Following admission, a contrast-enhanced CT
revealed a mass sized ~98×79 mm, blocking the left main bronchus
and invading the left pulmonary artery and its branches.
Bronchoscopy was performed and a tumor was identified in the left
lower airway. Pathological examination of a biopsy specimen
identified the lesion as lung adenocarcinoma. Genetic analysis
identified an exon 19 EGFR mutation in the patient. Following
magnetic resonance imaging and ultrasound studies, metastases were
found in the brain, skull, adrenal gland and abdominal lymph nodes.
No significant symptoms or body dysfunction were associated with
the metastases, except for a painless horn-like protrusion on the
right side of the forehead. administration of EGFR-TKI therapy was
immediately recommended. However, the patient's family rejected
this treatment strategy due to its high cost, and opted for
chemotherapy instead. Pemetrexed disodium (75 mg/m2) and
carboplatin (area under the curve = 5) were administered every 21
days for a total of two cycles.
Eleven days after the second cycle of chemotherapy,
the patient was admitted to our hospital due to left body
dysfunction for 5 days. The physical examination revealed no
changes in muscle tone. Muscle strength was rated 0/5 in the left
upper limb and 1/5 in the left lower limb. The right-sided muscle
strength was 5/5. The right patellar tendon reflex was rated as 2+,
but was absent on the left side. The Babinski sign was negative.
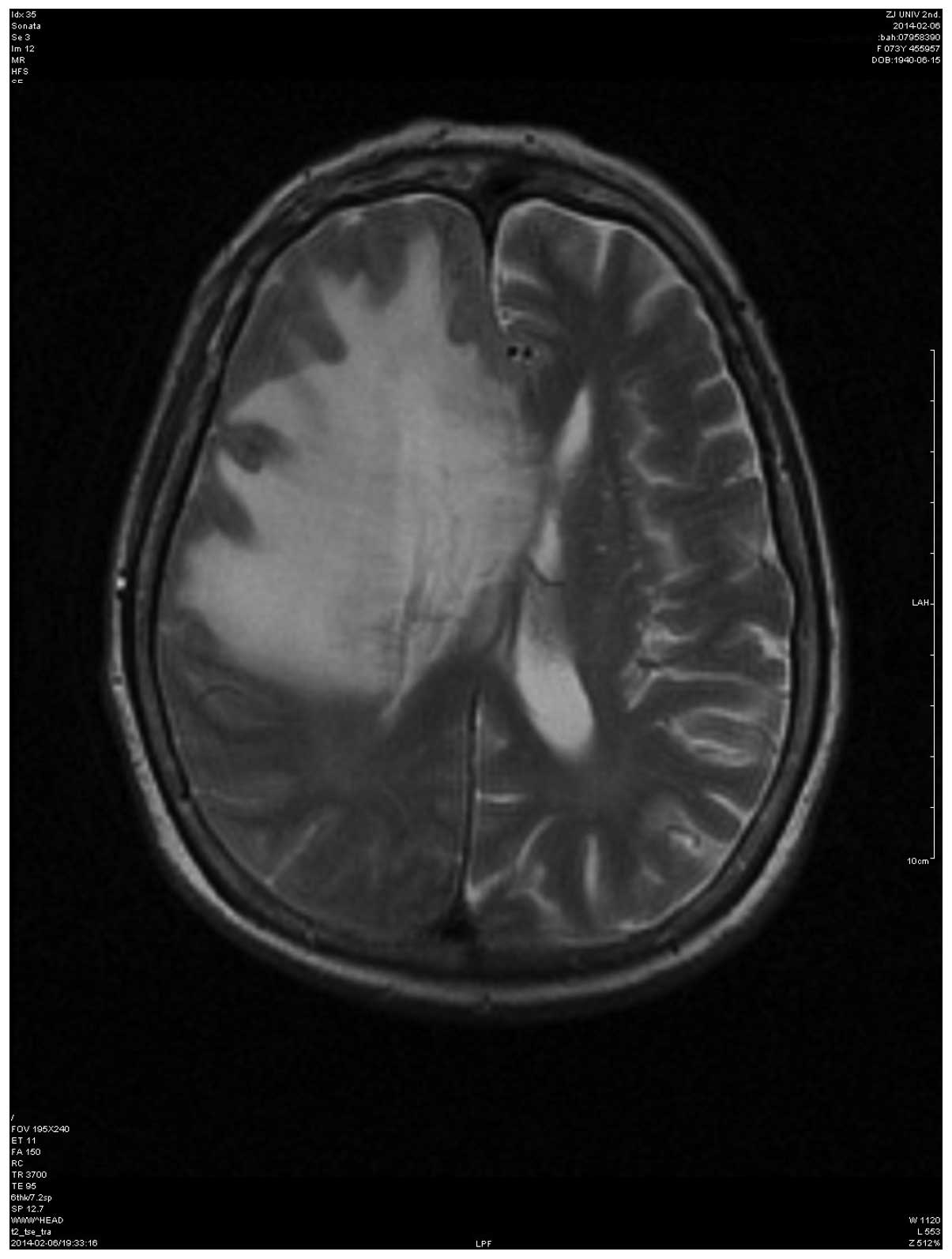
The patient underwent an emergency brain MRI scan, which revealed
that the brain metastatic lesion had grown significantly compared
with the original scan. Contrast-enhanced MRI showed T1 and T2
hyperintense changes in the superior frontal gyrus, as well as
enhancement in the nodular zones of the meninges surrounded with
cerebral edema, destruction of the frontoparietal bone plate and
diploe. The right anterior horn of the lateral ventricle was
compressed and the midline was shifted to the left. Imaging
diagnoses included frontal bone malignancy with involvement of the
superior frontal gyrus, which was considered as metastasis
(Fig. 1).
D-glycerol and steroids were initially administered,
but this treatment was ineffective. Moreover, brain surgery was
strongly recommended to avoid cerebral herniation; however, the
patient's family rejected surgical intervention. administration of
the EGFR-TKI icotinib (125 mg, p.o. 3 times/day) was then
recommended, to which the family agreed. Surprisingly, the
patient's left body function progressively improved after taking 4
tablets. The physical examination revealed that the muscle strength
of the left upper limb was 2/5 and of the left lower limb 3/5. The
Babinski sign was negative. After 48 h, the left body dysfunction
had resolved. In addition, the dimensions of the horn-like lesion
on the patient's forehead markedly decreased, from 18.3×2.3 to
12.2×1.5 cm. After 4 days of observation, the patient was
discharged.
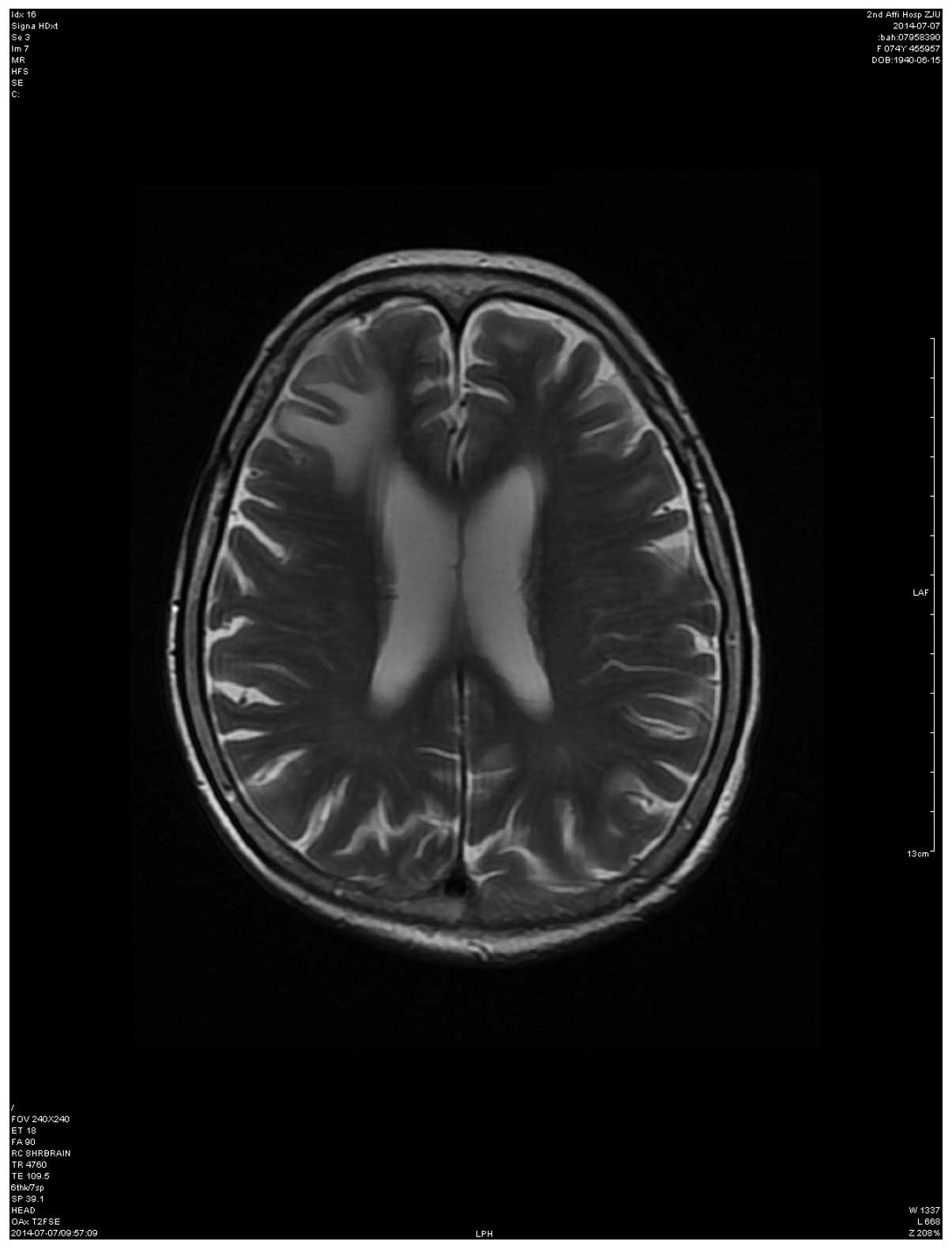
Over 4 months later, the patient underwent a
follow-up brain MRI scan, which revealed that the metastatic lesion
was significantly smaller compared with prior to treatment
(Fig. 2). In October, 2014, the
patient remained alive and was continuing icotinib therapy, without
other chemotherapies.
Discussion
Approximately 20–40% of NSCLC patients develop BM,
which is associated with a poor prognosis. The majority of these
patients survive for 3–6 months and the 1-year survival rate is 10%
(4,8,9).
Considerable efforts have been made to explore additional or
alternative treatment modalities to improve survival, quality of
life and local tumor control.
For patients with a single metastatic lesion in the
brain, whole-brain radiation therapy (WBRT) is the standard of
care, and is often combined with chemotherapy or surgery. When
combined with surgical resection, WBRT reduces the risk or relapse
and may increase the overall survival of patients with BM (5,10).
Moreover, the combined treatment of pemetrexed-cisplatin with
concurrent WBRT has been proven effective in patients with NSCLC
and BM (11). However, these
treatment protocols require the patients to be in relatively good
health (i.e., high Karnofsky performance status score) prior to
treatment. If a patient is in poor health, as is common with
advanced NSCLC, fewer treatment options are available.
In the present case, the patient had a large
metastatic lesion in the brain, which invaded the skull in the area
of the forehead and caused a midline shift, potentially increasing
the risk of increased intracranial pressure (IICP). Glycerol and
steroid therapy was not effective in this patient. Given the
patient's severe conscious impairment and increasing IICP, she was
in an emergency situation requiring a rapid response. Ideally,
local control of tumor progression by surgical removal, with or
without radiation or radiosurgery, may be the first or optimal
method to manage IICP, as illustrated by a previous case of a
57-year-old female patient with a large BM who was succesfully
treated with macroscopically complete excision of the brain tumor
and postoperative radiotherapy (12).
However, in our case, our patient had a poor baseline performance
status, she was elderly, and the large lung tumor caused left lung
atelectasis and invaded the left pulmonary artery, which further
increased the risk associated with anesthesia and surgery. Second,
edema and brain injury following surgery or radiotherapy is highly
possible, potentially compromising the patient's quality of life.
The primary tumor in the lung was not sensitive to radiotherapy;
therefore surgery and WBRT were not considered to be a safe and
effective option for this patient.
As an alternative to WBRT, other therapeutic
approaches are available to treat BM. Drugs targeting mutated EGFR
and anaplastic lymphoma kinase (ALK) genes have been highly
effective when administered systemically (13,14).
Several reports demonstrated that gefitinib or icotinib are
associated with a favorable response in lung adenocarcinoma with
BM, particularly in cases harboring EGFR mutations, such as our
patient (15–19). EGFR-TKIs are reported to cross the
blood-brain barrier, although it has been suggested that TKI
concentration is reduced in the central nervous system compared
with the serum levels (20). In such
cases, increased doses may improve the efficacy (21). However, in the present case, the
standard dose of icotinib quickly relieved the patient's symptoms
and suppressed the growth of the metastatic lesion for at least 4
months.
The current standard approach to the management of a
life-threatening BM is surgery and radiotherapy. In the present
case, we demonstrated that NSCLC with BM may be efficiently treated
with the EGFR-TKI icotinib. A standard dose of icotinib reduced the
size of the brain lesion and relieved the patient's symptoms as
quickly as surgery. Icotinib decreased the size of the protrusion
on the patient's forehead as well as the size of the brain mass in
~12 h, which was confirmed by recovery of left body function. This
rapid effect may be attributed to two reasons: First, genetic
analysis of the primary tumor identified an exon 19 mutation in the
EGFR gene. It has been reported that primary tumor EGFR status is a
good surrogate for EGFR mutation status of the BM, with a
concordance rate of 93.3% (22).
Second, our patient's brain had a large lesion, which disrupted the
frontoparietal bone plate and diploe. This damage may have
facilitated the transport of icotinib across the blood-brain
barrier.
Therefore, our case suggests that EGFR-TKI treatment
may be a quick, safe and effective option for patients with BM,
particularly those harboring an EGFR mutation, with a poor
functional status, or in an emergency situation.
Acknowledgements
The present study was supported in part by
Department of Education of Zhejiang province (grand no.
Y201121356).
References
|
1
|
Jemal A, Bray F, Center MM, Ferlay J, Ward
E and Forman D: Global cancer statistics. CA Cancer J Clin.
61:69–90. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Schuette W: Treatment of brain metastases
from lung cancer: Chemotherapy. Lung Cancer. 45(Suppl 2):
S253–S257. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Langer CJ and Mehta MP: Current management
of brain metastases, with a focus on systemic options. J Clin
Oncol. 23:6207–6219. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Patchell RA, Tibbs PA, Walsh JW, Dempsey
RJ, Maruyama Y, Kryscio RJ, Markesbery WR, Macdonald JS and Young
B: A randomized trial of surgery in the treatment of single
metastases to the brain. N Engl J Med. 322:494–500. 1990.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Patchell RA, Tibbs PA, Regine WF, Dempsey
RJ, Mohiuddin M, Kryscio RJ, Markesbery WR, Foon KA and Young B:
Postoperative radiotherapy in the treatment of single metastases to
the brain: A randomized trial. JAMA. 280:1485–1489. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Hazard LJ, Jensen RL and Shrieve DC: Role
of stereotactic radiosurgery in the treatment of brain metastases.
Am J Clin Oncol. 28:403–410. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Qin H, Pan F, Li J, Zhang X, Liang H and
Ruan Z: Whole brain radiotherapy plus concurrent chemotherapy in
non-small cell lung cancer patients with brain metastases: A
meta-analysis. PLoS One. 9:e1114752014. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Hsiung CY, Leung SW, Wang CJ, Lo SK, Chen
HC, Sun LM and Fang FM: The prognostic factors of lung cancer
patients with brain metastases treated with radiotherapy. J
Neurooncol. 36:71–77. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Lagerwaard FJ, Levendag PC, Nowak PJ,
Eijkenboom WM, Hanssens PE and Schmitz PI: Identification of
prognostic factors in patients with brain metastases: A review of
1292 patients. Int J Radiat Oncol Biol Phys. 43:795–803. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Armstrong JG, Wronski M, Galicich J, Arbit
E, Leibel SA and Burt M: Postoperative radiation for lung cancer
metastatic to the brain. J Clin Oncol. 12:2340–2344.
1994.PubMed/NCBI
|
|
11
|
Dinglin XX, Huang Y, Liu H, Zeng YD, Hou X
and Chen LK: Pemetrexed and cisplatin combination with concurrent
whole brain radiotherapy in patients with brain metastases of lung
adenocarcinoma: A single-arm phase II clinical trial. J Neurooncol.
112:461–466. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Kataoka K, Uejima T, Niiyama K, Kuroda R,
Arita N, Ioku M, Yamada K, Taneda M and Hayakawa T: Long survival
after removal of a huge brain tumor which had metastasized from a
lung cancer: Case report. Neurological Surgery. 22:339–341.
1994.(In Japanese). PubMed/NCBI
|
|
13
|
Ettinger DS, Akerley W, Borghaei H, Chang
AC, Cheney RT, Chirieac LR, D'Amico TA, Demmy TL, Govindan R,
Grannis FW Jr, et al: National comprehensive cancer network:
Non-small cell lung cancer, version 2. 2013. J Natl Compr Canc
Netw. 11:645–653; quiz 653. 2013.PubMed/NCBI
|
|
14
|
Shaw AT, Kim DW, Nakagawa K, Seto T, Crinó
L, Ahn MJ, De Pas T, Besse B, Solomon BJ, Blackhall F, et al:
Crizotinib versus chemotherapy in advanced ALK-positive lung
cancer. N Engl J Med. 368:2385–2394. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Ceresoli GL, Cappuzzo F, Gregorc V,
Bartolini S, Crinò L and Villa E: Gefitinib in patients with brain
metastases from non-small-cell lung cancer: A prospective trial.
Ann Oncol. 15:1042–1047. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Park SJ, Kim HT, Lee DH, Kim KP, Kim SW,
Suh C and Lee JS: Efficacy of epidermal growth factor receptor
tyrosine kinase inhibitors for brain metastasis in non-small cell
lung cancer patients harboring either exon 19 or 21 mutation. Lung
Cancer. 77:556–560. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Jung YH, Han CW, Jung YD, Cho YY and Han
DJ: Complete remission of brain metastases in non-small cell lung
cancer patients harboring an EGFR mutation treated with tyrosine
kinase inhibitor without radiotherapy: A report of 3 cases. Case
Rep Oncol. 7:149–154. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Iuchi T, Shingyoji M, Sakaida T, Hatano K,
Nagano O, Itakura M, Kageyama H, Yokoi S, Hasegawa Y, Kawasaki K
and Iizasa T: Phase II trial of gefitinib alone without radiation
therapy for Japanese patients with brain metastases from
EGFR-mutant lung adenocarcinoma. Lung Cancer. 82:282–287. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Sun X and Zheng Y: Retreatment with
icotinib in a patient with metastatic lung adenocarcinoma. Tumori.
99:e124–e126. 2013.PubMed/NCBI
|
|
20
|
Zhao J, Chen M, Zhong W, Zhang L, Li L,
Xiao Y, Nie L, Hu P and Wang M: Cerebrospinal fluid concentrations
of gefitinib in patients with lung adenocarcinoma. Clin Lung
Cancer. 14:188–193. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Yuan Y, Tan C, Li M, Shen H, Fang X, Hu Y
and Ma S: Activity of pemetrexed and high-dose gefitinib in an
EGFR-mutated lung adenocarcinoma with brain and leptomeningeal
metastasis after response to gefitinib. World J Surg Oncol.
10:2352012. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Luo D, Ye X, Hu Z, Peng K, Song Y, Yin X,
Zhu G, Ji Q and Peng Y: EGFR mutation status and its impact on
survival of Chinese non-small cell lung cancer patients with brain
metastases. Tumour Biol. 35:2437–2444. 2014. View Article : Google Scholar : PubMed/NCBI
|