Introduction
Appendiceal mucocele results from obstruction of the
appendiceal orifice and cystic dilatation of the appendiceal lumen
due to mucinous secretions (1).
Appendiceal mucocele may be inflammatory or have a neoplastic
origin. Primary neoplastic lesions presenting with a mucocele of
the appendix are rare. Mucoceles may occur as a result of a
retention cyst, mucosal hyperplasia, mucinous cystadenoma or
mucinous cystadenocarcinoma. Cystadenoma of the appendix is one of
the most common causes and may be detected in 0.6% of appendectomy
specimens (2). In the majority of the
patients, asymptomatic; pain in the right lower quadrant of the
abdomen may be the only symptom. Preoperative diagnosis is
difficult and patients are often diagnosed incidentally by
abdominal surgery for other causes (3,4).
We herein present a case of a female patient who was
misdiagnosed with retroperitoneal hydatid cyst and underwent
laparoscopic appendectomy with partial resection of the caecum
following laparoscopic exploration.
Case report
A 59-year old female patient was admitted to the Dr
Lütfi Kirdar Kartal Research and Education Hospital (Istanbul,
Turkey) with right upper quadrant abdominal pain for 3 years. The
physical examination and laboratory findings revealed no
abnormalities. Abdominal ultrasonography (US) revealed a
retroperitoneal cystic mass with low-level internal echoes,
suspicious for hydatid disease, in the right upper quadrant. A
computed tomography scan (CT) revealed a retroperitoneal cystic
mass, sized 11×6 cm, with partial calcifications of the wall,
consistent with the characteristics of echinococcal hydatid cyst
(Fig. 1). Serodiagnostic markers were
within the normal range, but the patient resided in a part of
Turkey endemic for echinococcosis.
Laparoscopic cystectomy was planned. Three trocars
were placed in the left lateral decubitus position, as applied
during adrenalectomy procedures. The paracolic peritoneum was
divided and posterior attachments with the kidney and duodenum were
released. With the help of a gauze pad, the cyst was manipulated
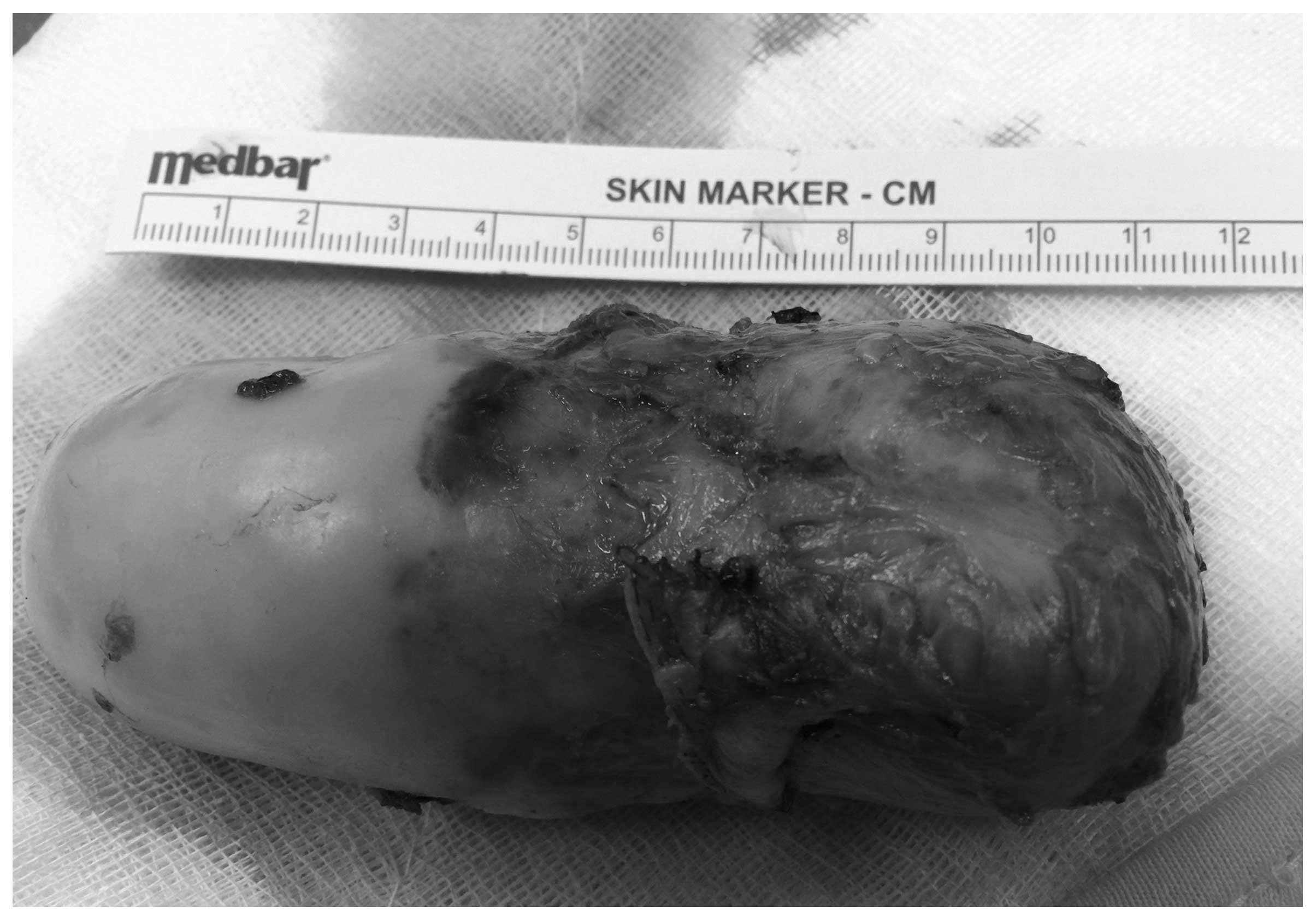
carefully to avoid perforation. Laparoscopic exploration revealed a
giant appendiceal mucocele. The caecum, including the base of the
appendix, was partially resected with an endoscopic stapler and the
specimen was extracted with an endobag (Fig. 2).
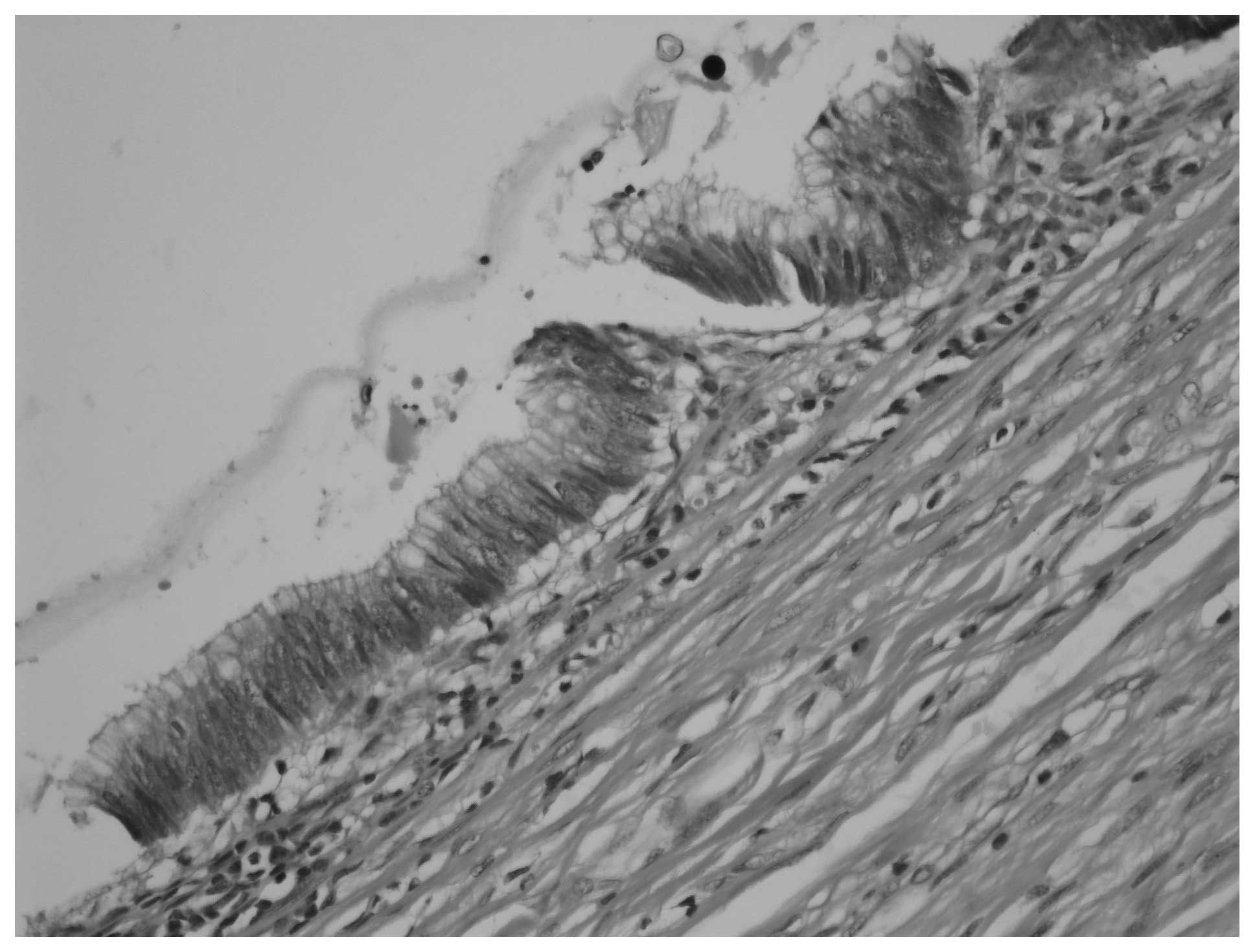
The histopathological examination revealed an
appendix sized 11×6 cm, filled with mucin. The definitive diagnosis
was mucinous cystadenoma of the appendix and the surgical margins
were clear behind the staple line (Fig.
3). The postoperative recovery was uneventful and the patient
was discharged on postoperative day 3. Colonoscopy and US were
performed 3 months after surgery for the possibility of
metachronous cancer and pseudomyxoma peritonei, respectively, with
no pathological findings.
Discussion
The term appendiceal mucocele refers to the cystic
dilatation of the appendiceal lumen caused by mucinous secretions
(1). Appendiceal mucocele may develop
due to mucinous cystadenoma (63%), mucosal hyperplasia (25%),
mucinous cystadenocarcinoma (11%) and retention cyst of the
appendiceal lumen (1%) (3).
Appendiceal mucocele is more frequent in women aged >50 years.
The most common cause of appendiceal mucocele is mucinous
cystadenoma, which is detected in 0.6% of appendectomy specimens
(2). Preoperative diagnosis is
difficult, as ~25–50% of the patients are asymptomatic and
diagnosed incidentally during physical examination or during
abdominal imaging or surgery (4).
Symptomatic patients present with acute or chronic right lower
quadrant pain. Other symptoms, such as nausea, vomiting or weight
loss, may point towards mucinous cystadenocarcinoma or pseudomyxoma
peritonei.
Abdominal US and CT scan may be helpful for
diagnosis. A round, ovoid, sausage-, pear- or chicken
drumstick-shaped cystic mass, with a variable intraluminal
echotexture and low-level internal echoes or septae are diagnostic
findings on US (4,5). CT scan is superior to US for evaluation
of the appendix, as it shows the topographic anatomical
associations between the caecum and the mucocele. In addition, CT
scan is more sensitive in the detection of mural curvilinear
calcifications compared with US.
Hydatid disease is a zoonosis and generally caused
by infection with echinococcus granulosus. The most common
type of disease appearance is cysts, and the liver is the most
common site (6). Although
retroperitoneal hydatid disease is a very rare condition, the
eastern region of Turkey is an endemic area for echinococcosis and
cystectomy is the treatment of choice for preventing spread and
recurrence. The serodiagnosis was negative, but the sensitivity and
specificity of serodiagnostic tests for echinococcosis have been
reported to range between 80 and 90% (7). False-negative results in our daily
practice increased the significance of imaging for diagnosis and
led to a revision of treatment options. Cystectomy or
pericystectomy is our choice of treatment, rather than
puncture-aspiration-irrigation-reaspiration or partial cystectomy,
in cases highly suspicious for hydatid disease but with negative
serodiagnosis. Complex ovarian cyst, urolithiasis or cystic hydatid
disease of the liver have been reported to mimick appendiceal
mucocele based on US or CT findings and non-specific clinical
symptoms (3,4,8). To the
best of our knowledge, there are no reports of mucinous appendiceal
neoplasms presenting as retroperitoneal hydatid cysts.
Spontaneous or intraoperative rupture of the
mucocele and spread of epithelial cells and mucoid fluid throughout
the peritoneal cavity, resulting in pseudomyxoma peritonei, is the
most serious complication of appendiceal mucocele (1). Although some authors do not recommend
laparoscopic treatment for appendiceal mucocele, the laparoscopic
approach is suitable when performed carefully. Every effort is made
to maintain the mucocele intact; direct manipulation of the
mucocele may result in rupture and should be avoided; a gauze pad
must be used to manipulate the appendiceal mucocele (9–11).
Extracting the specimen with an endobag is mandatory.
It is generally accepted that appendectomy is
suitable for unruptured benign mucoceles localized to the appendix
(1,11). There is no consensus on the surgical
treatment for mucoceles involving the base of the appendix or
invaginating into the caecum. Right hemicolectomy, ileocaecal
resection and appendectomy with partial resection of the caecum
have been evaluated as therapeutic modalities (1,4,8,11). The
postoperative period in patients undergoing appendectomy with
partial resection of the caecum is generally uneventful (8,11). Due to
the higher morbidity rate of right hemicolectomy, appendectomy with
partial resection of the caecum is the preferred treatment in
selected cases.
The postoperative follow-up of patients is
important, due to the high incidence of synchronous or metachronous
cancer (20%) (11). Colonoscopy
should be performed after recovery for close follow-ups; it is also
recommended for preoperative diagnosis. In addition, abdominal US
is important for the detection of postoperative pseudomyxoma
peritonei caused by unnoticed contamination.
In conclusion, appendiceal mucocele should be
considered when an atypical cystic mass is identified in the right
upper or lower quadrants of the abdomen by US or CT scan. The
laparoscopic approach is suitable when performed carefully. In
cases highly suspicious for hydatid disease with negative
serodiagnosis, cystectomy is the treatment of choice for the
prevention of spread and recurrence.
Glossary
Abbreviations
Abbreviations:
|
US
|
ultrasonography
|
|
CT
|
computed tomography
|
References
|
1
|
Maa J and Kirkwood KS: The appendix.
Sabiston Textbook of Surgery. Townsend CM, Beauchamp RD, Ever BM
and Mattox KL: Elsevier Saunders. (Philadelphia). 1279–1293. 2012.
View Article : Google Scholar
|
|
2
|
Marudanayagam R, Williams GT and Rees Bl:
Review of the pathological results of 2660 appendicectomy
specimens. J Gastroenterol. 41:745–749. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Demirci RK, Habibi M, Karakaş BR, Buluş H,
Akkoca M and Öner OZ: Appendix mucocele mimicking a complex ovarian
cyst. Ulus Cerrahi Derg. 31:58–60. 2013.PubMed/NCBI
|
|
4
|
Krieg A, Esch JS II, Poll LW, Braunstein S
and Knoefel WT: Mucinous cystadenoma of the appendix misdiagnosed
as cystic hydatid disease of the liver: A case report. J Med Case
Rep. 2:2182008. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Madwed D, Mindelzun R and Jeffrey RB Jr:
Mucocele of the appendix: Imaging findings. AJR AM J Roentgenol.
159:69–72. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Cakir OO, Ataseven H and Demir A: Hydatid
acute pancreatitis. Turkiye Parazitol Derg. 36:251–253. 2012.(In
Turkish). PubMed/NCBI
|
|
7
|
Siracusano A, Buttari B, Delunardo F,
Profumo E, Margutti P, Ortona E, Riganò R and Teggi A: Critical
points in the immunodiagnosis of cystic echinococcosis in humans.
Parassitologia. 46:401–403. 2004.PubMed/NCBI
|
|
8
|
Dandin Ö, Balta AZ, Sücüllü I, Yucel E,
Ozgan ET and Yıldırım Ş: Appendiceal mucocele mimicking
urolithiasis. Ulus Cerrahi Derg. 29:88–91. 2013.PubMed/NCBI
|
|
9
|
Rangarajan M, Palanivelu C, Kavalakat AJ
and Parthasarathi R: Laparoscopic appendectomy for mucocele of the
appendix: Report of 8 cases. Indian J Gastroenterol. 25:256–257.
2006.PubMed/NCBI
|
|
10
|
Navarra G, Asopa V, Basaglia E, Jones M,
Jiao LR and Habib NA: Mucous cystadenoma of the appendix: Is it
safe to remove it by a laparoscopic approach? Surg Endosc.
17:833–834. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Kılıç MÖ, İnan A and Bozer M: Four
mucinous cystadenoma of the appendix treated by different
approaches. Ulus Cerrahi Derg. 30:97–99. 2014.PubMed/NCBI
|