Introduction
Glioblastoma multiforme (GBM) is the most aggressive
and common tumor among primary adult malignant brain tumors,
classified as grade IV by the World Health Organization (WHO). GBM
is associated with poor survival, despite an aggressive treatment
approach including surgery, radiation and chemotherapy (1).
Angiogenesis is required for the growth, invasion
and metastasis of cancer cells (2).
It has been demonstrated that GBMs exhibit intense angiogenesis,
which may be associated with tumor progression and intratumoral
hemorrhage (3–5). Angiogenesis is a complex, multistage
process that leads to the formation of new blood vessels and
depends on the local balance between various molecules that induce
or inhibit neovascularization (6). It
has been demonstrated that vascular endothelial growth factor
(VEGF) plays a pivotal role in the induction of brain tumor
angiogenesis (6). Other growth
factors, including basic fibroblast growth factor (bFGF), are
secreted by the tumor cells, as well as by platelets and,
potentially, vascular mesenchymal cells. These factors bind to
specific receptors and activate endothelial cells. It has been
demonstrated that increased bFGF and VEGF production by cancer
cells is directly correlated with tumor angiogenesis and
progression (7). Cytosolic
thioredoxin (Trx) also participates in important endothelial cell
activities, including migration, proliferation, angiogenesis and
apoptosis. The activity of Trx is regulated by thioredoxin
reductase 1 (TrxR1) (8).
Evaluating the expression of specific angiogenic and
tumorigenic markers is useful for predicting therapeutic responses,
grading and prognosis of malignant gliomas (4). Novel treatment options targeting TrxR1
and certain angiogenic molecules are currently under development,
with promising results (4,9,10).
The aim of this study was to investigate the
association between VEGF, bFGF and TrxR1 expression and
intratumoral hemorrhage in GBMs.
Materials and methods
Patient groups
Surgically resected human GBM samples from 20
patients who underwent surgery at our university (Necmettin Erbakan
University, Meram Faculty of Medicine hospital) between 2006 and
2015, were obtained from pathology archives.
The specimens had been fixed in 4%
phosphate-buffered formaldehyde, processed and embedded in paraffin
blocks. Histopathological examination, typing and grading of the
hematoxylin and eosin-stained slides were performed by an
experienced neuropathologist, according to the WHO criteria
(11).
The samples included 10 GBM samples containing
radiologically and histopathologically confirmed intratumoral
hemorrhage (group 1) and 10 GBM samples without evidence of
intratumoral hemorrhage (group 2).
None of the patients had been administered
radiotherapy, chemotherapy or immunotherapy prior to surgery.
Informed consent for the study was obtained from all
patients or their families. Approval for this study was obtained
from the local Ethics Committee of Necmettin Erbakan University,
Meram Faculty of Medicine.
Immunohistochemistry
Tumor samples previously embedded in paraffin were
sectioned (4 µm) and mounted onto positively charged slides (Slides
Micro Life®; Glaswarenfabrik Karl Hecht GmbH & Co
KG, Sondheim, Germany). Immunocytochemistry was then performed
using an automated avidin-biotin system (Ventana BenchMark XT;
Ventana Medical Systems, Tucson, AZ, USA).
TrxR1 expression was evaluated using a polyclonal
antibody (anti-TXNRD1 rabbit polyclonal antibody; 1:200, cat. no.
bs-8299R; Bioss, Woburn, MA, USA). VEGF expression was evaluated
using a rabbit polyclonal antibody (anti-VEGF; 0.5 mg/ml, cat. no.
GTX59912; Gene Tex, Irvine, CA, USA) and bFGF expression was
evaluated using a rabbit polyclonal antibody (anti-FGF2; 100 µg at
0.5 mg/ml, cat. no. ab126861; Abcam, MA, USA).
The immunointensity of TrxR1 was classified into
four groups as follows: 0, negative; 1+, weak; 2+, moderate; and
3+, strong, as previously reported (12).
VEGF immuno-reactivity was evaluated based on the
proportion of immunopositive cells. Five categories were defined as
follows: 0, all negative; 1+, <25% positive cells; 2+, 25–49%;
3+, 50–74%; and 4+, >75% positive cells. Immunointensity was
also subclassified into four groups as follows: 0, negative; 1+,
weak; 2+, moderate; and 3+, strong (6,13).
bFGF immunoreactivity was evaluated based on the
proportions of immunopositive cells. Four categories were defined
as follows: 0, all negative; 1+, <10% positive cells; 2+,
10–50%; and 3+, >50% positive cells. Immunointensity was also
subclassified into four groups as follows: 0, negative; 1+, weak;
2+, moderate; and 3+, strong (14).
Statistical analysis
Statistical analyses were performed using SPSS for
Windows, version 18.0 (SPSS, Inc., Chicago, IL, USA). Data are
expressed as minimum-maximum value, mean ± standard deviation (SD)
and percentage. Statistical analyses were performed using the
Chi-square test. A P-value of <0.05 was considered to indicate
statistically significant differences.
Results
VEGF, bFGF and TrxR1 expression
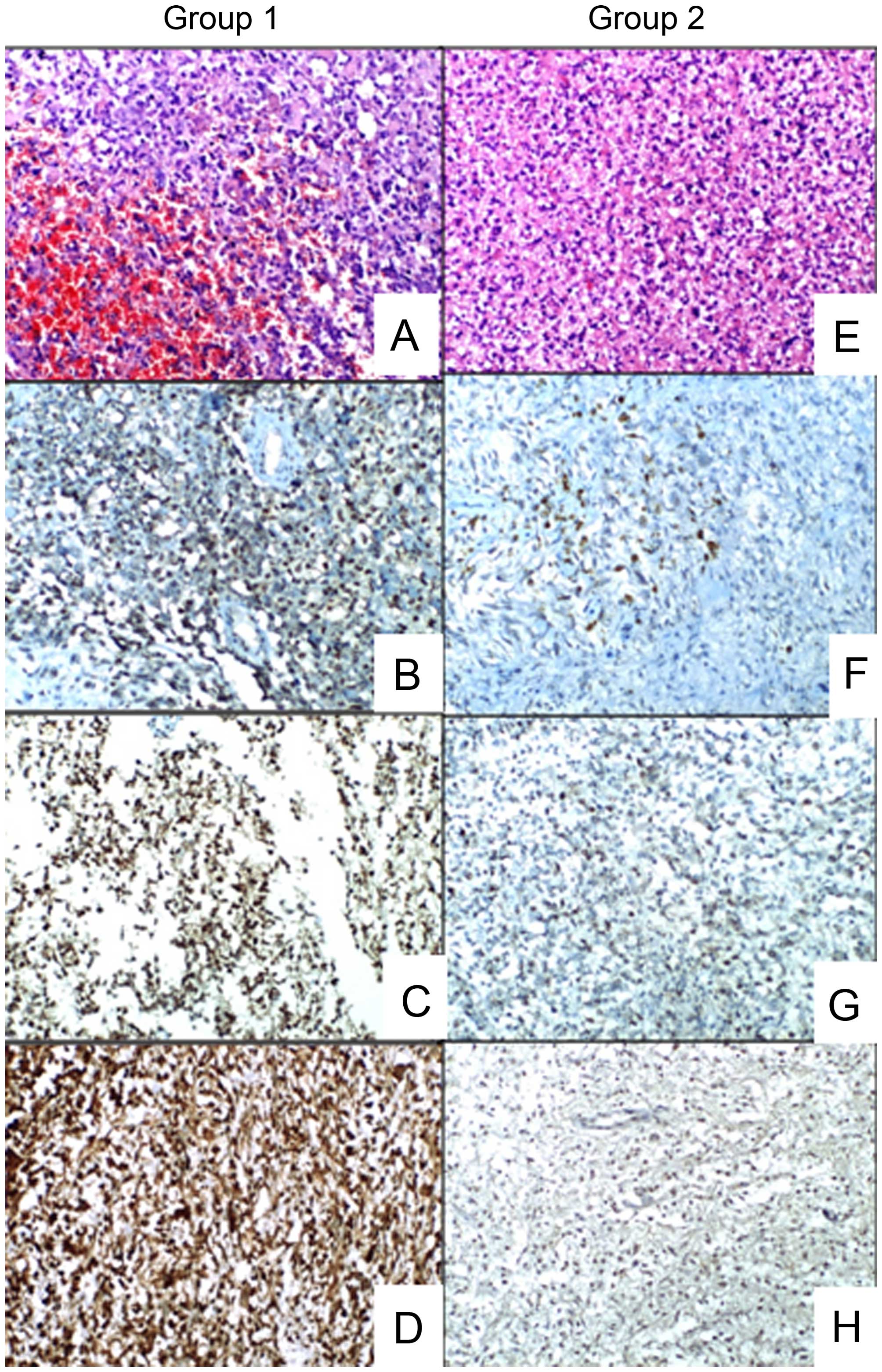
Group 1 GBM tissues exhibited statistically
significantly higher VEGF and bFGF immunoreactivity (P<0.05).
Group 1 GBM tissues exhibited statistically significantly higher
VEGF, bFGF and TrxR1 immunointensity (P<0.05). Group 1 GBM
tissues showed 100%, ≥2+ immunoreactivity for VEGF and bFGF, and
100%, ≥2+ immunointensity for VEGF, bFGF and TrxR1. Group 2 GBM
tissues exhibited 100%, ≤2+ immunoreactivity for VEGF and bFGF, and
100%, ≤2+ immunointensity for VEGF, bFGF and TrxR1.
The minimum-maximum and mean ± SD expression values
are summarized in Table I.
Representative images of the groups are presented in Fig. 1.
 | Table I.VEGF, bFGF and TrxR1 expression in
groups 1 (with intratumoral hemorrhage) and 2 (without intratumoral
hemorrhage). |
Table I.
VEGF, bFGF and TrxR1 expression in
groups 1 (with intratumoral hemorrhage) and 2 (without intratumoral
hemorrhage).
| Groups | VEGF
immunoreactivity | VEGF
immunointensity | bFGF
immunoreactivity | bFGF
immunointensity | TrxR1
immunointensity |
|---|
| 1 (n=10) | 2.60±0.60 | 2.30±0.48 | 2.60±0.51 | 2.70±0.48 | 2.70±0.48 |
|
| (2–4) | (2–3) | (2–3) | (2–3) | (2–3) |
| 2 (n=10) | 1.50±0.52 | 1.20±0.78 | 1.70±0.67 | 1.20±0.63 | 1.40±0.69 |
|
| (1–2) | (0–2) | (1–3) | (0–2) | (0–2) |
Discussion
The angiogenetic process is crucial for GBMs, which
exhibit intense neovascularization (1,15).
Anti-angiogenic targeted therapy is currently being increasingly
investigated fort he management of GBM (1).
It has been demonstrated that VEGF and its receptors
play a major role in the angiogenesis of malignant gliomas
(16). A strong correlation has
previously been identified between malignancy in human astrocytic
tumors and increased expression of certain fibroblast growth
factors, including bFGF (17). The
growth and angiogenesis of astrocytomas are positively regulated by
bFGF and VEGF, which are secreted by the tumor cells, as well as by
platelets and, potentially, by vascular mesenchymal cells (1,7,18). Cytosolic Trx 1 is an isoform of the
endogenous antioxidant Trx system, which exerts significant
modulating effects on cellular redox status. Growing evidence
suggests that Trx 1 participates in angiogenic signaling pathways
by interacting with various transcription factors. The activity of
Trx1 is mainly regulated by TrxR1 (8).
The tumoral neovasculature is characterized by
increased vessel diameter, length, density and permeability
(19). Increased venular and
capillary permeability due to enhanced formation of vascular
endothelial fenestrations may lead to intratumoral hemorrhage in
GBMs (3,15).
Overexpression of VEGF is known to induce
tumor-related cyst formation, peritumoral edema formation and
intratumoral hemorrhage (3). Cheng
et al (15) stereotactically
implanted VEGF-overexpressing glioblastoma cells into mouse brains
and demonstrated the rapidly developing intracerebral hemorrhage
within 60–90 h. Jung et al (20) mentioned the possible role of VEGF
overexpression in metastatic brain tumor-related hemorrhage, by
achieving rapid vessel growth and breakdown around the tumors. Jin
Kim et al (3) indicated the
role of VEGF overexpression in tumor-related hemorrhage of
pituitary adenomas. However, little is known regarding the role of
bFGF and, particularly, TrxR1 in GBMs, although GBMs are associated
with a high incidence of spontaneous intratumoral hemorrhage.
In astrocytic tumors, bFGF expression increases with
increasing malignancy grade (14).
FGF family members, including bFGF, possess mitogenic and
angiogenic properties, which may explain the role of bFGF in the
malignant progression of astrocytic tumors (17). Similarly, the Trx system plays a
critical role in the modulation of angiogenesis (8). Trx 1 and VEGF have been found to be
overexpressed in a variety of cancers, and increased levels of Trx
1 were correlated with poor prognosis (8). However, there is currently no study in
the literature directly demonstrating the expression patterns of
bFGF and TrxR1 in tumor-related hemorrhage of GBMs.
In this study, we observed a significant
overexpression of VEGF, bFGF and TrxR1 in GBMs containing
intratumoral hemorrhage. Our results indicate a role for VEGF, bFGF
and TrxR1 in the promotion of angiogenesis. As mentioned
previously, enhanced angiogenesis may lead to intratumoral
hemorrhage (18) and tumoral growth
(20) by complex mechanisms that have
not yet been fully elucidated. To the best of our knowledge, our
results represent the first evidence on the expression variations
of VEGF, TrxR1 and bFGF in GBMs with or without intratumoral
hemorrhage.
There were certain limitations to this study,
including the relatively small sample size and semiquantitative
assessment method by immunohistochemical staining. Futher research,
using quantitative reverse transcription polymerase chain reaction
with immunostaining, may yield more sensitive results.
References
|
1
|
Zhang M, Ye G, Li J and Wang Y: Recent
advance in molecular angiogenesis in glioblastoma: The challenge
and hope for anti-angiogenic therapy. Brain Tumor Pathol.
32:229–236. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Arnér ES and Holmgren A: The thioredoxin
system in cancer. Semin Cancer Biol. 16:420–426. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
JinKim Y, Hyun Kim C, Hwan Cheong J and
Min Kim J: Relationship between expression of vascular endothelial
growth factor and intratumoral hemorrhage in human pituitary
adenomas. Tumori. 97:639–646. 2011.PubMed/NCBI
|
|
4
|
Gatson NN, Chiocca EA and Kaur B:
Anti-angiogenic gene therapy in the treatment of malignant gliomas.
Neurosci Lett. 527:62–70. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Stiver SI: Angiogenesis and its role in
the behavior of astrocytic brain tumors. Front Biosci. 9:3105–3123.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Hara A and Okayasu I: Cyclooxygenase-2 and
inducible nitric oxide synthase expression in human astrocytic
gliomas: Correlation with angiogenesis and prognostic significance.
Acta Neuropathol. 108:43–48. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Jang FF, Wei W and De WM: Vascular
endothelial growth factor and basic fibroblast growth factor
expression positively correlates with angiogenesis and peritumoural
brain oedema in astrocytoma. J Ayub Med Coll Abbottabad.
20:105–109. 2008.PubMed/NCBI
|
|
8
|
Dunn LL, Buckle AM, Cooke JP and Ng MK:
The emerging role of the thioredoxin system in angiogenesis.
Arterioscler Thromb Vasc Biol. 30:2089–2098. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Yagublu V, Arthur JR, Babayeva SN, Nicol
F, Post S and Keese M: Expression of selenium-containing proteins
in human colon carcinoma tissue. Anticancer Res. 31:2693–2698.
2011.PubMed/NCBI
|
|
10
|
Holash J, Maisonpierre PC, Compton D,
Boland P, Alexander CR, Zagzag D, Yancopoulos GD and Wiegand SJ:
Vessel cooption, regression, and growth in tumors mediated by
angiopoietins and VEGF. Science. 284:1994–1998. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Louis DN, Ohgaki H, Wiestler OD, Cavenee
WK, Burger PC, Jouvet A, Scheithauer BW and Kleihues P: The 2007
WHO classification of tumours of the central nervous system. Acta
Neuropathol. 114:97–109. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Haapasalo H, Kyläniemi M, Paunul N,
Kinnula VL and Soini Y: Expression of antioxidant enzymes in
astrocytic brain tumors. Brain Pathol. 13:155–164. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
ElSayed M and Taha MM: Immunohistochemical
expression of cycloxygenase-2 in astrocytoma: Correlation with
angiogenesis, tumor progression and survival. Turk Neurosurg.
21:27–35. 2011.PubMed/NCBI
|
|
14
|
Torp SH and Alsaker M: Ki-67
immunoreactivity, basic fibroblastic growth factor (bFGF)
expression, and microvessel density as supplementary prognostic
tools in low-grade astrocytomas. An immunohistochemical study with
special reference to the reliability of different Ki-67 anti.
Pathol Res Pract. 198:261–265. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Cheng SY, Nagane M, Huang HS and Cavenee
WK: Intracerebral tumor-associated hemorrhage caused by
overexpression of the vascular endothelial growth factor isoforms
VEGF121 and VEGF165 but not VEGF189. Proc Natl Acad Sci USA.
94:12081–12087. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Plate KH and Risau W: Angiogenesis in
malignant gliomas. Glia. 15:339–347. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Morrison RS, Yamaguchi F, Saya H, Bruner
JM, Yahanda AM, Donehower LA and Berger M: Basic fibroblast growth
factor and fibroblast growth factor receptor I are implicated in
the growth of human astrocytomas. J Neurooncol. 18:207–216. 1994.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Bian XW, Du LL, Shi JQ, Cheng YS and Liu
FX: Correlation of bFGF, FGFR-1 and VEGF expression with
vascularity and malignancy of human astrocytomas. Anal Quant Cytol
Histol. 22:267–274. 2000.PubMed/NCBI
|
|
19
|
Harrigan MR: Angiogenic factors in the
central nervous system. Neurosurgery. 53:639–660; discussion
660-661. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Jung S, Moon KS, Jung TY, Kim IY, Lee YH,
Rhu HH, Sun HS, Jeong YI, Kim KK and Kang SS: Possible
pathophysiological role of vascular endothelial growth factor
(VEGF) and matrix metalloproteinases (MMPs) in metastatic brain
tumor-associated intracerebral hemorrhage. J Neurooncol.
76:257–263. 2006. View Article : Google Scholar : PubMed/NCBI
|