Introduction
Acute myeloid leukemia (AML) is an aggressive
heterogeneous disease that is associated with low survival rates,
and the majority of patients who are diagnosed with this malignancy
will ultimately die without appropriate treatment (1). It is the most common form of leukemia
among adults, and has the lowest rate of survival (2). Furthermore, the incidence of any second
malignancy following AML is 2.43% (3). Second primary breast cancer generally
develops in women who are first diagnosed with endometrial
colon/rectal, stomach, ovarian, thyroid gland or skin cancers,
although its occurrence following AML is rare (4). Additionally, adenosquamous carcinoma of
the breast is a rare tumor that exists as one of the subgroups of
metaplastic breast carcinoma (5).
Metaplastic carcinoma occurs at a prevalence of 1% of all breast
carcinomas (6). In the present
study, a case is reported of adenosquamous carcinoma of the breast
[invasive ductal carcinoma and squamous cell carcinoma (SCC)]
following AML, with metastatic cutaneous lesions of invasive ductal
carcinoma on the thorax and abdomen.
Case study
In May 2010, a 39-year-old Iranian woman was
admitted to the Hematology and Medical Oncology Department of the
Ali-Ebne-Abitaleb Hospital, Zahedan, Iran, due to non-exertional
dyspnea, productive cough and low-grade fever that had lasted over
the course of the previous 10 days. On medical evaluation, other
symptoms were identified as a decrease in appetite and night
sweating. Furthermore, using the routine tests of a peripheral
blood smear and complete blood count for pancytopenia, and the
modified Westergren method for the erythrocyte sedimentation rate
(ESR), pancytopenia and an ESR of 122 mm/h were observed. Two
months prior to admission, the patient had been diagnosed with
areas of microcalcifications in her right breast following
mammography. The patient's laboratory parameters were as follows:
White blood cells, 2.3×103; red blood cells,
2.05×106 cells/ml; and platelet count, 66,000 cells/ml.
Based on the pathological report, the patient was diagnosed with
AML.
On evaluation in the hematology and medical oncology
ward, the patient was diagnosed with AML subtype M4 (acute
myelomonocytic leukemia), and this diagnosis also concurred with
the results of the bone marrow aspiration, blood smear and flow
cytometric analyses. Cytogenetic analysis was not accessible at
that time in our center. The patient's chemotherapy was started
with a 7+3 regimen, with a combination of cytarabine and
daunorubicin. Subsequently, fever and cough had developed, and the
patient coughed up a plug of dense brown mucus. Pathology reports
of the plug of dense mucus revealed septate hyphae with regular
branches of aspergillosis, necrosis and inflammatory cell
infiltration. Furthermore, a follow-up chest computed tomographic
(CT) scan revealed blebs in the right lower and middle lobes of the
lungs, and high-resolution CT (HRCT) revealed collapse and
consolidation in the lateral segment of the right middle lobe, even
though the trachea, bronchus and mediastinum were normal.
Amphotericin B (50 mg) was administered intravenously (i.v.) for 42
days. After a subsequent 10 days, the patient began to take a
regimen and her fever was controlled with imipenem (750 mg) and
vancomycin (500 mg). At this stage, the treatment continued with
itraconazole (600 mg for 3 days). The patient's treatment was
subsequently interrupted for ~2 years, even though she was a
candidate for an allogene bone marrow transplant.
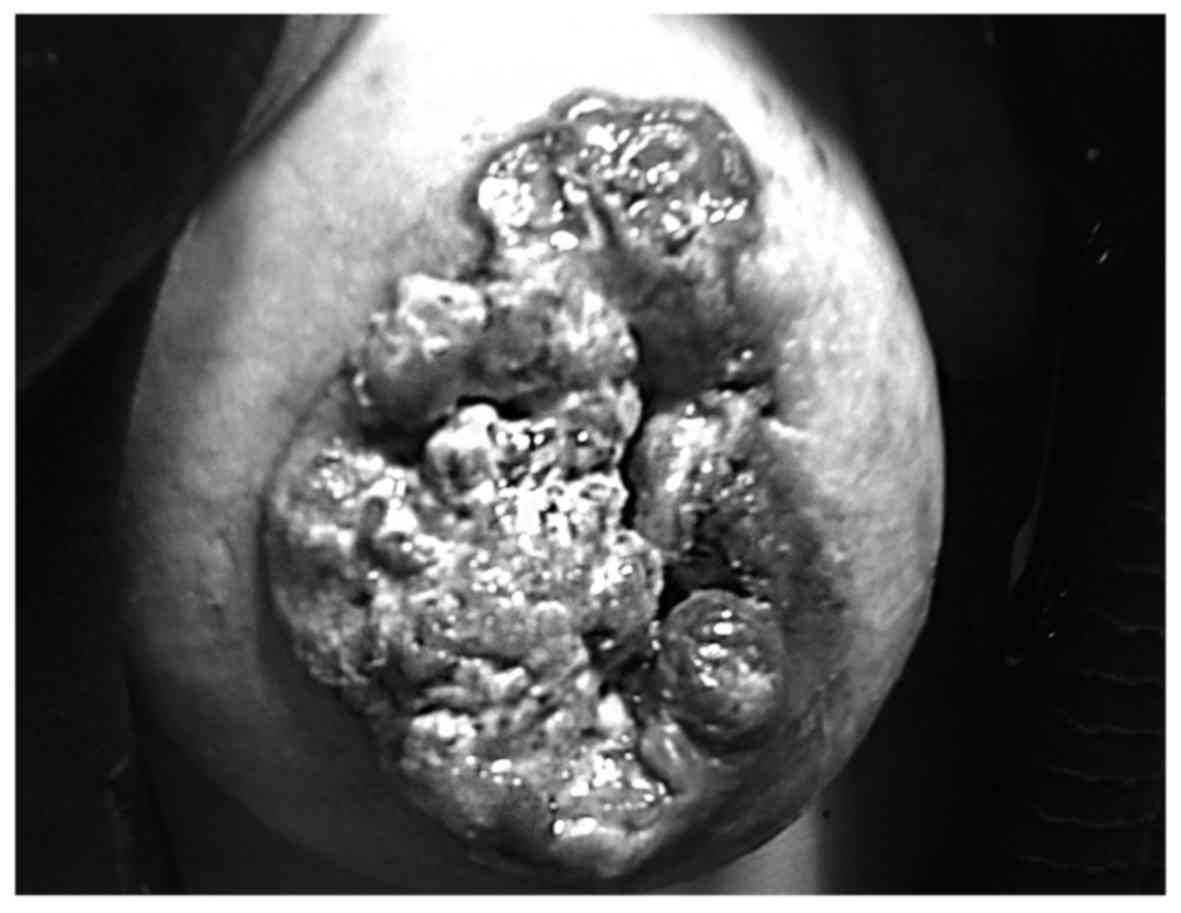
After 2 years, the patient was readmitted to the
hospital due to a mass in the right breast, and concurrent skin
lesions on the breast (Fig. 1).
Following evaluation, the patient was reported to have invasive
ductal carcinoma with squamous cell differentiation (SCC) of the
breast, with metastasis to the right axillary lymph nodes.
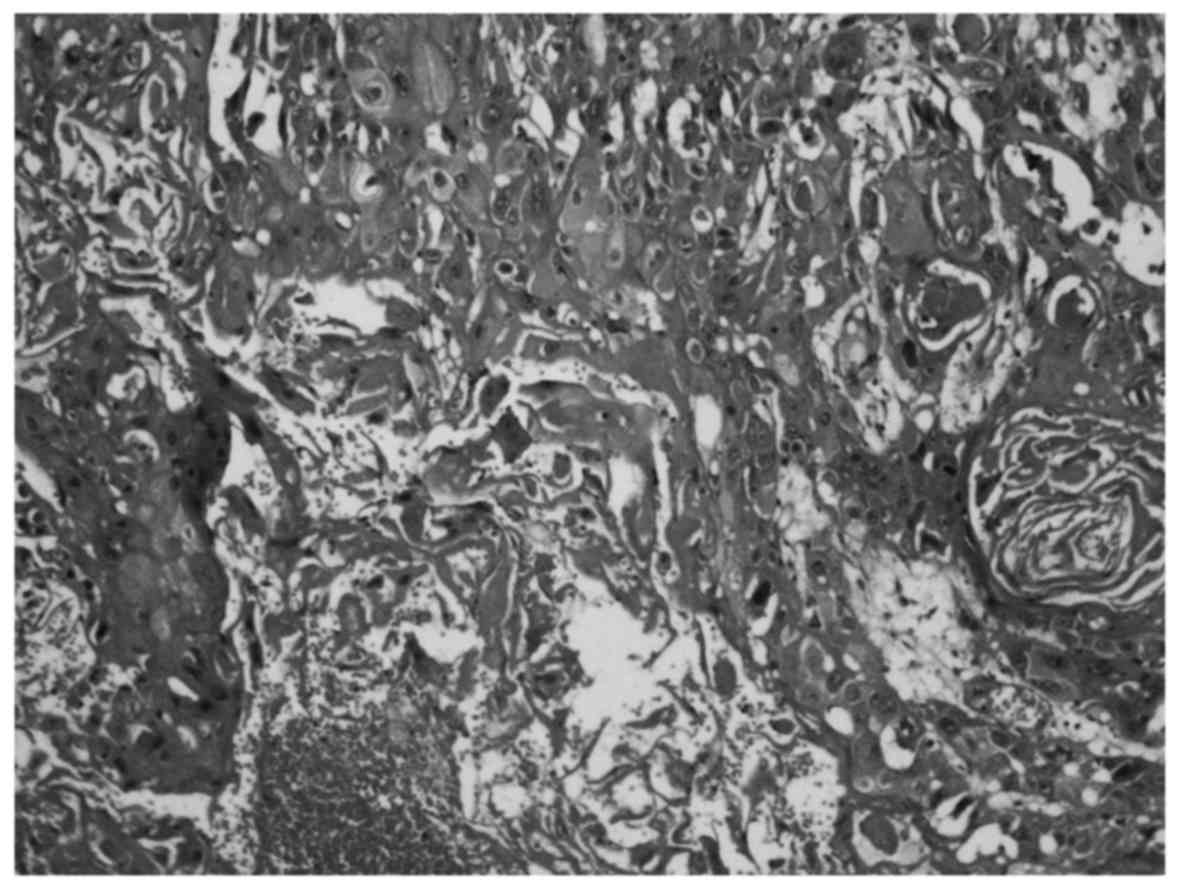
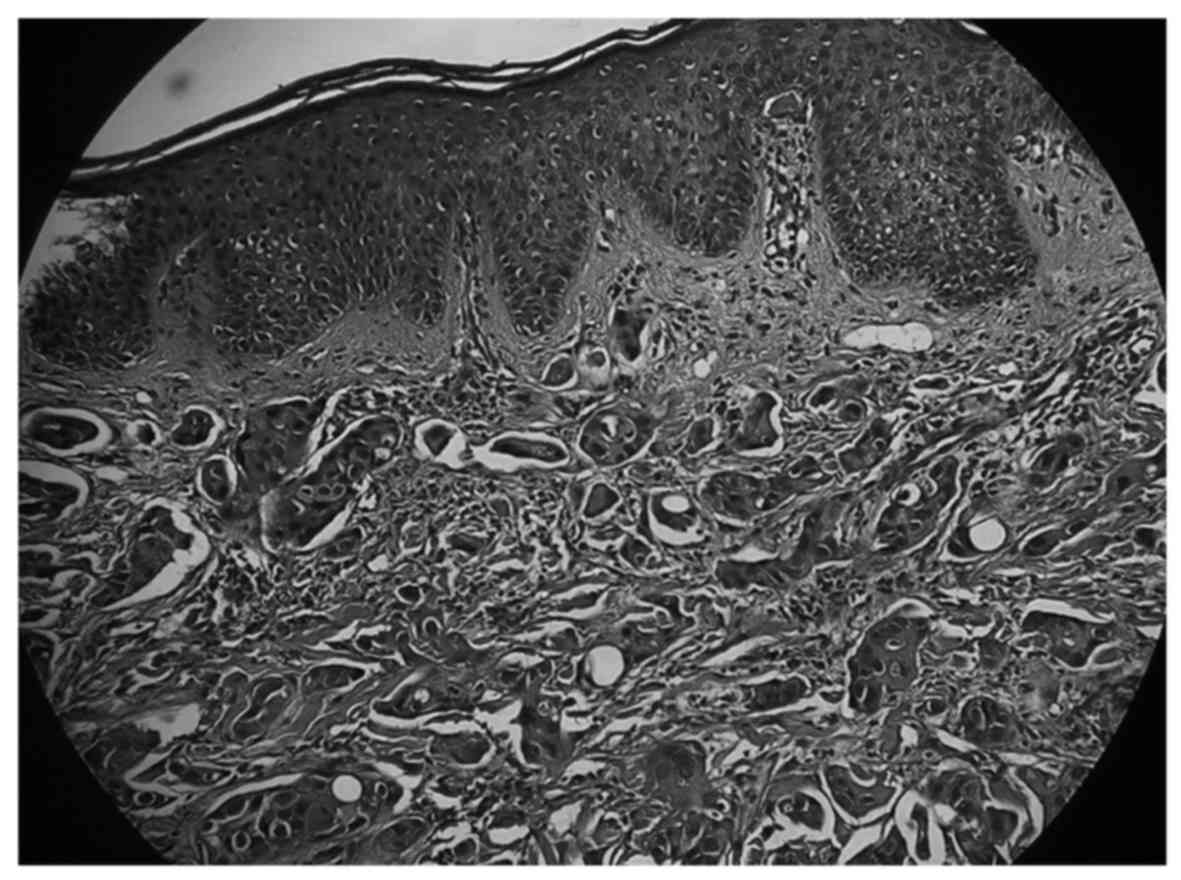
Pathology reported metaplastic carcinoma of the breast
(adenosquamous carcinoma), and a lymph node involvement (Figs. 2 and 3). Testing for the estrogen receptor (ER)
and progesterone receptor (PR) proteins proved to be negative, but
human epidermal growth factor receptor type 2 (HER2) was positive.
p53, ki-67 and cytokeratin 5/6 also tested positive. Following the
diagnosis, the patient underwent a modified radical mastectomy
(MRM). During the first week following MRM, the patient took the
first course of combination chemotherapy, which comprised a
combination of taxotere (160 mg) and carboplatin [6 area under the
curve (AUC); mg/ml/min]/trastuzumab (6 mg/kg) for 6 cycles and,
following involved-field radiation therapy (IFRT), targeted therapy
was allowed to continue.
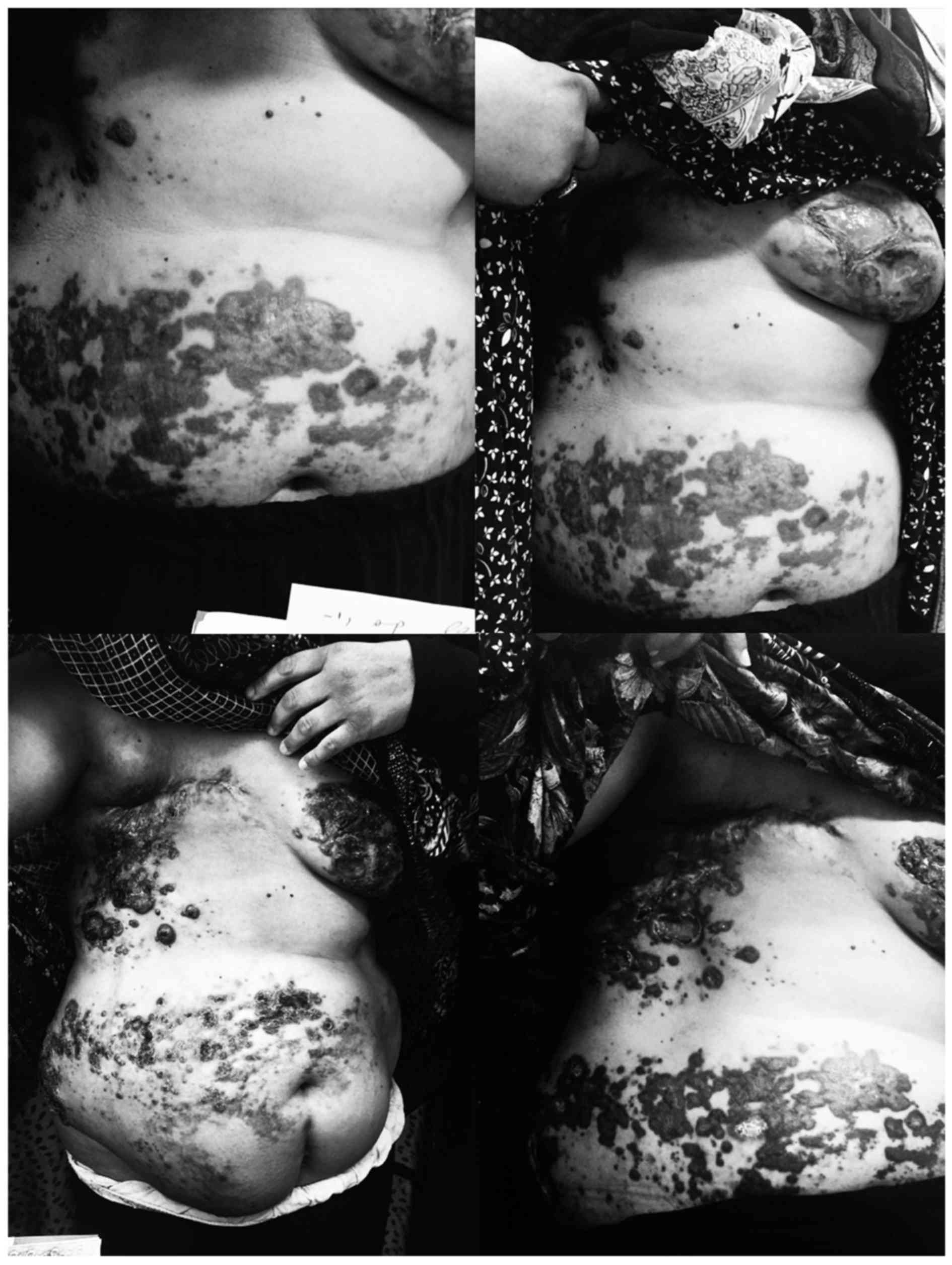
The patient presented with extensive dermatomal skin
lesions at ~9 months following the final cycle of chemotherapy, and
while she was on targeted therapy with trastuzumab, the patient was
followed and her condition was managed as herpes zoster, due to
appearance of lesions that induced it. The patient was a candidate
for a skin biopsy 14 days afterwards due to the progression of the
lesions. During this time, the patient was provided with a regimen
of TAC [taxotere (160 mg), adriamycin (60 mg) and cyclophosphamide
(50 mg)]. The biopsy report revealed metastatic lesions of invasive
ductal carcinoma to the abdomen, left breast and right axillary
region (Fig. 4).
Immunohistochemical (IHC) analysis of the skin
lesions revealed a test result of ER/PR+++; however,
HER2 was negative at this time. During this phase, the patient was
administered liposomal doxorubicin hydrochloride (60 mg) for 3
weeks. After the completion of 3 cycles, the lesions underwent a
marked improvement, and so chemotherapy was continued again for 6
cycles with an identical treatment in all respects, but without
trastuzumab during this course of treatment. However, our patient
succumbed to mortality due to an endemic hemagglutinin type 1 and
neuraminidase type 1 (H1N1) outbreak of influenza, 1 month
following the final cycle of the second course of treatment (a
summary of the clinical course, and all the therapeutic measures
taken, is provided in Table I).
 | Table I.Summary of the clinical course and
therapeutic measures. |
Table I.
Summary of the clinical course and
therapeutic measures.
| Time point | Clinical
event(s) | Therapeutic
measure(s) |
|---|
| Last surveillance
visit | Metastatic lesions of
invasive ductal carcinoma | Liposomal doxorubicin
hydrochloride (60 mg) for 6 cycles |
| Day 1 (onset of
symptoms) | Diagnosis of AML | 7+3 regimen, with the
combination of cytarabine and daunorubicin |
| Second admission | Aspergillus
infection | Amphotericin B (50
mg) and the start of the 5+2 regimen [imipenem (750 mg), vancomycin
(500 mg) and itraconazole (600 mg)] |
| Third admission
(following 2 years' interruption of the treatment) | Mass in the right
breast with concurrent skin lesions on the breast (adenosquamous
carcinoma) | MRM; first course of
chemotherapy [taxotere (160 mg), carboplatin (50 mg) and
trastuzumab (6 mg); IFRT |
| Fourth admission | Progression of
symptoms | Trastuzumab (6
mg) |
| Fifth admission (9
months following the | Extensive dermatomal
skin lesions | TAC regimen [taxotere
(160 mg), adriamycin (60 mg) and cyclophosphamide (50 mg)] final
cycle of chemotherapy) |
| Sixth admission (14
days later) | Progression of
lesions (diagnosis of metastatic lesions | Liposomal doxorubicin
hydrochloride (60 mg) for 6 cycles of invasive ductal
carcinoma) |
Discussion
Adenosquamous carcinoma of the breast is a rare
cancer that occurs as one of the variants of metaplastic breast
carcinoma (5). Adenosquamous
carcinoma has a prevalence of <1% of all breast cancers
(7). It develops as glands and
tubules admixed with solid nests of squamous cells in a spindle
cell background (8). Second primary
breast cancer generally develops in women who are first diagnosed
with endometrial, colon/rectal, stomach, ovarian, thyroid gland or
skin cancers (4), although its
development following AML is rare and, to our best of knowledge, no
report of breast cancer following AML has been previously
published. However, several cases of second primary AML following
breast cancer have been noted in the literature (9–12).
In the present study, our 45-year-old patient had
AML. Treatment options included a 7+3 regimen with a combination of
cytarabine and daunorubicin, although the patient's treatment was
interrupted for ~2 years. Unusually, our patient survived for ~2
years with only one cycle of induction and without taking any
medication, whereas others have reported a long-term survival rate
for AML of <10% (13). Such a
survival rate for AML subtype M4 is very unusual, based on the
above-mentioned medications and complicated sequels. Several
hematological malignancies, including AML, can be effectively
treated using allogeneic hematopoietic stem cell transplantation
(HSCT) (14). The patient was
recommended to have HSCT due to a delay in remission and the M4
subtype of AML, although she refused to continue with the treatment
process. Immunocompromised patients, including those who have AML,
are at risk from fungal infections, and, although several
treatments for fungal infection have been identified, 12–18% of AML
patients still die from fungal infections (15,16).
Invasive aspergillosis is the most common fungal infection that can
threaten the lives of patients with AML (17). Common antifungal drugs that are used
for these patients include amphotericin B, itraconazole,
voriconazole, posaconazole and isavuconazole (18). The patient in the present case study
was treated with amphotericin B (administered i.v. for 42 days),
and subsequently itraconazole (600 mg for 3 days).
The most interesting aspect of the present case
report was the feature of primary adenosquamous carcinoma of breast
invasive ductal carcinoma and SCC following AML. Adenosquamous
carcinoma is one of the types of metaplastic carcinoma that are
characterized by the presence of non-epithelial cellular elements
(4). Following diagnosis, and due to
right axillary lymph nodes metastases, treatment options included
MRM and combination chemotherapy [a combination of taxotere (160
mg) and carboplatin (6 AUC; mg/ml/min)/trastuzumab (6 mg/kg)] for 6
cycles], followed by IFRT, and again, a continuation of the
targeted therapy with trastuzumab. According to previous studies,
mastectomy is an effective treatment for breast cancer, and it has
been demonstrated that a bilateral risk-reducing mastectomy
decreases the risk of invasion and metastases in patients with
breast cancer by up to 90% (19,20).
Based on a review of the literature, almost 20% of all breast
cancers are HER2-positive, and one of the monoclonal antibodies
against the HER2 receptor is trastuzumab, which has been used for
HER2-positive breast cancers as an adjuvant treatment and target
therapy (21,22). SCC may present with smooth or
hyperkeratotic lesions, abscesses, nodules and ulceration of the
skin, although nipple discharge is uncommon (23,24), and
the symptoms of invasive ductal carcinoma are lumps, itching,
burning and pain (25). In the
present study, the patient presented with ulceration lesions on the
breast with lumps. Breast carcinoma is the most common cancer that
causes skin metastases. This metastasis may be presented with
nodules on the thoracic wall and abdomen, limbs, head and neck,
with ulceration, bleeding and pain (26,27). The
patient's specific metastatic invasive ductal carcinoma lesions
were observed as ulcerated plaques and nodules.
The patient, who was diagnosed with AML subtype M4,
and subsequently with breast cancer (adenosquamous carcinoma) with
metastatic lesions of invasive ductal carcinoma, was an unusual
case, exhibiting certain differences with respect to other cases
that have been described in several other case reports. Our patient
had AML, but her treatment was interrupted for ~2 years.
Unexpectedly, the patient was able to survive for ~2 years with
only one cycle of induction, and without taking any medication.
Additionally, the most interesting characteristic of the present
case was the features of primary adenosquamous carcinoma of breast.
In several other cases, certain differences have been demonstrated.
According to the study of Geyer et al (28), who discussed five case studies of
adenosquamous carcinoma, all the patients were at an age of 54–76
with negative axillary lymph nodes, whereas our patient was 41
years old with positive axillary nodes (28). In addition, in the study of Swathy
et al (8), the lesions were
identified as being cystic, whereas our patient presented with
ulceration lesions on the breast with lumps.
Glossary
Abbreviations
Abbreviations:
|
AML
|
acute myeloid leukemia
|
|
AUC
|
area under the curve
|
|
MRM
|
modified radical mastectomy
|
|
IFRT
|
involved-field radiation therapy
|
|
HRCT
|
high-resolution computed
tomography
|
|
ER
|
estrogen receptor
|
|
PR
|
progesterone receptor
|
|
HER2
|
human epidermal growth factor receptor
type 2
|
|
HSCT
|
hematopoietic stem cell
transplantation
|
References
|
1
|
Juliusson G, Karlsson K, Lazarevic VL,
Wahlin A, Brune M, Antunovic P, Derolf A, Hägglund H, Karbach H,
Lehmann S, et al: Swedish Acute Leukemia Registry Group, the
Swedish Acute Myeloid Leukemia Group, the Swedish Adult Acute
Lymphoblastic Leukemia Group: Hematopoietic stem cell
transplantation rates and long-term survival in acute myeloid and
lymphoblastic leukemia: Real-world population-based data from the
Swedish Acute Leukemia Registry 1997–2006. Cancer. 117:4238–4246.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Robak T and Wierzbowska A: Current and
emerging therapies for acute myeloid leukemia. Clin Ther.
31:2349–2370. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Ghimire KB and Shah BK: Second primary
malignancies in adult acute myeloid leukemia-A US population-based
study. Anticancer Res. 34:3855–3859. 2014.PubMed/NCBI
|
|
4
|
Molina-Montes E, Pollán M, Payer T, Molina
E, Dávila-Arias C and Sánchez MJ: Risk of second primary cancer
among women with breast cancer: A population-based study in Granada
(Spain). Gynecol Oncol. 130:340–345. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Agrawal A, Saha S, Ellis IO and Bello AM:
Adenosquamous carcinoma of breast in a 19 years old woman: A case
report. World J Surg Oncol. 8:442010. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Esbah O, Turkoz FP, Turker I, Durnali A,
Ekinci AS, Bal O, Sonmez OU, Budakoglu B, Arslan UY and Oksuzoglu
B: Metaplastic breast carcinoma: Case series and review of the
literature. Asian Pac J Cancer Prev. 13:4645–4649. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Senger JL, Meiers P and Kanthan R:
Bilateral synchronous low-grade adenosquamous carcinoma of the
breast: A Case report with review of the current literature. Int J
Surg Case Rep. 14:53–57. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Swathy PU, Arunalatha P,
Chandramouleeswari K, Lily SM and Ramya S: Adenosquamous variant of
metaplastic carcinoma of breast - an unusual histological variant.
J Clin Diagn Res. 9:ED05–ED06. 2015.PubMed/NCBI
|
|
9
|
Renella R, Verkooijen HM, Fioretta G,
Vlastos G, Kurtz J, Sappino AP, Schäfer P, Neyroud-Caspar I and
Bouchardy C: Increased risk of acute myeloid leukaemia after
treatment for breast cancer. Breast. 15:614–619. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Payandeh M, Khodarahmi R, Sadeghi M and
Sadeghi E: Appearance of Acute Myelogenous Leukemia (AML) in a
Patient with Breast Cancer after Adjuvant Chemotherapy: Case Report
and Review of the Literature. Iran J Cancer Prev. 8:125–128.
2015.PubMed/NCBI
|
|
11
|
Noronha V, Berliner N, Ballen KK, Lacy J,
Kracher J, Baehring J and Henson JW: Treatment-related
myelodysplasia/AML in a patient with a history of breast cancer and
an oligodendroglioma treated with temozolomide: Case study and
review of the literature. Neuro-oncol. 8:280–283. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Aidan JC, Priddee NR and McAleer JJ:
Chemotherapy causes cancer! A case report of therapy related acute
myeloid leukaemia in early stage breast cancer. Ulster Med J.
82:97–99. 2013.PubMed/NCBI
|
|
13
|
Yanada M and Naoe T: Acute myeloid
leukemia in older adults. Int J Hematol. 96:186–193. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Berro M, Basquiera AL, Rivas MM,
Foncuberta MC, Burgos R, Jaimovich G, Milovic V, Martínez Rolón J,
Remaggi G, Alberbide J, et al: Allogeneic hematopoietic stem cell
transplantation in the elderly. Predicting the risk for non relapse
mortality. Medicina (B Aires). 75:201–206. 2015.PubMed/NCBI
|
|
15
|
Ducassou S, Rivaud D, Auvrignon A, Vérité
C, Bertrand Y, Gandemer V and Leverger G: Invasive Fungal
Infections in Pediatric Acute Myelogenous Leukemia. Pediatr Infect
Dis J. 34:1262–1264. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Domenech C, Leick-Courtois C, Bienvenu AL,
Pracros JP, Picot S, Bleyzac N and Bertrand Y: Improvement in the
Outcome of Invasive Aspergillosis in a Pediatric Hematology
Department: A 10-Year Review. J Pediatr Hematol Oncol. 37:560–565.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Gheith S, Ranque S, Bannour W, Ben Youssef
Y, Khelif A, Ben Said M, Njah M and Saghrouni F: Hospital
environment fungal contamination and aspergillosis risk in acute
leukaemia patients in Sousse (Tunisia). Mycoses. 58:337–342. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Karthaus M and Buchheidt D: Invasive
aspergillosis: New insights into disease, diagnostic and treatment.
Curr Pharm Des. 19:3569–3594. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Morrow M, Winograd JM, Freer PE and
Eichhorn JHA: Case records of the Massachusetts General Hospital.
Case 8-2013. A 48-year-old woman with carcinoma in situ of the
breast. N Engl J Med. 368:1046–1053. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Sismondi P, D'Alonzo M, Pecchio S, Bounous
VE, Robba E and Biglia N: Chemoprevention or mastectomy for women
at high risk of developing breast cancer. Maturitas. 82:271–273.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Gallagher CM, More K, Masaquel A, Kamath
T, Guerin A, Ittu R Ionescu, Nitulescu R, Loiselle M Gauthier,
Sicignano N, Butts E, et al: Survival in patients with non
metastatic breast cancer treated with adjuvant trastuzumab in
clinical practice. Springerplus. 5:3952016. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Parhi P and Sahoo SK: Trastuzumab guided
nanotheranostics: A lipid based multifunctional nanoformulation for
targeted drug delivery and imaging in breast cancer therapy. J
Colloid Interface Sci. 451:198–211. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Gupta C, Malani AK, Weigand RT and
Rangineni G: Pure primary squamous cell carcinoma of the breast: A
rare presentation and clinicopathologic comparison with usual
ductal carcinoma of the breast. Pathol Res Pract. 202:465–469.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Lansbury L, Hextall F Bath, Perkins W,
Stanton W and Leonardi Bee J: Interventions for non metastatic
squamous cell carcinoma of the skin: systematic review and pooled
analysis of observational studies. BMJ. 347:f61532013. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Dye TD, Bogale S, Hobden C, Tilahun Y,
Deressa T and Reeler A: Experience of initial symptoms of breast
cancer and triggers for action in ethiopia. Int J Breast Cancer.
2012:9085472012. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Bittencourt MdJS, Carvalho AH, Nascimento
BAMd, Freitas LKM and Parijós AMd: Cutaneous metastasis of a breast
cancer diagnosed 13 years before. An Bras Dermatol. 90:134–147.
2015. View Article : Google Scholar
|
|
27
|
Cabula C, Campana LG, Grilz G, Galuppo S,
Bussone R, De Meo L, Bonadies A, Curatolo P, De Laurentiis M, Renne
M, et al: Electrochemotherapy in the Treatment of Cutaneous
Metastases from Breast Cancer: A Multicenter Cohort Analysis. Ann
Surg Oncol. 22:(Suppl 3). S442–S450. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Geyer FC, Lambros MB, Natrajan R, Mehta R,
Mackay A, Savage K, Parry S, Ashworth A, Badve S and Reis-Filho JS:
Genomic and immunohistochemical analysis of adenosquamous carcinoma
of the breast. Mod Pathol. 23:951–960. 2010. View Article : Google Scholar : PubMed/NCBI
|