Introduction
The advancement of surgical instruments and
equipment over the last 5 years has expanded and confirmed the
advantages of minimally invasive surgery in the treatment of
numerous gynecological diseases, particularly in cases of
gynecological malignancies. Numerous studies have confirmed that
laparoscopic techniques associated with various gynecological
oncological conditions yield improved results compared with
surgical and oncological outcomes of the abdominal staging, with
the advantages of shorter hospital stays, fewer postoperative
adhesions and an improved quality of life (1–3).
Since laparoscopic extraperitoneal para-aortic
lymphadenectomy was described by Vasilev and McGonigle in 1996
(1), it has been accepted in the
literature that laparoscopic extraperitoneal para-aortic
lymphadenectomy may be performed in patients. This approach
theoretically combines the benefits of laparoscopy with the
extraperitoneal approach. It leads to a decrease in the risk of
direct bowel injury, adhesion formation, and wound complications,
and possibly decreases the length of hospital stay and treatment
delay (2).
However, in the majority of cases of laparoscopic
para-aortic lymphadenectomy, total laparoscopic pelvic
lymphadenectomy and hysterectomy with bilateral
salpingo-oophoerctomy (TLH&BSO) will be performed on the
patients, and occasionally even radical hysterectomy, which are all
transperitoneal operations. Furthermore, the conventional incision
positions are neither suitable nor easy for surgeons to reach.
In the present study, a novel technique has been
introduced and described, which is termed ‘laparoscopic local
extraperitoneal para-aortic lymphadenectomy’, and its feasibility
and safety were evaluated.
Materials and methods
The present retrospective case study included a
series of 21 patients, who underwent laparoscopic local
extraperitoneal para-aortic lymphadenectomy for gynecological
malignancies between March and August 2014 in the Obstetrics and
Gynecology Hospital of Fudan University, Shanghai, China.
Diagnoses for the patients included ovarian cancer,
endometrial carcinoma with high-risk factors (i.e., myometrial
invasion >50%, large tumor diameter, and grade 3 or
non-endometrioid pathology) and cervical cancer with common iliac
nodal involvement. All the surgical procedures were performed by
the same operational team. Patients' data were collected
retrospectively, and the characteristics included patient age, body
mass index (BMI), tumor stage and grade, blood loss, operative time
(laparoscopic local extraperitoneal para-aortic lymphadenectomy),
length of hospital stay, intraoperative and postoperative
complications, pathology, lymph node count and lymph node
status.
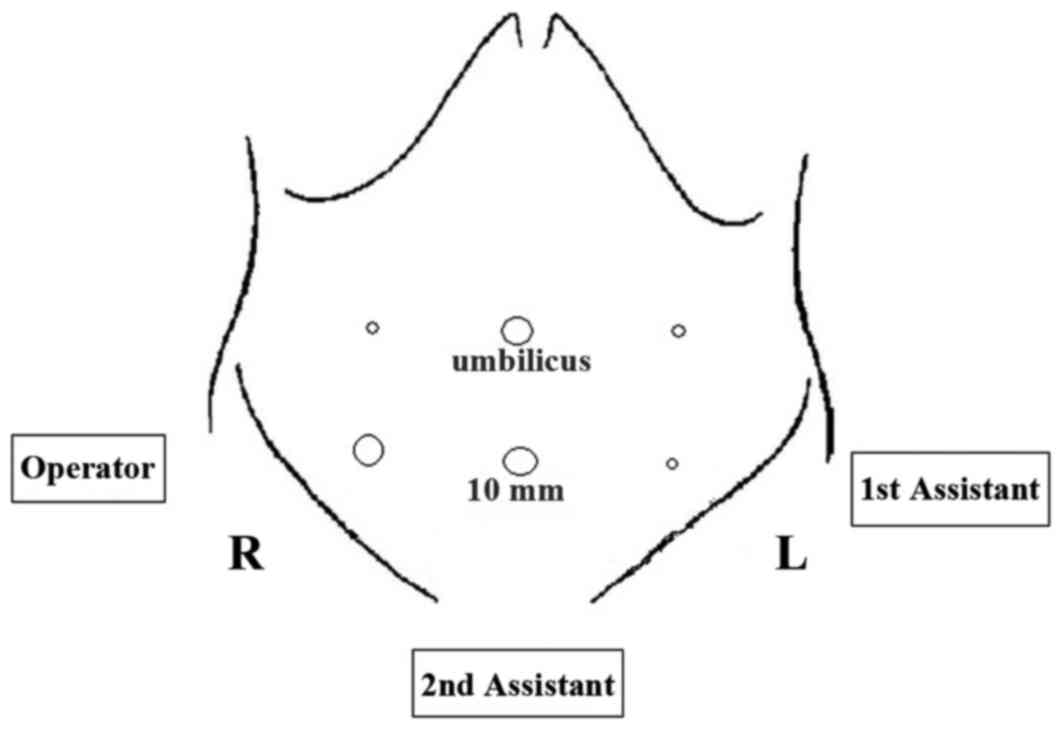
Once the patient had been anesthetized, she was
placed in the Trendelenburg and lithotomy position. The operator
was positioned to the left of the patient, while the first
assistant stood on the right of the patient. A 10-mm trocar was
sub-umbilically inserted for the introduction of the camera and
intraperitoneal inspection. A carbon dioxide pneumoperitoneum was
subsequently generated, keeping the intra-abdominal pressure <14
mmHg. A 30-degree laparoscope was the introduced, and the
peritoneal cavity was inspected. Associated with the inspection,
ancillary trocars were placed within the patient in the supine
position, as follows: i) A 10-mm trocar at the McBurney's point;
ii) a 5-mm trocar at the right lateral of the umbilicus, 4 cm in
distance; and iii) two further 5-mm trocars at the left side of the
patient, opposite to the right two trocars (Fig. 1). These procedures conformed with
those of TLH&BSO, also even including radical hysterectomy,
starting with conventional transperitoneal laparoscopy, as has been
widely reported.
Subsequently, an additional 10-mm trocar was placed
4 cm above the pubic symphysis, and the laparoscope was inserted in
this suprapubic port (Fig. 2). The
operator and first assistant changed their positions, turning
around and facing the TV monitor, which was moved to the head of
the patient. The present authors consider that this position makes
the following operation easier compared with the conventional
position.
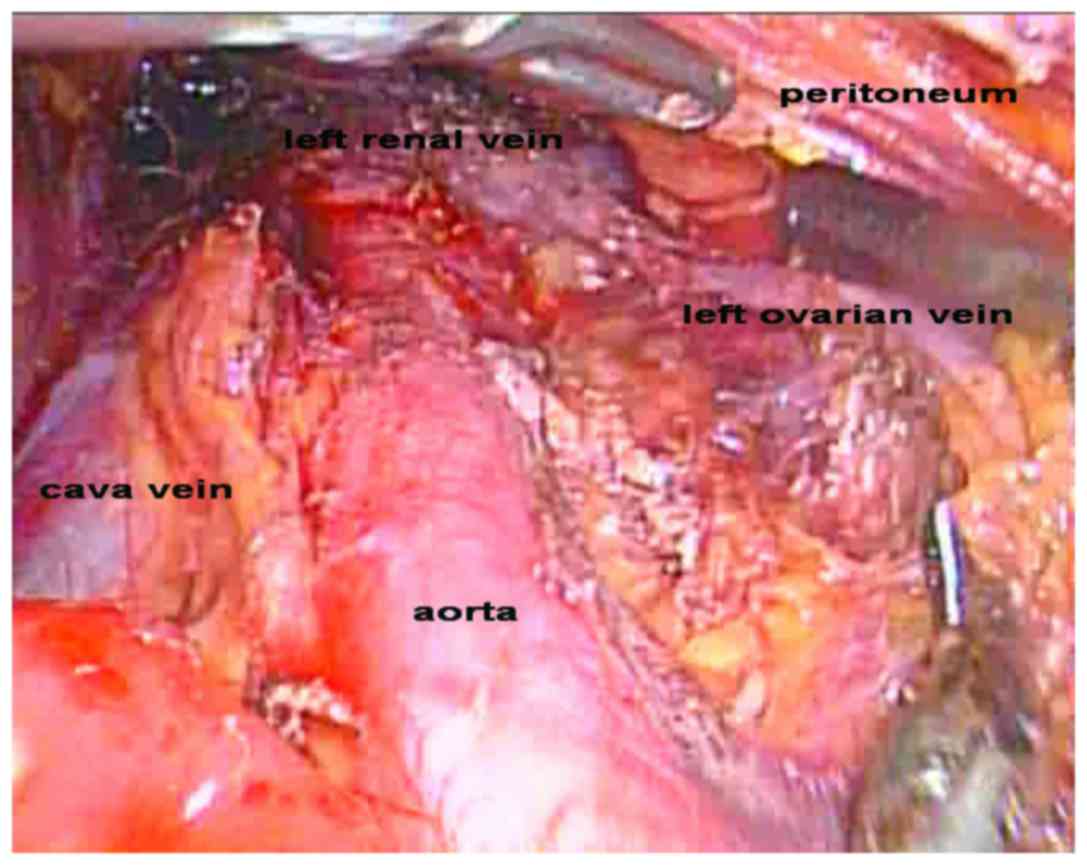
The local peritoneum on top of the lower aorta was
incised using a Harmonic scalpel (Ethicon Endosurgery, Inc.;
Johnson & Johnson, Cincinatti, OH, USA), the peritoneum was
raised with atraumatic graspers, and the laparoscope was then
inserted beneath the peritoneum. Subsequently, the exposure of
aorta was optimized up to the left renal vein (Fig. 3). In this procedure, the duodenum and
the small intestine in the peritoneal cavity were kept isolated
from the operation area by this local extraperitoneal approach. The
nodal tissue was subsequently gently dissected.
With the identification of the inferior mesenteric
artery and the left ureter, the left para-aortic lymphadenectomy
included inframesenteric lymphadenectomy (the aorta up to the level
of the inferior mesenteric artery) and infrarenal lymphadenectomy
(the aorta up to the level of the left renal vein). The right
para-aortic lymphadenectomy included the lymph nodes around the
vena cava up to the right ovarian vein.
Since the greater omentum is located at the upper
abdomen, the improved position also facilitated the operation in
cases with omentectomy.
Results
A total of 21 patients underwent laparoscopic local
extraperitoneal para-aortic lymphadenectomy, including 14 with
endometrioid endometrial cancer, two with cervical cancer and five
with ovarian cancer. The median patient age was 52 years (range,
45–71 years). The median body mass index was 24.8 kg/m2
(range, 22.2–32.4 kg/m2) (Table I). All patients tolerated the
procedure and positioning well.
 | Table I.Patient characteristics. |
Table I.
Patient characteristics.
| Characteristic (total
no. of patients, n=21) | n |
|---|
| Endometrial
cancer | 14 |
| FIGO
stage |
|
|
Ib | 10 |
|
IIa | 4 |
|
Grade |
|
|
2 | 11 |
|
3 | 3 |
| Cervical cancer | 2 |
| FIGO
stage |
|
|
Ib2 | 1 |
|
IIa1 | 1 |
| Ovarian cancer | 5 |
| FIGO
stage |
|
|
IIb | 1 |
|
IIIa | 2 |
|
IIIb | 2 |
| Age (years), median
(range) | 52 (45–71) |
| BMI
(kg/m2), median (range) | 24.8 (22.2–32.4) |
All patients with endometrial cancer were surgically
treated using TLH&BSO. The patients with cervical cancer were
managed by radical hysterectomy, with or without BSO. The three
cases of ovarian cancer underwent cytoreductive surgery. All
patients underwent pelvic lymphadenectomy. The median operating
time of para-aortic lymphadenectomy was 70 min (range, 58–95 min).
The median estimated blood loss of the total surgery was 200 ml
(range, 100–600 ml). No patient required a blood transfusion during
the operation. The median length of hospital stay was 7 days
(range, 5–9 days). There were no conversions or intraoperative
complications in any of the patients. The median number of
para-aortic lymph nodes was 12 (range, 7–17), and the mean number
of pelvic lymph nodes was 22 (range, 20–25). Positive aortic nodes
metastasis was detected in one patient with ovarian cancer.
Postoperative complications included one patient
with chylous ascites, who responded to conservative management with
intravenous somatostatin.
Discussion
The present study demonstrated the effectiveness and
the safety of laparoscopic local extraperitoneal para-aortic
lymphadenectomy in patients with gynecological cancer.
There are two advantages associated with this novel
procedure compared with the methods previously reported. The first
advantage was the positional change of the laparoscope to the
suprapubic port, and the operator and first assistant turning
around to face the TV located at the head of the patient, which
facilitates the performance of this operation compared with the
conventional position. The para-aortic lymph nodes were located at
the upper abdomen, and laparoscopic inframesenteric lymphadenectomy
(the aorta up to the level of inferior mesenteric artery) was
commonly performed with the conventional position and umbilicus
trocar for the laparoscope. However, infrarenal lymphadenectomy
(the aorta up to the level of left renal vein) was more difficult,
as the lymph nodes are located immediately under the umbilicus, and
the operation of the laparoscopic clamp was aligned vertically to
the abdominal wall. It is well established that, the smaller the
angle between the laparoscopic clamp and abdominal wall, the more
difficult will be the operation. Since the greater omentum is
located at the upper abdomen, the improved position also
facilitated the operation in cases involving an omentectomy.
The second advantage was that the novel procedure
reported in the present study is different from total
extraperitoneal para-aortic lymphadenectomy. Since para-aortic
lymphadenectomy usually follows the transperitoneal pelvic
lymphadenectomy, total extraperitoneal para-aortic lymphadenectomy
does not appear to have specific superiority, and the
extraperitoneal laparoscopic approach should be considered for
endometrial cancer staging in patients with a BMI ≥35
kg/m2 (3). Laparoscopic
local extraperitoneal para-aortic lymphadenectomy, particularly
infrarenal lymphadenectomy, may facilitate the operation and avoid
injury to the duodenum.
The median number of harvested para-aortic lymph
nodes in the present study was 12 (range, 7–17). The lymph node
numbers obtained in this study are similar to those in previously
published reports. For example, Escobar et al (4) reported para-aortic lymph node sampling
lymphadenectomy performed through a single 2–3 cm umbilical
incision using a single-port device, and the lymph nodes count was
6 (range, 2–14). A similar median number of para-aortic nodes (14;
range, 12–24) was revealed by Kavallaris et al (5) by means of a standardized technique of
laparoscopic para-aortic lymphadenectomy in gynecological
cancer.
A previous study demonstrated that single-port
laparoscopic para-aortic lymphadenectomy was associated with only a
relatively postoperative hidden umbilical scar, and resulted in
shorter hospital stays, an improved quality of life and surgical
and oncological outcomes that were comparable with those of
abdominal staging (6). However, the
major disadvantage of single-port surgery is the collision of
instruments, and the requirement for specialized instruments, such
as the single-port device.
The present study did have a number of limitations,
due to its retrospective nature, the small number of patients
involved, and lack of randomization. In conclusion, this case
report has demonstrated the feasibility of performing a
laparoscopic local extraperitoneal para-aortic lymphadenectomy in
gynecological cancers. Studies involving a bigger sample size are
necessary, and are eagerly awaited, to help to determine the
long-term risks and benefits.
Acknowledgements
The present study was supported by the Science and
Technology Committee of Shanghai (grant no. 20144Y0096).
References
|
1
|
Vasilev SA and McGonigle KF:
Extraperitoneal laparoscopic para-aortic lymph node dissection.
Gynecol Oncol. 61:315–320. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Iacoponi S, De Santiago J, Diestro MD,
Hernandez A and Zapardiel I: Single-port laparoscopic
extraperitoneal para-aortic lymphadenectomy. Int J Gynecol Cancer.
23:1712–1716. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Pakish J, Soliman PT, Frumovitz M, Westin
SN, Schmeler KM, Reis RD, Munsell MF and Ramirez PT: A comparison
of extraperitoneal versus transperitoneal laparoscopic or robotic
para-aortic lymphadenectomy for staging ofendometrial carcinoma.
Gynecol Oncol. 132:366–371. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Escobar PF, Fader AN, Rasool N and
Espalliat LR: Single-port laparoscopic pelvic and para-aortic lymph
node sampling or lymphadenectomy: Development of a technique and
instrumentation. Int J Gynecol Cancer. 20:1268–1273. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Kavallaris A, Kalogiannidis I, Chalvatzas
N, Hornemann A, Bohlmann MK and Diedrich K: Standardized technique
of laparoscopic pelvic and para-aortic lymphadenectomy in
gynecologic cancer optimizes the perioperative outcomes. Arch
Gynecol Obstet. 283:1373–1380. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Gouy S, Uzan C, Scherier S, Gauthier T,
Bentivegna E, Kane A, Morice P and Marchal F: Single-port
laparoscopy and extraperitoneal para-aortic lymphadenectomy for
locally advanced cervical cancer: Assessment after 52 consecutive
patients. Surg Endosc. 28:249–256. 2014. View Article : Google Scholar : PubMed/NCBI
|