Introduction
Although the adrenal glands contain no lymphoid
tissue, primary adrenal lymphoma (PAL) is identified in <1% of
cases of non-Hodgkin lymphoma (1).
As a type of extranodal lymphoma, PAL is rare and constitutes
<1% of cases of extranodal lymphomas; PAL is primarily bilateral
but secondary involvement of the adrenal gland is typically
unilateral (2,3). Diffuse large B cell lymphoma (DLBCL) is
the most common subtype of PAL, which represents ~70% of PAL cases
(4,5). Characteristically, PAL predominantly
affects elderly patients without nodular lesions. Diagnosis of PAL
is frequently challenging due to its nonspecific clinical
manifestation and imaging results, and pathological examination is
the only method of confirming this diagnosis (6). The prognosis of PAL is typically poor,
and the 1-year survival rate is 17.5% (3). The current study reports a case of
bilateral primary adrenal diffuse large B cell lymphoma and
performs a review of the literature.
Case report
In June 2016, a 52-year-old female patient was
admitted to the Department of Urology of Peking University Shenzhen
Hospital (Shenzhen, China) due to abdominal pain in the left lumbar
region lasting ~2 weeks. The patient had experience anorexia and
weight loss of ~15 kg in the previous 0.5 months. The patient's
past medical history included grade one hypertension for ~3 years
and cerebral infarction ~2 years previously. On admission, physical
examination revealed that no enlarged superficial lymph nodes were
palpable and there was no hepatosplenomegaly. A full blood count
revealed that had a hemoglobin level of 91 g/l (normal range,
115–150 g/l), a white blood cell count of 5.45×109/l
(normal range, 3.5–9.5×109/l), 55.2% neutrophils (normal
range, 40–75%), 27.2% lymphocytes (normal range, 20–50%), 13.8%
monocytes (normal range, 3–10%), 3.1% eosinophils (normal range,
0.4–8%), 0.7% basophils (normal range, 0–1%), and a platelet count
of 449×109/l (normal range, 125–350×109/l). A
biochemical profile revealed a potassium level of 2.8 mmol/l
(normal range, 3.5–5.3 mmol/l), a sodium level of 138 mmol/l
(normal range, 137–147 mmol/l), an albumin level of 33.7 g/l
(normal range, 40–55 g/l), a uric acid level of 558 µmol/l (normal
range, 155–357 µmol/l), triglyceride levels of 2.13 mmol/l (normal
range, 0–1.7 mmol/l), low density lipoprotein levels of 3.79 mmol/l
(normal range, 0–3.64 mmol/l) and high density lipoprotein levels
of 0.78 mmol/l (normal range, 0.91–1.55 mmol/l). Aldosterone,
cortisol, catecholamines and results of other tests were normal.
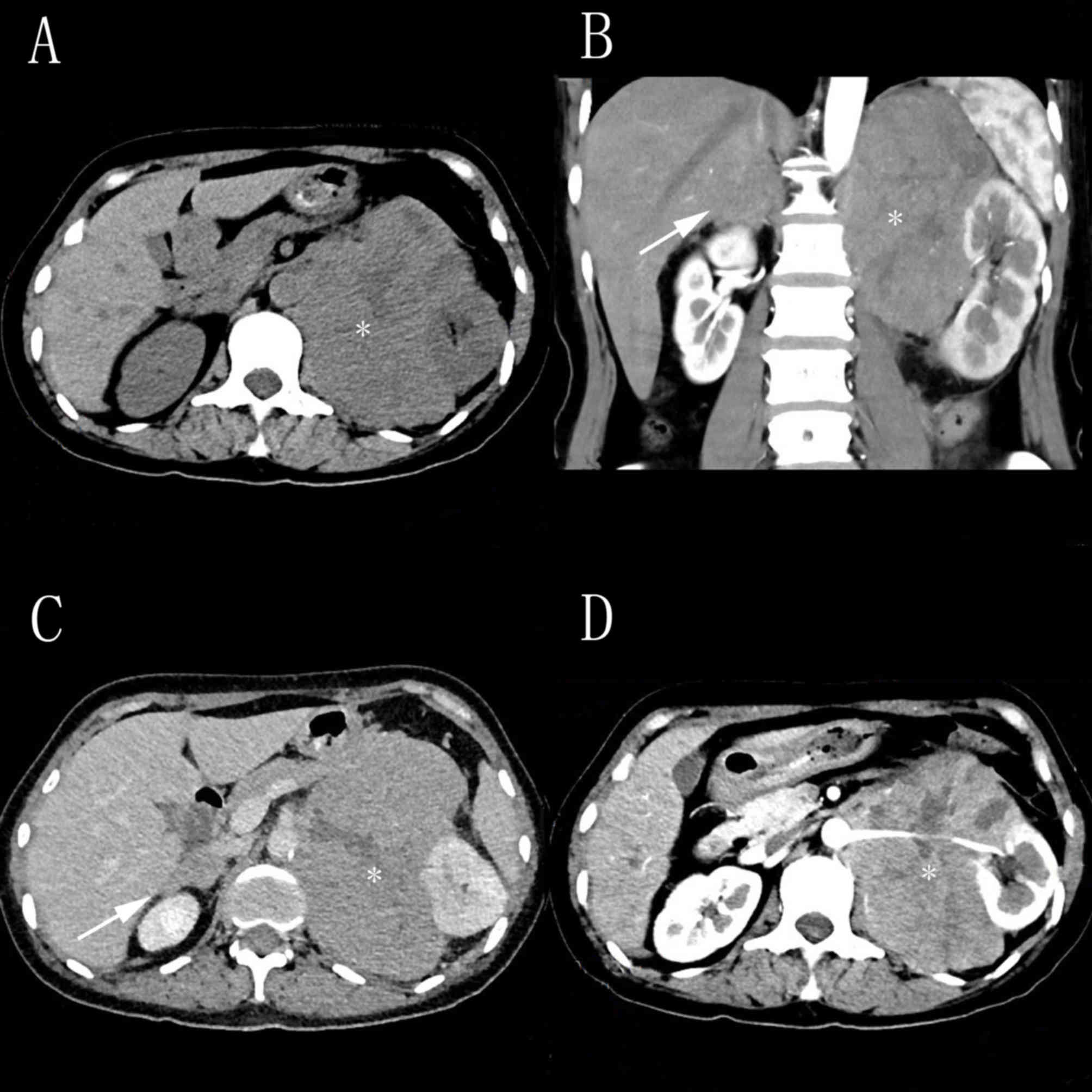
Abdominal ultrasound examination revealed a retroperitoneal tumor,
and computed tomography (CT) scanning revealed that a mass of
132×119×101 mm on the left adrenal gland and a mass of 53×27 mm on
the right adrenal gland without other structural abnormalities
(Fig. 1). Following percutaneous
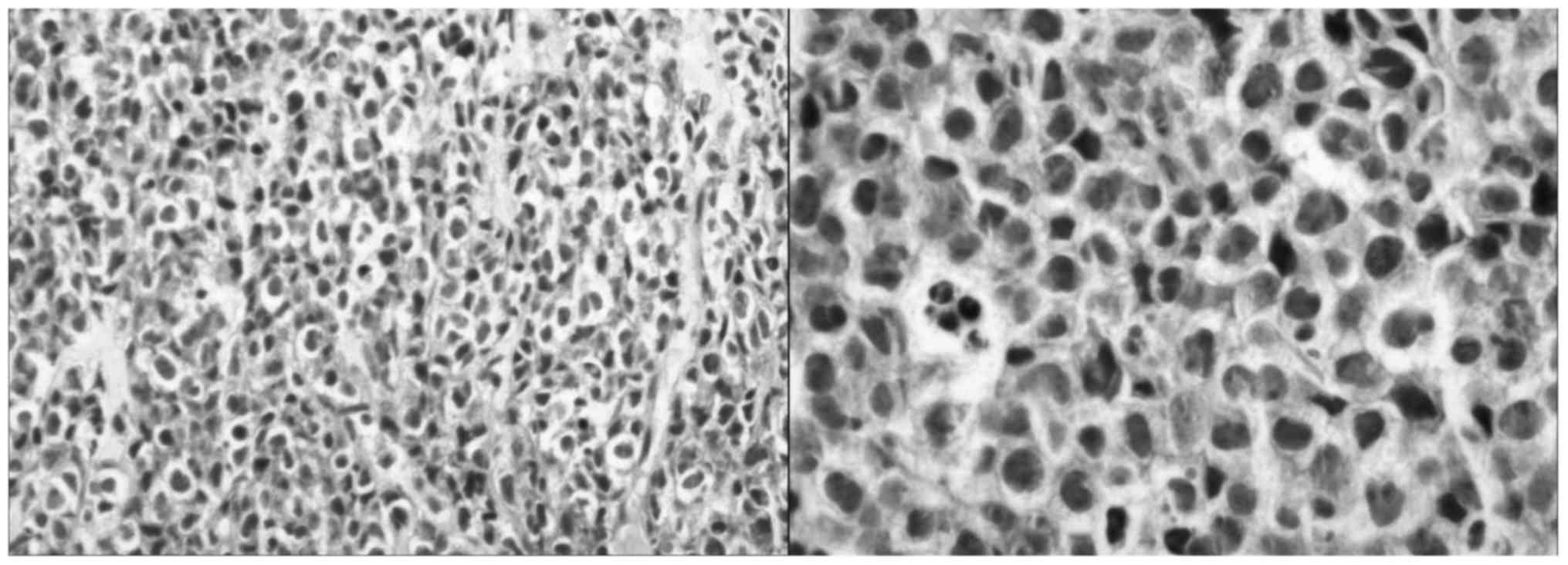
biopsy of the left adrenal gland, histopathological examination
revealed the presence of diffuse large B-cell lymphoma (Fig. 2) positive for CD20, CD5, LCA, Mnm1,
Bcl-6, C-Myc and Ki-67 staining, with a proliferative index of
>98%. Immunostains for cyclin D1, CD3, CD10, CD56, S-100, Cg A,
CK, CK-L and Syn were negative. The patient requested to leave
hospital without surgery, chemotherapy or radiotherapy.
Discussion
PAL without any other extra-adrenal involvement is a
rare subtype of extranodal non-Hodgkin lymphoma, with only ~100
cases reported in the previous medical literature (5). PAL typically occurs in elderly and
male, and ~70% of cases are bilateral (4,7,8). According to previous studies, the male
to female ratio is 7:1 and the average age at diagnosis is 70 years
old (9–11). In the present case, CT revealed no
other lesions except those detected in the bilateral adrenal
glands.
The exact pathogenesis of PAL remains to be
established; however, multifactorial associations have been
described, including autoimmune-associated infections, immune
dysfunction, originating from hematopoietic tissue resting within
adrenal glands, Epstein-Barr virus infection and mutations in the
p53 and c-kit genes (3,12,13). For
example, Epstein-Barr virus serves a role in lymphoma formation
through lymphoid infiltration into the adrenal glands, which lack
lymphoid tissue (3).
The diagnosis of PAL is typically challenging to
perform due to its nonspecific clinical manifestation and uncommon
presentations, which include vague abdominal pain, anemia, weight
loss, unexplained fever, hypercalcemia, thrombocytopenia and
adrenal insufficiency, some of which were present in the current
patient (14). In addition, obvious
clinical manifestations tend to appear when >90% of the adrenal
gland is damaged (6). Various
adrenal gland enlargement sizes have been reported, ranging from
4–17 cm (15). Nevertheless, there
is no correlation between tumor size and adrenal hypofunction
(7). DLBCL is the predominant
histological subtype, which represents ~70% of PAL cases, whereas
the T-immunophenotype makes up ~10% of cases (16–19).
Ultrasound-guided biopsy is recommend for the differential
diagnosis following the identification of low density of adrenal
glands on CT scan images, and immunohistochemical examination
further confirm the diagnosis and prognosis. The recommended
treatment regimen for PAL is R-CHOP (rituximab, cyclophosphamide,
doxorubicin, vincristine and prednisone), a classical chemotherapy
regimen (20), with chemotherapy
being the typical treatment. It has been reported that surgery is
not recommended for treatment (21).
This disease appears to have a poor prognosis, and the median
survival of patients with PAL is reported to be ~1 year (22). There are certain factors effecting
prognosis, such as age, tumor size, lactate dehydrogenase levels
and bilateral involvement.
In conclusion, bilateral primary adrenal diffuse
large B cell lymphoma is a rare entity. PAL with poor prognosis
must be diagnosed at an early stage to potentially improve survival
rates.
Acknowledgements
The present study was supported by the National
Natural Science Foundation of China (grant no. 81101922), Science
and Technology Development Fund Project of Shenzhen (grant nos.
JCYJ20130402114702124 and JCYJ20150403091443329) and the fund of
Guangdong Key medical subject.
References
|
1
|
Mozos A, Ye H, Chuang WY, Chu JS, Huang
WT, Chen HK, Hsu YH, Bacon CM, Du MQ, Campo E and Chuang SS: Most
primary adrenal lymphomas are diffuse large B-cell lymphomas with
non-germinal center B-cell phenotype, BCL6 gene rearrangement and
poor prognosis. Mod Pathol. 22:1210–1217. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Hsu CW, Ho CL, Sheu WH, Harn HJ and Chao
TY: Adrenal insufficiency caused by primary aggressive
non-Hodgkin's lymphoma of bilateral adrenal glands: Report of a
case and literature review. Ann Hematol. 78:151–154. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Grigg AP and Connors JM: Primary adrenal
lymphoma. Clin Lymphoma. 4:154–160. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Erçolak V, Kara O, Günaldı M, Afşar C
Usul, Duman B Bozkurt, Açıkalın A, Ergin M and Erdoğan S: Bilateral
primary adrenal non-hodgkin lymphoma. Turk J Haematol. 31:205–206.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
De Miguel Sánchez C, Ruiz L, González JL
and Hernández JL: Acute adrenal insufficiency secondary to
bilateral adrenal B-cell lymphoma: A case report and review of the
literature. Ecancermedicalscience. 10:6342016. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Ezer A, Parlakgümüş A, Kocer NE, Colakoğlu
T, Nursal GN and Yildirim S: Primary adrenal non-Hodgkin's
lymphoma: Report of two cases. Turk J Gastroenterol. 22:643–647.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Wang J, Sun NC, Renslo R, Chuang CC,
Tabbarah HJ, Barajas L and French SW: Clinically silent primary
adrenal lymphoma: A case report and review of the literature. Am J
Hematol. 58:130–136. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Aziz SA, Laway BA, Rangreze I, Lone MI and
Ahmad SN: Primary adrenal lymphoma: Differential involvement with
varying adrenal function. Indian J Endocrinol Metab. 15:220–223.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Lee KS, Chung YS, Park KH, Kim HS and Kim
HM: A case of primary bilateral adrenal lymphoma with partial
adrenal insufficiency. Yonsei Med J. 40:297–300. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Dahami Z, Debbagh A, Dakir M, Hafiani M,
Joual A, Bennani S, Mrini M and Benjelloun S: Phenotype B primitive
adrenal lymphoma, diagnosed by percutaneous aspiration biopsy. Ann
Urol (Paris). 35:22–25. 2001.(In French). View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Wang JP, Sun HR, Li YJ, Bai RJ and Gao S:
Imaging features of primary adrenal lymphoma. Chin Med J (Engl).
122:2516–2520. 2009.PubMed/NCBI
|
|
12
|
Ohsawa M, Tomita Y, Hashimoto M, Yasunaga
Y, Kanno H and Aozasa K: Malignant lymphoma of the adrenal gland:
Its possible correlation with the Epstein-Barr virus. Mod Pathol.
9:534–543. 1996.PubMed/NCBI
|
|
13
|
Padhi S and Sahoo J: Primary adrenal non
Hodgkin lymphoma: Changing trends. Turk J Gastroenterol. 26:85–86.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Ozimek A, Diebold J, Linke R, Heyn J,
Hallfeldt K and Mussack T: Bilateral primary adrenal non-Hodgkin's
lymphoma and primary adrenocortical carcinoma-review of the
literature preoperative differentiation of adrenal tumors. Endocr
J. 55:625–638. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Kacem K, Zriba S, Lakhal RB, Bouteraa W,
Aissaoui L, Amor RB, Abdennebi YB, Ali ZB, Abid HB and Meddeb B:
Primary adrenal lymphoma. Turk J Haematol. 31:188–191. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Li Y, Sun H, Gao S and Bai R: Primary
bilateral adrenal lymphoma: 2 case reports. J Comput Assist Tomogr.
30:791–793. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Libé R, Giavoli C, Barbetta L, Dall'Asta
C, Passini E, Buffa R, Beck-Peccoz P and Ambrosi B: A primary
adrenal non-Hodgkin's lymphoma presenting as an incidental adrenal
mass. Exp Clin Endocrinol Diabetes. 114:140–144. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Mantzios G, Tsirigotis P, Veliou F,
Boutsikakis I, Petraki L, Kolovos J, Papageorgiou S and Robos Y:
Primary adrenal lymphoma presenting as Addison's disease: Case
report and review of the literature. Ann Hematol. 83:460–463. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Rashidi A and Fisher SI: Primary adrenal
lymphoma: A systematic review. Ann Hematol. 92:1583–1593. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Kim YR, Kim JS, Min YH, Hyunyoon D, Shin
HJ, Mun YC, Park Y, Do YR, Jeong SH, Park JS, et al: Prognostic
factors in primary diffuse large B-cell lymphoma of adrenal gland
treated with rituximab-CHOP chemotherapy from the consortium for
improving survival of lymphoma (CISL). J Hematol Oncol. 5:492012.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Bouchikhi AA, Tazi MF, Amiroune D, Mellas
S, El Ammari J, Khallouk A, El Fassi MJ and Farih MH: Primary
bilateral Non-Hodgkin's lymphoma of the adrenal gland: A case
report. Case Rep Urol. 2012:3256752012.PubMed/NCBI
|
|
22
|
Horiguchi K, Hashimoto K, Hashizume M,
Masuo T, Suto M, Okajo J, Handa H, Kaneko Y, Yokoo H, Sasaki A, et
al: Primary bilateral adrenal diffuse large B-cell lymphoma
demonstrating adrenal failure. Intern Med. 49:2241–2246. 2010.
View Article : Google Scholar : PubMed/NCBI
|