Introduction
Liver resections are feasible and safe procedures
when performed by specialized hepatobiliary teams (1). However, in certain, more complex cases,
applying techniques such as the liver hanging manoeuvre may be
required (2). In addition, when
there is compression or malignant invasion of the inferior vena
cava (IVC) by hepatic tumours, as indicated by preoperative
radiological imaging (3,4), the associated perioperative morbidity
and mortality increase. In order to mitigate these risks and safely
perform complex resections, modifications of the conventional liver
resection techniques become necessary. We herein report the
technical modifications of the classic hanging manoeuvre used in a
patient with colorectal liver metastasis (CRLM) who required an
extended right hepatectomy with en bloc resection and
reconstruction of the IVC.
Case report
A 54-year old man presented 3 years after right
hemicolectomy for a caecal carcinoma with an asymptomatic CRLM in
the right liver. The patient had completed 8 cycles of adjuvant
systemic treatment with leucovorin, flourouracil and oxaliplatin
(FOLFOX regimen) after the index right hemicolectomy. After CRLM
was detected on surveillance computed tomography (CT) scans, 3
courses of second-line bevacizumab-based systemic therapy were
administered. There was minimal demonstrable response, so the
patient was referred to the hepatobiliary team for evaluation.
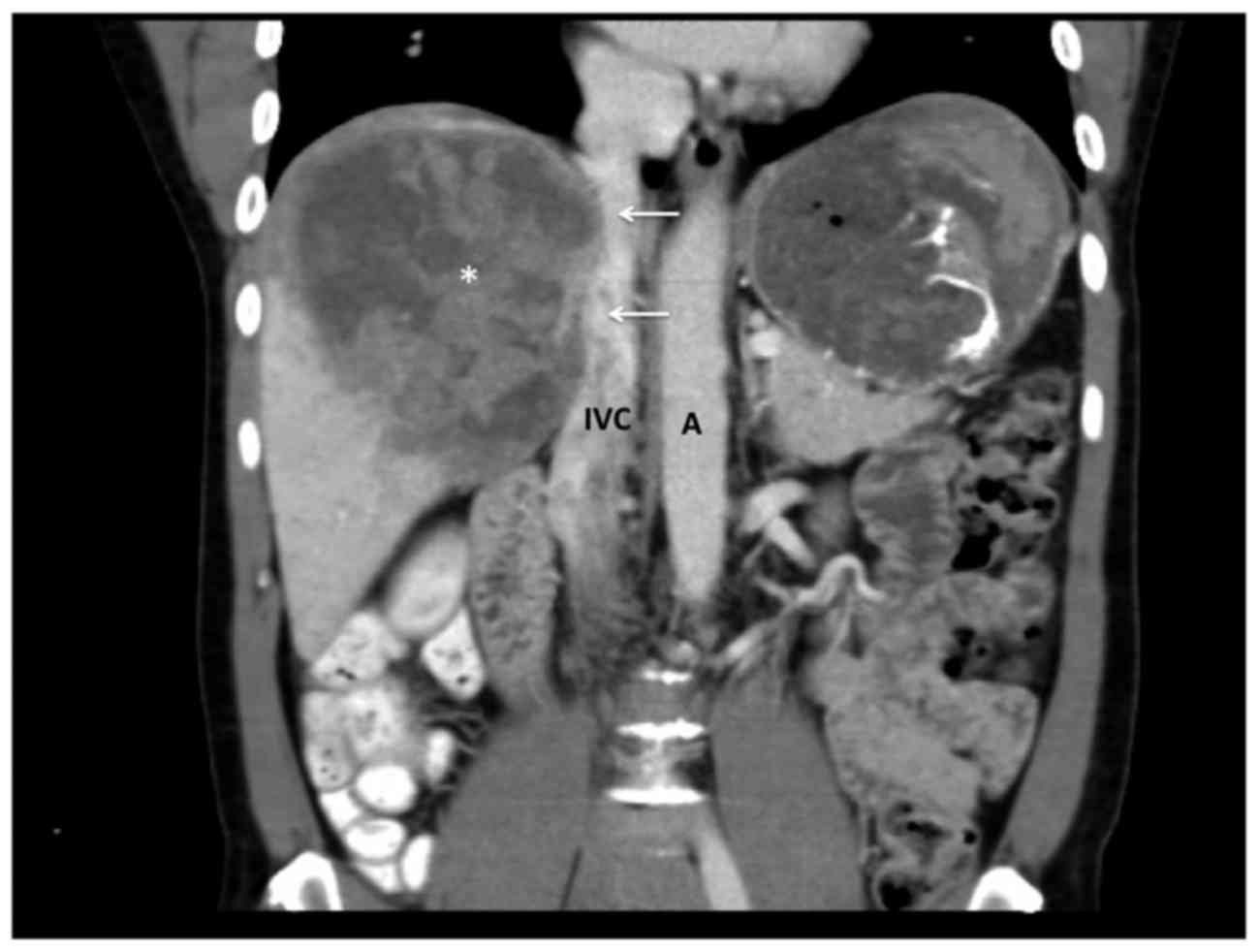
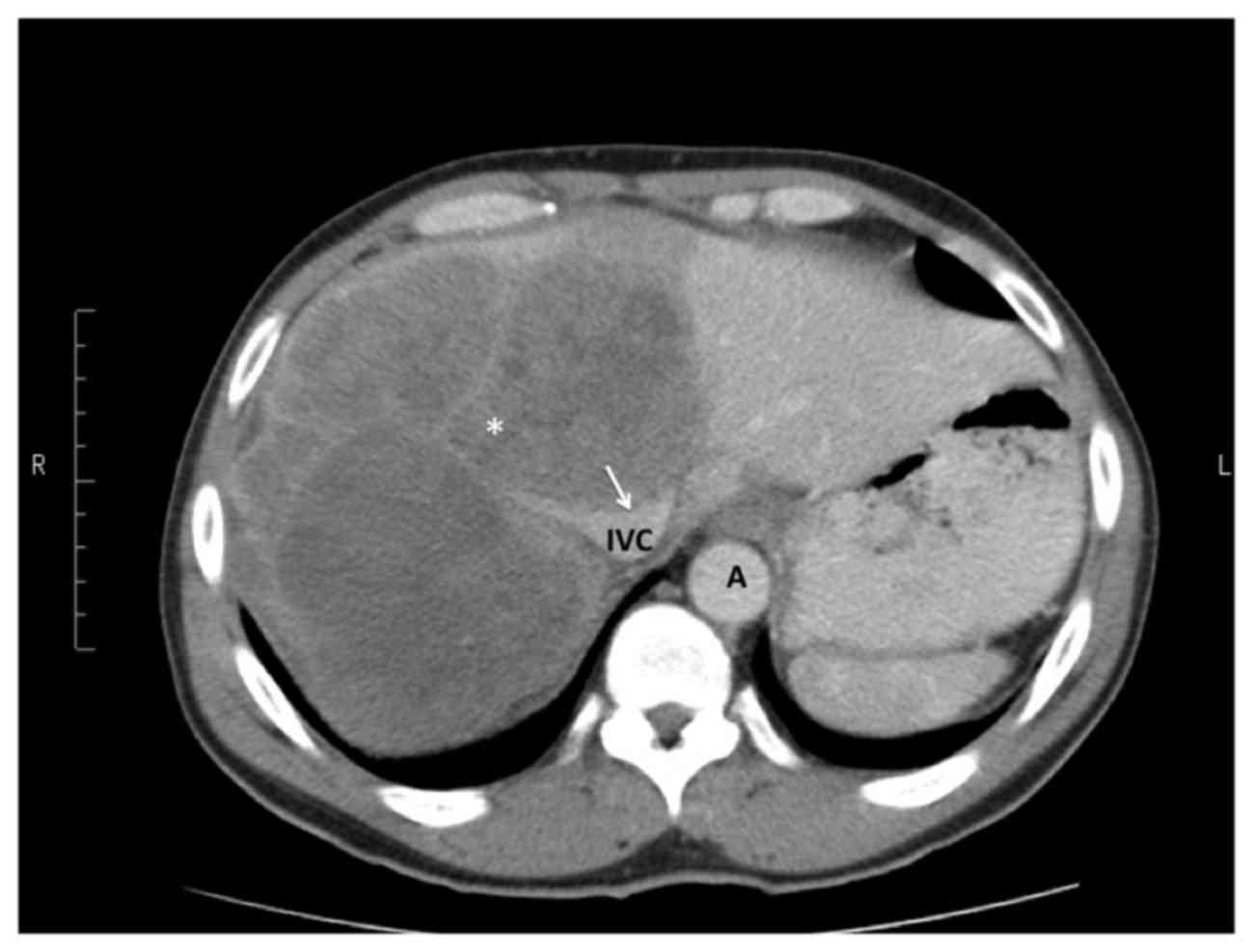
On CT scans, a solitary 25.4-cm CRLM was identified
in the right hemi-liver extending into SIV. There was
suspected caval invasion on CT scans, as evidenced by distortion of
the upper IVC and loss of the plane at the posterior liver surface
(Figs. 1 and 2). Although the CRLM completely encased the
right hepatic vein and appeared to involve the middle hepatic vein,
the left hepatic vein remained uninvolved and the hilar structures
were tumour-free.
A decision was made to proceed with extended right
hepatectomy, with planned resection and reconstruction of the IVC.
The abdomen was accessed using an upper midline incision with
transverse extension. The line of parenchymal transection was
identified using intraoperative ultrasound to select a plane that
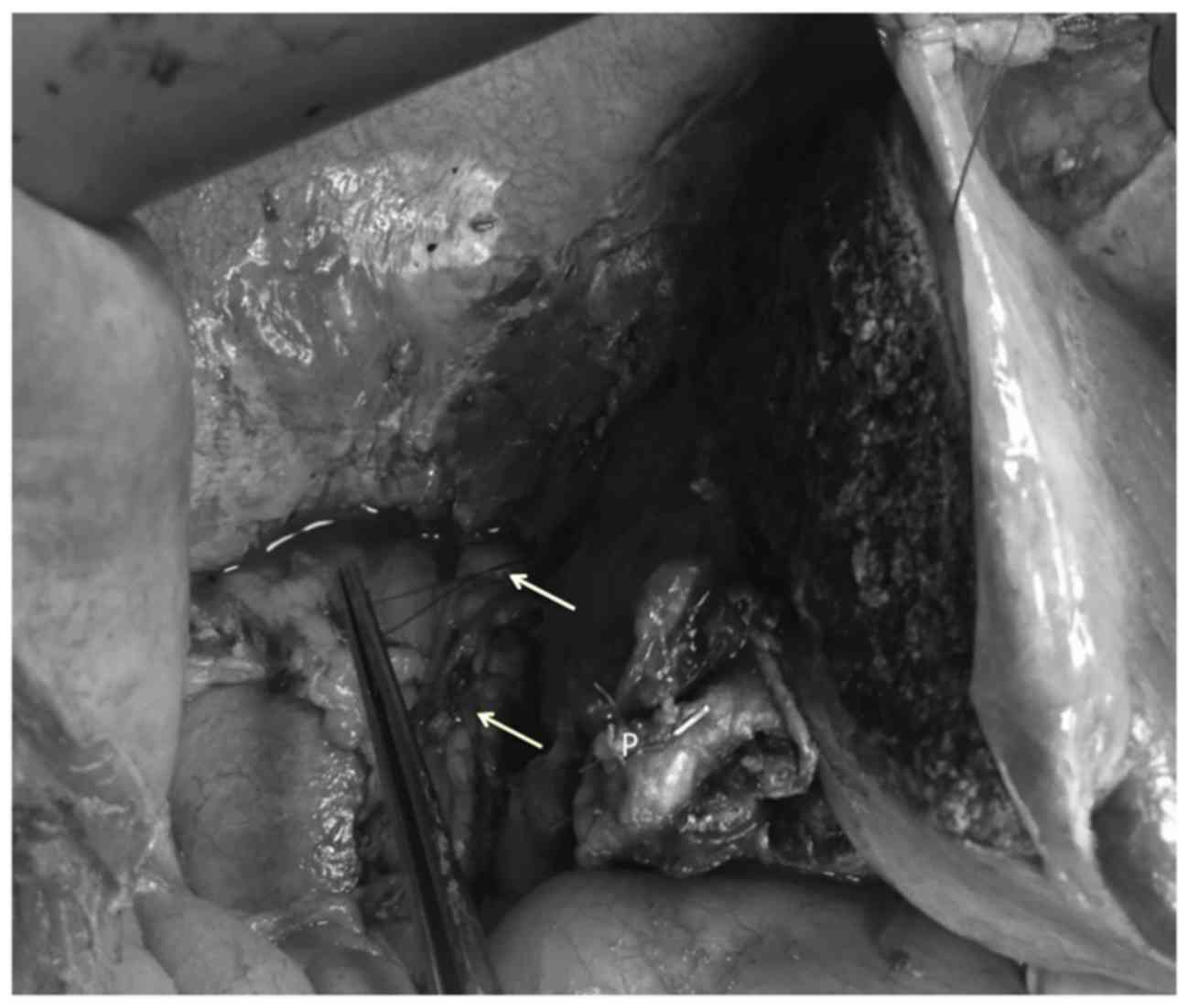
was clear of the margins of the tumour. The CRLM occupied the
entire right upper quadrant (Fig.
3), effectively precluding visualization of diaphragmatic
attachments. Without being able to mobilize the right liver for
conventional resection, transection via the anterior approach
without prior mobilization was considered, which would require a
hanging manoeuvre to be executed safely. The classic hanging
manoeuvre involves lifting the liver with a tape passed along the
avascular plane at the 10–11 o'clock position over the IVC
(2). In this case, preoperative
scans suggested that this avascular plane was involved by the
tumour. Therefore, blind passage of an instrument in this plane
would be likely to cause torrential bleeding and breach the tumour,
preventing R0 resection.
Instead, a modification of the classic hanging
manoeuvre was used. Initially, the left hepatic vein junction was
dissected out superiorly to establish access. A DeBakey vascular
clamp was then passed over the anterior surface of the
retro-hepatic IVC at the 2–3 o'clock position, directing it
cephalad to exit at the left side of the left hepatic vein. This
facilitated passage of a 20Fr nasogastric tube posteromedially
behind the liver. Traction on this nasogastric tube anteriorly and
to the left allowed partially lifting the liver with the heavy CRLM
off the IVC. This allowed passing a second DeBakey clamp over the
IVC at the 1 o'clock position with less resistance. The second
instrument was directed between the middle and left hepatic veins,
and was used to pass a second nasogastric tube in that plane
(Fig. 4). The cephalad end of the
second nasogastric tube was tied to our Omnitract® retractor and
the surgeon pulled on the caudal end to provide controlled traction
(Fig. 5).
This allowed performing an anterior transection of
the hepatic parenchyma at the line previously selected with
intraoperative ultrasound, guided down to the uninvolved IVC
surface with controlled traction on the nasogastric tube. Once
anterior transection was complete, the point of tumour invasion
into the IVC was visualized (Fig.
6). The anterior wall of the IVC was invaded by the tumour for
5–6 cm in length and 25% of its diameter. The IVC was controlled
with side-biting Satinsky clamps and the IVC wall was resected en
bloc with the tumour to achieve 3–5-mm margins. The IVC was
reconstructed primarily with 4/0 PDS sutures, resulting in
narrowing to approximately 2/3 of its original diameter (Fig. 7).
After the parenchymal transection and IVC repair
were completed, the operation proceeded in a conventional manner.
The right liver was mobilized by dividing the right triangular and
coronary ligaments under direct visualization. The right hepatic
pedicle was dissected and ligated using 3/0 polypropylene sutures.
The right liver was then removed from the abdomen.
The operation was completed uneventfully in 315 min.
The total blood loss was estimated to be 1,100 ml and the patient
required transfusion of two units of packed cells intraoperatively.
The postoperative recovery was also uneventful. The patient
remained in the high dependency unit for 48 h. The remaining
recovery was uneventful and he was discharged from the hospital on
the tenth postoperative day.
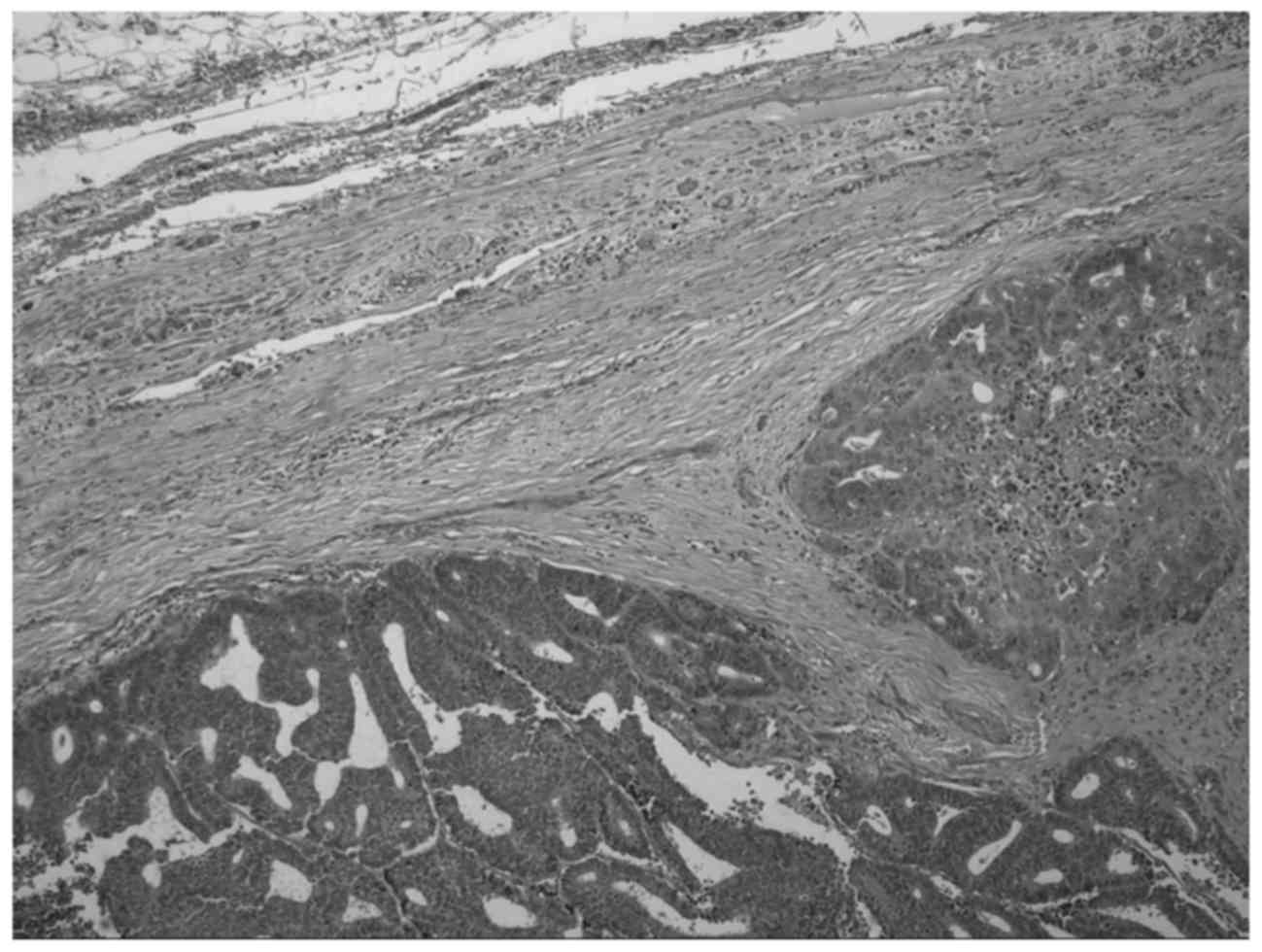
Histopathological assessment of the specimen
confirmed CRLM with malignant invasion of the IVC. The parenchymal
resection margins were clear of tumour. The tumour had invaded into
the IVC, but the caval resection margins were histologically clear
(Fig. 8).
Written informed consent was obtained from the
patient regarding the publication of this case report and
accompanying images.
Discussion
Malignant invasion of the IVC is difficult to
predict on preoperative imaging, as it is a low-pressure vessel
that may easily be compressed by hepatic tumours (3,4). The
radiological criteria predictive of malignant invasion include:
Longitudinal IVC indentation for >50 mm, transverse compression
of >50% of the IVC circumference, lesions protruding into the
IVC lumen, and the presence of well-developed collaterals (4). Maeba et al (4) reported that the presence of ≥1 of these
radiological criteria may predict malignant IVC invasion with 60%
overall accuracy. Using these criteria, IVC invasion was
anticipated in our patient, since there was compression of >50%
of the transverse IVC diameter and >5 cm longitudinal IVC
compression. Endoscopic ultrasonography may have added to the
preoperative assessment of malignant IVC invasion (5), but it was unavailable.
Despite malignant IVC invasion, an aggressive
attempt was made at R0 margin clearance, as IVC resection and
reconstruction is currently considered to be potentially curative
when it results in histologically clear margins (3,4,6–8). In
these cases, the conventional techniques for liver resection may
not be feasible. The conventional technique involves complete
mobilization of the right liver in order to approach the IVC and to
control the hepato-caval junction prior to parenchymal transection
(9). Mobilization was not possible
in the present case, as the large CRLM precluded visualization and
dissection of the right triangular and coronary ligaments. It would
also have been ill-advised from an oncological standpoint, as there
is a risk of tumour rupture and seeding with the force that would
be applied to mobilize a fixed and non-compliant liver heavily
infiltrated with tumour. Therefore, two techniques were utilized
for resection: The hanging manoeuvre and anterior parenchymal
transection.
Ozawa (10) described
the anterior transection technique in 1990. This technique was
popularized over the next decade (11–15),
driven by the perceived disadvantages of conventional right liver
mobilization, namely impaired hepatic blood flow with rotational
displacement of the liver (10),
potential avulsion of hepatic veins (13), iatrogenic tumour rupture (13,16), and
hematogenous dissemination of malignant cells when the hepatic
veins remained patent (16–19).
Liu et al (13) were the first to evaluate this in a
prospective randomized trial, in which 120 patients undergoing
major resections were randomized to hepatectomy via the anterior or
the conventional approach. The authors did not include any patients
with IVC invasion, but there were caudate resections in 7 patients
with conventional and in 4 patients with anterior transection.
There were no attempts at the hanging manoeuvre in that study.
There was a statistically significant reduction in the number of
patients with massive blood loss >2 l (8.3 vs. 28.3%; P=0.005),
reduced transfusion requirements (0 vs. 0.3 l; P=0.001) and better
median survival (68.1 vs. 22.6 months; P=0.006) with the anterior
vs. conventional transection technique, respectively. However,
Capussotti et al (20)
prospectively randomized 65 patients undergoing right hepatectomy
via the conventional or anterior approach, excluding patients with
caudate lobe involvement (n=9) or IVC invasion (n=3). Although the
authors routinely attempted the hanging manoeuvre, it was only
completed in 30/33 patients in the anterior transection group,
being abandoned due to adhesions (n=2) or major bleeding (n=1), and
they could not demonstrate any significant advantage with the
anterior vs. the conventional approach in terms of overall blood
loss (437 vs. 500 ml, respectively; P=0.960), perioperative
transfusion rates (18 vs. 9.3%, respectively; P=0.253) or
perioperative mortality (P=0.746). Thus, Capussotti et al
(20) did not support routine use of
the anterior approach.
Due to the conflicting data, Li et al
(16) performed a meta-analysis of
807 patients across 2 prospective randomized trials (13,20),
plus an additional 6 non-randomized controlled trials (11,12,21–24)
comparing 444 patients undergoing conventional right hepatectomy to
363 undergoing right hepatectomy via anterior transection. The
authors reported that the anterior approach resulted in significant
reductions in transfusion rate (35 vs. 57.3%; P<0.01), mortality
(1.9 vs. 7.4%; P<0.01) and local recurrence (48.9 vs. 62.9%;
P<0.01; odds ratio=0.57; 95% confidence interval: 0.37–0.87).
Although existing data lean towards the anterior approach, there
are currently insufficient high-quality data to determine which is
the optimal method for right hepatectomy. It is clear, however,
that hepatobiliary surgeons should be familiar with the anterior
transection technique as a part of their armamentarium. In the
present case, the anterior transection technique was deemed
necessary as i) the bulky right liver could not be mobilized by the
conventional technique and ii) the point of malignant IVC invasion
could be approached in a controlled manner in preparation for
resection.
The hanging manoeuvre was also utilized in order to
guide the line of transection and control bleeding from deep
parenchymal vessels. Several investigators have reported good
outcomes when they used the combination of anterior transection and
the hanging manoeuvre to complete resections for a variety of
pathologies (11,13,25–29).
Apart from serving as a directional guide during parenchymal
transection (25), utilizing the
hanging manoeuvre is associated with a lower risk of tumour
dissemination into the hepatic veins (13), reduced incidence of tumour rupture
(11,13), reduced blood loss (28), lower operative time (28), reduced transfusion requirements
(28), and shorter duration of
hospitalization (26).
Malignant IVC invasion was initially considered an
absolute contraindication to the hanging manoeuvre (30). However, there have been published
case reports (29,31,25) and
one small series of 7 cases (27),
where this manoeuvre was used to perform complex resections
facilitating partial IVC resection and reconstruction in patients
with malignant invasion. There were good outcomes in all cases, all
with R0 resection. Also in the series published by Coppa et
al (27) there was no mortality,
40% morbidity, and an 83% overall 5-year survival rate.
In the present case, we opted to attempt an
IVC-preserving strategy using a modified hanging manoeuvre. In the
original description by Belghiti et al (2) in 2001, a long vascular clamp was passed
along the avascular plane at the 10–11 o'clock position on the
anterior surface of the IVC in order to pass a tape to suspend the
liver during transection. This could not be achieved for two
reasons: i) Preoperative imaging demonstrated CRLM invasion into
the anterolateral IVC over the 11 o'clock position and ii) the
large, heavy CRLM exerted pressure on the surface of the IVC,
adding resistance to instrument passage. Thus, Belghiti's (2) classic hanging manoeuvre was modified by
passing the instrument to the left of IVC at the 2–3 o'clock
position. The instrument was directed cephalad to exit to the left
of the left hepatic vein. Many caution against instrument passage
at this location (25), as it is the
usual location of the short hepatic and caudate veins. However,
these are usually small veins, mostly sub-millimeter in diameter
(32–36), and they vary in number, position and
dimensions (33–35). If they are encountered during the
hanging manoeuvre, the resultant bleeding is often mild due to the
small diameter and low pressure within these veins. This bleeding
should be easy to control by allowing the interrupted veins to be
compressed by the weight of the liver. Moreover, Kanamura et
al (37) demonstrated that
similar short hepatic/caudate veins may be found in the classic
avascular plane in 16.3% of the cases, and do not usually pose a
problem. Some have described this manoeuvre under sonographic
(38) or endoscopic (39,40)
guidance, in order to detect and avoid short hepatic veins when
they exist; however, this was not available in our institution. In
the present case, the encountered bleeding was minimal and easy to
control with gentle, blind passage of the instruments aided by
bimanual finger dissection, when necessary, as described by Aydin
et al (41).
Once the plane was established, a 20Fr nasogastric
tube was passed and used it to deliver traction anteriorly and to
the left, in order to lift the liver and heavy CRLM, partially
relieving the pressure applied onto the IVC. This in turn allowed
passage of another instrument at the 1 o'clock position, with
passing of a second tube directed between the middle and left
hepatic veins. This double-tube hanging manoeuvre effectively
lifted the central hepatic segments off the IVC, allowing us to
safely define the intended resection plane. In 2008, Chen et
al (42) described a double-tape
hanging manoeuvre, where two tapes were placed in an avascular
plane to the right of the IVC. The rationale for this modification
was to achieve complete outflow control when the tapes were lifted
in opposite directions (42).
However, Liddo et al (25)
pointed out that this manoeuvre could not guide transection, since
the tapes were not positioned along the resection line. In our
modification, the tubes were passed in different planes, the
rationale being to safely identify the intended plane along the IVC
that would be clear of tumour, in order to guide the transection
lines. We acknowledge that this modification increases the risk of
rupture of the short hepatic veins and, although we believe that
the resultant bleeding would be mild and can be managed
appropriately, we also acknowledge that this modification is
unnecessary in simple resections; it only became necessary as we
were unable to safely pass an instrument in the plane described by
Belghiti et al (2).
Using these techniques followed by mobilization of
the right liver allowed us to expose both sides of the IVC invaded
by tumour and to pass a side-biting Satinsky clamp to allow
controlled resection of the IVC wall to achieve clear margins. This
selective IVC clamping technique was initially described by Togo
et al (5) as a means to
maintain flow through the systemic and hepatic circulations. It
also allowed us to evaluate the degree of narrowing that resection
and primary repair would yield, in order to decide whether total
vascular exclusion and IVC replacement would be necessary.
Most authorities recommend IVC reconstruction, as
complete ligation usually results in venous insufficiency and acute
renal failure (3,6,8). Ohwada
et al (7) recommended
reconstruction with an interposed segment of
polytetrafluoroethylene when primary closure would result in
>50% narrowing of the normal IVC diameter. In the present case,
selective clamping revealed that resection would result in
narrowing to ~2/3 of the original IVC diameter. Therefore, we opted
for primary repair with vascular sutures, since this would
sacrifice less caval wall compared with a stapled repair.
In conclusion, complex liver resection with IVC
resection and reconstruction may be performed safely in centralized
referral centers with dedicated hepatobiliary teams. Aggressive
attempts at R0 resections are justified, since they are potentially
curative for patients with CRLM. In these cases, hepatobiliary
surgeons must be familiar with modified resection techniques, such
as the classic hanging manoeuvre, anterior transection, selective
caval clamping, total extravascular control, and IVC
replacement/reconstruction. We recommend that this modification of
the hanging manoeuvre be added to the armamentarium of
hepatobiliary surgeons to improve safety in complex resections.
References
|
1
|
Fong Y, Gonen M, Rubin D, Radzyner M and
Brennan MF: Long term survival is superior after resection for
cancer in high volume centres. Ann Surg. 242:540–547.
2005.PubMed/NCBI
|
|
2
|
Belghiti J, Guevara OA, Noun R, Saldinger
PF and Kianmanesh R: Liver hanging maneuver: A safe approach to
right hepatectomy without liver mobilization. J Am Coll Surg.
193:109–111. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Okada Y, Nagino M, Kamiya J, Yamamoto H,
Hayakawa N and Nimura Y: Diagnosis and treatment of inferior vena
caval invasion by hepatic cancer. World J Surg. 27:689–694. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Maeba T, Okano K, Mori S, Karasawa Y, Goda
F, Wakabayashi H, Usuki H and Maeta H: Extent of pathologic
invasion of the inferior vena cava in resected liver cancer
compared with possible caval invasion diagnosed by preoperative
images. J Hepatobiliary Pancreat Surg. 7:299–305. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Togo S, Shimada H, Tanaka K, Masui H,
Fujii S, Endo I and Sekido H: Management of malignant tumor with
intracaval extension by selective clamping of IVC.
Hepatogastroenterology. 43:1165–1171. 1996.PubMed/NCBI
|
|
6
|
Huguet C, Ferri M and Gavelli A: Resection
of the suprarenal inferior vena cava. The role of prosthetic
replacement. Arch Surg. 130:793–798. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Ohwada S, Ogawa T, Kawashima Y, Ohya T,
Kobayashi I, Tomizawa N, Otaki A, Takeyoshi I, Nakamura S and
Morishita Y: Concomitant major hepatectomy and inferior vena cava
reconstruction. J Am Coll Surg. 188:63–71. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Duckett JW Jr, Lifland JH and Peters PC:
Resection of the inferior vena cava for adjacent malignant
diseases. Surg Gynecol Obstet. 136:711–716. 1973.PubMed/NCBI
|
|
9
|
Schwartz SI: Right Hepatic Lobectomy. Am J
Surg. 148:668–673. 1984. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Ozawa K: Hepatic function and liver
resection. J Gastroenterol Hepatol. 5:296–309. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Liu CL, Fan ST, Lo CM, Tung-Ping Poon R
and Wong J: Anterior approach for major right hepatic resection for
large hepatocellular carcinoma. Ann Surg. 232:25–31. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Lai EC, Fan ST, Lo CM, Chu KM and Liu CL:
Anterior approach for difficult major right hepatectomy. World J
Surg. 20:314–318. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Liu CL, Fan ST, Cheung ST, Lo CM, Ng IO
and Wong J: Anterior approach versus conventional approach right
hepatic resection for large hepatocellular carcinoma: A prospective
randomized controlled study. Ann Surg. 244:194–203. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Azoulay D, Marin-Hargreaves G, Castaing D,
Adam R, Savier E and Bismuth H: The anterior approach: The right
way for right massive hepatectomy. J Am Coll Surg. 192:412–417.
2001. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Abdalla EK, Noun R and Belghiti J: Hepatic
vascular occlusion: Which technique? Surg Clin North Am.
84:563–585. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Li L, Wang HQ, Wang Q, Yang J and Yang JY:
Anterior vs. conventional approach hepatectomy for large liver
cancer: A meta-analysis. World J Gastroenterol. 20:17235–17243.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Miyazono F, Takao S, Natsugoe S, Uchikura
K, Kijima F, Aridome K, Shinchi H and Aikou T: Molecular detection
of circulating cancer cells during surgery in patients with
biliary-pancreatic cancer. Am J Surg. 177:475–479. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Hayashi N, Egami H, Kai M, Kurusu Y,
Takano S and Ogawa M: No-touch isolation technique reduces
intraoperative shedding of tumor cells into the portal vein during
resection of colorectal cancer. Surgery. 125:369–374. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Louha M, Nicolet J, Zylberberg H, Sabile
A, Vons C, Vona G, Poussin K, Tournebize M, Capron F, Pol S, et al:
Liver resection and needle liver biopsy cause hematogenous
dissemination of liver cells. Hepatology. 29:879–882. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Capussotti L, Ferrero A, Russolillo N,
Langella S, Lo Tesoriere R and Viganò L: Routine anterior approach
during right hepatectomy: Results of a prospective randomised
controlled trial. J Gastrointest Surg. 16:1324–1332. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Li SQ, Liang LJ, Peng BG, Yin XY, Lü MD,
Kuang M, Li DM and Fu SJ: A comparative study of anterior versus
conventional approach right hepatectomy for large hepatocellular
carcinoma. Zhonghua Yi Xue Za Zhi. 90:1670–1673. 2010.PubMed/NCBI
|
|
22
|
Wu TJ, Wang F, Lin YS, Chan KM, Yu MC and
Lee WC: Right hepatectomy by the anterior method with liver hanging
versus conventional approach for large hepatocellular carcinomas.
Br J Surg. 97:1070–1078. 2010. View
Article : Google Scholar : PubMed/NCBI
|
|
23
|
Takács I, Furka A, Kotán R, Mehrdad G
Boland, Pósán J, Vágvölgyi A, Hallay J and Sápy P: Anterior
approach for liver resection in the cases of the treatment of large
liver tumors. Magy Seb. 59:362–368. 2006.PubMed/NCBI
|
|
24
|
Wang CC, Jawade K, Yap AQ, Concejero AM,
Lin CY and Chen CL: Resection of large hepatocellular carcinoma
using the combination of liver hanging maneuver and anterior
approach. World J Surg. 34:1874–1878. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Liddo G, Buc E, Nagarajan G, Hidaka M,
Dokmak S and Belghiti J: The liver hanging manoeuvre. HPB.
11:296–305. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Llado L, Muñoz A, Ramos E, Torras J,
Fabregat J and Rafecas A: The anterior hanging-approach improves
postoperative course after right hepatectomy in patients with
colorectal liver metaseases. Resutls of a prospective study with
propensity-score mathing comparison. Eur J Surg Oncol. 42:176–183.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Coppa J, Citterio D, Cotsoglou C, Germini
A, Piccioni F, Sposito C and Mazzaferro V: Transhepatic anterior
approach to the inferior vena cava in large retroperitoneal tumours
resected en bloc with the right liver lobe. Surgery. 154:1061–1068.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Beppu T, Ishiko T, Chikamoto A, Komori H,
Masuda T, Hayashi H, Okabe H, Otao R, Sugiyama S, Nasu J, et al:
Liver hanging maneuver decreases blood loss and operative time in a
right side hepatectomy. Hepatogastroenterology. 59:542–545.
2012.PubMed/NCBI
|
|
29
|
Hwang S, Lee SG, Yee YJ, Kim KH, Ahn CS,
Kim KW, Ko KH and Choi NK: Modified liver hanging maneuver to
facilitate left hepatectomy and caudate lobe resection for hilar
bile duct cancer. J Gastrointest Surg. 12:1288–1292. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Nanashima A, Sumida Y, Abo T, Takeshita H,
Hidaka S, Sawai T, Yasutake T and Nagayasu T: Trisectionectomy for
large hepatocellular carcinoma using the liver hanging maneuver.
Eur J Surg Oncol. 35:326–330. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Cawich SO, Thomas DA, Ramjit C, Bhagan R
and Naraynsingh V: Complex liver resections for colorectal
metastases: Are they safe in a low-volume, resource-poor caribbean
setting? Case Rep Surg 2015. 5709682015.
|
|
32
|
Kogure K, Kuwano H, Fujimaki N and
Makuuchi M: Relation among portal segmentation, proper hepatic
vein, and external notch of the caudate lobe in the human liver.
Ann Surg. 231:223–228. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Hirai I, Murakami G, Kimura W, Kanamura T
and Sato I: How should we treat short hepatic veins and paracaval
branches in anterior hepatectomy using the hanging manoeuvre
without mobilization of the liver? An anatomical and experimental
study. Clin Anat. 16:224–232. 2003. View
Article : Google Scholar : PubMed/NCBI
|
|
34
|
Sato TJ, Hirai I, Murakami G, Kanamura T,
Hata F and Hirata K: An anatomical study of short hepatic veins,
with special reference to delineation of the caudate lobe for
hanging manoeuvre of the liver without the usual mobilization. J
Hepatobiliary Pancreat Surg. 9:55–60. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Trotovsek B, Belghiti J, Gadzijev EM,
Ravnik D and Hribernik M: Anatomical basis of the liver hanging
manoeuvre. Hepatogastroenterology. 52:728–730. 2005.PubMed/NCBI
|
|
36
|
Kogure K, Kuwano H, Yorifuji H, Ishikawa
H, Takata K and Makuuchi M: The caudate processus hepatic vein: A
boundary hepatic vein between the caudate lobe and the right liver.
Ann Surg. 247:288–293. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Kanamura T, Murakami G, Hirai L, Hata F,
Sato TJ, Kumon M and Nakajima Y: High dorsal drainage routes of
Spiegel's lobe. J Hepatobiliary Pancreat Surg. 8:549–556. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Kokudo N, Imamura H, Sano K, Zhang K,
Hasegawa K, Sugawara Y and Makuuchi M: Ultrasonically assisted
retrohepatic dissection for a liver hanging manoeuvre. Ann Surg.
242:651–654. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Lai PB, Wong J, Ng WW, Lee WL, Cheung YS,
Tsang YY and Lee KF: Safe modification of the liver-hanging
manoeuvre by endoscopic-assisted dissection of the retrohepatic
tunnel. Surg Today. 37:915–917. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Meng WC, Shao CX, Mak KL, Lau PY, Yeung YP
and Yip AW: Anatomical justification of Belghiti's ‘liver hanging
manoeuvre’ in right hepatectomy with anterior approach. ANZ J Surg.
73:407–409. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Aydin U, Yazici P, Zeytunlu M, Kilic M and
Coker A: Bimanual ‘bi-finger’ liver hanging manoeuvre: An
alternative and safe technique for liver hanging. HPB (Oxford).
9:195–198. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Chen XP, Zhang WG, Lau WY and Qiu FZ:
Right hepatectomy using the liver double-hanging manoeuvre through
the retrohepatic avascular tunnel on the right of the inferior vena
cava. Surgery. 144:830–833. 2008. View Article : Google Scholar : PubMed/NCBI
|