Introduction
Renal angiomyolipoma (RAML) is a type of benign
hamartoma that may occur sporadically or be associated with
tuberous sclerosis complex (TSC) (1–3). It has
been reported that the number of sporadic angiomyolipomas is four
times that of the cases associated with TSC (3,4).
Generally, ~80% of patients with TSC have hamartoma. However, RAML
associated with TSC comprises only 0.3% of all renal neoplasms
(5). In short, RAML is common in
patients with TSC, but rare in the general population (2). Notably, TSC-associated RAMLs are
typically bilateral and multifocal, larger, and more likely to lead
to potentially life-threatening hemorrhage compared with isolated
RAML (1).
TSC is a rare autosomal dominant disease with
incomplete penetrance; it is characterized by a constellation of
findings affecting multiple organ systems, and has a worldwide
prevalence of ~1/6,000 to 1/12,000 individuals (2,6–8). According to the relevant literature,
TSC may be associated with glial tumors, adenoma sebaceum,
rhabdomyoma and hamartomatous tumors of the thyroid, retina, liver,
pancreas, lung, kidney, adrenals and ovaries. The clinical
manifestations of TSC depend on the target organs, such as the
brain, skin, kidneys, lungs and heart, or the organs that are
oppressed by the expansion of the lesions (3,9,10).
The present study reports two cases of
TSC-associated RAML.
Case reports
Case one
A 31-year-old woman with a chief complaint of left
flank pain and abdominal pain of three months duration was admitted
to Peking University Shenzhen Hospital (Shenzhen, China) in March
2016. Laboratory examinations yielded the following results: Red
blood cell (RBC) count, 3.59×1012/l (normal range,
4.0–5.5×1012/l); and hemoglobin (HGB) level, 111 g/l
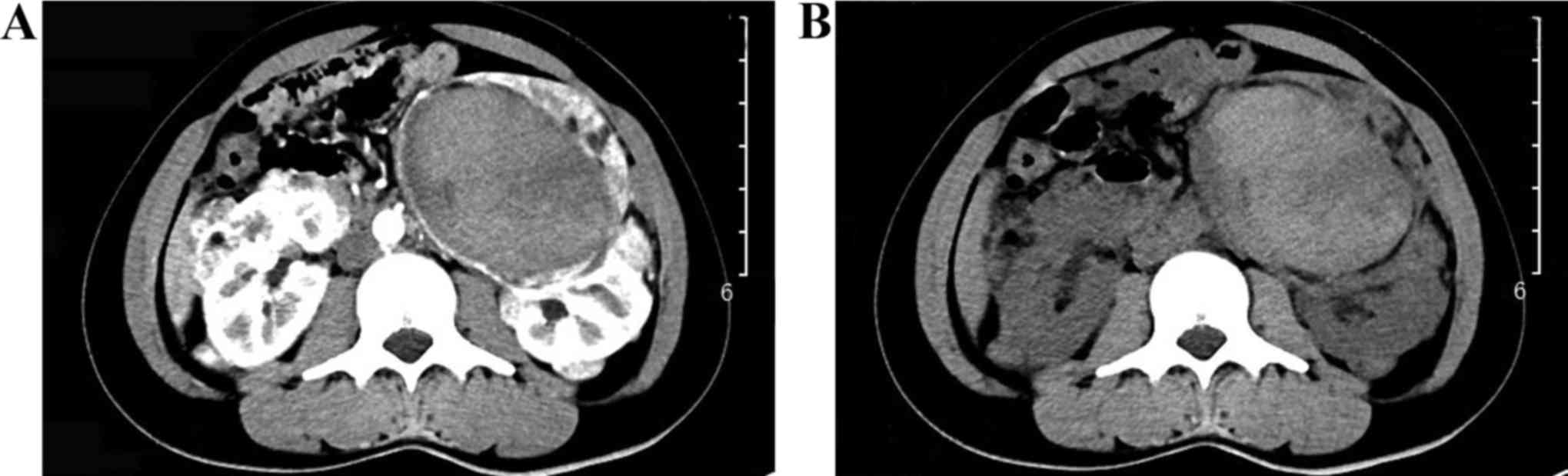
(normal range, 120–160 g/l). Subsequently, a contrast-enhanced
computed tomography (CE-CT) scan indicated bilateral multiple renal
masses with a large hematoma in the left kidney (Fig. 1A), and no enhancement (Fig. 1B). Additionally, magnetic resonance
imaging (MRI) of the brain was performed, revealing multiple
swellings of the cortex, with increased signal intensity in the
left temporal lobe, parietal lobe, occipital lobe, and two frontal
lobes, and a small focal ischemia in the right basal ganglion
(Fig. 2). The patient was diagnosed
with bilateral RAMLs and spontaneous rupture of the left RAML with
TSC, which was temporarily managed conservatively without further
intervention, as the hemorrhage was controlled by the use of
hemostatic drugs; therefore, selective arterial embolization was
not performed.
In May 2016, the patient returned to hospital for
further treatment. The results of laboratory examinations were as
follows: RBC count, 3.77×1012/l; and HGB level, 113 g/l.
In addition, physical examination revealed tenderness and pain on
percussion pain over the region of the left kidney. Abdominal
palpation revealed a giant mass with tenderness in the left
quadrant. Prior to the planned partial nephrectomy, ultrasonography
of the urinary system was performed, which revealed bilateral
multiple solid lesions; among these masses, the largest one was
~8.75×7.95 cm and located in the left kidney. A further CE-CT scan
of the abdomen revealed bilateral multiple renal masses with a
massive hematoma in the left kidney (Fig. 3A), with no enhancement (Fig. 3B).
Following the diagnosis of left-sided RAML with TSC,
it was determined that the patient required surgical treatment, and
a left partial nephrectomy was planned as the tumor size was >4
cm, in line with the surgical indications. However, during the
surgery, the residual kidney tissue was found to be insufficient;
therefore, rather than suturing the kidney to retain the residual
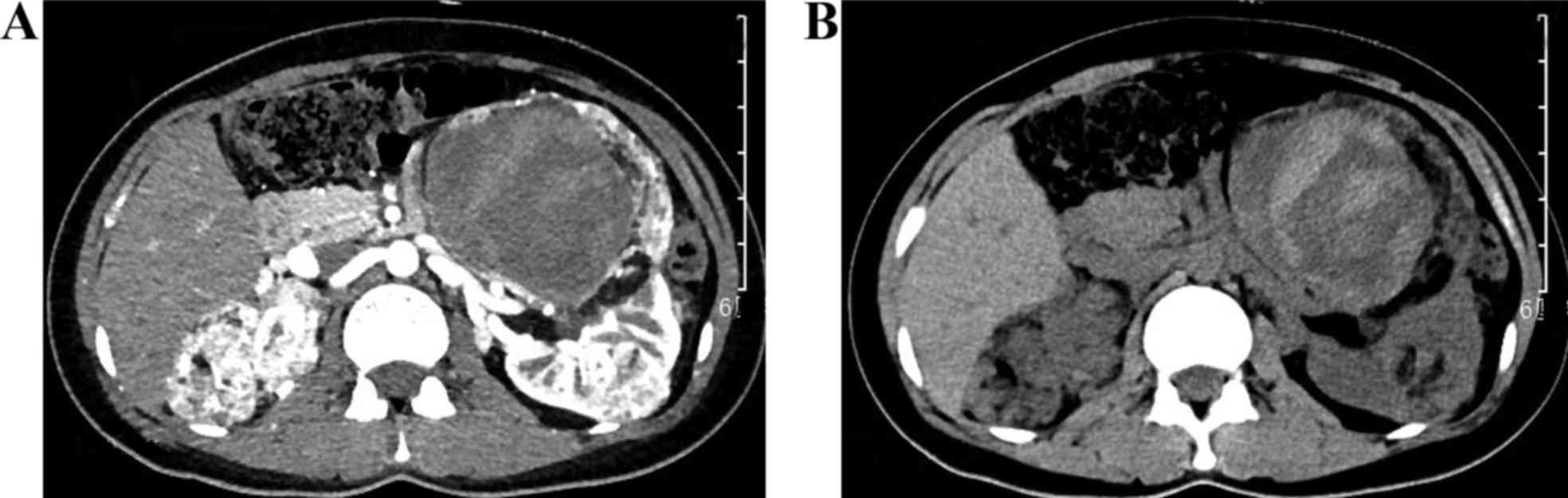
tissue, a total nephrectomy was carried out. Histological
examination indicated a left RAML composed of well-differentiated
vessels, smooth muscle and adipose tissue (Fig. 4). To date, the patient has been
followed up for ~1 year post-surgery. The patient recovered well,
and no postoperative complications were observed. Urinary
ultrasound every 6 months was suggested as follow-up over the next
few years.
Case two
In June 2016, a 45-year-old man presented to the
Emergency Department of Peking University Shenzhen Hospital with
sudden-onset abdominal pain, hematuria and proteinuria. The patient
had a history of left lumbar pain of 9 years duration, and his son
had previously been diagnosed with bilateral multiple RAML.
Laboratory examinations were performed, yielding the following
results: RBC count, 4.57×1012/l; HGB level, 132 g/l;
white blood cell count, 12.84×109/l (normal range,
4–10×109/l); neutrophilic granulocyte percentage, 82.7%
(normal range, 50–70%); urine protein, 2+ (normal, -); urine occult
blood, 2+ (normal, -). Emergency ultrasonography was performed,
revealing bilateral multiple renal lesions, prompting suspicion for
RAML. Among the masses revealed by ultrasound, the largest measured
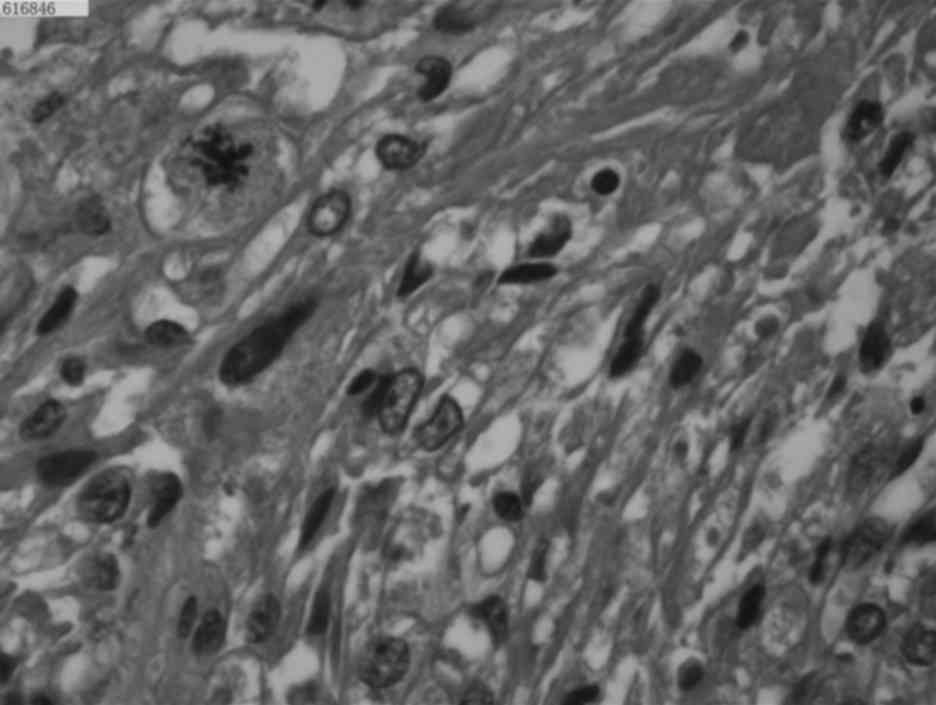
~11.1×8.6 cm and was located in the left kidney. Additionally, a
CE-CT scan of the abdomen and pelvis was carried out, which showed
bilateral renal masses in both kidneys (Fig. 5A), with perinephric and subcapsular
hematoma secondary to rupture of the left-sided RAML (Fig. 5C). No enhancement was observed
(Fig. 5B and D).
The patient was transferred to the Department of
Urology for treatment of a spontaneous retroperitoneal hemorrhage.
According to the chief complaint, laboratory examination results,
imaging findings and family history of bilateral multiple RAML, the
patient was diagnosed with TSC-associated RAML. The patient's
condition was managed with conservative treatment, comprising
analgesia, hemostasis and fluid infusion; selective arterial
embolization was not performed at the time of hospitalization as
the hemorrhage had been under control. Partial nephrectomy was
planned for 3 months later as the tumor size of ~10 cm was in line
with the surgical indications. The patient was followed up for ~1
year. Although a partial nephrectomy was suggested, the patient
insisted on conservative treatment, such as use of hemostatic
drugs. To date, the patient has only complained of mild flank pain,
and no abnormal laboratory examination results have been noted.
Partial nephrectomy is still recommended for this patient as it is
expected to have a positive effect on preventing rupture of the
tumor.
Discussion
RAMLs are benign hamartomas that are histologically
composed of blood vessels, smooth muscle and adipose tissues in
variable proportions (1–3,11). For
angiomyolipomas in general, ~80% of cases occur sporadically and
20% of cases occur in patients with TSC (1). Overall, the number of sporadic RAMLs is
four times that of the cases of TSC-associated RAML (3). Furthermore, TSC-associated RAMLs are
more likely to be large, multifocal, and complicated by flank pain,
abdominal pain, retroperitoneal hemorrhage or hematuria (1–3,6,11,12).
TSC-associated RAMLs have a greater risk of hemorrhage compared
with sporadic RAMLs (12–14).
As described, TSC-associated RAML is an unusual
lesion that behaves like a benign tumor. At present, few cases have
been reported that illustrate the potential for life-threatening
hemorrhage due to spontaneous rupture of the RAML in patients with
TSC; this hemorrhage may occur because, along with the growth of
the tumor, the increased blood supply can result in angiectasis and
enlargement of arterial aneurysms (11,12).
Additionally, multifocal lesions associated with TSC grow rapidly
and are more likely to rupture if their size exceeds 4 cm (2,5,11). Thus, patients with lesions measuring
>4 cm require proper intervention at the appropriate time in
order to avoid the primary complications of retroperitoneal
hemorrhage, as the risk of hemorrhage is critical in such
patients.
The treatment strategy predominantly depends on the
size of the lesion and the presence of symptoms. Surgical treatment
for RAML is considered the optimal approach if complications occur,
if the size of the tumor reaches 4 cm, or if renal malignancy is
suspected. Generally, the indications for intervention include
acute hemorrhage and pain, or size >4 cm even when asymptomatic
(2,6,8,11).
For the two patients described in the current
report, rupture of RAML occurred, and the patients presented with
flank pain, abdominal pain, hemorrhage and large neoplasms.
Typically, the first choice for treatment should be selective
embolization. However, in the present cases, hemorrhage was
controlled due to the use of hemostatic drugs, so selective
arterial embolization was not immediately performed. During the
following three months, the two patients complained of only mild
flank pain, and had no abnormal laboratory examination results, so
selective arterial embolization was still not performed.
Eventually, in the fourth month, when bleeding was under control,
the tumor size in each case (respectively ~8 and ~10 cm) was in
line with the indications for surgery, and surgery was therefore
considered. In addition to the typical clinical symptoms, surgical
treatment was deemed necessary in the two cases as this is the most
effective way to avoid recurrences of tumor rupture and
retroperitoneal hemorrhage. Partial nephrectomy was the primary
surgical option.
In conclusion, the present case report highlights
two important aspects for clinicians. First, in order to avoid
potentially life-threatening hemorrhage, the spontaneous rupture of
RAML in patients with TSC requires timely and proper intervention
by hemostatic drugs or selective arterial embolization. Second,
tumors >4 cm should be resected to avoid the primary
complications of retroperitoneal hemorrhage. It is clear that early
detection and diagnosis of the disease can reduce the occurrence of
serious complications. In order to ensure timely and proper
treatment, urologists should be conscious of the risk of
hemorrhage.
Acknowledgements
The present study was supported by the National
Natural Science Foundation of China (grant no. 81101922), Science
and Technology Development Fund Project of Shenzhen (grant nos.
JCYJ20130402114702124 and JCYJ20150403091443329), the fund of
‘San-ming’ project of medicine in Shenzhen and the fund of
Guangdong Key Medical Subject.
References
|
1
|
Parekh S, Jolapara M, Shah T and Rajpura
H: Emergency embolization of actively bleeding renal angiomyolipoma
in a patient of tuberous sclerosis. Ren Fail. 36:1114–1118. 2014.
View Article : Google Scholar
|
|
2
|
Azim A and Rajkumar G: Renal
angiomyolipomas in tuberous sclerosis-rare but potentially
life-threatening lesions. BMJ Case Rep. 2012:pii: bcr2012007720.
2012. View Article : Google Scholar
|
|
3
|
Redkar N, Patil MA, Dhakate T and Kolhe P:
Tuberous sclerosis complex presenting as bilateral large renal
angiomyolipomas. BMJ Case Rep. 2012:pii: bcr2012006412. 2012.
View Article : Google Scholar
|
|
4
|
Kushwaha R, Dhawan I, Arora R, Gupta K and
Dhupia JS: Multifocal renal angiomyolipoma presenting as massive
intraabdominal hemorrhage. Indian J Pathol Microbiol. 53:340–341.
2010. View Article : Google Scholar
|
|
5
|
Moratalla MB: Wunderlich's syndrome due to
spontaneous rupture of large bilateral angiomyolipomas. Emerg Med
J. 26:722009. View Article : Google Scholar
|
|
6
|
Sukumar S, Nair Balagopal T, Saheed
Mohammed CS and Bhat Sanjay H: Bilateral nephron sparing surgeries
for multiple renal angiomyolipomas in Bourneville's disease. Int
Urol Nephrol. 39:389–391. 2007. View Article : Google Scholar
|
|
7
|
Sarraf M, Masoumi A, Castro-Silva FJ,
Myers JB, Wilson SS and Schrier RW: A case of tuberous sclerosis
complex that progressed to end-stage renal disease. Nat Clin Pract
Nephrol. 5:172–176. 2009. View Article : Google Scholar
|
|
8
|
Wong IY and Shortliffe LD: The management
of renal angiomyolipomas in a patient with tuberous sclerosis. Nat
Clin Pract Urol. 6:168–172. 2009. View Article : Google Scholar
|
|
9
|
Siroky BJ, Yin H and Bissler JJ: Clinical
and molecular insights into tuberous sclerosis complex renal
disease. Pediatr Nephrol. 26:839–852. 2011. View Article : Google Scholar
|
|
10
|
Dixon BP, Hulbert JC and Bissler JJ:
Tuberous sclerosis complex renal disease. Nephron Exp Nephrol.
118:e15–e20. 2011. View Article : Google Scholar
|
|
11
|
Shen WH, Pan JH, Yan JN, Chen ZW, Zhou ZS,
Lu GS and Li WB: Resection of a giant renal angiomyolipoma in a
solitary kidney with preoperative arterial embolization. Chin Med J
(Engl). 124:1435–1437. 2011.
|
|
12
|
Granata A, Basile A, Figuera M, Mignani R
and Fiore CE: Spontaneous retroperitoneal hemorrhage due to massive
rupture of renal angiomyolipoma treated with nephrectomy: An
unusual onset of tuberous sclerosis complex. Clin Nephrol.
71:441–444. 2009. View
Article : Google Scholar
|
|
13
|
Sparks D, Chase D, Thomas D and Arnott J:
The Wunderlich's syndrome secondary to massive bilateral
angiomyolipomas associated with advanced tuberous sclerosis. Saudi
J Kidney Dis Transpl. 22:534–537. 2011.
|
|
14
|
Taviloglu K, Yanar H, Dilege E, Poyanli A,
Zorba O, Ertekin C, Guloglu R and Dursun M: Non-traumatic kidney
rupture in a tuberosclerosis patient with renal angiomyolipomas.
Intern Med J. 37:504–505. 2007. View Article : Google Scholar
|