Introduction
The treatment of high-grade serous ovarian cancer
(HGSOC) is complicated by the fact that it is usually in an
advanced stage at the time of diagnosis. HGSOC accounts for 70–80%
of ovarian cancer deaths, and overall survival has not changed
significantly despite advances in therapy (www.seer.cancer.gov). HGSOC is distinctive in that it
shows an initial favourable response to platinum-based chemotherapy
(1). This response is probably
related to a high rate of defects in the homologous recombination
(HR) DNA repair pathway, mainly due to mutations in BRCA1 and
BRCA2. Tumours with mutations in other components of the HR pathway
(BRCAness phenotype) have the same likelihood of response to
alkylating agents (2).
Regardless of extensive surgery and chemotherapy,
over 80% of HGSOC patients relapse and require additional therapy.
Metronomic oral cyclophosphamide has gained increasing interest in
recent years as a promising maintenance therapy in advanced HGSOC
after response to platinum based chemotherapy (3). It may cause long-term response in an
outpatient setting with a low toxicity profile.
In the current study we present an exceptional
responder: a patient with metastasized HGSOC who underwent
different types of treatment modalities, including several episodes
of platinum-based chemotherapy, and who after 13 years went into
complete remission on low-dose and continuous oral cyclophosphamide
alone. We discuss the possible underlying mechanism of this
treatment with metronomic cyclophosphamide and the potential
advantages compared to newer regimens.
Case report
In December 2003, a 47-year-old woman presented with
obstipation, abdominal pain and a palpable mass in the lower right
abdomen. The relevant previous medical history consisted of
diabetes mellitus type I. She had no family history of breast or
ovarian cancer. Ultrasound showed a solid and cystic mass of
14×14×8 cm and a CA-125 level of 5.659 kU/l. Exploratory laparotomy
revealed a large mass with multiple peritoneal depositions.
Subsequently, the patient underwent a bilateral ovariectomy,
hysterectomy, omentectomy and resection of the rectosigmoid with
closure of the rectal stump and formation of an end colostomy
(Hartmann procedure). Macroscopic residual mass remained on the
left iliacal external vein, and microscopic pathology demonstrated
a high-grade papillary serous adenocarcinoma. A CT scan evaluation,
performed before starting additional chemotherapy, revealed a mass
between the liver and the right kidney, and presacral and
para-aortal lymph node metastases. Six cycles of platinum-based
chemotherapy, administered in accordance with the AGO-OVAR study
(4), resulted in a partial response.
This regimen was followed by a second debulking operation, reversal
of the colostomy and another 3 cycles of chemotherapy. The patient
had intra-abdominal recurrences in October 2005, in May 2007 and in
February 2008, which were successfully treated with chemotherapy,
consecutive paclitaxel and carboplatin, liposomal doxorubicin and
further combinations of paclitaxel and carboplatin. In 2009, a
recurrence at the lower part of the vagina was diagnosed. This was
surgically removed and followed by radiotherapy. In 2011, a
solitary liver metastasis was treated with radiofrequency ablation
(RFA) and four cycles of cisplatin and etoposide. In August 2012, a
tumour mass in the abdominal scar resulting from the RFA needle
insertion was treated with radiotherapy, and at reoccurrence in May
2013, the tumour was resected. Tumour tissue at the next
intra-abdominal reappearance in August 2014 was proven to be
oestrogen receptor positive, and treatment was started with the
aromatase inhibitor letrozole. Within several weeks, a slow
biochemical progression could be observed. Several treatment
options were considered.
At that time, treatment with PARP inhibitors only
occurred in clinical trials. Independent revision of microscopic
pathology confirmed the high-grade papillary serous adenocarcinoma.
The patient was invited to participate in a trial with olaparib but
waived this option. Molecular mapping by then revealed no
BRCA1 and BRCA2 gene mutations. Considering the
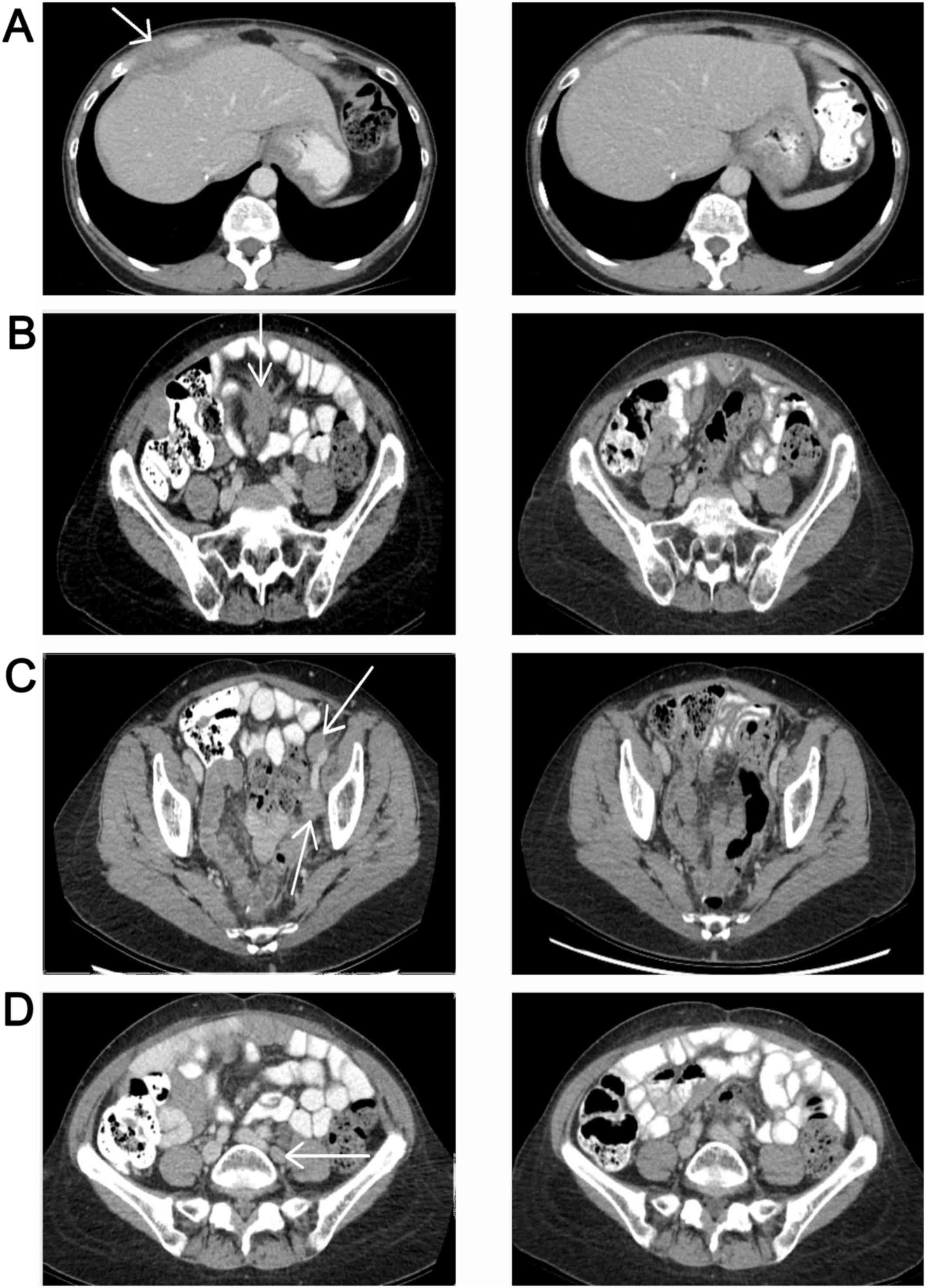
solitary reccurrence, radiotherapy was started. In July 2015, a CT
scan revealed new lymph node metastases and a 4-cm mass ventral of
and connected to the right liver lobe (Fig. 1; left side). Although the patient had
previously responded well to platinum-based (alkylating)
chemotherapy, at this stage, several courses of neurotoxic
chemotherapy and the pre-existing diabetes had caused significant
neuropathy and retinopathy, which diminished her vision. Treatment
with bevacizumab was therefore not an option. Otherwise, the
clinical condition was excellent. In the Netherlands, bevacizumab
is indicated only in first line treatment, at first recurrence of
platinum sensitive ovarian cancer in combination with carboplatin
and paclitaxel, or at recurrent platinum resistant ovarian cancer.
Therefore, treatment with bevacizumab was no option. In addition,
bevacizumab is contraindicated in this patient because of
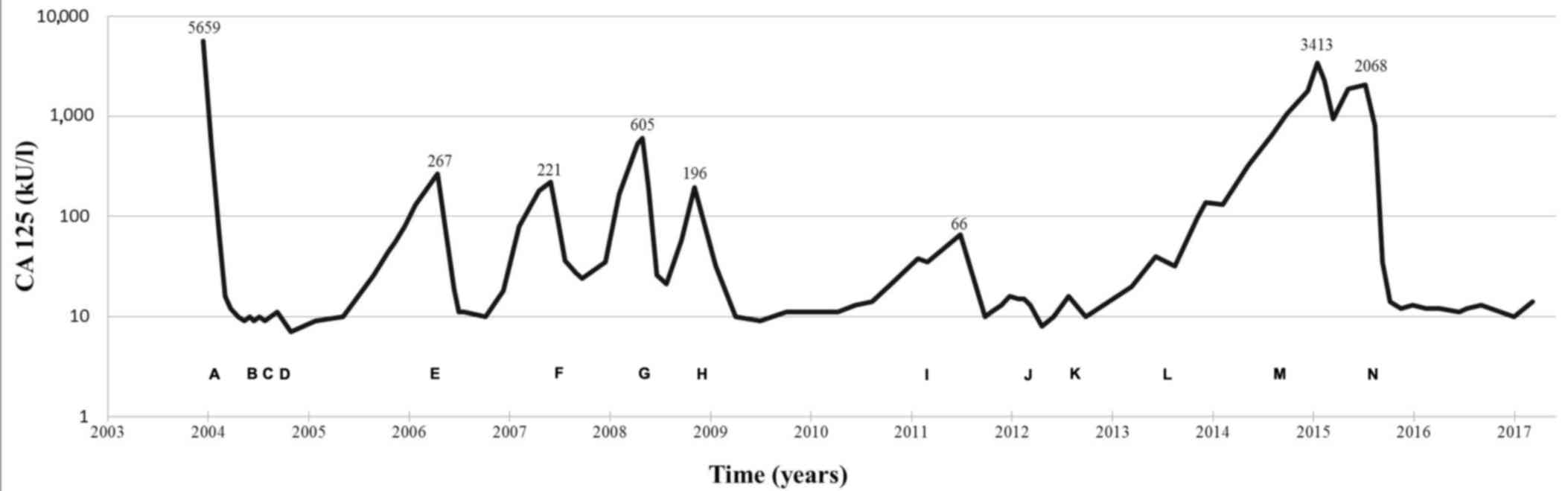
preexistent neuropathy. In July 2015, treatment with continuous
low-dose oral cyclophosphamide (100 mg daily) was started and
resulted in a complete remission of tumour load within 3 months. In
May 2017, 22 months after the start of this treatment, the patient
was still without any signs of cancer activity: CT-scan in January
2016 was negative (Fig. 1; right
side), ultrasound in March 2017 was negative and tumour marker
CA-125 had normalised (Fig. 2
clarifies the dose and cycles of chemotherapy and other
interventions). Thus far, reports of cyclophosphamide-related
toxicity have been limited to grade 1 fatigue, without signs of
myelosuppression or physical discomfort. Treatment was interrupted
once for several weeks, but this was not clinically relevant.
Lately, several dose reductions were applied (50 mg p.o.) on the
patient's request, partly due to her general aversion to drugs, as
well as the drug-related toxicity symptoms (grade 1 fatigue). The
patient is to proceed to treatment with cyclophosphamide until
progressive disease or unacceptable toxicity.
Discussion
This case study presents a patient with metastasized
HGSOC who underwent different types of treatment modalities,
including several episodes of platinum-based chemotherapy, and who
after 13 years went in a complete remission on low-dose and
continuous oral cyclophosphamide alone. Cyclophosphamide, a
mustard-alkylating agent, is one of the most important, the eldest
and the most effective alkylating cytostatic (5). Metronomic treatment with
cyclophosphamide consists of frequent, usually daily,
administration of a low (oral) dose of cyclophosphamide without
prolonged drug-free breaks. The efficacy of metronomic
cyclophosphamide can be explained by an anti-angiogenic effect that
continuously inhibits the endothelial cells that attempts to
restore the vascular status of the tumour. Furthermore, previous
studies described a direct effect on the induction of tumour stem
cell differentiation, which can cause a selective reduction in
circulating regulatory T cells. This reduction also leads to a
suppression of conventional T cells and natural killer cells, with
restoration of peripheral T-cell proliferation and innate killing
activities (6–8). As the dose in metronomic treatment is
far below the maximum tolerated dose (MTD), it causes fewer side
effects. This strategy can benefit patients suffering from types of
cancer known to be sensitive to alkylating agents, such as
lymphomas, breast cancer and ovarian cancer (9).
In recent years, several publications have
underlined the advantage of this regimen for patients with
recurrent HGSOC (10–12). Moreover, Kummar et al
demonstrated in a small randomized trial of oral cyclophosphamide
with or without velaparib (a PARP inhibitor) that low-dose
cyclophosphamide is associated with responses and prolonged disease
stabilization in pre-treated HGSOCs (11). There was a 19,4% (7/36 patients)
overall response in the cyclophosphamide-only arm. In this arm,
four of the patients who responded had BRCA-mutant ovarian cancer
(including the patient who had a CR) and two had HGSOC. Notably,
the addition of velaparib to cyclophosphamide did not increase the
response rate (overall response of 11,8%, 4/34 patients). Major
restrictions of this study are the relatively small group of
patients and a low dose of velaparib. The efficacy of olaparib,
another PARP inhibitor, in ovarium cancer is undisputed (13). It would be interesting to compare the
efficacy of metronomic cyclophosphamide and PARP inhibitors in this
group of patients. Unfortunately, large randomized studies of
metronomic cyclophosphamide versus PARP inhibitors are lacking.
Alternative treatment options for patients with
HGSOC include liposomal doxorubicin, gemcitabine and topotecan.
However, those do not contribute to a long-term remission and are
associated with significant toxicities (14,15).
More recently, additional compounds have become available. Firstly,
the combination of bevacizumab (a monoclonal antibody against VEGF)
with chemotherapy has been approved in the Netherlands (16). Secondly, PARP inhibitors are
indicated for patients with a defect in the homologue recombinant
(HR) DNA repair pathway, which is present in 51% of HGSOCs
(17). These HR defects make HGSOC
sensitive to alkylating chemotherapy, e.g., platinum compounds and
cyclophosphamide, and other DNA-damaging agents, such as PARP
inhibitors (18,19). Notably, a benefit of PARP inhibitors
has also been reported in non-BRCA-mutant tumours, suggesting that
the indication for these agents may be expanded (19). Nevertheless, PARP inhibitors have
three main disadvantages. Firstly, recent studies demonstrated that
HGSOCs become resistant to PARP inhibitors (11). Secondly, PARP inhibitors as well as
bevacizumab combined with chemotherapy may cause significant side
effects (15,16,19). By
contrast, low-dose cyclophosphamide is well tolerated (20,21). The
main known toxicities, such as cytopenia, haemorrhagic cystitis or
cardiac toxicity, occur when using high-dose cyclophosphamide.
Low-dose cyclophosphamide, however, may cause some degree of
leukopenia (7). Lastly, the costs of
oral metronomic cyclophosphamide treatment are significantly lower
than the costs of administering intravenous cytotoxic drugs or
novel treatments such as PARP inhibitors. In this context, it
should be noted that in most countries treatment strategies for
HGSOCs do no longer routinely include cyclophosphamide (intravenous
or oral).
The main limitation of a case report is that its
findings cannot be generalized. However, exceptional responders may
provide insights into the contribution of factors that are
important for therapy response and long-term survival. We here
presented an exceptional responder and described the advantages of
metronomic cyclophosphamide. Further research should be undertaken
to compare the efficacy, toxicity and cost- effectiveness of
metronomic cyclophosphamide and newer agents such as PARP
inhibitors in HGSOC ovarian cancer. Although the ovarian cancer in
this case does not have BRCA1 or BRCA2 mutation, the genomic
profile of this tumour shows BRCAness (on the basis of classifiers
developed and validated in mamma carcinoma, as there are no
classifiers developed and validated in ovarian cancer), class 4
pathogenic variation in TP53 and class 5 pathogenic variation in
GNAS. There was no mutation in ATM. We are aware that NBS1, RAD51,
BARD1, GAPDH and other damage response genes can also be tested. In
retrospect, it would be interesting to examine these other damage
response genes, as has been pointed out by Lee et al
(22), particular as exposition of
some of these genes is associated with aggressive parameters in
epithelial ovarian cancers. However, these were not available
during molecular tumor analysis at that time. Genomic profiling of
tumours also is an interesting and possible important part of
future possibilities to predict therapy response.
We here presented an exceptional responder: a
patient with metastasized HGSOC, who underwent different types of
treatment modalities, including several episodes of platinum-based
chemotherapy. She eventually, after 13 years of disease, went in
complete remission on low-dose and continuous oral cyclophosphamide
alone. In our opinion, this case may serve as a reminder that old
drugs can be used successfully even in the age of targeted therapy
and molecularly designed drugs. Metronomic cyclophosphamide can be
considered first instead of PARP inhibitors in patients with HGSOC
who responded to platinum-based chemotherapy and cannot continue
platinum-based chemotherapy because of toxicity, independent of
BRCA mutation or BRCA-ness tumour profile. Metronomic
cyclophosphamide has several advantages, which include effective
reduction of tumour activity, oral administration, good
tolerability and low cost. Further research should be undertaken to
compare the efficacy, toxicity and cost- effectiveness of
metronomic cyclophosphamide and newer agents, such as PARP
inhibitors, in HGSOC ovarian cancer.
References
|
1
|
Bowtell DD, Böhm S, Ahmed AA, Aspuria PJ,
Bast RC Jr, Beral V, Berek JS, Birrer MJ, Blagden S, Bookman MA, et
al: Rethinking ovarian cancer II: Reducing mortality from
high-grade serous ovarian cancer. Nat Rev Cancer. 15:668–679. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Liu G, Yang D, Sun Y, Shmulevich I, Xue F,
Sood AK and Zhang W: Differing clinical impact of BRCA1 and BRCA2
mutations in serous ovarian cancer. Pharmacogenomics. 13:1523–1535.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Ferrandina G, Corrado G, Mscilini F,
Malaguti P, Samaritani R, Distefano M, Masciullo V, Di Legge A,
Saveresse A and Scambia G: Metronomic oral cyclophosphamide (MOC)
in the salvage therapy of heavily treated recurrent ovarian cancer
patients: A retrospective, multicenter study. BMC Cancer.
14:9472014. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Du Bois A, Belau A, Wagner U, Pfisterer J,
Schmalfeldt B, Richter B, Staehle A, Jackisch C, Lueck HJ,
Schroeder W, et al: A phase II study of paclitaxel, carboplatin,
and gemcitabine in previously untreated patients with epithelial
ovarian cancer FIGO stage IC-IV (AGO-OVAR protocol OVAR-8). Gynecol
Oncol. 96:444–451. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Penel N, Adenis A and Bocci G:
Cyclophosphamide-based metronomic chemotherapy: 10 years of
experience, where do we stand and where are we going? Crit Rev
Oncol Hematol. 82:40–50. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Kerbel RS and Kamen BA: The
anti-angiogenic basis of metronomic chemotherapy. Nat Rev Cancer.
4:423–436. 2004. View
Article : Google Scholar : PubMed/NCBI
|
|
7
|
Madondo MT, Quinn M and Plebanski M: Low
dose cyclophosphamide: Mechanisms of T cell modulation. Cancer
Treat Rev. 42:3–9. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
André N, Carré M and Pasquier E:
Metronomics: Towards personalized chemotherapy? Nat Rev Clin Oncol.
11:413–431. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Scharovsky OG, Mainetti LE and Rozados VR:
Metronomic chemotherapy: Changing the paradigm that more is better.
Curr Oncol. 16:7–15. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Samaritani R, Corrado G, Vizza E and
Sbiroli C: Cyclophosphamide ‘metronomic’ chemotherapy for
palliative treatment of a young patient with advanced epithelial
ovarian cancer. BMC Cancer. 7:652007. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Kummar S, Oza AM, Fleming GF, Sullivan DM,
Gandara DR, Naughton MJ, Villalona-Calero MA, Morgan RJ Jr, Szabo
PM, Youn A, et al: Randomized trial of oral cyclophosphamide and
veliparib in high-grade serous ovarian, primary peritoneal, or
fallopian tube cancers, or BRCA-mutant ovarian cancer. Clin Cancer
Res. 21:1574–1582. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Perroud HA, Scharovsky OG, Rozados VR and
Alasino CM: Clinical response in patients with ovarian cancer
treated with metronomic chemotherapy. Ecancermedicalscience.
11:7232017. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Ledermann J, Harter P, Gourley C,
Friedlander M, Vergote I, Rustign G, Scott C, Meier W,
Shapira-Frommer R, et al: Olaparib maintenance therapy in
platinum-sensitive relapsed ovarian cancer. Engl J Med.
366:1382–1392. 2012. View Article : Google Scholar
|
|
14
|
Gordon AN, Fleagle JT, Guthrie D, Parkin
DE, Gore ME and Lacave AJ: Recurrent epithelial ovarian carcinoma:
A randomized phase III study of pegylated liposomal doxorubicin
versus topotecan. J Clin Oncol. 19:3312–3322. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Pfisterer J, Plante M, Vergote I, du Bois
A, Hirte H, Lacave AJ, Wagner U, Stähle A, Stuart G, Kimmig R, et
al: Gemcitabine plus carboplatin compared with carboplatin in
patients with platinum-sensitive recurrent ovarian cancer: An
intergroup trial of the AGO-OVAR, the NCIC CTG, and the EORTC GCG.
J Clin Oncol. 24:4699–4707. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Aghajanian C, Blank SV, Goff BA, Judson
PL, Teneriello MG, Husain A, Sovak MY, Yi J and Nycum LR: OCEANS: A
randomized, double-blind, placebo-controlled phase III trial of
chemotherapy with or without bevacizumab in patients with
platinum-sensitive recurrent epithelial ovarian, primary
peritoneal, or fallopian tube cancer. J Clin Oncol. 30:2039–2045.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Cancer Genome Atlas Research Network:
Integrated genomic analyses of ovarian carcinoma. Nature.
474:609–615. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Bast RC Jr and Mills GB: Personalizing
therapy for ovarian cancer: BRCAness and beyond. J Clin Oncol.
28:3545–3548. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Mirza MR, Monk BJ, Herrstedt J, Oza AM,
Mahner S, Redondo A, Fabbro M, Ledermann JA, Lorusso D, Vergote I,
et al: Niraparib maintenance therapy in platinum-sensitive,
recurrent ovarian cancer. N Engl J Med. 375:2154–2164. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
El-Husseiny K, Motawei H and Ali MS:
Continuous low-dose oral cyclophosphamide and methotrexate as
maintenance therapy in patients with advanced ovarian carcinoma
after complete clinical response to platinum and paclitaxel
chemotherapy. Int J Gynecol Cancer. 26:437–442. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Ferrandina G, Corrado G, Mascilini F,
Malaguti P, Samaritani R, Distefano M, Masciullo V, Di Legge A,
Saverese A, et al: Metronomic oral cyclophosphamide (MOC) in the
salvage therapy of heavily treated recurrent ovarian cancer
patients: a retrospective, multicenter study. BMC Cancer.
14:9472014. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Lee YK, Park NH and Lee H:
Clinicopathological values of NBS1 and DNA damage response genes in
epithelial ovarian cancers. Exp Mol Med. 47:e1952015. View Article : Google Scholar : PubMed/NCBI
|