|
1
|
Department of Veterans Affairs Laryngeal
Cancer Study Group, . Wolf GT, Fisher SG, Hong WK, Hillman R,
Spaulding M, Laramore GE, Endicott JW, McClatchey K and Henderson
WG: Induction chemotherapy plus radiation compared with surgery
plus radiation in patients with advanced laryngeal cancer. N Engl J
Med. 324:1685–1690. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Lefebvre JL, Chevalier D, Luboinski B,
Kirkpatrick A, Collette L and Sahmoud T: Larynx preservation in
pyriform sinus cancer: Preliminary results of a European
organization for research and treatment of cancer phase III trial.
EORTC Head and Neck Cancer Cooperative Group. J Natl Cancer Inst.
88:890–899. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Posner MR, Hershock DM, Blajman CR,
Mickiewicz E, Winquist E, Gorbounova V, Tjulandin S, Shin DM,
Cullen K, Ervin TJ, et al: Cisplatin and fluorouracil alone or with
docetaxel in head and neck cancer. N Engl J Med. 357:1705–1715.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Vermorken JB, Remenar E, van Herpen C,
Gorlia T, Mesia R, Degardin M, Stewart JS, Jelic S, Betka J, Preiss
JH, et al: Cisplatin, fluorouracil, and docetaxel in unresectable
head and neck cancer. N Engl J Med. 357:1695–1704. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Adelstein DJ, Saxton JP, Rybicki LA,
Esclamado RM, Wood BG, Strome M, Lavertu P, Lorenz RR and Carroll
MA: Multiagent concurrent chemoradiotherapy for locoregionally
advanced squamous cell head and neck cancer: Mature results from a
single institution. J Clin Oncol. 24:1064–1071. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Forastiere AA, Goepfert H, Maor M, Pajak
TF, Weber R, Morrison W, Glisson B, Trotti A, Ridge JA, Chao C, et
al: Concurrent chemotherapy and radiotherapy for organ preservation
in advanced laryngeal cancer. N Engl J Med. 349:2091–2098. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Hanna GJ, Haddad RI and Lorch JH:
Induction chemotherapy for locoregionally advanced head and neck
cancer: Past, present, future? Oncologist. 18:288–293. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Haddad R, O'Neill A, Rabinowits G, Tishler
R, Khuri F, Adkins D, Clark J, Sarlis N, Lorch J, Beitler JJ, et
al: Induction chemotherapy followed by concurrent chemoradiotherapy
(sequential chemoradiotherapy) versus concurrent chemoradiotherapy
alone in locally advanced head and neck cancer (PARADIGM): A
randomised phase 3 trial. Lancet Oncol. 14:257–264. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Hoffman HT, Porter K, Karnell LH, Cooper
JS, Weber RS, Langer CJ, Ang KK, Gay G, Stewart A and Robinson RA:
Laryngeal cancer in the United States: Changes in demographics,
patterns of care, and survival. Laryngoscope. 116 9 Pt 2 Suppl
111:S1–S13. 2006. View Article : Google Scholar
|
|
10
|
Newman JR, Connolly TM, Illing EA, Kilgore
ML, Locher JL and Carroll WR: Survival trends in hypopharyngeal
cancer: A population-based review. Laryngoscope. 125:624–629. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Machtay M, Moughan J, Trotti A, Garden AS,
Weber RS, Cooper JS, Forastiere A and Ang KK: Factors associated
with severe late toxicity after concurrent chemoradiation for
locally advanced head and neck cancer: An RTOG analysis. J Clin
Oncol. 26:3582–3589. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Argiris A, Brockstein BE, Haraf DJ,
Stenson KM, Mittal BB, Kies MS, Rosen FR, Jovanovic B and Vokes EE:
Competing causes of death and second primary tumors in patients
with locoregionally advanced head and neck cancer treated with
chemoradiotherapy. Clin Cancer Res. 10:1956–1962. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Corry J, Peters LJ and Rischin D:
Optimising the therapeutic ratio in head and neck cancer. Lancet
Oncol. 11:287–291. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Kumamoto Y, Masuda M, Kuratomi Y, Toh S,
Shinokuma A, Chujo K, Yamamoto T and Komiyama S: ‘FAR’
chemoradiotherapy improves laryngeal preservation rates in patients
with T2N0 glottic carcinoma. Head Neck. 24:637–642. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Masuda M, Kamizono K, Uryu H, Fujimura A
and Uchi R: Roles of therapeutic selective neck dissection in
multidisciplinary treatment. Journal, 2012Neck Dissection -
Clinical Application and Recent Advances. In Tech; Croatia: pp.
49–60. 2012
|
|
16
|
Hirata K, Horikoshi N, Aiba K, Okazaki M,
Denno R, Sasaki K, Nakano Y, Ishizuka H, Yamada Y, Uno S, et al:
Pharmacokinetic study of S-1, a novel oral fluorouracil antitumor
drug. Clin Cancer Res. 5:2000–2005. 1999.PubMed/NCBI
|
|
17
|
Nonoshita T, Shioyama Y, Nakamura K,
Nakashima T, Ohga S, Yoshitake T, Ohnishi K, Terashima K and Asai
K: Concurrent chemoradiotherapy with S-1 for T2N0 glottic squamous
cell carcinoma. J Radiat Res. 51:481–484. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Ohnishi K, Shioyama Y, Nakamura K,
Nakashima T, Ohga S, Nonoshita T, Yoshitake T, Terashima K, Komune
S and Honda H: Concurrent chemoradiotherapy with S-1 as first-line
treatment for patients with oropharyngeal cancer. J Radiat Res.
52:47–53. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
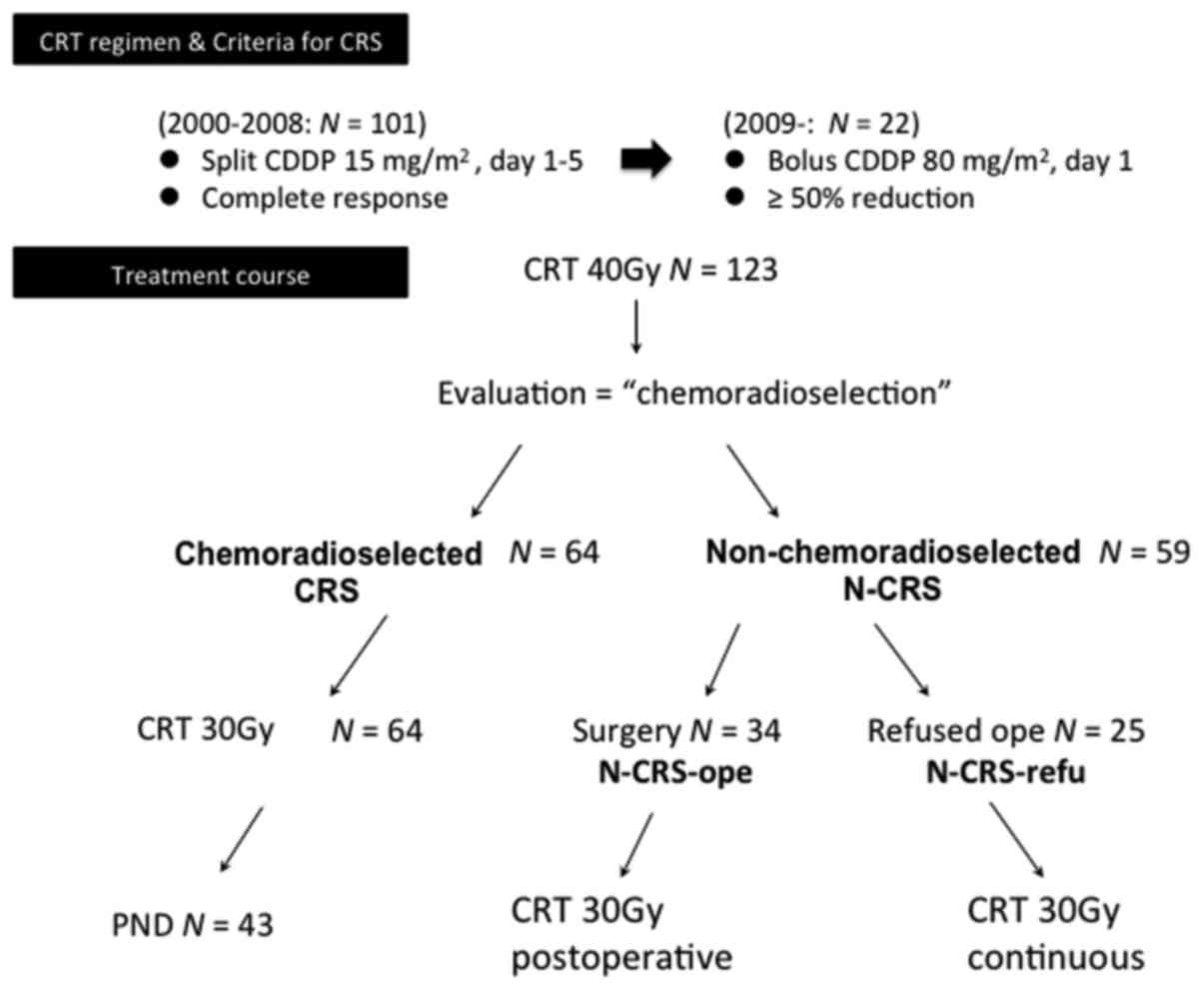
Masuda M, Matsuo M, Aso T, Kiyohara H,
Rikimaru F, Kunitake N and Higaki Y: Utility of algorithm-based
chemoradioselection in the treatment for advanced hypopharyngeal
carcinoma. Head Neck. 37:1290–1296. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Strojan P, Haigentz M Jr, Bradford CR,
Wolf GT, Hartl DM, Langendijk JA, Rinaldo A, Eisbruch A, Mendenhall
WM, Forastiere AA, et al: Chemoradiotherapy vs. total laryngectomy
for primary treatment of advanced laryngeal squamous cell
carcinoma. Oral Oncol. 49:283–286. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Forastiere AA, Weber RS and Trotti A:
Organ preservation for advanced larynx cancer: Issues and outcomes.
J Clin Oncol. 33:3262–3268. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Lefebvre JL and Ang KK: Larynx
Preservation Consensus Panel: Larynx preservation clinical trial
design: Key issues and recommendations-a consensus panel summary.
Int J Radiat Oncol Biol Phys. 73:1293–1303. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Cohen EE, Karrison TG, Kocherginsky M,
Huang CH, Agulnik M, Mittal BB, Yunus F, Samant S, Brockstein B,
Raez LE, et al: DeCIDE: A phase III randomized trial of docetaxel
(D), cisplatin (P), 5-fluorouracil (F) (TPF) induction chemotherapy
(IC) in patients with N2/N3 locally advanced squamous cell
carcinoma of the head and neck (SCCHN). J Clin Oncol. 30
suppl:S55002012.
|
|
24
|
Hitt R, Grau JJ, Lopez-Pousa A,
López-Pousa A, Berrocal A, García-Girón C, Irigoyen A, Sastre J,
Martínez-Trufero J, Castelo Brandariz JA, et al: A randomized phase
III trial comparing induction chemotherapy followed by
chemoradiotherapy versus chemoradiotherapy alone as treatment of
unresectable head and neck cancer. Ann Oncol. 25:216–225. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Blanchard P, Landais C, Petit C, et al:
Meta-analysis of chemotherapy in head and neck cencer (MACH-NC): an
update on 100 randamized traials and 19,248 patients, on behalf of
MANH-HN group. ESMO Meeting abstract. 950O:2016
|
|
26
|
Ang KK: Concurrent radiation chemotherapy
for locally advanced head and neck carcinoma: Are we addressing
burning subjects? J Clin Oncol. 22:4657–4659. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Melotek JM, Cooper BT, Koshy M, Silverman
JS and Spiotto MT: Weekly versus every-three-weeks platinum-based
chemoradiation regimens for head and neck cancer. J Otolaryngol
Head Neck Surg. 45:622016. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Ho KF, Swindell R and Brammer CV: Dose
intensity comparison between weekly and 3-weekly Cisplatin
delivered concurrently with radical radiotherapy for head and neck
cancer: A retrospective comparison from New Cross Hospital,
Wolverhampton, UK. Acta Oncol. 47:1513–1518. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Urba S, Wolf G, Eisbruch A, Worden F, Lee
J, Bradford C, Teknos T, Chepeha D, Prince M, Hogikyan N and Taylor
J: Single-cycle induction chemotherapy selects patients with
advanced laryngeal cancer for combined chemoradiation: A new
treatment paradigm. J Clin Oncol. 24:593–598. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Aso T, Matsuo M, Kiyohara H, Taguchi K,
Rikimaru F, Shimokawa M, Segawa Y, Higaki Y, Umeno H, Nakashima T
and Masuda M: Induction of CD44 variant 9-expressing cancer stem
cells might attenuate the efficacy of chemoradioselection and
Worsens the prognosis of patients with advanced head and neck
cancer. PLoS One. 10:e01165962015. View Article : Google Scholar : PubMed/NCBI
|