Introduction
Surgery is the mainstay of treatment for patients
with colorectal cancer (CRC). Where indicated, chemo- and
radiotherapy are also utilized either pre- or postoperatively and
have improved the outlook of CRC patients. However, despite these
treatments 25–30% of patients undergoing ‘curative’ resection
develop tumor recurrences from unrecognized tumor microfoci and the
majority eventually succumb to the cancer (1,2).
Notably, there is both clinical and small animal evidence that the
surgical trauma associated with resection of the primary tumor may
promote the growth of residual tumor deposits in the weeks
following surgery, making the postoperative period a crucial period
for cancer patients (3–7). The cause(s) of this surgery-associated
tumor stimulation is unclear, however, these effects have been
attributed to the transient immunosuppression attendant to major
surgery as well as the loss of tumor generated inhibitors of
angiogenesis following resection of the primary tumor (8–10). There
is also human evidence, reported during the last decade,
demonstrating that colorectal resection is associated with
proangiogenic plasma protein changes that persist for 3–5 weeks
after surgery.
Plasma levels of the following proangiogenic
proteins have been shown to be persistently increased after
minimally invasive colorectal resection (MICR): Vascular
endothelial growth factor (VEGF), angiopoeitin-2 (Ang-2), placental
growth factor (PIGF), soluble vascular adhesion molecule-1
(sVCAM-1), monocyte chemotactic protein-1 (MCP-1), human chitinase
3-like 1 (Chi3L1), matrix metalloproteinase-3 (MMP-3), and others
(11–16). It has also been shown via in
vitro endothelial cell (EC) culture studies that plasma from
weeks 2 and 3 after MICR significantly stimulates endothelial cells
to proliferate, migrate, and invade when compared to EC culture
results obtained with the same patients preoperative plasma
(12,17); these EC activities are critical to
angiogenesis. It is possible, then, that the long duration
proangiogenic plasma protein elevations may promote angiogenesis in
residual tumor deposits left behind after resection of the primary
tumor.
Interleukin-8 (IL-8), a member of the CXC chemokine
family, is a powerful chemoattractant for neutrophils, basophils
and T cells. IL-8 has also been shown to promote angiogenesis,
tumor growth, and metastasis in several murine models (18). IL-8 is notably upregulated in
colorectal and other cancer types and has been shown to promote
angiogenesis as well as enhance proliferation and survival of tumor
cells through autocrine activation (18–20). In
addition exogenous IL-8 has been shown to stimulate tumor cell
proliferation (21). IL-8 blockade
has been demonstrated to inhibit tumor growth (22). IL-8 also plays a role in and is a
marker of tumor progression and metastatic disease for a wide range
of cancers including gliomas as well as breast and prostate cancers
(23–25). Finally, IL-8 is prominent in
keratinocytes after IHC staining; this presence suggests that it is
a cell migration and chemotactic factor for keratinocytes,
suggesting that IL-8 plays a role in wound healing (26,27).
The effect of minimally invasive colon resection
(MICR) on postoperative (postop) plasma IL-8 levels is unknown. If
IL-8 levels are elevated postop, IL-8 may contribute to the
proangiogenic state of plasma following surgery and may also
directly promote tumor cell growth in patients with residual tumor
post resection. The purpose of this study was to assess plasma
levels of IL-8 in CRC patients during the first 5 weeks following
MICR.
Patients and methods
Study population
CRC patients who underwent elective MICR at Mount
Sinai West Hospital (formerly Roosevelt Hospital) between October
2007 and April 2012 who had been enrolled in an IRB approved
multicenter prospective tissue and data bank were eligible for the
present study. The broadly stated purpose of this tissue banking
effort was to study the physiologic, immunologic, and oncologic
ramifications of major abdominal surgery. Enrolled patients
underwent minimally invasive laparoscopic-assisted or hand assisted
laparoscopic surgery alone and did not receive a novel drug or
other therapy. The indications and type of surgery as well as the
demographic, operative, and short-term recovery data were
prospectively collected for all the patients. Recently transfused
patients, immunosuppressed patients (medication-related and HIV+),
and those who received radio- or chemotherapy within 6 weeks of
surgery were excluded. Patients undergoing urgent or emergent
surgery were, similarly, excluded. Clinical, demographic, and
operative data were obtained from this IRB approved data bank
[Mount Sinai School of Medicine IRB no.: GCO no. 1:16-2619 (0001)]
and the hospital and office charts as well as operative and
pathology records.
Blood sampling and processing
Only those CRC MICR patients for whom adequate
preoperative (preop) and postoperative (postop) plasma specimens
were available were eligible. As per the tissue banking protocol
research dedicated blood samples were obtained preoperatively, on
postoperative days (POD) 1, 3, and, if possible, at one or more
time late point(s) beyond POD 7. Only those patients for whom
adequate volumes of plasma were available for the preop, POD 1, POD
3, and 1 late time point (or more) were enrolled. As post discharge
blood samples were taken at the time of follow-up office visits, it
was not possible to obtain the late specimens on the same
postoperative days, thus it was necessary to ‘bundle’ the late
samples into 7 day time blocks (POD7-13, POD14-20, POD21-27, and
POD 28–34) that were each considered as single time points.
Specimens were collected in heparin-containing tubes, and were
processed within 5–6 h of collection. After centrifugation at 450 ×
g for 10 min, the plasma was frozen and stored at −80°C until the
assays were performed.
IL-8 determination
Plasma IL-8 levels were analyzed in duplicate using
a commercially available enzyme-linked immunoabsorbant assay (R and
D Systems, Minneapolis, MN, USA) according to the manufacturer's
instructions. IL-8 concentrations (pg/ml) were calculated using a
standard curve made for every assay and were reported as mean ± SD
for PreOp vs. PostOp IL-8 comparisons.
Statistical analysis
Demographic and clinical data are expressed as the
mean ± SD for continuous variables. In the analysis of preop vs.
postop IL-8 levels in CRC patients, the Wilcoxon signed rank test
was used for analysis. Comparisons of IL-8 levels of male vs.
female patients, the hand-assisted vs. laparoscopic subgroup and
patients who had postoperative complications vs. patient who had no
post-operative complications were carried out using the Mann
Whitney test. Correlation between postop plasma IL-8 levels and
age, incision size and length of surgery was assessed by the
Spearman's rank correlation coefficient (rs). Data analysis was
performed using SPSS version 15.0 (SPSS, Inc., Chicago, IL,
USA).
Results
A total of 73 CRC patients (36 males, 37 females;
mean age 65.8±12.8 years) who underwent MICR were included in the
study. Of the 73 patients, 45 patients (62%) had colon cancer,
while 28 patients (38%) had rectal malignancies. The majority of
patients underwent laparoscopic-assisted resection (60%), whereas
the remainder (40%) underwent a hand-assisted or hybrid
laparoscopic procedure. The breakdown of operations performed was
as follows: Right colectomy, 31.5%; LAR/anterior resection, 30.1%;
transverse/left colectomy, 16%; sigmoid/rectosigmoid, 12.3%; and
other 11%. The mean incision length was 7.75±3.51 cm and the mean
length of stay was 6.35±2.6 days (Table
I). The final cancer stage breakdown was as follows: Stage I,
27.5%; Stage II, 27.5%; Stage III, 41%; and Stage IV, 4%. Ten
different types of complications were noted (n for each
complication in parentheses): Pleural effusion (n=1), C-Diff
colitis (n=1), ileus (n=8), urinary retention (n=6), urinary tract
infections (n=2), superficial wound infection (n=1), seroma (n=1),
pulmonary hypertension (n=1), tachycardia (n=1), and small bowel
obstruction (n=1). Some patients had more than 1 complication.
There were no perioperative deaths.
 | Table I.Demographic and clinical
characteristics of the plasma IL-8 study population. |
Table I.
Demographic and clinical
characteristics of the plasma IL-8 study population.
| Characteristic | Value (n=73) |
|---|
| Age, years (mean ±
SD) | 65.77±12.73 |
| Sex (n) |
|
| Male | 36 (49.3%) |
|
Female | 37 (50.7%) |
| Incision length, cm
(mean ± SD) | 7.75±3.51 |
| Operative time, min
(mean ± SD) | 302.1±128.3 |
| Length of stay, days
(mean ± SD) | 6.35±2.6 |
| Type of resection
(%) |
|
| Right
colectomy | 23 (31.5) |
|
Transverse colectomy | 6 (8.2) |
| Left
colectomy | 5 (6.8) |
|
Sigmoid/rectosigmoid | 9 (12.3) |
|
LAR/AR | 22 (30.2) |
| APR | 4 (5.5) |
|
Subtotal/total | 4 (5.5) |
| Surgical method
(%) |
|
|
Laparoscopic-assisted | 44 (60.3) |
|
Hand-assisted/hybrid
laparoscopic | 29 (39.7) |
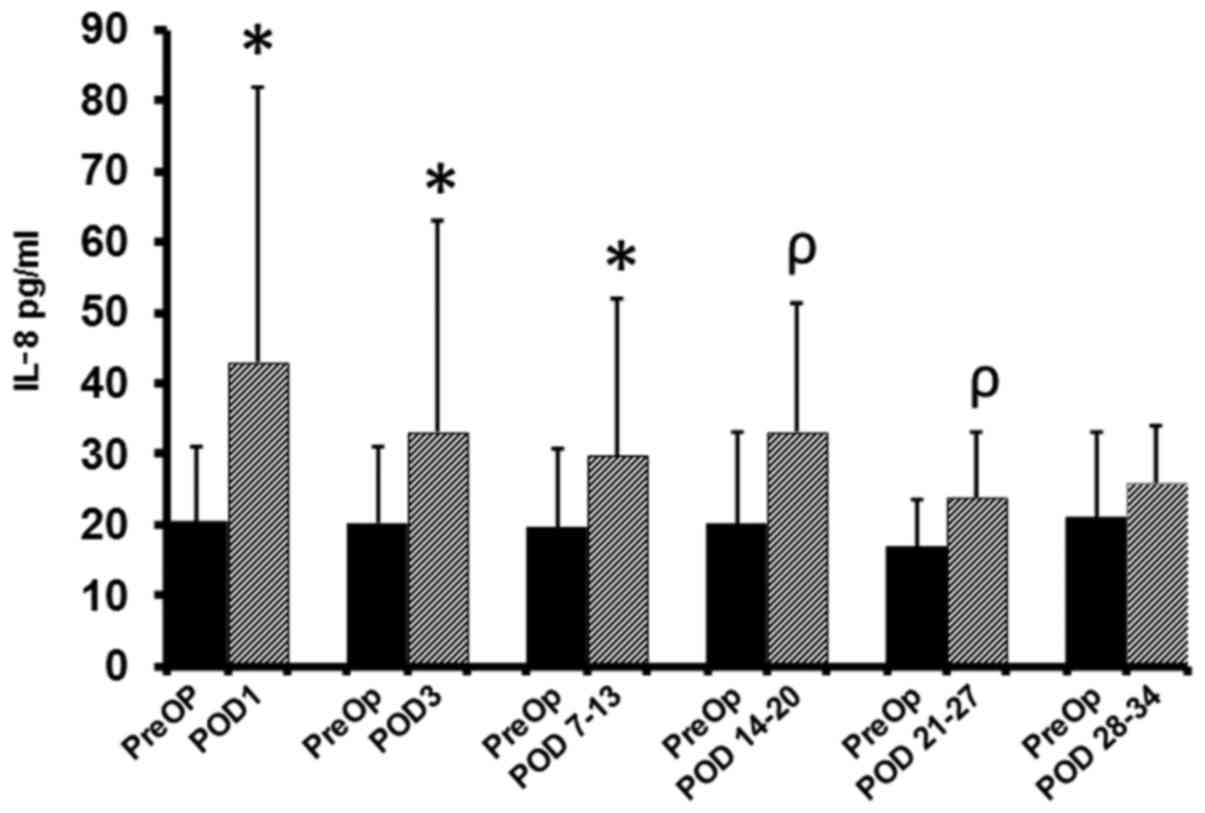
Comparison of preop vs. postop IL-8
plasma levels in CRC patients
The mean preop IL-8 level was 20.4±10.6 pg/ml (n=73)
(Fig. 1). When compared to preop
levels, significant elevations in the mean plasma IL-8 levels
(pg/ml) were identified on POD1 (43.1±38.6; n=72, P<0.0001), POD
3 (33.0±30.1, n=71, P<0.0001), POD7-13 (29.9±21.9, n=50,
P<0.0001), POD14-20 (33.1±18.3, n=24, P=0.002), and for the POD
21–27 (24.0±9.2, n=16, P=0.002). There was no significant
difference in plasma levels noted on POD 28–34 (vs. preop). As the
‘n’ for the POD 1 and later time points was <73 and unique for
each time point, the preop baseline level for each of these time
points was somewhat different. This is reflected in Fig. 1, which provides in bar graph form the
mean preop baseline level for each postop time point. The
percentage increase from baseline at each time point was: POD 1,
111%; POD 3, 63%; POD 7–13, 53%; POD 14–20, 45.0%; POD 21–27, 42%;
and POD 28–34, 24%.
There was no statistically significant correlation
found between age and IL-8 levels preoperatively or at any of the
post-operative time points. Similarly there was no significant
statistical difference found between male and female patients as
regards plasma IL-8 levels preoperatively or at any post-operative
time point. Of note, no significant correlation was found between
cancer stage and preoperative IL-8 plasma levels. To assess whether
incision size (i.e., extent of abdominal wall trauma) correlated
directly with the extent of the IL-8 elevation noted
postoperatively, the hand-assisted laparoscopic subgroup's (n=29,
mean incision length 10.54 cm ± 3.19) mean IL-8 levels at each time
point were compared to the laparoscopic-assisted subgroups results
(n=44, mean incision length 5.63 cm ± 2.29). The hand-assisted
groups mean IL-8 levels were significantly higher than the
laparoscopic-assisted groups results on POD 1 (P=0.02) and 3
(P=0.017), however, there were no significant differences noted for
the POD 7–13, POD 14–20, POD 21–27, and POD 28–34 time points.
As mentioned, there were 23 complications noted in
this patient population. Plasma IL-8 levels of patients who
developed complications were compared to the levels identified in
the larger subgroup which had no complications. As the ‘n’ for all
but 2 of the complications was low, it was not possible to do
individual analyses for each complication, therefore, the patients
with complications were considered together as a group and compared
to the no-complication group. On POD 3 the postoperative IL-8 level
was significantly higher in the sub-group of patients who had
complications vs. the no postoperative complication sub-group (30.5
CI 23.8:75.5; n=14 patients vs. 21.8 CI 18.1:27.9; n=57, P=0.039).
There were no significant differences identified between the
complication group and the no-complication group at the other 4
postop time points, however, the complication groups median IL-8
levels were slightly higher at several of the postop time
points.
Discussion
The vast majority of surgery-related blood protein
alterations are short-lived with a duration of 6 h to 5 days, as is
the case for CRP, IL-6, IL-2, EGF, HGF, IGFBP-3 and others
(28–30). Most of the short duration blood
compositional changes are related to the acute phase inflammatory
response to surgical trauma and anesthesia. The present study
demonstrates that unlike the above proteins, postop plasma IL-8
levels are significantly elevated from the preop baseline for up to
4th weeks after MICR for CRC. Of note, the percentage change from
baseline for the mean plasma IL-8 levels was relatively large,
between 45 and 111%, for the first 4 postop time points assessed
(through the 3rd week following surgery).
As mentioned earlier, over the last decade it has
been found that there is a group of proteins that demonstrate
similar patterns of sustained elevation in plasma levels during the
first month after surgery. Notably, although these proteins each
have numerous actions and effects, all play some role in the
complex process of angiogenesis. IL-8, although better known for
its other effects, has been shown to promote tumor angiogenesis in
murine and in vitro studies (18,19).
Additionally, Li et al showed that MMP-2 and MMP-9
expression in EC's were enhanced by recombinant human IL-8,
suggesting that IL-8 is involved in the degradation of
extracellular matrix which facilitates EC migration, invasion, and
capillary tube organization (31).
Lastly, indirect evidence that IL-8 plays a role in angiogenesis
can be found in experimental data demonstrating that IL-8 confers
resistance to anti-VEGF therapy as regards colon cancer (32). Thus, it is not altogether surprising
that IL-8 joins the group of 7 proteins listed in the introduction
that all exhibit sustained increases during the first month after
surgery. However, what the etiology of the IL-8 increase after
surgery is remains to be determined.
Various types of cancer including colon have been
shown to express IL-8 (CXCR8) and its receptors CXCR1 and CXCR2
(23–25). Although IL-8 levels have been shown
to be elevated in colorectal cancer patients, the tumor, once
removed, cannot account for the postoperative elevation. Since IL-8
plays a role in angiogenesis as well as keratinocyte chemotaxis, it
is possible that the healing surgical wounds may be the source of
the added protein. Both angiogenesis and the attraction of
keratinocytes to a surgical site are critically important to wound
healing and, thus, the levels of IL-8 in the wound may be notably
increased. If this is the case then IL-8 may diffuse from the
wounds into the bloodstream. It is also possible that the etiology
of the IL-8 increase may vary at different postop time points. The
fact that IL-8 levels directly correlated with incision length on
POD 1 and 3 (hand vs. lap. assisted comparison) but not for the
rest of the 1st month after surgery is consistent with there being
a different early mechanism. A likely candidate is the short-lived
acute inflammatory response that occurs after major surgery and has
been shown to directly correlate with incisional length (29,30).
Perhaps after the acute response the healing wounds are the
principal source of the added IL-8 in the blood stream. There is
evidence that the healing wounds may be the source of the long
duration increase in plasma VEGF levels noted after surgery,
mentioned above. Wound levels of VEGF have been found to be much
higher than plasma levels in a variety of surgical patients
(33–35). The authors are currently conducting
several studies investigating plasma and wound levels of the above
listed proteins after MICR and hope to settle this issue.
The possible ramifications of persistently elevated
IL-8 plasma levels after surgery remain to be elucidated. It is
possible that the growth of residual tumor deposits may be
stimulated since IL-8 has been shown to promote tumor growth in
numerous experimental studies (19,20,23). It
is also possible that IL-8, via different mechanisms, may encourage
tumor angiogenesis (18,19). There is EC in vitro cell
culture evidence that plasma from the second and third weeks after
MICR or open surgery for CRC stimulates EC's to proliferate,
migrate, and invade at a significantly higher rate when compared to
results from EC cultures into which the same patients preoperative
plasma was added (12,17). Those results suggest that the net
effect of the sustained elevations of IL-8 and the other
proangiogenic proteins may encourage angiogenesis during the early
postoperative period. It is the authors' hypothesis that tumor
angiogenesis may be stimulated in patients with residual cancer
following surgery.
Direct evidence for this hypothesis is provided by
Peeters et al study of patients with synchronous CRC and
liver metastases that noted that CRC resection (liver lesions left
intact) was associated with an increase in the intra- and
peri-tumoral vascular density of pre-existing liver metastases 6–12
weeks after surgery (36). In
addition, 2 serial PET scan studies of similar patients with
synchronous disease noted that the mean and max SUV values of liver
metastases were significantly increased 6–12 weeks after CRC
resection; of note, in a control group of patients that received no
treatment, SUV values were not appreciably changed (37,10).
Since FDG uptake, reflects, to some extent, tumor vascularity,
these studies indirectly support the above hypothesis. Additional
clinical evidence linking the persistent elevation of IL-8 and the
other proangiogenic proteins to enhanced tumor growth after MICR is
needed before it will be reasonable to conclude that these surgery
related changes have clinical import. If surgery is truly
associated with a period of enhanced tumor growth then it behooves
us to develop anti-cancer treatments that can be given safely to
cancer patients in the perioperative period. Such agents must
inhibit tumor growth but not interfere with wound healing.
Weaknesses of the present study include the
relatively small number of late post-operative plasma samples and
the need to bundle the late samples into 7 day time blocks for the
statistical comparisons. The logistical impossibility of scheduling
outpatient follow-up visits on a particular postoperative day as
well as the fact that most patients returned to the office only
once during the first 3 weeks after surgery are the reasons for the
lower ‘n’s for the late time points and the need to bundle the
specimens. This study concerned only patients who underwent
minimally invasive surgery (either laparoscopic-assisted or
hand-assisted laparoscopic). No patients in this study group had
open CRC surgery. At our center approximately 85% of colorectal
resections are performed using MIS methods. Further research is
planned to evaluate perioperative plasma IL-8 levels of CRC
patients who undergo open colorectal resection once blood samples
for an adequate number of open resection patients are accumulated
in the tissue bank. The final cancer stage for the vast majority
(97%) of the patients included in this study was Stage 1, 2, and 3.
In all of these cases the resections were judged to be R-0
resections, based on pathologic assessment of the specimens. In the
three Stage 4 patients, 2 had liver metastasis and 1 had abdominal
wall metastasis. In these Stage 4 patients the primary tumor was
resected and the resections were judged to be R-0 in all cases. Of
note, in the 3 Stage 4 patients, the residual tumor may express
IL-8 postoperatively and contribute to the postop plasma
elevations. When the 3 Stage 4 patients are excluded, the overall
results are not altered. Further research is required to
investigate plasma IL-8 levels in patients with R-1 resection.
Another weakness is that there is insufficient intermediate and
late oncologic follow-up data for the study population to permit an
assessment of whether the extent of postop IL-8 elevation
correlates with recurrence rates or overall survival.
In summary, the present study has demonstrated that
MICR for CRC is associated with significant elevations in the
plasma concentrations of IL-8 when compared to preoperative
baseline levels. Increased blood levels persisted for the first
month. The etiology of these changes is uncertain; however, the
acute inflammatory response and the healing wounds may play a role.
The clinical ramifications of the IL-8 changes are unclear. The
IL-8 findings when considered in light of the prior demonstration
that plasma levels of at least 7 other proangiogenic proteins are
similarly increased raises the possibility that tumor growth may be
stimulated during the first month after surgery in patients with
residual but unknown metastases. Further investigations to confirm
the results of the present study are required.
Acknowledgements
The present study was made possible by a generous
donation from the Wade Thompson Foundation to the Division of Colon
and Rectal Surgery, Department of Surgery, Mount Sinai West
Hospital, New York, NY, USA.
References
|
1
|
Jagoditsch M, Lisborg PH, Jatzko GR, Wette
V, Kropfitsch G, Denk H, Klimpfinger M and Stettner HM: Long-term
prognosis for colon cancer related to consistent radical surgery:
Multivariate analysis of clinical, surgical, and pathologic
variables. World J Surg. 24:1264–1270. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Bird NC, Mangnall D and Majeed AW: Biology
of colorectal liver metastases: A review. J Surg Oncol. 94:68–80.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Fisher B and Fisher ER: Experimental
evidence in support of the dormant tumor cell. Science.
130:918–919. 1959. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Peeters CF, de Waal RM, Wobbes T, Westphal
JR and Ruers TJ: Outgrowth of human liver metastases after
resection of the primary colorectal tumor: A shift in the balance
between apoptosis and proliferation. Int J Cancer. 119:1249–1253.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Eggermont AM, Steller EP, Marquet RL,
Jeekel J and Sugarbaker PH: Local regional promotion of tumor
growth after abdominal surgery is dominant over immunotherapy with
interleukin-2 and lymphokine activated killer cells. Cancer Detect
Prev. 12:421–429. 1988.PubMed/NCBI
|
|
6
|
Lee JW, Shahzad MM, Lin YG, Armaiz-Pena G,
Mangala LS, Han HD, Kim HS, Nam EJ, Jennings NB, Halder J, et al:
Surgical stress promotes tumor growth in ovarian carcinoma. Clin
Cancer Res. 15:2695–2702. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Coffey JC, Wang JH, Smith MJ,
Bouchier-Hayes D, Cotter TG and Redmond HP: Excisional surgery for
cancer cure: Therapy at a cost. Lancet Oncol. 4:760–768. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
O'Reilly MS, Holmgren L, Shing Y, Chen C,
Rosenthal RA, Moses M, Lane WS, Cao Y, Sage EH and Folkman J:
Angiostatin: A novel angiogenesis inhibitor that mediates the
suppression of metastases by a Lewis lung carcinoma. Cell.
79:315–328. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Allendorf JD, Bessler M, Horvath KD,
Marvin MR, Laird DA and Whelan RL: Increased tumor establishment
and growth after open vs. laparoscopic surgery in mice may be
related to differences in postoperative T-cell function. Surg
Endosc. 13:233–235. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Peeters CF, de Geus LF, Westphal JR, de
Waal RM, Ruiter DJ, Wobbes T, Oyen WJ and Ruers TJ: Decrease in
circulating anti-angiogenic factors (angiostatin and endostatin)
after surgical removal of primary colorectal carcinoma coincides
with increased metabolic activity of liver metastases. Surgery.
137:246–249. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Belizon A, Balik E, Horst P, Feingold D,
Arnell T, Azarani T, Cekic V, Skitt R, Kumara S and Whelan RL:
Persistent elevation of plasma vascular endothelial growth factor
levels during the first month after minimally invasive colorectal
resection. Surg Endosc. 22:287–297. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Kumara HM, Feingold D, Kalady M, Dujovny
N, Senagore A, Hyman N, Cekic V and Whelan RL: Colorectal resection
is associated with persistent proangiogenic plasma protein changes:
Postoperative plasma stimulates in vitro endothelial cell growth,
migration, and invasion. Ann Surg. 249:973–977. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Kumara Shantha HM, Cabot JC, Yan X, Herath
SA, Luchtefeld M, Kalady MF, Feingold DL, Baxter R and Whelan RL:
Minimally invasive colon resection is associated with a persistent
increase in plasma PlGF levels following cancer resection. Surg
Endosc. 25:2153–2158. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Kumara Shantha HM, Tohme ST, Herath SA,
Yan X, Senagore AJ, Nasar A, Kalady MF, Baxter R and Whelan RL:
Plasma soluble vascular adhesion molecule-1 levels are persistently
elevated during the first month after colorectal cancer resection.
Surg Endosc. 26:1759–1764. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Kumara Shantha HM, Myers EA, Herath SA,
Jang JH, Njoh L, Yan X, Kirchoff D, Cekic V, Luchtefeld M and
Whelan RL: Plasma monocyte chemotactic protein-1 remains elevated
after minimally invasive colorectal cancer resection. World J
Gastrointest Oncol. 6:413–419. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Kumara Shantha HM, Gaita D, Miyagaki H,
Yan X, Hearth SA, Njoh L, Cekic V and Whelan RL: Plasma chitinase
3-like 1 is persistently elevated during first month after
minimally invasive colorectal cancer resection. World J
Gastrointest Oncol. 8:607–614. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Kumara Shantha HM, Kirchoff D, Naffouje S,
Grieco M, Herath SA, Dujovny N, Kalady MF, Hyman N, Njoh L and
Whelan RL: Plasma from the second and third weeks after open
colorectal resection for cancer stimulates in vitro endothelial
cell growth, migration, and invasion. Surg Endosc. 26:790–795.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Li A, Varney ML, Valasek J, Godfrey M,
Dave BJ and Singh RK: Autocrine role of interleukin-8 in induction
of endothelial cell proliferation, survival, migration and MMP-2
production and angiogenesis. Angiogenesis. 8:63–71. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Srivastava SK, Bhardwaj A, Arora S, Tyagi
N, Singh AP, Carter JE, Scammell JG, Fodstad Ø and Singh S:
Interleukin-8 is a key mediator of FKBP51-induced melanoma growth,
angiogenesis and metastasis. Br J Cancer. 112:1772–1781. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Lee YS, Choi I, Ning Y, Kim NY,
Khatchadourian V, Yang D, Chung HK, Choi D, LaBonte MJ, Ladner RD,
et al: Interleukin-8 and its receptor CXCR2 in the tumour
microenvironment promote colon cancer growth, progression and
metastasis. Br J Cancer. 106:1833–1841. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Brew R, Erikson JS, West DC, Flanagan BF
and Christmas SE: Interleukin-8 as a growth factor for human
colorectal carcinoma cells in vitro. Biochem Soc Trans.
25:264S1997. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Mian BM, Dinney CP, Bermejo CE, Sweeney P,
Tellez C, Yang XD, Gudas JM, McConkey DJ and Bar-Eli M: Fully human
anti-interleukin 8 antibody inhibits tumor growth in orthotopic
bladder cancer xenografts via down-regulation of matrix
metalloproteases and nuclear factor-kappaB. Clin Cancer Res.
9:3167–3175. 2003.PubMed/NCBI
|
|
23
|
Yao C, Lin Y, Chua MS, Ye CS, Bi J, Li W,
Zhu YF and Wang SM: Interleukin-8 modulates growth and invasiveness
of estrogen receptor-negative breast cancer cells. Int J Cancer.
121:1949–1957. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Brat DJ, Bellail AC and Van Meir EG: The
role of interleukin-8 and its receptors in gliomagenesis and
tumoral angiogenesis. Neuro-Oncol. 7:122–133. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Araki S, Omori Y, Lyn D, Singh RK,
Meinbach DM, Sandman Y, Lokeshwar VB and Lokeshwar BL:
Interleukin-8 is a molecular determinant of androgen independence
and progression in prostate cancer. Cancer Res. 67:6854–6862. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Jiang WG, Sanders AJ, Ruge F and Harding
KG: Influence of interleukin-8 (IL-8) and IL-8 receptors on the
migration of human keratinocytes, the role of PLC-γ and potential
clinical implications. Exp Ther Med. 3:231–236. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Sticherling M, Bornscheuer E, Schröder JM
and Christophers E: Localization of neutrophil-activating
peptide-1/interleukin-8-immunoreactivity in normal and psoriatic
skin. J Invest Dermatol. 96:26–30. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Kumara Shantha HM, Tohme ST, Kim IY, Kim
DG, Kalady MF, Luchtefeld M, Hoffman K, Dimaggio V and Whelan RL:
Minimally invasive colorectal resection is associated with a
transient increase in plasma hepatocyte growth factor levels early
after surgery for colon cancer. Surg Innov. 18:254–258. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Harmon GD, Senagore AJ, Kilbride MJ and
Warzynski MJ: Interleukin-6 response to laparoscopic and open
colectomy. Dis Colon Rectum. 37:754–759. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Ordemann J, Jacobi CA, Schwenk W,
Stösslein R and Müller JM: Cellular and humoral inflammatory
response after laparoscopic and conventional colorectal resections.
Surg Endosc. 15:600–608. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Li A, Dubey S, Varney ML, Dave BJ and
Singh RK: IL-8 directly enhanced endothelial cell survival,
proliferation, and matrix metalloproteinases production and
regulated angiogenesis. J Immunol. 170:3369–3376. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Mizukami Y, Jo WS, Duerr EM, Gala M, Li J,
Zhang X, Zimmer MA, Iliopoulos O, Zukerberg LR, Kohgo Y, et al:
Induction of interleukin-8 preserves the angiogenic response in
HIF-1alpha-deficient colon cancer cells. Nat Med. 11:992–997. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Karayiannakis AJ, Zbar A, Polychronidis A
and Simopoulos C: Serum and drainage fluid vascular endothelial
growth factor levels in early surgical wounds. Eur Surg Res.
35:492–496. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Wu FP, Hoekman K, Meijer S and Cuesta MA:
VEGF and endostatin levels in wound fluid and plasma after breast
surgery. Angiogenesis. 6:255–257. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Wu FP, Hoekman K, Sietses C, von Blomberg
BM, Meijer S, Bonjer HJ and Cuesta MA: Systemic and peritoneal
angiogenic response after laparoscopic or conventional colon
resection in cancer patients: A prospective, randomized trial. Dis
Colon Rectum. 47:1670–1674. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Peeters CF, Westphal JR, de Waal RM,
Ruiter DJ, Wobbes T and Ruers TJ: Vascular density in colorectal
liver metastases increases after removal of the primary tumor in
human cancer patients. Int J Cancer. 112:554–559. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Scheer MG, Stollman TH, Vogel WV, Boerman
OC, Oyen WJ and Ruers TJ: Increased metabolic activity of indolent
liver metastases after resection of a primary colorectal tumor. J
Nucl Med. 49:887–891. 2008. View Article : Google Scholar : PubMed/NCBI
|