|
1
|
Ostrom Q, Gittleman H, Farah P, Ondracek
A, Chen Y, Wolinsky Y, et al: CBTRUS statistical report: primary
brain and central nervous system tumors diagnosed in the United
States in 2006–2010. Neuro-Οncol. 15:ii1–ii56. 2013.
|
|
2
|
Stupp R, Brada M, van den Bent MJ, Tonn JC
and Pentheroudakis G: ESMO Guidelines Working Group: High-grade
glioma: ESMO Clinical Practice Guidelines for diagnosis, treatment
and follow-up. Ann Oncol. 25 Suppl 3:iii93–iii101. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Louis DN, Ohgaki H, Wiestler OD, Cavenee
WK, Burger PC, Jouvet A, Scheithauer BW and Kleihues P: The 2007
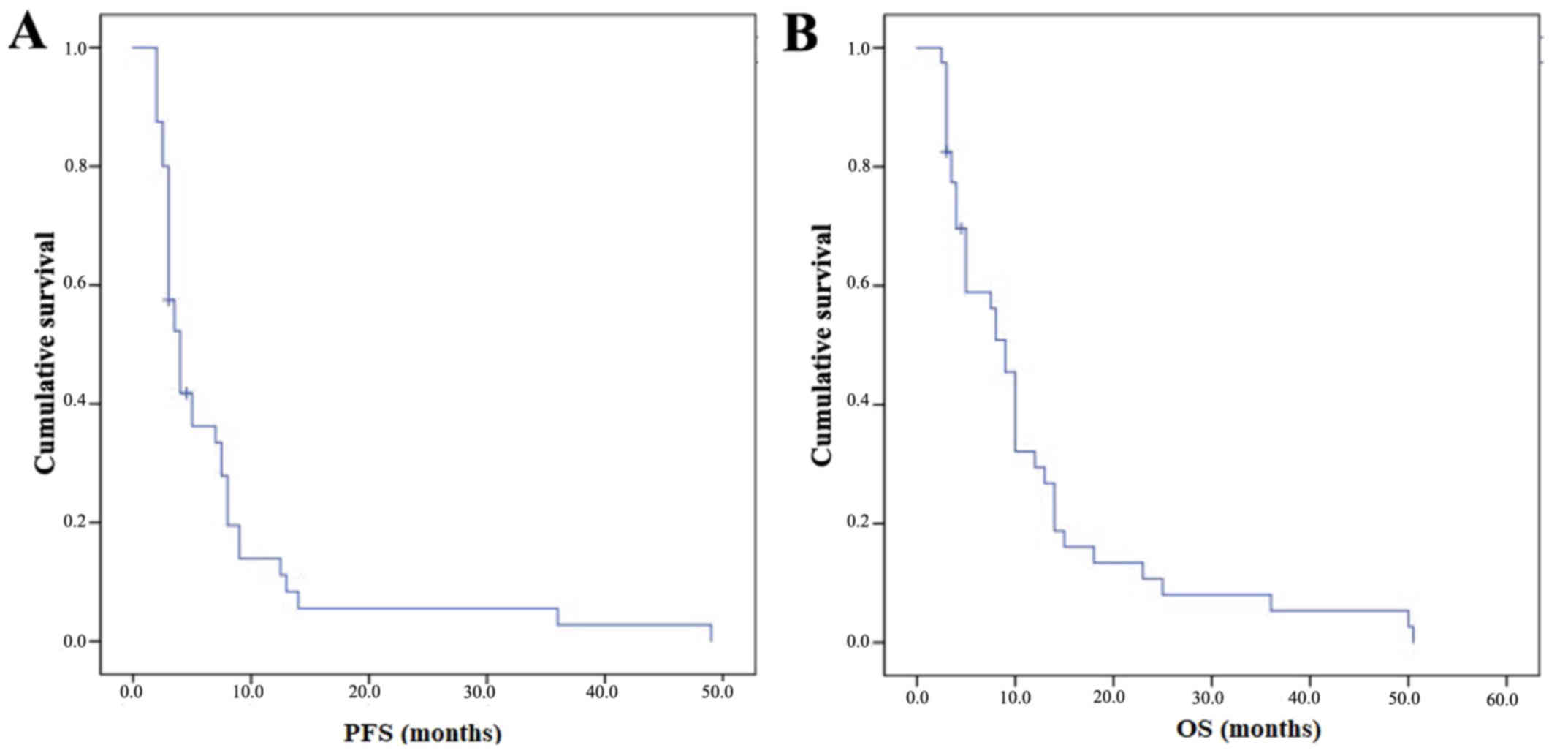
WHO classification of tumours of the central nervous system. Acta
Neuropathol. 114:97–109. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Stupp R, Mason WP, van den Bent MJ, Weller
M, Fisher B, Taphoorn MJ, Belanger K, Brandes AA, Marosi C, Bogdahn
U, et al: European Organisation for Research and Treatment of
Cancer Brain Tumor and Radiotherapy Groups; National Cancer
Institute of Canada Clinical Trials Group: Radiotherapy plus
concomitant and adjuvant temozolomide for glioblastoma. N Engl J
Med. 352:987–996. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Weller M, Cloughesy T, Perry JR and Wick
W: Standards of care for treatment of recurrent glioblastoma-are we
there yet? Neuro-oncol. 15:4–27. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Fabi A, Metro G, Vidiri A, Lanzetta G,
Carosi M, Telera S, Maschio M, Russillo M, Sperduti I, Carapella
CM, et al: Low-dose fotemustine for recurrent malignant glioma: A
multicenter phase II study. J Neurooncol. 100:209–215. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Tosoni A, Franceschi E, Poggi R and
Brandes AA: Relapsed Glioblastoma: Treatment Strategies for Initial
and Subsequent Recurrences. Curr Treat Options Oncol. 17:492016.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Beauchesne P: Fotemustine: A
third-generation nitrosourea for the treatment of recurrent
malignant gliomas. Cancers (Basel). 4:77–87. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Silvani A, Gaviani P, Lamperti E, Botturi
A, Ferrari D, Simonetti G and Salmaggi A: Lecture: Fotemustine in
brain tumors. Neurol Sci. 32 Suppl 2:S255–S257. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Lombardi G, Farina P, Della Puppa A,
Cecchin D, Pambuku A, Bellu L and Zagonel V: An overview of
fotemustine in high-grade gliomas: From single agent to association
with bevacizumab. BioMed Res Int. 2014:6985422014. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Kyritsis AP and Levin VA: An algorithm for
chemotherapy treatment of recurrent glioma patients after
temozolomide failure in the general oncology setting. Cancer
Chemother Pharmacol. 67:971–983. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Frenay M, Giroux B, Khoury S, Derlon JM
and Namer M: Phase II study of fotemustine in recurrent
supratentorial malignant gliomas. Eur J Cancer. 27:852–856. 1991.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Scoccianti S, Detti B, Sardaro A, Iannalfi
A, Meattini I, Leonulli BG, Borghesi S, Martinelli F, Bordi L,
Ammannati F, et al: Second-line chemotherapy with fotemustine in
temozolomide-pretreated patients with relapsing glioblastoma: A
single institution experience. Anticancer Drugs. 19:613–620. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Fabrini MG, Silvano G, Lolli I, Perrone F,
Marsella A, Scotti V and Cionini L: A multi-institutional phase II
study on second-line Fotemustine chemotherapy in recurrent
glioblastoma. J Neurooncol. 92:79–86. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Brandes AA, Tosoni A, Franceschi E, Blatt
V, Santoro A, Faedi M, Amistà P, Gardiman M, Labianca R, Bianchini
C, et al: Fotemustine as second-line treatment for recurrent or
progressive glioblastoma after concomitant and/or adjuvant
temozolomide: A phase II trial of Gruppo Italiano Cooperativo di
Neuro-Oncologia (GICNO). Cancer Chemother Pharmacol. 64:769–775.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Addeo R, Caraglia M, De Santi MS, Montella
L, Abbruzzese A, Parlato C, Vincenzi B, Carraturo M, Faiola V,
Genovese M, et al: A new schedule of fotemustine in
temozolomide-pretreated patients with relapsing glioblastoma. J
Neurooncol. 102:417–424. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Montemurro N, Perrini P, Blanco MO and
Vannozzi R: Second surgery for recurrent glioblastoma: A concise
overview of the current literature. Clin Neurol Neurosurg.
142:60–64. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Sulman EP, Ismaila N, Armstrong TS, Tsien
C, Batchelor TT, Cloughesy T, Galanis E, Gilbert M, Gondi V, Lovely
M, et al: Radiation Therapy for Glioblastoma: American Society of
Clinical Oncology Clinical Practice Guideline Endorsement of the
American Society for Radiation Oncology Guideline. J Clin Oncol.
35:361–369. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Wen PY, Macdonald DR, Reardon DA,
Cloughesy TF, Sorensen AG, Galanis E, Degroot J, Wick W, Gilbert
MR, Lassman AB, et al: Updated response assessment criteria for
high-grade gliomas: Response assessment in neuro-oncology working
group. J Clin Oncol. 28:1963–1972. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Common Terminology Criteria for Adverse
Events v4.03 (CTCAE). http://ctep.cancer.govAugust 10–2017
|
|
21
|
Kaplan E and Meier P: Nonparametric
estimation from incomplete observations. J Am Stat Assoc.
53:457–481. 1958. View Article : Google Scholar
|
|
22
|
Fabi A, Metro G, Russillo M, Vidiri A,
Carapella CM, Maschio M, Cognetti F, Jandolo B, Mirri MA, Sperduti
I, et al: Treatment of recurrent malignant gliomas with fotemustine
monotherapy: Impact of dose and correlation with MGMT promoter
methylation. BMC Cancer. 9:1012009. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Paccapelo A, Lolli I, Fabrini MG, Silvano
G, Detti B, Perrone F, Savio G, Santoni M, Bonizzoni E, Perrone T,
et al: A retrospective pooled analysis of response patterns and
risk factors in recurrent malignant glioma patients receiving a
nitrosourea-based chemotherapy. J Transl Med. 10:902012. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Gaviani P, Simonetti G, Salmaggi A,
Lamperti E and Silvani A: Safety of second-line chemotherapy with
non-conventional fotemustine schedule in recurrent high grade
gliomas: A single institution experience. J Neurooncol.
113:527–529. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Brandes AA, Franceschi E, Tosoni A, Blatt
V, Pession A, Tallini G, Bertorelle R, Bartolini S, Calbucci F,
Andreoli A, et al: MGMT promoter methylation status can predict the
incidence and outcome of pseudoprogression after concomitant
radiochemotherapy in newly diagnosed glioblastoma patients. J Clin
Oncol. 26:2192–2197. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Taal W, Brandsma D, de Bruin HG, Bromberg
JE, Swaak-Kragten AT, Smitt PA, van Es CA and van den Bent MJ:
Incidence of early pseudo-progression in a cohort of malignant
glioma patients treated with chemoirradiation with temozolomide.
Cancer. 113:405–410. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Hegi ME, Diserens AC, Gorlia T, Hamou MF,
de Tribolet N, Weller M, Kros JM, Hainfellner JA, Mason W, Mariani
L, et al: MGMT gene silencing and benefit from temozolomide in
glioblastoma. N Engl J Med. 352:997–1003. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Weller M, Tabatabai G, Kästner B, Felsberg
J, Steinbach JP, Wick A, Schnell O, Hau P, Herrlinger U, Sabel MC,
et al: DIRECTOR Study Group: MGMT promoter methylation is a strong
prognostic biomarker for benefit from dose-intensified temozolomide
rechallenge in progressive glioblastoma: The DIRECTOR Trial. Clin
Cancer Res. 21:2057–2064. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Taal W, Oosterkamp HM, Walenkamp AM,
Dubbink HJ, Beerepoot LV, Hanse MC, Buter J, Honkoop AH, Boerman D,
de Vos FY, et al: Single-agent bevacizumab or lomustine versus a
combination of bevacizumab plus lomustine in patients with
recurrent glioblastoma (BELOB trial): A randomised controlled phase
2 trial. Lancet Oncol. 15:943–953. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Brandes AA, Finocchiaro G, Zagonel V, Reni
M, Caserta C, Fabi A, Clavarezza M, Maiello E, Eoli M, Lombardi G,
et al: AVAREG: A phase II, randomized, noncomparative study of
fotemustine or bevacizumab for patients with recurrent
glioblastoma. Neuro-oncol. 18:1304–1312. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Azoulay M, Santos F, Shenouda G, Petrecca
K, Oweida A, Guiot MC, Owen S, Panet-Raymond V, Souhami L and
Abdulkarim BS: Benefit of re-operation and salvage therapies for
recurrent glioblastoma multiforme: Results from a single
institution. J Neurooncol. 132:419–426. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Seystahl K, Wick W and Weller M:
Therapeutic options in recurrent glioblastoma-An update. Crit Rev
Oncol Hematol. 99:389–408. 2016. View Article : Google Scholar : PubMed/NCBI
|