Introduction
Sarcomas are tumors with mesenchymal origin and very
poor prognosis compromising of 2% of all cancer deaths. These
neoplasms are very rare and account for 1 to 2% of all malignancies
(1-7).
Sarcomas of the female genital tract have a low frequency of 3%
(4,8,9). In
particular, vulvar sarcomas account for 1 to 2% of all the vulvar
tumors, compared to the uterine sarcomas, which represent the vast
majority of all sarcomas of the female reproductive system (90%)
(2,5-7).
Vulvar sarcomas comprise a highly heterogeneous
group of histological types, which include leiomyosarcomas,
epithelioid sarcomas, fibrosarcomas, liposarcomas,
hemangiosarcomas, rhabdomyosarcomas, angiosarcomas, malignant
hemagiopericytomas, neurogenous sarcomas, dermatofibrosarcomas
protuberans, Ewing sarcomas, synovial sarcomas, clear cells
carcinomas, malignant fibrous histiocytomas and sometimes
aggressive angiomyxomas (1,3,4,6,10-12).
The age of the described patients with vulvar leiomyosarcomas at
the time of clinical presentation ranged between 14 and 69 years of
age, with an average age of approximately 30-40 years (4,6,13,14).
Vulvar embryonal rhabdomyosarcoma typically presents in girls less
than 8 years of age (15). The size
of vulvar sarcomas varies between 2 and 10-cm (4). Vulvar sarcomas are usually
asymptomatic or they are characterized by non-specific clinical
manifestations, such an enlarging vulvar mass with a local
discomfort. Vulvar sarcomas located in the Bartholin's gland area
are often misdiagnosed as their clinical manifestations are very
similar to benign lesions. These lesions are most commonly
misdiagnosed as Bartholin's cysts or abscesses resulting in
delaying diagnosis and worsening the prognosis (11,12,6). In
these cases, the late symptoms include pain, ulceration, bleeding
and voiding dysfunction (3,6,11).
Vulvar sarcomas are characterized by a high chance of metastasis;
it seems that chemotherapy achieves regression of lung metastasis
(6,12,14,16).
Leiomyosarcomas are the most common histological
variants of vulvar sarcomas (2,5,7,17-22).
Vulvar leiomyosarcomas are considered to originate from the smooth
muscles within erectile tissue, blood vessel walls, rough
ligaments, dartos muscles, erector-pili muscles and from stem cells
localized in Bartholin's gland (22-24).
Leiomyosarcomas occur most frequently in the labia majora, followed
in a decreasing order by the Bartholin's gland area, the
pericloitoral area and the labia minora (25,26).
Localizations of leiomyosarcomas in the Bartholin's gland area are
extremely rare and only few such cases are reported in the
international literature (1,2,5,7,10,12,13,17,18).
The biological behavior of the vulvar leiomyosarcomas is not fully
understood and very little information is available so far
(1). Most of the described cases of
vulvar leiomyosarcomas in the international literature are about
patients from Western countries suggesting therefore genetic
disposition and lifestyle connection (27). A possible carcinogenetic precursor
of these neoplasms is the chronic inflammation. This hypothesis is
supported by the findings of coexistence between vulvar
leiomyosarcomas and longstanding lichen sclerosus (28). Also, another predisposing factor of
vulvar leiomyosarcomas seems to be the pregnancy because occurrence
of them during pregnancy has been reported (10,17,29).
It seems that the positivity of estrogen and progesterone receptors
is implicated in the development of vulvar leiomyosarcomas. The
potential impact of estrogens and progesterone signaling through
their receptors may result in induction of proliferation and growth
of DNA damaged cells resulting finally in tumorogenesis of the
vulvar leiomyosarcomas (10,17,29).
The histopathological examination of the excised
mass confirms the diagnosis of the extremely rare entity of vulvar
leiomyosarcomas (2,5,7). Given
the extreme rarity of vulvar leiomyosarcomas, an optimal treatment
strategy has not yet been elucidated. It seems that their primary
treatment of choice is the surgical excision, including wide local
excision or radical hemivulvectomy. The usefulness of ipsilateral
lymphadenectomy in the treatment of vulvar leiomyosarcomas is not
clear because these neoplasms metastasize mostly by the bloodstream
compared to lymphogenous metastasis. Locally recurrent tumors
require adjuvant treatment in the form of radiotherapy. Adjuvant
chemotherapy is placed in the treatment of distal metastases;
however the exact role of adjuvant chemotherapy and/or radiotherapy
remains uncertain for vulvar leiomyosarcomas, which display very
aggressive behavior and rapid progression (2,5,7).
Herein, we present a very rare case of vulvar
leiomyosarcoma localized in the Bartholin's gland area in a
42-year-old female and describe its histopathological and
immunohistochemical features. Also, the current literature is
reviewed in terms of clinical signs and symptoms, diagnosis,
biological behavior, prognosis and treatment. Vulvar sarcomas
located in the Bartholin's gland are often mistakenly considered as
benign lesions resulting in delayed diagnosis.
Case report
A 42-year-old patient presented to outpatient clinic
because of a vulvar lump in the area of the left Bartholin's gland
with a 6-month history of progressive swelling. In her
gynecological history, the patient reported laparoscopic
hysterectomy without salpingo-oophorectomy, two years ago, due to
heavy metrorrhagia and the uterus was taken out through the vagina
directly. The final histological exam of the hysterectomy showed
benign leiomyomas within the uterus.
Pelvic examination showed a solid mass of 6.5-cm in
maximum diameter, in the area of the left Bartholin's gland.
Palpation of the inguinal lymph nodes in either groin was normal;
there were no palpable nodes. The patient underwent wide local
excision and the mass was enucleated completely from the bed. The
surgical specimen was sent for pathological examination. We did not
indicate a biopsy of the mass before the excision because our
initial clinical diagnosis was as a chronic left Bartholin's gland
abscess.
Macroscopically, the tumor was 6.5x4.5x3.5-cm in
size with regular margins. Cut surface showed a whitish,
homogeneous lesion with fibroelastic consistency.
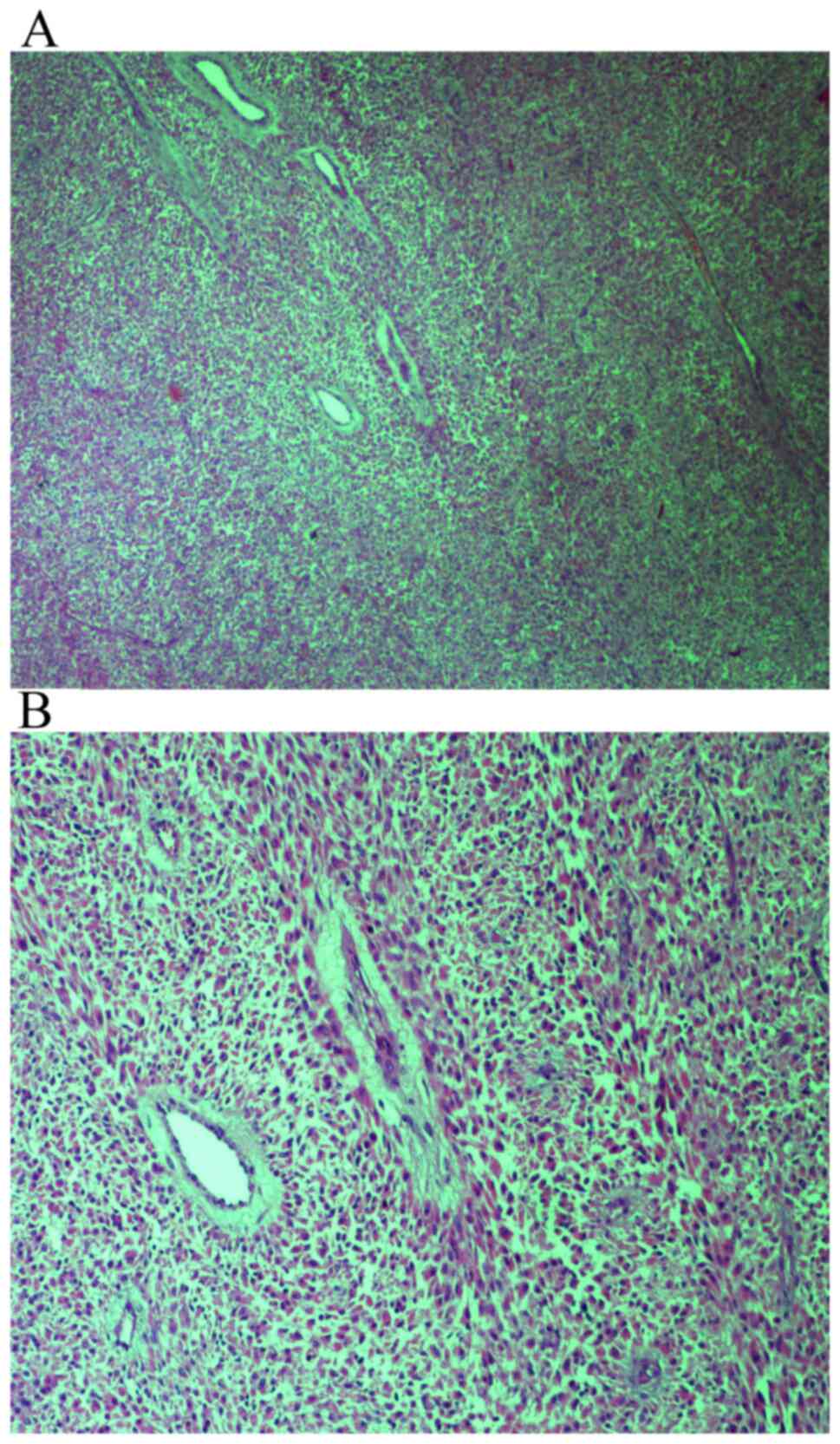
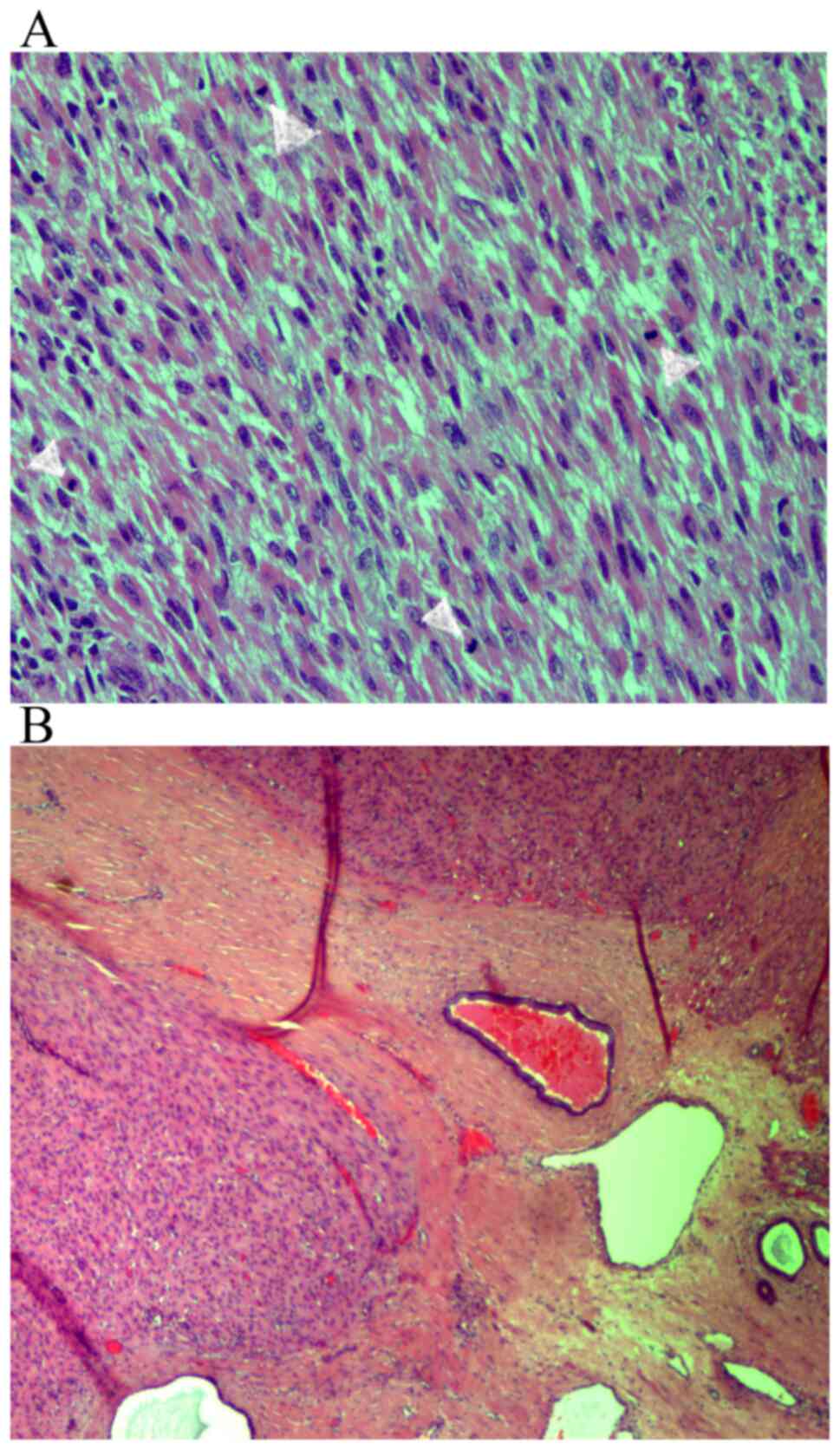
Microscopic examination of the hematoxylin and
eosin-stained sections showed intersecting fascicles of spindle
cells (Fig. 1A and B), with moderate to severe atypia
(Fig. 2A and B). The number of mitoses was up to 8 per
10 high power fields (Fig. 3A). The
neoplasm to its greatest extent was circumscribed and in places had
an invasive growth pattern. Tumoral necrosis was not seen. Involved
Bartholin' gland by the tumor was identified. The tumor extended
focally to the surgical margin (Fig.
3B). The neoplastic cells showed positive staining for smooth
muscle actin (SMA) (Fig. 4A),
desmin (Fig. 4B), HHF35 (Fig. 4C), caldesmon (Fig. 5A), vimentin (Fig. 5B) and estrogen (Fig. 5C) and progesterone receptors
(Fig. 5D). Immunohistochemistry was
negative for S100, myoglobulin, keratin 116, CD117, CD34 and
CD31.
Thoracic and upper and lower abdominal CT scans were
negative for malignancy. Also, pelvic MRI was non suggestive for
infiltrative pelvic lymph nodes. The diagnosis was primary vulvar
leiomyosarcoma, localized in the Bartholin's gland area. The
patient was discharged from the hospital and during the follow-up,
every four months, no local recurrences or metastases of the
disease were observed 53 months after surgery and the patient is in
excellent physical condition. Although the mass was greater than
5-cm and a focally infiltrated surgical margin was found in the
histological specimen, the patient denied further surgery or/and
local radiotherapy. During the close follow-up the patient did not
complain about itching, burning, pain, numbness at the treatment
site, body image disturbance or sexual problems.
Discussion
Primary vulvar leiomyosarcomas are extremely rare
tumors and the localization of these tumors in the Bartholin's
gland area results in diagnostic delays (7). Clinical differential diagnosis of
vulvar leiomyosarcomas located in the Bartholin's gland area
include Bartholin's gland cyst or abscess, infectious granuloma,
syringeal, lipoma, fibroma, leiomyoma, hidradenoma, hidradentis
suppurativa, hematoma, endometriosis, accessory breast gland,
warts, paraganglioma or squamous cell carcinoma, adenosquamous
carcinoma, adenocarcinoma, adenoid cystic carcinoma, small cell
carcinoma, transitional carcinoma, differential carcinoma,
melanoma, spindle cell synovial sarcoma, embryonal
rhabdomyosarcoma, dermatofibrosarcoma, malignant fibrous
histiocytoma, extraskeletal Ewing's sarcoma, hibrosarcoma and
epithelioid sarcoma (4,7,30-38).
Furthermore, when the tumor is located in the Bartholin's gland,
leiomyosarcoma should be distinguished from adenosarcoma, which is
composed by a mixture of benign glandular epithelium and a
malignant sarcomatous stroma (39,40).
Diagnosis is made by the histopathological examination of a biopsy
of the lesion or of the complete excision of the neoplasm. In our
case, non-epithelial component was identified microscopically in
the tumor and therefore we concluded the diagnosis of vulvar
leiomyosarcoma. Metastatic dissemination of vulvar leiomyosarcomas
is thought to be through the hematogenous routes. The most common
sites of distant metastatic sites have been reported to be the
liver and the lungs and occasionally the bones (1,37). The
role of the lymphogenous routes for the metastatic dissemination of
vulvar leiomyosarcomas is questionable (28).
Vulvar leiomyosarcomas can be distinguished from
vulvar leiomyomas or vulvar atypical leiomyomas according to the
suggestions of Nielsen et al (38). Three or more of the following
histological and pathological characteristics are important for the
diagnosis of vulvar leiomyosarcomas: i) The tumor has size greater
than 5-cm in diameter; ii) infiltration is seen in the margins of
the tumor; iii) the tumoral background consists of more than five
mitotic figures per 10 high-power fields; and iv) the tumoral cells
show moderate to severe atypia. Leiomyomas exhibit only one of the
above features; atypical leiomyomas exhibit only two of these
features (38). Both leiomyomas and
leiomyosarcomas exhibit immunopositivity for muscle markers
including smooth muscle actin, muscle-specific actin and desmin and
focal positivity for S-100 and cytokeratin (10). In our case, the neoplastic cells
showed positive staining for smooth muscle actin (SMA), desmin,
HHF35, caldsmon, vimentin and estrogen and progesterone receptors
(Figs. 4 and 5).
A preoperative biopsy of vulvar masses located in
the Bartholin's gland area and particularly in those with a
complicated appearance is highly recommended because early
diagnosis is important for curative treatment without delays of
these extremely rare neoplasms (3,7,12,16,26).
However, in our case we did not indicate a biopsy of the mass
before operation because our preoperative diagnosis was as a
chronic Bartholin's gland abscess. Superficial lymphadenopathy is
due to a cyst, inflammation, lymphoma or metastatic malignant tumor
(41,42). In the presence of a pathognomonic
inguinal node the use of fine-needle aspiration biopsy is an easy,
reliable and safe office procedure, which immediately provides an
important tool of diagnosis (41).
In the study by Altinboğa and Yüce (43) the lymph node fine-needle aspiration
cytology (FNAC) showed sensitivity of 95.4%, specificity of 94.1%,
positive predictive value of 95.4% and negative predictive value of
94.1% (43).
The first-line treatment involves surgical excision
of the lesion. Localized disease is usually managed with wide local
excision with surgically free margins. According to Aartsen and
Albus-Lutter (1) the width of
normal margin-tissue proposed for the surgeon doing the excision is
2-cm and for the pathologist 1-cm because of the shrinking effect.
Poor prognostic factors are considered to be mitotic rate more than
10 mitotic figures per 10 HPF, high histological grade, tumor size
>5-cm, local recurrence and distal metastases (38,44).
These neoplasms tend to metastasize by bloodstream and therefore
ipsilateral lymphadenectomy is questionable (28). The decision to treat with vulvectomy
is made by the size of the lesion (7,10,18).
Inguinal lymphadenectomy does not improve treatment (1,22). The
available data is limited and uncertain regarding radiosensitivity
and chemosensitivity in the treatment of the vulvar
leiomyosarcomas. However, in the presence of negative prognostic
factors radiotherapy and chemotherapy should be given. Important
favorite prognostic factors are the lower grade of nuclear atypia,
the smaller tumoral size, the pathological confirmation of at least
2-cm negative surgical margins and the absence of local recurrences
(1,2,12,14,22,38).
Favor immunohistochemical factors include the overexpression of
estrogen, progesterone and androgen receptors, the moderate
immunopositivity for Ki-67 and the absence of p53 expression
(4,22). It seems that the type of operation
with inadequately resected tumors is the most significant negative
prognostic factor for the appearance of local recurrences and
distal metastases, compared to tumoral size of more than 5-cm
(1). In addition to these factors,
vulvar leiomyosarcomas with more aggressive behavior are defined on
the basis of high cellularity, anaplasia, mitotic activity more
than ten per 10 high-power fields, high grade of nuclear atypia and
presence of tumoral necrosis (12,16).
The indications for radiotherapy includes: a) positive margin tumor
involvement at the initial surgical treatment and b) tumor size
>5-cm (22,25,38,44,45).
Pharmacogenomics biomarkers for the prediction of response to
chemotherapeutic regimens seem to be involved in the improvement of
molecular diagnostics in treatment of a specific subset of patients
with soft tissue sarcomas. Actually, human equilibrative nucleotide
transporter 1 (hENT1) is a molecular biomarker that could predict
gemcitabine efficacy in leiomyosarcoma (46). Furthermore, TP53 mutations are
significantly associated with longer progression-free survival
compared to TP53 wild-type (47).
In addition, after 12 weeks of treatment with pazopanib, it has
been found that the progression-free survival was positively
correlated to high levels of interleukin (IL)-12 and mitochondrial
pyruvate carrier 3 (MPC3) levels and negatively correlated with low
levels of VEGF2 and high levels of placental growth factor (PGF)
(48). In addition, in soft tissue
sarcoma the activity of trabectedin was found to inversely
correlate with the mRNA levels of BRCA1. Particularly, low levels
of mRNA BRCA1 expression were associated with improvement in
outcome of patients (49).
In our case, the neoplastic cells showed positive
staining for estrogen and progesterone receptors (Fig. 5C and D), suggesting the potential role of
estrogen and progesterone in the development and progression of
vulvar leiomyosarcoma. However, in our case we did not examine the
pre- and post-operative serum estrogen levels of our patient.
Nethertheless, the predisposing role of estrogen and progesterone
in vulvar leiomyosarcoma tumorogenesis is supported by their
occurrence during pregnancy (10,17,29).
It is possible that the positivity of estrogen and progesterone
receptors may initiate the proliferation and growth of DNA damaged
cells resulting in development and progression of vulvar
leiomyosarcoma (10,17,29).
The role of aromatase inhibitors (AIs), selective estrogen receptor
modulators (SERMs), progestins and GnRH-analogues for the treatment
of vulvar leiomyosarcoma and especially for their recurrences is
not clear due to the rarity of this entity and the lack of clinical
trials to determine the clinical efficacy and usefulness of the
above regiments for first- and second-line therapies. However, we
have some evidence in the case of uterine leiomyosarcoma.
Particularly, patients with uterine leiomyosarcoma and a high
expression rate of ER and PR show good response to hormonal therapy
(50). Yamaguchi et al
suggested that Letrozole as well as progestins could be the first
choice for patients with recurrent or residual low-grade
endometrial stromal sarcoma (51).
It seems that letrozole is the first-line hormone drug for
postoperative adjuvant therapy in patients with stage I uterine
leiomyosarcoma, while exemestane and anastrozole are for
second-line treatment in patients with recurrent, metastatic and
unresectable uterine leiomyosarcoma (52). In a clinical trial by George et
al (53) of 27 postmenopausal
women with metastatic and/or unresectable uterine leiomyosarcoma
with positive estrogen receptors and/or postive progesteron
receptors it has been found that the rate of stable disease was 54%
in all patients and the 12-week rate of progression free survival
50%. These findings suggest that strong expression of estrogen and
progesterone expression in tumors is related with longer
progression free survival (53). On
the other hand, the use of progestins in uterine leiomyosarcoma
should be cautious because medroxyprogesterone acetate in higher
doses (5 mg/day) is able to significantly increase the growth of
this neoplasm (52). In addition,
it has been found that patients who receive tamoxifen treatment for
more than five years show an increase in the incidence of uterine
leiomyosarcoma to 17/100,000 women yearly (50,54).
Therefore, tamoxifen is contraindicated for the treatment of
uterine leiomyosarcoma (52).
In the present case, we chose to treat our patient
with wide local excision because of the patients' age. Also, after
the histopathological confirmation of the disease, in view of the
absence of pelvic lymph node infiltration suggested by the MRI
examination, inguinal lymphadenectomy was decided not to be done.
Our patient denied radiotherapy although the tumor extended focally
to the surgical margin. In such cases, we recommend radiotherapy
because the risk of local recurrence is related to the inadequate
resection margins and not to the size of the tumor (39). Furthermore, Aartsen and Albus-Lutter
suggested that the degree of differentiation should not be
determined for the case of vulvar leiomyosarcoma (1). Therefore, in our case we did not
indicate the grade of the vulvar leiomyosarcoma localized in the
Bartholin's gland area. In addition, in the present study we
resumed reported cases of vulvar leiomyosarcoma in a table
according to their histological and immunohistochemical features,
treatment and clinical outcome (Table
I).
 | Table IHistological and immunohistochemical
features, treatment and clinical outcome of vulvar leiomyosarcoma
reported cases. |
Table I
Histological and immunohistochemical
features, treatment and clinical outcome of vulvar leiomyosarcoma
reported cases.
| Author- Published
year | Age (years) | Size (cm) | MFI | MTCN | IHC | Initial
treatment | Margins | Local
recurrence | Treatment of
recurrence | Follow-up | (Refs.) |
|---|
| Davos and Abell
(1976) | 41 | NS | >10 | NS | NS | Wide local
excision | NS | NS | - | 28 months, alive,
NED | (18) |
| Davos and Abell
(1976) | 49 | NS | >10 | NS | NS | Local excision | NS | + | Wide local
excision | 9 years, alive,
NED | (18) |
| Davos and Abell
(1976) | 84 | NS | >10 | NS | NS | Wide local
excision | NS | + | No further
treatment | 6 months,
disseminated metastases, died of disease | (18) |
| Davos and Abell
(1976) | 54 | NS | >10 | NS | NS | Local excision | NS | + | Hemivulvectomy;
hysterectomy and excision of vaginal mass | 9 years,
disseminated metastases, died of disease | (18) |
| Davos and Abell
(1976) | 35 | NS | >10 | NS | NS | Local excision | NS | + | Re-excision;
radical vulvectomy | 9 years, alive | (18) |
| Møller et al
(1990) | 54 | 8 | 15 | Yes- Focal | Desmin:
Positive | Radical vulvectomy
+ inguinofemoral lymphadenectomy | No | No | - | 30 months, alive,
NED | (55) |
| Tawfik et al
(1994) | 52 | 15 | 25-30 | Yes- Focal | SMA, vimentin,
HHF-35, ER, p53: Positive | Local excision +
radiotherapy | Infiltrative | No | - | 14 months, alive,
NED | (25) |
| Aartsen and
Albus-Lutter (1994) | 15 | 7 | NS | NS | NS | Radiotherapy 40
Gy | | +; 2.5 years | Wide Local Excision
+ Radiotherapy 40 Gy | 24 years, alive,
NED | (1) |
| Aartsen and
Albus-Lutter (1994) | 41 | 4.5 | NS | NS | NS | Wide local
excision | - | - | - | 17 years, died of
disease | (1) |
| Aartsen and
Albus-Lutter (1994) | 75 | 10 | NS | NS | NS | Radical
vulvectomy | NS | 6 months & 3
months | Local excision
-Local excision | 4 months, died of
disease | (1) |
| Aartsen and
Albus-Lutter (1994) | 67 | 10 | NS | NS | NS | Radical
vulvectomy | NS | 5 months | Radiotherapy 49
Gy | 7 years, died of
disease | (1) |
| Fried-Oginski et
al (1995) | 31 | 5 | 4 | Yes- Focal | SMA, muscular
actin, vimentin: Positive | Local Excision + 8
weeks later Wide Local Excision | NS | 10 months | Wide Local Excision
+ Radiotherapy | NS | (56) |
| Nielsen et
al (1996) | 33 | 5.5 | 5 | NS | SMA, muscular
actin, vimentin, desmin, ER, PR: Positive; keratin, S-100:
Negative | Local Excision | Infiltrative | 4 months | Wide local
Excision | 36 months, alive,
NED | (38) |
| Nielsen et
al (1996) | 46 | 10 | 5 | NS | SMA, muscular
actin, vimentin, desmin, ER, PR: Positive; keratin, S-100:
Negative | Modified Radical
Vulvectomy | No | - | - | 30 months, alive,
NED | (38) |
| Nielsen et
al (1996) | 37 | 5 | 8 | NS | SMA, muscular
actin, vimentin, ER, PR: Positive; keratin, S-100, desmin:
Negative | Wide Local
Excision | Infiltrative | 3 months | Wider Excision;
positive margins again; modified radical vulvectomy | 36 months, alive,
NED | (38) |
| Nielsen et
al (1996) | 67 | 16 | 10 | NS | SMA, muscular
actin, vimentin, ER, PR: Positive; keratin, S-100, desmin:
Negative | NS | NS | - | Local, radiotherapy
chemotherapy | 7 months,
metastases to lungs and bones, died of disease | (38) |
| Nielsen et
al (1996) | 56 | 5.5 | 5 | NS | SMA, muscular
actin, vimentin: Positive; keratin, desmin, S-100, ER, PR:
Negative | NS | Infiltrative | NS | NS | NS | (38) |
| Torres et al
(2000) | 14 | 6 | - | - | - | Local Excision | - | +; 13 months | Wide Local Excision
+ Chemotherapy; Wide Local Excision + Radiotherapy 50 Gy;
Vulvectomy + Hysterectomy + Radiotherapy 65 Gy | 22 Years, alive,
NED | (13) |
| Rubin and Fletcher
(2000) | 26 | 1.2 | 6 | Yes, <50% | SMA, desmin:
Positive; Cam52, EMA: Negative | Local Excision | Infiltrative | 8 months & 35
months | NS | 62 months, NED | (57) |
| Rubin and Fletcher
(2000) | 30 | ND | 5 | No | SMA, HHF: Positive;
desmin, Cam52, EMA: Negative | Local Excision | NS | 19 months | NS | 11 years: 39 Local
Recurrences, died of disease | (57) |
| Rubin and Fletcher
(2000) | 32 | 2 | 10 | No | SMA, desmin:
Positive; Cam52, EMA: Negative | Wide Local
Excision | NS | - | - | 83 months, alive,
NED | (57) |
| Lösch et al
(2001) | 38 | - | - | - | ER, PR, Ki-67:
Positive; p53: Negative | - | - | - | - | 24 months, alive,
NED | (22) |
| Di Gilio et
al (2004) | 36 | 6 | 2 | NS | - | Wide Local Excision
+ Ipsilateral Lymphadenectomy | NS | - | - | 30 months, alive,
NED | (10) |
| Dewdney et
al (2005) | 36 | 5 | - | - | - | Vulvectomy | - | - | - | 13 months, alive,
NED | (3) |
| Rewal et al
(2005) | 81 | 5 | 35-40 | Yes | SMA: Positive | Wide Local
Excision | NS | 9 months | - | Died of unrelated
cause (cardiac failure) | (28) |
| Shankar et
al (2006) | 58 | 3 | NS | NS | Actin, desmin:
Positive | Wide Local
Excision | NS | - | - | 42 months, alive,
NED | (11) |
| González-Bugatto
et al (2009) | 52 | 6 | 21 | No | SMA, Vimentin,
Desmin, ER, PR: Positive; S-100, CK, CD31, p53, c-erbB-2,
Leukocyte Common Antigen: Negative | Hemivulvectomy +
ipsilateral lympadenectomy + radiotherapy 66.6 Gy +
chemotherapy | Yes | +; 12 months | Wide local
excision | 4 years, alive,
NED | (12) |
| Salehin et
al (2011) | 71 | 2 | 10 | NS | SMA, Ki-67:
Positive | Hemivulvectomy +
hysterectomy + salpingo- oophorectomy + inguinal
lymphadenectomy | No | NS | NS | NS | (4) |
| Mowers et al
(2014) | 48 | 4 & 10 (5 years
later) | NS | NS | SMA, desmin, ER,
PR: Positive | Incision and
drainage | Infiltrative | +; 5 years | Partial excision
and marsupialization; Left radical Hemivulvectomy + hysterectomy +
bilateral salpingo- oophorectomy + chemotherapy | 18 months, alive,
NED | (26) |
| Levy et al
(2014) | 57 | 2.5 | 16 | NS | SMA: Positive;
Desmin: Positive | Local excision +
Radical excision | Infiltrative -
Then, no residual disease | NS | NS | NS | (16) |
| Teramae et
al (2014) | 51 | 13.5 | 7-10 | NS | Desmin, Ki-67:
Positive | Local excision | No | - | - | 32 months, alive,
NED | (44) |
| Alnafisah and
Alfieri (2016) | 37 | 5 | NS | NS | SMA, ER, PR:
Positive | Wide local excision
+ Chemotherapy; Left radical vulvectomy + ipsilateral inguinal
lymphadenectomy | Residual
disease | 15 months | Left hemivulvectomy
+ ipsilateral iliac, inferior epigasric and obturator
lymphadenectomy | Lung metastatic
disease | (14) |
| Korkmaz et
al (2016) | 65 | 6 | 20 | Yes | Calponin, Ki-67:
Positive; S-100: Negative | Local Excision | NS | NS | - | 6 months, alive,
NED | (7) |
| Sayeed et al
(2018) | 72 | 11 | 8 | Yes | - | Wide local
excision | Infiltrative | NS* | NS* | aDied of disease | (58) |
| Sayeed et al
(2018) | 56 | 13.5 | 34 | Yes | - | Wide local
excision | Infiltrative | NS* | NS* | aDied of disease | (58) |
| Sayeed et al
(2018) | 68 | 5.5 | 23 | Yes | - | Wide local
excision | No | NS* | NS* | aDied of disease | (58) |
| Nath et al
(2019) | 38 | 8 | 4-5 | Yes | SMA, vimentin:
Positive; CK, desmin, S-100, HMB-45, CD34, ER, PR: Negative | Wide local
excision | - | - | - | 21 months, alive,
NED | (9) |
| Sameeta et
al, (2019) | 63 | 2.1 | 25 | No | SMA, desmin, ER:
Positive; S-100, cytokeratin AE1/AE3: Negative | Wide local excision
+ radiotherapy | Infiltrative
(focal) | NS | NS | NS | (59) |
| Saquib et al
(2020) | 63 | 2.8 | 22 | Yes- Focal | SMA, desmin,
caldesmon, Ki-67: Positive; CD117, CD4, vimentin, S100:
Negative | Local excision;
ipsilateral lymphadenectomy + ipsilateral hemivul- vectomy | Infiltrative
(focal); Negative: After the second operation | - | - | NS | (60) |
| Smith et al
(2020) | 46 | 3 | NS | NS | SMA, desmin:
Positive; cytokeratin AE1/AE3, p40, S100, myogenin, myo-D1,
caldesmon, CD34, STAT-6, TLE1: Negative | Local excision;
ipsilateral partial radical vulvectomy; posterior radical
vulvectomy, bilateral inguino-femoral lympadenectomy | Yes; after 3
operations: Negative | NS | NS | NS | (61) |
| Swanson et
al (2020) | 80 | 5.2 | 12 | Yes | NS | Resection +
chemotherapy | No | NS | NS | Liver metastasis at
the time of resection | (62) |
| Swanson et
al (2020) | NS | 9.7 | 36 | No | SMA: Diffusely
positive; h-Caldesmon: Multifocally positive; Desmine:
Negative | Resection | Infiltrative | NS | NS | NS | (62) |
| Swanson et
al (2020) | NS | 2.5 | 12 | No | Desmin, h-Caldesmon
and SMA: Diffusely positive; S100 protein: Negative | Resection | Infiltrative | NS | NS | NS | (62) |
| Akrivi et al
(present case) | 42 | 6.5 | 8-10 | No | Desmin, Caldesmon,
Vimentin, SMA, ER, PR: Positive; S100, myoglobulin, Keratin-116,
CD117, CD34, CD31: Negative | Wide local
excision | Focally
infiltrative margin | No | Wide local
Excision | 53 months, alive,
NED | - |
In conclusions, any vulvar lesion with unusual
characteristics in the Bartholin's gland area should be carefully
evaluated. Vulvar leiomyosarcomas localized in the Bartholin's
gland area could masquerade as chronic Bartholin's gland abscess or
as a benign lesion. For vulvar leiomyosarcomas, a wide local
excision of the mass with free surgical margins should be a good
option of surgery. This is particularly important to perform an
effective surgery in cases with these extremely rare neoplasms to
avoid recurrences and distal metastases. In case of recurrence, a
new extensive surgical resection of the lesion with ipsilateral
lympadenectomy and radiotherapy are suggested. Chemotherapy is
given in cases of distal metastases.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
CA, ZA, CP, AV were involved treated the patient.
SA, MV, ZA, CP, AV, EB, CA, conceived and designed this case
report. SA, MV, ZA, CP, AV, VKV, FNV, EB, CA, wrote the initial
draft of the report. SA, ZA, CP, AV, EB, CA, collected the clinical
data. EB performed histopathological and immunohistochemical
analysis and provided the related images. CA, ZA and EB were
responsible for confirming the assessment of the authenticity of
all the raw data. All authors have read and approved the final
version of the manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
The patient gave written informed consent for
publication of the case details and associated images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Aartsen EJ and Albus-Lutter CE: Vulvar
sarcoma: Clinical implications. Eur J Obstet Gynecol Reprod Biol.
56:181–189. 1994.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Curtin JP, Saigo P, Slucher B, Venkatraman
ES, Mychalczak B and Hoskins WJ: Soft-tissue sarcoma of the vagina
and vulva: A clinicopathologic study. Obstet Gynecol. 86:269–272.
1995.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Dewdney S, Kennedy CM and Galask RP:
Leiomyosarcoma of the vulva: A case report. J Reprod Med.
50:630–632. 2005.PubMed/NCBI
|
|
4
|
Salehin D, Haugk C, William M, Hemmerlein
B, Thill M, Diedrich K and Friedrich M: Leiomyosarcoma of the
vulva. Eur J Gynecol Oncol. 33:306–308. 2012.PubMed/NCBI
|
|
5
|
Duganzija T, Mikov MM, Salajic N, Nikolin
B, Trifunovic J and Ilic M: Increasing frequency of soft tissue
sarcomas in Vojvodina-comparison with the literature. Asian Pac J
Cancer Prev. 15:1011–1014. 2014.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Chokoeva AA, Tchernev G, Cardoso JC,
Tatterson JW, Dechev I, Valkanov S, Zanardelli M, Lotti T and
Wollina U: Vulvar sarcomas: Short guideline for histopathological
recognition and clinical management. Part I. Int J Immunopath
Pharmacol. 28:168–177. 2015.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Korkmaz V, Kurdoğlu Z, Kardag B, Arslanca
T, Caydere M and Ergun Y: A rare case of leiomyosarcoma localized
in the Bartholin's gland area and review of the literature. J
Obstet Gynaecol Res. 42:589–592. 2016.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Youssef A, Neji K, M'Barki M, Ben Amara F,
Malek M and Reziga H: Leimyoma of the vulva. Tunis Med. 91:78–80.
2013.PubMed/NCBI
|
|
9
|
Nath B, Gaikwad HS, Rajamani N, Chouhan M,
Sharma M and Topden S: Vulvar smooth muscle tumours: Case series
and review of the literature. J Clin Diagn Res. 13:QR01–QR04.
2019.
|
|
10
|
Di Gilio AR, Cormio G, Resta L, Carriero
C, Loizzi V, Parisi AM and Selvaggi L: Rapid growth of myxoid
leiomyosarcoma of the vulva during pregnancy: A case report. Int J
Gynecol Cancer. 14:172–175. 2004.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Shankar S, Todd PM, Rytina E and Crawford
RA: Leiomyosarcoma of the vulva. J Eur Acad Derm Venereol.
20:116–117. 2006.PubMed/NCBI View Article : Google Scholar
|
|
12
|
González-Bugatto F, Añόn-Requena
Lόpez-Guerrero MA, Báez-Perea JM, Bartha JL and Hervías-Vivancos B:
Vulvar leiomyosarcoma in Bartholin's gland area: A case report and
literature review. Arch Gynecol Obstet. 279:171–174.
2009.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Torres Lobaton A, Cruz Ortiz H, Rojo
Herrera G and Avila Medrano L: Sarcomas of the vulva. Report of 2
cases. Ginecol Obstet Mex. 68:429–434. 2000.PubMed/NCBI(In Spanish).
|
|
14
|
Alnafisah F and Alfieri J: Lung Metastasis
in a case of recurrent poorly differentiated leiomyosarcoma of the
Bartholin Gland: A case report and review of the literature.
Cureus. 8(e550)2016.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Youngstrom EA and Bartkowski DP: Vulvar
embyonal rhabdomyosarcoma: A case report. J Pediatr Urol.
9:e144–e146. 2013.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Levy RA, Winham WM, Bryant CS and Quick
CM: Smooth muscle neoplasms of the vulva masquerading as Bartholin
gland duct cysts. Proc (Bayl Univ Med Cent). 27:25–27.
2014.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Kuller JA, Zucker PK and Peng TC: Vulvar
leiomyosarcoma in pregnancy. Am J Obstet Gynecol. 162:164–166.
1990.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Davos I and Abell MR: Soft tissue sarcomas
of vulva. Gynecol Oncol. 4:70–86. 1976.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Tavassoli PA and Norris HJ: Smooth muscle
tumors of the vulva. Obstet Gynecol. 53:213–217. 1979.PubMed/NCBI
|
|
20
|
Newman PL and Fletcher CD: Smooth muscle
tumors of the extreme genitalia: Clinicopathological analysis of a
series. Histopathology. 18:523–529. 1991.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Grove A and Backman Nøhr S: Supperficial
perineal leiomyosarcoma in an adolescent female and review of the
literature including vulvar leiomyosarcomas. APMIS. 100:1081–1088.
1992.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Lösch A, Joura EA, Stani J, Breitenecker G
and Lahodny J: Leiomyosarcoma of the vulva. A case report. J Reprod
Med. 46:609–612. 2001.PubMed/NCBI
|
|
23
|
Kaufman RH and Gardner HL: Benigh
mesodermal tumors. Clin Obstet Gynec. 8:953–981. 1965.PubMed/NCBI
|
|
24
|
Reyad MM, Gazvani MR and Khine MM: A rare
case of primary leiomyoma of the vulva. J Obstet Gynecol. 26:73–74.
2006.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Tawfik O, Huntrakoon M, Collins J, Owiety
T, Seoud MA and Weed J Jr: Leiomyosarcoma of the vulva: Report of a
case. Gynaecol Oncol. 54:242–249. 1994.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Mowers EL, Shank JJ, Frisch N and Reynolds
RK: Myxoid leiomyosarcoma of the Bartholin Gland. Obstet Gynecol.
124 (Suppl 1):S433–S435. 2014.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Mensch LS, Trask CE and Eltabbakh GH:
Leiomyosarcoma of the vulva: A brief communication. Eur J Gynaecol
Oncol. 21(61)2000.PubMed/NCBI
|
|
28
|
Rawal N, Saridogan E, Khan N and Weekes A:
Leiomyosarcoma of the vulva in association with lichen sclerosus. J
Obstet Gynaecol. 25:87–88. 2005.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Bakri YN, Akhtar M, El-Senoussi M and
Wierzbicki R: Vulvar sarcoma: A report of four cases. Gynecol
Oncol. 46:384–390. 1992.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Tjalma WAA, Hauben EL, Deprez SME, Van
Marck EA and van Dam PA: Epitheliod sarcomaof the vulva. Gynecol
Oncol. 73:160–164. 1999.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Khoury-Collado F, Elliott KS, Lee YC, Chen
PC and Abulafia O: Merkel cell carcinoma of the Bartholin's gland.
Gynecol Oncol. 97:928–931. 2005.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Woida FM and Ribeiro-Silva A: Adenoid
cystic carcinoma of the Bartholin gland: An overview. Arch Pathol
Lab Med. 131:796–798. 2007.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Kacerovska D, Nemcova J, Petrik R, Michal
M and Kazakov DV: Lymphoepithelioma-like carcinoma of the Bartholin
gland. Am J Dermatopathol. 30:586–589. 2008.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Kyriazi MA, Carvounis EE, Kitsou M,
Arkadopoulos N, Nicolaidou E, Fotiou S and Smyrniotis V:
Myoepithelial carcinoma of the vulva mimicking Bartholin gland
abscess in a pregnant woman: Case report and review of literature.
Inter J Gynecol Pathol. 29:501–504. 2010.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Lee MY, Dalpiaz A, Schwamb R, Miao Y,
Waltzer W and Khan A: Clinical pathology of Bartholin's glands: A
review of the literature. Curr Urol. 8:22–25. 2014.
|
|
36
|
Morandeira C, Isusi M, Bárcena MV,
Lecumberri G and Ibañez A: Vulvar Leiomyosarcoma in Bartholin's
Gland. Eurorad Case. (14583)2017.
|
|
37
|
Vural B, Ozkan S, Yildiz K, Corakçi A and
Gürbüz Y: Malignant fibrous histiocytoma of the vulva: A case
report. Arch Gynecol Obstet. 273:122–125. 2005.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Nielsen GP, Rosenberg AE, Koerner FC,
Young RH and Scully RE: Smooth-muscle tumors of the vulva. A
clinicopathological study of 25 cases and review of the literature.
Am J Surg Pathol. 20:779–793. 1996.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Ramos P, Ruiz A, Carabias E, Piñero I,
Garzon A and Alvarez I: Müllerian adenosarcoma of the cervix with
heterogenous elements: Report of a case and review of the
literature. Gynecol Oncol. 84:161–166. 2002.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Gollard R, Kosty M, Bordin G, Wax A and
Lancey C: Two unusual presentations of Müllerian adenosarcoma: Case
reports, literature review and treatment considerations. Gynecol
Oncol. 59:412–422. 1995.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Kline TS, Kannan V and Kline IK:
Lymphadenopathy and aspiration biopsy cytology. Review of 376
superficial nodes. Cancer. 54:1076–1081. 1984.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Choi AH, Bolaris M, Nguyen DK, Panosyan
EH, Lasky JL III and Duane GB: Clinicocytopathological correlation
in an atypical presentation of lymphadenopathy with review of
literature. Am J Clin Pathol. 143:749–754. 2015.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Altinboğa AA and Yüce G: Fine-needle
aspiration cytology in the diagnosis of lymph nodes: Correlation
with histopathological diagnosis. South Clin Ist Euras. 30:52–59.
2019.
|
|
44
|
Teramae M, Fukuda T, Iami K, Yamauchi M,
Hashiguchi Y, Ichimura T, Yasui T and Sumi T: Leiomyosarcoma of the
vulva: A case report. Int J Reprod Contracept Obstet Gynecol.
3:225–228. 2014.
|
|
45
|
Guidozzi F, Sadan O, Koller AB and Marks
SR: Combined chemotherapy and irradiation therapy after radical
surgery for leiomyosarcoma of the vulva. A case report. S Afr Med
J. 71:327–328. 1987.PubMed/NCBI
|
|
46
|
Vincenzi B, Stacchiotti S, Collini P,
Pantano F, Rabitti C, Perrone G, Iuliani M, Baldi A, Badalamenti G,
Sanfilippo R, et al: Human equilibrative nucleoside transporter 1
gene expression is associated with gemcitabine efficacy in advanced
leiomyosarcoma and angiosarcoma. Br J Cancer. 117:340–346.
2017.PubMed/NCBI View Article : Google Scholar
|
|
47
|
Koehler K, Liebner D and Chen JL: TP53
mutational status is predictive of pazopanib response in advanced
sarcomas. Ann Oncol. 27:539–543. 2016.PubMed/NCBI View Article : Google Scholar
|
|
48
|
Sleijfer S, Gorlia T, Lamers C, Burger H,
Blay JY, Le Cesne A, Scurr M, Collin F, Pandite L, Marreaud S and
Hohenberger P: Cytokine and angiogenic factors associated with
efficacy and toxicity of pazopanib in advanced soft-tissue sarcoma:
An EORTC-STBSG study. Br J Cancer. 107:639–645. 2012.PubMed/NCBI View Article : Google Scholar
|
|
49
|
Schöffski P, Taron M, Jimeno J, Grosso F,
Sanfilipio R, Casali PG, Le Cesne A, Jones RL, Blay JY, Poveda A,
et al: Predictive impact of DNA repair functionality on clinical
outcome of advanced sarcoma patients treated with trabectedin: A
retrospective multicentric study. Eur J Cancer. 47:1006–1012.
2011.PubMed/NCBI View Article : Google Scholar
|
|
50
|
Thanopoulou E, Thway K, Khabra K and
Judson I: Treatment of hormone positive uterine leiomyosarcoma with
aromatase inhibitors. Clin Sarcoma Res. 4(5)2014.PubMed/NCBI View Article : Google Scholar
|
|
51
|
Yamaguchi M, Erdenebaatar C, Saito F,
Motohara T, Miyahara Y, Tashiro H and Katabuchi H: Long-term
outcome of aromatase inhibitor therapy with letrozole in patients
with advanced low-grade endometrial stromal sarcoma. Int J Gynecol
Cancer. 25:1645–1651. 2015.PubMed/NCBI View Article : Google Scholar
|
|
52
|
Zang Y, Dong M, Zhang K, Gao C, Guo F,
Wang Y and Xue F: Hormonal therapy in uterine sarcomas. Cancer Med.
8:1339–1349. 2019.PubMed/NCBI View Article : Google Scholar
|
|
53
|
George S, Feng Y, Manola J, Nucci MR,
Butrynski JE, Morgan JA, Ramaiya N, Quek R, Penson RT, Wagner AJ,
et al: Phase 2 trial of aromatase inhibition with letrozole in
patients with uterine leiomyosarcomas expressing estrogen and/or
progesterone receptors. Cancer. 120:738–743. 2014.PubMed/NCBI View Article : Google Scholar
|
|
54
|
Ricci S, Stone RL and Fader AN: Uterine
leiomyosarcoma: Epidemiology, contemporary treatment strategies and
the impact of uterine morcellation. Gynecol Oncol. 145:208–216.
2017.PubMed/NCBI View Article : Google Scholar
|
|
55
|
Møller KL, Nygaard Nielsen M and Trolle C:
Leiomyosarcoma vulvae. Acta Obstet Gynecol Scand. 69:187–189.
1990.PubMed/NCBI View Article : Google Scholar
|
|
56
|
Fried-Oginski W, Lovecchio JL, Farahani G
and Smilari T: Malignant myxoid sarcoma of the Bartholin gland in
pregnancy. Am J Obstet Gynecol. 173:1633–1635. 1995.PubMed/NCBI View Article : Google Scholar
|
|
57
|
Rubin BP and Fletcher CD: Myxoid
leiomyosarcoma of soft tissue, an underrecognized variant. Am J
Surg Pathol. 24:927–936. 2000.PubMed/NCBI View Article : Google Scholar
|
|
58
|
Sayeed S, Xing D, Jenins SM, Weisman PS,
Beuhler D, Warmke L, Uram-Tuculescu C, Bakkum-Gamez JN, Howitt BE,
Cortese C, et al: Criteria for risk stratification of vulvar and
vaginal smooth muscle tumors: An evaluation of 71 cases comparing
proposed classification systems. Am J Surg Pathol. 42:84–94.
2018.PubMed/NCBI View Article : Google Scholar
|
|
59
|
Sameeta F, Haque M, Akbar S, Zotto VD and
Kahn A: Leiomyosarcoma: A rare tumor of the vulva. Am J Clin
Pathol. 152 (Suppl 1):S37–S75. 2019.
|
|
60
|
Saquib S, Cherawala M, Abdel Rahman O and
Keloth TE: Leiomyosarcoma of the vulva mimicking as chronic
Bartholin cyst: A case report. Oman Med J. 35(e153)2020.PubMed/NCBI View Article : Google Scholar
|
|
61
|
Smith S, Bou Zgheib N, Vallejos A and Cuda
JD: Case report of leiomyosarcoma of the vulva: A rare pathology.
Marshall J Med. 6(6)2020.
|
|
62
|
Swanson AA, Howitt BE and Schoolmeester
JK: Criteria for risk stratification of vulvar and vaginal smooth
muscle tumors: A follow-up study with application to leiomyoma
variants, smooth muscle tumors of uncertain malignant potential,
and leiomyosarcomas. Hum Pathol. 103:83–94. 2020.PubMed/NCBI View Article : Google Scholar
|