1. Introduction
Breast cancer has been a focus of attention for
numerous years due to its high incidence and high mortality rate.
According to Global Cancer Statistics 2020, in that year, the newly
diagnosed cases of breast cancer accounted for 11.7% of all newly
diagnosed cases of cancer worldwide, and breast cancer-related
deaths accounted for 6.9% of all new cancer-related deaths
(1). Despite the growing
popularity of early screening for breast cancer and the development
of increasingly diverse and precise diagnostic and treatment
methods, numerous patients with breast cancer are still diagnosed
after metastases (2). In recent
years, the incidence and mortality rates of breast cancer have
remained high, according to survey data (3).
Distant metastasis is considered as a significant
cause of mortality in patients with breast cancer. Existing studies
have shown that 20-30% of patients with breast cancer may develop
metastasis after diagnosis and treatment of the primary tumor, and
~90% of cancer-related deaths are also due to metastasis (4). A previous study has revealed that
breast cancer metastases exhibit significant heterogeneity, with
lung, bone, and liver being the most common metastatic targets, and
the sites of metastasis significantly affecting patient prognosis
(5). Bone is a predilection site
for distant metastasis of breast cancer. Data indicate that 62.5%
of patients with initial metastatic breast cancer are diagnosed
with bone metastases, and the proportion of bone metastases among
patients with advanced breast cancer is as high as 75%. The
occurrence of bone metastases significantly affects the quality of
life of patients, and their life expectancy is only two to three
years after the diagnosis of bone metastases (6-8).
Patients with liver metastases are traditionally considered to have
a poor prognosis. Survey and follow-up statistics reveal that the
median overall survival of patients with liver metastases is 16.3
months, and the estimated five-year survival rate is only 8.5%
(9).
Lung metastases often occur in patients with
basal-like breast cancer, and lead to a short life expectancy, with
a median survival period of only 22 months after treatment. What is
more concerning is that lung metastases develop in 60-70% of
patients who succumb to breast cancer (10,11).
Due to the complexity of the metastasis process, there is currently
a lack of effective treatment for metastatic breast cancer.
Therefore, it is highly necessary and beneficial to conduct
in-depth research on the mechanism of breast cancer metastasis,
promote accurate diagnosis and prevent metastasis as early as
possible.
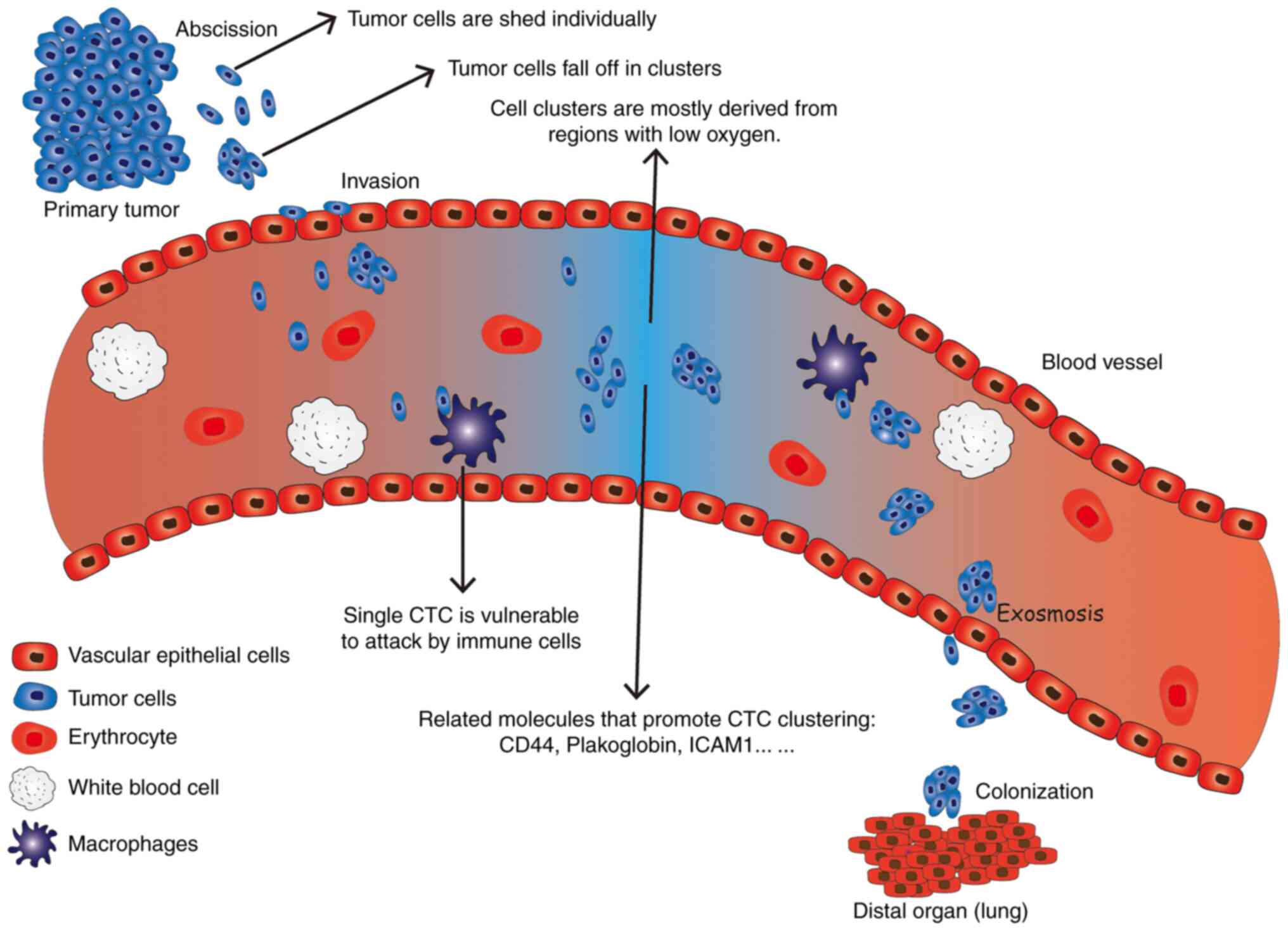
Circulating tumor cells (CTCs) are cancer cells that
have shed off from developed tumor tissues and entered the
vasculature or lymphatics, and are circulating in peripheral blood
vessels. CTCs are very rare in the blood, with only 1-10 CTCs per
milliliter of blood, compared with billions of blood cells
(12). However, they can now be
detected and counted by separating them from blood cells using
various enrichment methods (13,14).
CTC counts identify and quantify the epithelial cell adhesion
molecule (EpCAM) protein produced by epithelial tumor cells, making
it a useful diagnostic tool that may also aid in determining
prognosis and assessing treatment efficacy. It is currently
recognized that having ≥5 CTCs per 7.5 ml of blood is associated
with poorer overall survival and progression-free survival
(15). A previous study has
demonstrated that the number of CTCs is an independent predictor of
progression-free survival and overall survival in patients with
metastatic breast cancer prior to the initiation of treatment
(16). The CTC detection system
CellSearch (17) has been approved
by the Food and Drug Administration (FDA) for therapeutic
monitoring of metastatic breast cancer. In short, CTCs are
considered as the precursor cells for the formation of distant
metastasis, which promotes the occurrence of cancer metastasis. The
metastatic process experienced by CTCs generally includes
detachment from the primary tumor tissue, invasion into the blood
circulation, extravasation from the circulatory system, and finally
colonization in distant organs (18).
A recent study demonstrated that CTCs in the
circulating blood of patients with cancer exist not only in the
form of single cells, but also clusters. The size of CTC clusters
can range from two tumor cells to >100 cells. CTC clusters are
also known by various names such as circulating tumor microemboli,
circulating micrometastases, circulating tumor aggregates or tumor
cell clumps (19). CTC clusters
are rarer than single CTCs but may have a 50-fold higher potential
for distant metastasis than single CTCs (20).
Previous research on CTC has been limited by the
lack of CTC isolation technology. Due to their rarity in the blood
compared to blood cells, it has been difficult to isolate them
alive (21,22). However, with the development of CTC
detection and capture technology, the presence of CTC can be
detected in the blood of various patients with cancer (23-25).
Although the detection rate of CTC clusters is lower than that of
single CTCs, at least one CTC cluster can be detected in >50% of
the patients with cancer (26),
which suggests that most patients have a high risk of metastasis.
The formation of CTCs is the initiation of tumor metastasis, and
studying CTCs can provide a good understanding of the early
dynamics of breast cancer metastasis. Identifying CTCs in patients
at an early stage, and taking timely measures to inhibit their
generation and eliminate them, may have significant benefits in
suppressing breast cancer.
2. Formation of circulating tumor cell
clusters
As early as the 19th century, the Australian
pathologist John Ashworth introduced the concept of CTCs (27). In the 1970s, Nowell (28) revised the definition of CTCs
stating that they are cancer cells that originate from primary
tumors or metastatic tumors, acquire the ability to break away from
the basement membrane, invade the tissue matrix, and enter the
blood vessels.
With the advancement of CTC separation and detection
technology, the understanding of CTC is gradually improving. Using
multichromatographic lineage tracing, researchers have observed
that polyclonal dissemination from cell clusters account for
>90% of metastases in common mouse breast cancer models
(29). Although this cell mass in
animal models may not have come from the clonal growth of single
cells, it fully shows that metastasis through cell clusters is a
common means of cancer metastasis. CTC clusters have become the
focus of researchers due to their stronger ability to promote
metastasis than single CTCs. The source of CTC clusters has aroused
the interest of researchers. Currently, there are two main views on
the source of CTC clusters. The first supports that CTC clusters
are directly shed from the primary tumor tissue, and the second
suggests that they originate from the accumulation of single CTCs
in blood vessels (30,31). Currently, researchers are more
inclined to consider that the aggregation effect occurs after tumor
cells fall off, and various signaling pathways and related
molecules have been identified to be associated with the
aggregation of CTCs. Most of these related pathways and molecules
causing CTC aggregation are also related to breast cancer
metastasis. This suggests that the formation of CTC clusters is
strongly associated with breast cancer metastasis (19).
The high expression of cell-cell adhesion proteins
is considered an important factor for the formation of CTC clusters
in the blood. Plakoglobin, a key component of cell adhesion, can
promote metastasis by stimulating the formation of tumor cell
clusters in invasive micropapillary carcinoma of the breast (IMPC)
(32). Studies have revealed that
plakoglobin activates the PI3K/Akt/Bcl-2 signaling pathways
promoting the formation of tumor cell clusters in IMPCs (32). In addition, in vitro
experiments have shown that the formation of clusters greatly
inhibits the loss of cells compared to single cells in both
adherence and suspension cultures, making CTC clusters more likely
to survive (32). There are
numerous studies on how plakoglobin is involved in the signaling
pathways related to the prognosis of breast cancer. For example,
KRT13 promotes the differentiation and metastasis of breast cancer
stem cells through the plakoglobin/c-Myc signaling pathway
(33). In vitro experiments
have confirmed that overexpression of KRT13 can promote the
proliferation, migration and invasion ability of MCF7 cells, and
after inoculation of MCF7 cells overexpressing KRT13, accelerated
tumor growth and increased distant metastasis were observed in
vivo (33). Additionally,
detecting the plakoglobin status in vivo can also help to
predict the prognosis of patients with metastatic breast cancer. By
counting CTCs and CTC clusters in patients with metastatic breast
cancer and analyzing their protein expression, it has been
identified that the number of CTC clusters in the bodies of
patients with positive plakoglobin is markedly higher than that of
patients with negative plakoglobin. The abundant presence of CTC
clusters and high expression of plakoglobin, have been thus
revealed to be significantly associated with the poor prognosis of
patients with cancer (34).
CD44 is a non-kinase cell-surface transmembrane
glycoprotein that is involved in cell-cell interactions, cell
adhesion and migration. CD44 mediates cell aggregation through
affinity between tumor cells of the same type (30,35).
Cells that overexpress CD44 have various characteristics of cancer
stem cells. The CD44 gene produces multiple isoforms after
undergoing complex alternative splicing, and the interaction
between these isoforms and different ligands can stimulate numerous
cancer-related signals. For example, CD44v8-10, one of the CD44
variant subtypes, can promote MCF-7 cell migration and sphere
formation (36). CD44 is therefore
widely recognized as a tumor stem cell marker in various cancers
(35). A previous study revealed
that CD44 can guide the accumulation of CTCs and promote the
metastasis of breast cancer (30).
CD44 mediates tumor cell aggregation through intercellular
homophilic interactions and initiates CD44-PAK2 interaction to
further activate focal adhesion kinase (FAK) signal, which is a
non-receptor tyrosine kinase. Literature previously reported that
FAK can mediate the cell signal transduction by the integrin and
growth factor receptors and regulate various cellular functions
including adhesion and proliferation after activation (30,37).
CD44 can also mediate the aggregation of tumor cells through the
epidermal growth factor receptor (EGFR), a tyrosine kinase. The
combination of targeting HER2 and EGFR in the treatment of
triple-negative breast cancer (TNBC) was reported in a previous
study (38). A recent study has
demonstrated that EGFR can enhance CD44-mediated tumor cell
aggregation during the formation of CTC clusters. CD44 can in turn
regulate the stability of EGFR during cell separation and
circulation (39). The tumor
suppressor microRNA-30c (miR-30c) is transcriptionally regulated by
GATA3 in breast tumors and directly targets TWF1 to play a role in
drug resistance (40). Another
study has confirmed that CD44 is the direct target of miR-30c,
while EGFR is the downstream target of the miR-30c-CD44 pathway
(39). MiR-30c can become a
negative regulator of CTC accumulation and lung metastasis by
targeting CD44 and its downstream effector EGFR. Inhibiting EGFR
can block the accumulation of tumor stem cells in TNBC and lung
metastasis in vivo (39,40).
Intercellular adhesion molecule 1 (ICAM1) is a cell
surface glycoprotein and an adhesion receptor. Similar to CD44,
ICAM1 can also guide the accumulation of the same type of tumor
cells and promote the formation of CTC clusters (41). A recent study has also determined
that ICAM1 not only guides tumor cell aggregation through
homophilic ICAM1-ICAM1 interactions, but also promotes homotypic
tumor cell clustering to form CTC clusters. Moreover, it can drive
tumor-endothelial heterotypic cell adhesion, and knockdown of the
expression of ICAM1 significantly inhibits the aggregation of tumor
cells (41). ICAM1 also plays a
role in recruiting chemotactic leukocytes from circulating sites to
inflammatory sites. Additionally, ICAM1 serves as a biosensor to
transmit intracellular and extracellular signals, regulating cell
functions such as the barrier properties of epithelial cells and
endothelial cells and cell migration (42). Heparanase (HPSE) is an
endoglycosidase associated with metastasis, which can participate
in cell adhesion through its non-enzymatic activity. HPSE promotes
the formation of CTC clusters and regulates the FAK-Src-paxillin
signaling pathway and the expression of ICAM1(43). The coordinated effect between these
adhesion proteins and enzymes may jointly promote the aggregation
of tumor cells. These findings highlight the importance of adhesion
proteins and enzymes in the formation of CTC clusters and the
promotion of metastasis in breast cancer.
In addition to the aforementioned related molecules
that can promote the accumulation of CTCs, changes in the tumor
microenvironment can also lead to the accumulation of tumor cells.
Studies (31) have shown that
hypoxia in the tumor microenvironment is a triggering factor for
the upregulation of cell adhesion components and CTC aggregation.
To track breast cancer cells involved in breast cancer progression
in a mouse model, a research group dynamically tracked spontaneous
hypoxic events by expressing the reporter vector, HIF1a-expressing
eYFP, which is an expression-enhancing yellow fluorescent protein
that can only be generated under the control of hypoxic-response
element repeats. They observed that 80.6% of the CTC clusters were
positive for HIF1a (31). This
indicates that most of the CTC clusters originate from hypoxic
regions and are undergoing hypoxic processes, compared with the
normal oxygen content of individual CTCs. This study also revealed
that hypoxic CTC clusters have higher transfer ability than those
with normal oxygen levels (31).
Although there are few studies on hypoxia-triggered CTC
aggregation, there are numerous studies on hypoxia-mediated
angiogenesis and breast cancer metastasis. For example, the
interaction of HIF-2, desmoglein2 and other factors with a hypoxic
environment promotes angiogenesis and the metastatic process of
breast cancer (44,45), including the accumulation of
CTCs.
In summary, as revealed in Fig. 1, it is evident that CTCs can
produce an aggregation effect under the joint action of different
signaling pathways and the tumor microenvironment, leading to a
significant enhancement of their metastatic potential. However,
further research is required to explore effective strategies to
trigger the aggregation of CTCs to inhibit the spread of breast
cancer metastasis.
3. Comparison of single CTCs and CTC
cluster
It is widely recognized that CTCs in breast cancer,
similar to other cancers, exhibit significant heterogeneity
(46). This heterogeneity can be
observed not only among single CTCs but also between single CTCs
and CTC clusters, with differences in both cell structure and
function (47). Of particular
interest to researchers is the higher metastatic potential of CTC
clusters and the differences between individual CTCs and CTC
clusters, including their respective methylation levels, stem cell
characteristics, survival advantages, and immune escape, which are
all closely related to their ultimate metastatic potential.
The DNA of stemness and proliferation-associated
transcription factors in CTC clusters exhibits hypomethylation. DNA
methylation is an important epigenetic factor. By isolating CTCs
and CTC clusters from the blood of patients with breast cancer and
mouse xenograft models, researchers conducted whole-genome sulfite
sequencing at single-cell resolution, to analyze genome-wide DNA
methylation of individual CTCs and CTC clusters (48). The results revealed that,
transcription factors associated with stemness and proliferation,
including OCT4, NANOG, SOX2, and SIN3A, were specifically
hypomethylated in CTC clusters (48), which is suggestive of a connection
between CTC aggregation and DNA methylation that promotes stemness
and metastasis. A previous study has revealed that genome-wide
hypomethylation is associated with the expression of
proto-oncogenes and malignant transformation of tumors (49). In breast cancer, the promoters of
certain tumor suppressor genes are hypermethylated. For example,
ADAM family member ADAM23, which can participate in neuronal
differentiation, is usually downregulated in various types of
cancer and is considered to be a cancer suppressor gene. It is
observed to express epigenetic silencing by promoting
hypermethylation in breast cancer (50). The hypomethylation status of
transcription factors associated with stemness and proliferation in
CTC clusters increases the expression of proteins related to cell
stemness and proliferation, thus, CTC clusters have strong
proliferation and differentiation capabilities. This can promote
the overall process of metastasis mediated by CTC clusters
macroscopically, thereby rendering it a crucial area of research in
breast cancer.
Recent research on circulating tumor intercellular
proteins have demonstrated that cells in CTC clusters express more
adhesion proteins, which contributes to their increased
tumorigenicity. Researchers performed RNA sequencing on breast
cancer cells with different migration phenotypes isolated from the
same parent, characterized the adhesion behavior between cells, and
calculated the respective adhesion scores. It was found that cells
with weak migration phenotypes exhibited a higher adhesion score,
indicating increased expression of E-cadherin. Moreover, cells with
a weak migratory phenotype formed more CTC clusters in vivo
(51), suggesting that CTC
clusters express more cell-cell adhesion proteins, consistent with
the understanding that the CTC clusters form as multiple CTC
adhesion aggregates. Through the suspension culture of MDA-MB-231
breast cancer cells, researchers observed that these cells had a
clear tendency to aggregate over time during the culture process,
and the levels of fibronectin (FN) and desmosomal proteins also
increased in a time-dependent manner during the aggregation
process. Furthermore, the increase in the level of FN and
desmosomal protein plays a key role in cell aggregation, and the
expression of FN and desmosomal protein in CTC after aggregation
was also significantly enhanced compared with that of single CTCs
(52). The strength of cell-cell
adhesion in CTC clusters may endow them with a better chance of
survival in the circulation and thus higher tumorigenicity
(53). Taken together, the
increased expression of adhesion proteins in CTC clusters play a
significant role in their tumorigenicity and ability to survive in
circulation. These findings provided valuable insights into the
mechanisms underlying CTC cluster formation and into the
development of more effective therapeutic strategies to prevent or
target CTC clusters in breast cancer.
The acquisition of apoptosis resistance can provide
CTC clusters with a stronger survival advantage than single CTCs in
the same environment (54).
Anoikis is a form of apoptosis that is induced by the loss of
interaction between cells and the extracellular matrix, and CTCs
that enter the bloodstream from primary cancer tissues must acquire
anoikis resistance to survive in the absence of matrix attachment
and achieve successful distant metastasis (52). A previous study on lung cancer cell
line A549 revealed that it exhibited resistance to anoikis after
cell aggregation (55). Similarly,
another study demonstrated that breast cancer cells exhibit the
same phenomenon (56). In
vitro experiments showed that the acquisition of this anoikis
resistance can promote distant metastasis of cancer (52), and researchers have detected high
expression of anti-apoptotic BCL2 protein in CTC clusters,
indicating the presence of this resistance (56). Collectively, these findings suggest
that maintaining cell-cell adhesion contributes to the formation of
cell aggregates, which in turn can endow CTC clusters with anoikis
resistance, leading to a stronger survival advantage than single
CTCs in the same environment. Therefore, the acquisition of anoikis
resistance is a crucial factor in the formation and survival of CTC
clusters, and these findings provide valuable insights into the
mechanisms underlying the formation and metastasis of CTC clusters
in breast cancer. They may also contribute to the development of
more effective therapeutic strategies aimed at preventing or
targeting CTC clusters.
Recent studies have shown that cells in CTC clusters
exhibit more stemness characteristics, which may contribute to
their increased metastatic potential (57). Cancer stem cells are considered the
primary drivers of metastasis, and CTC aggregation has been shown
to confer stem cell properties on cells (58). In a previous study regarding colon
cancer, cancer stem cell cluster stemness genes, such as CD133 and
Lgr5, were expressed at higher levels in cell clusters than in
single cells and contributed to the formation of colon cancer cell
clusters (59). Similar findings
have been observed in breaster cancer. In zebrafish embryos and
mouse models and in vitro experiments studying the
metastatic ability and molecular mechanism of breast cancer CTCs
and CTC clusters, it was revealed that genes associated with the
cell cycle and stemness were upregulated in CTC clusters (60). Moreover, aforementioned CD44, a
surface glycoprotein on cancer stem cells that promotes CTC
aggregation (61), is
overexpressed in CTC clusters and is involved in the maintenance of
stem cell signals of various tumor cells. CD44 signals can mediate
the expression of lipoprotein lipase in breast cancer stem cells
promoting tumorigenesis (62).
Compared to single CTCs, the aggregation of CTCs may provide cancer
stem cells with the protection needed to travel to metastatic sites
in order to form distant metastases more efficiently. In summary,
the stemness characteristics observed in cells within CTC clusters
may contribute to their increased metastatic potential,
highlighting the importance of understanding the underlying
mechanisms of CTC cluster formation and the role of cancer stem
cells in this process.
The clustering of CTCs is a crucial factor in immune
escape and contributes to their increased metastatic potential.
CTCs exhibit a marked ability to evade the immune system during
metastasis, and the immune escape mediated by CTC clusters is one
of the reasons they are more likely to form metastases compared
with single CTCs (63,64). A previous study revealed that CTC
clusters recruit more immunosuppressive cells in order to protect
them from being attacked by antitumor immune cells such as natural
killer (NK) cells. CTC clusters are less sensitive to NK-mediated
immunosuppression than single CTCs, and this is related to the fact
that the aggregation of CTCs improves cell adhesion and epithelial
gene expression (65). The immune
escape of CTCs in the blood circulation and metastatic sites
involves multiple mechanisms. For example, highly expressed PD-L1
on the surface of CTCs can mediate the immunosuppressive effect of
regulatory T cells (63), and the
association between neutrophils and CTCs also promotes cell cycle
progression in the bloodstream and increases the metastatic
potential of CTCs (66).
As revealed in Table
I, CTC clusters are different from single CTCs in various
aspects, providing them with a greater survival advantage during
metastasis. This increased survival advantage makes CTC clusters
more likely to metastasize and become an important target for early
diagnosis, prognostic detection indication, and clinical treatment.
Overall, understanding the mechanisms underlying CTC cluster
formation and immune escape is essential for the development of
more effective therapeutic strategies aimed at preventing or
targeting CTC clusters in breast cancer.
 | Table IComparison of single CTCs and CTC
clusters. |
Table I
Comparison of single CTCs and CTC
clusters.
| Type of CTC | Description | DNA of stemness and
proliferation-associated transcription factors | Cell-cell adhesion
proteins | Anoikis
resistance | Stemness
characteristics | Immune escape |
|---|
| CTC clusters | The size of CTC
clusters can range from two tumor cells to >100 cells; it exists
in clusters | • OCT4, NANOG,
SOX2, SIN3A as well as the DNA of other stemness and
proliferation-associated transcription factors are specifically
hypomethylated | Expression of
intercellular adhesion proteins such as E-cadherin, fibronectin and
desmosomal protein are significantly increased | Anti-apoptotic
protein BCL2 exhibits high expression | • Stem genes such
as CD133 and Lgr5 are highly expressed in cell clusters | • CTC clusters are
insensitive to NK cell-mediated immunity due to cell adhesion and
upregulation of epithelial gene expression |
| | | | | | • The cell cycle
and stemness are upregulated in CTC clusters | • The high
expression of PD-L1 mediates the immunosuppressive effect of
Treg |
| | | • Cancer suppressor
gene ADAM23 expresses epigenetic silencing by promoting
hypermethylation | | | • The surface
glycoprotein on cancer stem cells CD44 is expressed at a high level
in CTC clusters | |
| Single CTCs | Cancer cells that
have shed off from developed tumor tissues and entered the
vasculature or lymphatics, and are circulating in peripheral blood
vessels | Compared to CTC
clusters, the DNA of stemness and proliferation-associated
transcription factors is methylated in a single CTC, resulting in
epigenetic silencing | Expression of
single CTC surface adhesion protein is low, and there is a tendency
to increase with cell agglomeration fibronectin and desmosomal
proteins during suspension culture | A single CTC
lacking anoikis resistance has a higher number of apoptosis cells
in the circulatory system, which affects the transfer
efficiency | A single CTC lacks
protection against cancer stem cells in the circulatory system and
is more difficult to form distant metastases | It is difficult for
a single CTC to escape the attack of the immune system and the
survival rate is low |
4. Isolation and enrichment of CTC and the
clinical significance for patients with metastatic breast
cancer
Various methods have been developed for the
isolation of CTCs based on their physical or chemical
characteristics that differ from those of other cells. Examples of
these methods include microfluidic separation technology based on
the mechanism of magnetophoresis (67,68),
and size-based microfilters that capture CTCs according to the
their size and hardness compared to other cells (69). The choice of separation method
depends on various factors, including the type of cancer and the
equipment available. For breast cancer, the CellSearch system, is
the most widely used clinical method for the monitoring of
metastatic breast cancer. This system has been approved by the FDA
and automates the processing of CTC counts, thus playing a
significant role in monitoring metastatic cancer, predicting
progression-free survival and overall survival. The CellSearch
system works by counting CTCs that are positive for EpCAM and
keratin-positive, and only requires 7.5 ml of peripheral blood for
each test. The separation process invovles two parts, which are
completed by different instruments. The first step is AutoPrep,
which automatically captures CTCs, followed by immunostaining of
the captured cells, and then the semi-automated fluorescence
microscopy CellTrack Analyzer distinguishes white blood cells from
CTCs by immunofluorescence staining of captured cells with
anti-keratin and anti-CD45 antibodies. Experiments have revealed
that the CellSearch system has a sensitivity of >90% for the
detection of EpCAM and keratin-positive cancer cells (70). However, the high purchase price of
the equipment and the high cost of a single test, as well as the
fact that the detection of CTCs is a long-term dynamic process, has
put great economic pressure on patients. Therefore, numerous
medical institutions and patients do not choose to isolate CTCs
using this method.
The detection of CTCs has become an increasingly
important tool in clinical practice for in vitro
non-invasive early diagnosis, individualized treatment, and
prognostic prediction. However, the clinical application of CTCs
faces numerous challenges, including the cost and efficiency of
isolating CTCs and the difficulty in standardizing the
identification of CTCs, which limits their clinical utility
(71). As previosuly reported
(72) numerous clinical trials and
studies have demonstrated that the presence of CTCs is
significantly associated with poor prognosis in patients with
various cancers. The clinical monitoring of the number and status
of CTCs is therefore of great significance in formulating treatment
strategies and predicting the prognosis of patients with metastatic
breast cancer. In-depth studies of CTCs and their clinical
applications will help guide the development of new diagnostic and
therapeutic strategies, inhibit cancer metastasis, and ultimately
benefit patients. Despite the current limitations, the close
association between CTCs and clinical practice provides a promising
avenue for improving the diagnosis and treatment of breast
cancer.
Current treatment strategies for breast cancer
mainly target the primary tumor tissue and have limited effect on
the initial cells in the initial stage of metastasis (73), which increase the likelihood of
metastasis. Thus, developing treatment strategies that target CTCs
has become a new direction for breast cancer treatment, and there
are increasing clinical applications. Inhibiting the metastatic
ability of CTCs by targeting them with drugs can be an effective
therapeutic approach for patients with breast cancer with a high
risk of metastasis. For patients with early-stage breast cancer,
cluster-targeted therapy is currently being developed to identify
CTC clusters in patient groups. It helps identify patients with
high risk of metastasis and initiates anti-cluster treatment early,
which can reduce the ability of cancer cells to metastasize and
prevent the occurrence of metastasis (74). For patients with HER2-positive
metastatic breast cancer, targeted HER2 therapy can significantly
decrease the total number of CTCs in patients (75). Furthermore, the status of CTCs can
predict the benefit of radiotherapy on overall survival in patients
with early breast cancer and detectable CTCs (76). CTC count can be a reliable
biomarker method (77) to guide
treatment selection between single-agent endocrine therapy and
chemotherapy in patients with hormone receptor-positive,
ERBB2-negative metastatic breast cancer (78). The combined monitoring of
circulating tumor DNA and CTCs after surgery can also help with the
prediction of the risk of disease recurrence (79). Overall, the development of
treatment strategies that target CTCs offers a promising approach
to breast cancer treatment, and the combined monitoring of CTCs and
other biomarkers has the potential to improve prognosis and
treatment selection for patients with breast cancer.
The presence of CTCs is strongly associated with
poor prognosis of patients with breast cancer (80). CTCs serve as a non-negligible
prognostic biomarker in metastatic breast cancer (81). CTC counts based on the CellSearch
detection platform (70) have been
revealed to be an independent predictor of survival in patients
with metastatic breast cancer (82). In HER2-negative metastatic breast
cancer, epithelial-mesenchymal transition marker-based CTC
detection can identify disease progression and treatment resistance
in advance, and combined criteria considering both CTC count and
the proportion of CTCs expressing mesenchymal markers are
significantly associated with prognosis (83). A longitudinal assessment of CTCs
and CTC clusters in patients with metastatic breast cancer showed
an increase in their prognostic value over time (84). The status of CTCs changes
dynamically during treatment of metastatic breast cancer, which
affects prognostic judgements. Therefore, the timing of CTC
detection must be well grasped when using CTCs to assess prognosis.
A previous study revealed that the CTC counts and status in the
later stages of treatment were more reliable for predicting the
prognosis status of patients (85). In addition to metastatic breast
cancer, the detection rate of CTC is 39% in non-metastatic
inflammatory breast cancer, which has strong independent prognostic
value (86).
5. Summary and prospects
CTCs are shed from primary tumors or metastases and
enter the bloodstream, playing a crucial role in the understanding
of breast cancer and other cancer metastasis mechanisms.
Investigating CTCs is of great significance due to their ability to
initiate tumor metastasis in distant organs. Understanding the
molecular mechanisms through which CTCs promote tumor metastasis is
an important area of research. CTCs have been identified to form
clusters, which exhibit a higher metastatic potential than single
CTCs. This enhanced potential can be attributed to differences in
the expression of intercellular adhesion proteins, levels of DNA
methylation, anti-apoptotic properties, and immune escape
mechanisms. Consequently, targeting CTC clusters has emerged as a
novel approach for intervening in breast cancer metastasis.
Targeting CTC clusters offers a promising strategy
for reducing the risk of breast cancer metastasis, whether by
disrupting their collective shedding or dissociating them in the
circulation. The distinctive characteristics exhibited by CTC
clusters, including altered intercellular adhesion protein
expression, DNA methylation patterns, anti-apoptotic properties,
and immune escape mechanisms, confer a survival advantage and
ultimately contribute to their heightened metastatic potential.
Currently, the clinical application of CTCs
primarily revolves around predicting treatment efficacy and
prognosis based on CTC enumeration and characterization. Combined
assessment of CTCs with other biomarkers enables effective
monitoring of disease progression and prognosis prediction.
However, the high cost associated with CTC isolation and monitoring
limits their widespread clinical implementation. Future
advancements in CTC detection technology should focus on achieving
higher enrichment efficiency and standardization to meet the
clinical demands. Continued progress in the clinical application of
CTCs holds the potential to significantly benefit patients with
breast cancer.
Acknowledgements
Not applicable.
Funding
Funding: The present study was supported by the Project of
Shandong Traditional Chinese Medicine Classic Famous Prescription
Collaborative Innovation (grant no. 2019KF203).
Availability of data and materials
Not applicable.
Authors' contributions
This review article was initiated and written by JZ.
ZL, YC, YL, HS, LH and YD contributed to the review process by
reviewing and editing the manuscript to varying degrees. Data
authentication is not applicable. All authors have read and
approved the final manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Sung H, Ferlay J, Siegel RL, Laversanne M,
Soerjomataram I, Jemal A and Bray F: Global cancer statistics 2020:
GLOBOCAN estimates of incidence and mortality worldwide for 36
cancers in 185 countries. CA Cancer J Clin. 71:209–249.
2021.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Park M, Kim D, Ko S, Kim A, Mo K and Yoon
H: Breast cancer metastasis: Mechanisms and therapeutic
implications. Int J Mol Sci. 23(6806)2022.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Giaquinto AN, Sung H, Miller KD, Kramer
JL, Newman LA, Minihan A, Jemal A and Siegel RL: Breast cancer
statistics, 2022. CA Cancer J Clin. 72:524–541. 2022.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Liang Y, Zhang H, Song X and Yang Q:
Metastatic heterogeneity of breast cancer: Molecular mechanism and
potential therapeutic targets. Semin Cancer Biol. 60:14–27.
2020.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Wang H, Zhang C, Zhang J, Kong L, Zhu H
and Yu J: The prognosis analysis of different metastasis pattern in
patients with different breast cancer subtypes: A SEER based study.
Oncotarget. 8:26368–26379. 2017.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Xiong Z, Deng G, Huang X, Li X, Xie X,
Wang J, Shuang Z and Wang X: Bone metastasis pattern in initial
metastatic breast cancer: A population-based study. Cancer Manag
Res. 10:287–295. 2018.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Tulotta C and Ottewell P: The role of
IL-1B in breast cancer bone metastasis. Endocr Relat Cancer.
25:R421–R434. 2018.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Tahara RK, Brewer TM, Theriault RL and
Ueno NT: Bone metastasis of breast cancer. Adv Exp Med Biol.
1152:105–129. 2019.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Pentheroudakis G, Fountzilas G, Bafaloukos
D, Koutsoukou V, Pectasides D, Skarlos D, Samantas E, Kalofonos HP,
Gogas H and Pavlidis N: Metastatic breast cancer with liver
metastases: A registry analysis of clinicopathologic, management
and outcome characteristics of 500 women. Breast Cancer Res Treat.
97:237–244. 2006.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Jin L, Han B, Siegel E, Cui Y, Giuliano A
and Cui X: Breast cancer lung metastasis: Molecular biology and
therapeutic implications. Cancer Biol Ther. 19:858–868.
2018.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Dan Z, Cao H, He X, Zhang Z, Zou L, Zeng
L, Xu Y, Yin Q, Xu M, Zhong D, et al: A pH-Responsive host-guest
nanosystem loading succinobucol suppresses lung metastasis of
breast cancer. Theranostics. 6:435–445. 2016.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Boya M, Chu CH, Liu R, Ozkaya-Ahmadov T
and Sarioglu AF: Circulating tumor cell enrichment technologies.
Recent Results Cancer Res. 215:25–55. 2020.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Di Lorenzo G, Zappavigna S, Crocetto F,
Giuliano M, Ribera D, Morra R, Scafuri L, Verde A, Bruzzese D,
Iaccarino S, et al: Assessment of total, PTEN(-), and AR-V7(+)
circulating tumor cell count by flow cytometry in patients with
metastatic castration-resistant prostate cancer receiving
enzalutamide. Clin Genitourin Cancer. 19:e286–e298. 2021.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Ning D, Cui K, Liu M, Ou Y, Wang Z, Zou B,
Shen Y, Lu X, Li S and Li P: Comparison of CellSearch and
Circulating Tumor Cells (CTC)-Biopsy systems in detecting
peripheral blood circulating tumor cells in patients with gastric
cancer. Med Sci Monit. 27(e926565)2021.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Schuster E, Taftaf R, Reduzzi C, Albert
MK, Romero-Calvo I and Liu H: Better together: Circulating tumor
cell clustering in metastatic cancer. Trends Cancer. 7:1020–1032.
2021.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Cristofanilli M, Budd GT, Ellis MJ,
Stopeck A, Matera J, Miller MC, Reuben JM, Doyle GV, Allard WJ,
Terstappen LW and Hayes DF: Circulating tumor cells, disease
progression, and survival in metastatic breast cancer. N Engl J
Med. 351:781–791. 2004.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Andree KC, van Dalum G and Terstappen LW:
Challenges in circulating tumor cell detection by the CellSearch
system. Mol Oncol. 10:395–407. 2016.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Pineiro R: Introduction-Biology of breast
cancer metastasis and importance of the analysis of CTCs. Adv Exp
Med Biol. 1220:1–10. 2020.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Pineiro R, Martinez-Pena I and Lopez-Lopez
R: Relevance of CTC clusters in breast cancer metastasis. Adv Exp
Med Biol. 1220:93–115. 2020.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Aceto N, Bardia A, Miyamoto DT, Donaldson
MC, Wittner BS, Spencer JA, Yu M, Pely A, Engstrom A, Zhu H, et al:
Circulating tumor cell clusters are oligoclonal precursors of
breast cancer metastasis. Cell. 158:1110–1122. 2014.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Alix-Panabieres C and Pantel K: Challenges
in circulating tumour cell research. Nat Rev Cancer. 14:623–631.
2014.PubMed/NCBI View
Article : Google Scholar
|
|
22
|
Yu M, Stott S, Toner M, Maheswaran S and
Haber DA: Circulating tumor cells: Approaches to isolation and
characterization. J Cell Biol. 192:373–382. 2011.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Ahn JC, Teng PC, Chen PJ, Posadas E, Tseng
HR, Lu SC and Yang JD: Detection of circulating tumor cells and
their implications as a biomarker for diagnosis, prognostication,
and therapeutic monitoring in hepatocellular carcinoma. Hepatology.
73:422–436. 2021.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Chemi F, Mohan S and Brady G: Circulating
tumour cells in lung cancer. Recent Results Cancer Res.
215:105–125. 2020.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Hu M, Wang Z, Wu Z, Ding P, Pei R, Wang Q
and Xing C: Circulating tumor cells in colorectal cancer in the era
of precision medicine. J Mol Med (Berl). 100:197–213.
2022.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Cho EH, Wendel M, Luttgen M, Yoshioka C,
Marrinucci D, Lazar D, Schram E, Nieva J, Bazhenova L, Morgan A, et
al: Characterization of circulating tumor cell aggregates
identified in patients with epithelial tumors. Phys Biol.
9(016001)2012.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Ashworth T: R. A case of cancer in which
cells similar to those in the tumours were seen in the blood after
death. Aust Med J. 14(146)1869.https://cir.nii.ac.jp/crid/1573105974858034560.
|
|
28
|
Nowell PC: The clonal evolution of tumor
cell populations. Science. 194:23–28. 1976.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Cheung KJ, Padmanaban V, Silvestri V,
Schipper K, Cohen JD, Fairchild AN, Gorin MA, Verdone JE, Pienta
KJ, Bader JS and Ewald AJ: Polyclonal breast cancer metastases
arise from collective dissemination of keratin 14-expressing tumor
cell clusters. Proc Natl Acad Sci USA. 113:E854–E863.
2016.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Liu X, Taftaf R, Kawaguchi M, Chang YF,
Chen W, Entenberg D, Zhang Y, Gerratana L, Huang S, Patel DB, et
al: Homophilic CD44 interactions mediate tumor cell aggregation and
polyclonal metastasis in patient-derived breast cancer models.
Cancer Discov. 9:96–113. 2019.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Donato C, Kunz L, Castro-Giner F,
Paasinen-Sohns A, Strittmatter K, Szczerba BM, Scherrer R, Di
Maggio N, Heusermann W, Biehlmaier O, et al: Hypoxia triggers the
intravasation of clustered circulating tumor cells. Cell Rep.
32(108105)2020.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Huang L, Ji H, Yin L, Niu X, Wang Y, Liu
Y, Xuan Q, Li L, Zhang H, Zhou X, et al: High expression of
plakoglobin promotes metastasis in invasive micropapillary
carcinoma of the breast via tumor cluster formation. J Cancer.
10:2800–2810. 2019.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Yin L, Li Q, Mrdenovic S, Chu GC, Wu BJ,
Bu H, Duan P, Kim J, You S, Lewis MS, et al: KRT13 promotes
stemness and drives metastasis in breast cancer through a
plakoglobin/c-Myc signaling pathway. Breast Cancer Res.
24(7)2022.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Xie N, Hu Z, Tian C, Xiao H, Liu L, Yang
X, Li J, Wu H, Lu J, Gao J, et al: In vivo detection of CTC and CTC
plakoglobin status helps predict prognosis in patients with
metastatic breast cancer. Pathol Oncol Res. 26:2435–2442.
2020.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Hassn Mesrati M, Syafruddin SE, Mohtar MA
and Syahir A: CD44: A multifunctional mediator of cancer
progression. Biomolecules. 11(1850)2021.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Hiraga T and Nakamura H: Comparable roles
of CD44v8-10 and CD44s in the development of bone metastases in a
mouse model. Oncol Lett. 12:2962–2969. 2016.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Kolev VN, Tam WF, Wright QG, McDermott SP,
Vidal CM, Shapiro IM, Xu Q, Wicha MS, Pachter JA and Weaver DT:
Inhibition of FAK kinase activity preferentially targets cancer
stem cells. Oncotarget. 8:51733–51747. 2017.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Lev S: Targeted therapy and drug
resistance in triple-negative breast cancer: The EGFR axis. Biochem
Soc Trans. 48:657–665. 2020.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Liu X, Adorno-Cruz V, Chang YF, Jia Y,
Kawaguchi M, Dashzeveg NK, Taftaf R, Ramos EK, Schuster EJ,
El-Shennawy L, et al: EGFR inhibition blocks cancer stem cell
clustering and lung metastasis of triple negative breast cancer.
Theranostics. 11:6632–6643. 2021.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Bockhorn J, Dalton R, Nwachukwu C, Huang
S, Prat A, Yee K, Chang YF, Huo D, Wen Y, Swanson KE, et al:
MicroRNA-30c inhibits human breast tumour chemotherapy resistance
by regulating TWF1 and IL-11. Nat Commun. 4(1393)2013.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Taftaf R, Liu X, Singh S, Jia Y, Dashzeveg
NK, Hoffmann AD, El-Shennawy L, Ramos EK, Adorno-Cruz V, Schuster
EJ, et al: ICAM1 initiates CTC cluster formation and
trans-endothelial migration in lung metastasis of breast cancer.
Nat Commun. 12(4867)2021.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Bui TM, Wiesolek HL and Sumagin R: ICAM-1:
A master regulator of cellular responses in inflammation, injury
resolution, and tumorigenesis. J Leukoc Biol. 108:787–799.
2020.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Wei RR, Sun DN, Yang H, Yan J, Zhang X,
Zheng XL, Fu XH, Geng MY, Huang X and Ding J: CTC clusters induced
by heparanase enhance breast cancer metastasis. Acta Pharmacol Sin.
39:1326–1337. 2018.PubMed/NCBI View Article : Google Scholar
|
|
44
|
Niu Y, Bao L, Chen Y, Wang C, Luo M, Zhang
B, Zhou M, Wang JE, Fang YV, Kumar A, et al: HIF2-Induced Long
Noncoding RNA RAB11B-AS1 Promotes Hypoxia-Mediated angiogenesis and
breast cancer metastasis. Cancer Res. 80:964–975. 2020.PubMed/NCBI View Article : Google Scholar
|
|
45
|
Chang PH, Chen MC, Tsai YP, Tan GYT, Hsu
PH, Jeng YM, Tsai YF, Yang MH and Hwang-Verslues WW: Interplay
between desmoglein2 and hypoxia controls metastasis in breast
cancer. Proc Natl Acad Sci USA. 118(e2014408118)2021.PubMed/NCBI View Article : Google Scholar
|
|
46
|
Tashireva LA, Savelieva OE, Grigoryeva ES,
Nikitin YV, Denisov EV, Vtorushin SV, Zavyalova MV, Cherdyntseva NV
and Perelmuter VM: Heterogeneous manifestations of
epithelial-mesenchymal plasticity of circulating tumor cells in
breast cancer patients. Int J Mol Sci. 22(2504)2021.PubMed/NCBI View Article : Google Scholar
|
|
47
|
Fabisiewicz A and Grzybowska E: CTC
clusters in cancer progression and metastasis. Med Oncol.
34(12)2017.PubMed/NCBI View Article : Google Scholar
|
|
48
|
Gkountela S, Castro-Giner F, Szczerba BM,
Vetter M, Landin J, Scherrer R, Krol I, Scheidmann MC, Beisel C,
Stirnimann CU, et al: Circulating tumor cell clustering shapes DNA
methylation to enable metastasis seeding. Cell. 176:98–112.e14.
2019.PubMed/NCBI View Article : Google Scholar
|
|
49
|
Sheaffer KL, Elliott EN and Kaestner KH:
DNA hypomethylation contributes to genomic instability and
intestinal cancer initiation. Cancer Prev Res (Phila). 9:534–546.
2016.PubMed/NCBI View Article : Google Scholar
|
|
50
|
Zmetakova I, Kalinkova L, Smolkova B,
Horvathova Kajabova V, Cierna Z, Danihel L, Bohac M, Sedlackova T,
Minarik G, Karaba M, et al: A disintegrin and metalloprotease 23
hypermethylation predicts decreased disease-free survival in
low-risk breast cancer patients. Cancer Sci. 110:1695–1704.
2019.PubMed/NCBI View Article : Google Scholar
|
|
51
|
Hapach LA, Carey SP, Schwager SC,
Taufalele PV, Wang W, Mosier JA, Ortiz-Otero N, McArdle TJ,
Goldblatt ZE, Lampi MC, et al: Phenotypic heterogeneity and
metastasis of breast cancer cells. Cancer Res. 81:3649–3663.
2021.PubMed/NCBI View Article : Google Scholar
|
|
52
|
Han HJ, Sung JY, Kim SH, Yun UJ, Kim H,
Jang EJ, Yoo HE, Hong EK, Goh SH, Moon A, et al: Fibronectin
regulates anoikis resistance via cell aggregate formation. Cancer
Lett. 508:59–72. 2021.PubMed/NCBI View Article : Google Scholar
|
|
53
|
Mutlu BR, Dubash T, Dietsche C, Mishra A,
Ozbey A, Keim K, Edd JF, Haber DA, Maheswaran S and Toner M:
In-flow measurement of cell-cell adhesion using oscillatory
inertial microfluidics. Lab Chip. 20:1612–1620. 2020.PubMed/NCBI View Article : Google Scholar
|
|
54
|
Neophytou CM, Trougakos IP, Erin N and
Papageorgis P: Apoptosis deregulation and the development of cancer
multi-drug resistance. Cancers (Basel). 13(4363)2021.PubMed/NCBI View Article : Google Scholar
|
|
55
|
Kim H, Sung JY, Park EK, Kho S, Koo KH,
Park SY, Goh SH, Jeon YK, Oh S, Park BK, et al: Regulation of
anoikis resistance by NADPH oxidase 4 and epidermal growth factor
receptor. Br J Cancer. 116:370–381. 2017.PubMed/NCBI View Article : Google Scholar
|
|
56
|
Thangavel H, De Angelis C, Vasaikar S,
Bhat R, Jolly MK, Nagi C, Creighton CJ, Chen F, Dobrolecki LE,
George JT, et al: A CTC-cluster-specific signature derived from
OMICS analysis of patient-derived xenograft tumors predicts
outcomes in basal-like breast cancer. J Clin Med.
8(1772)2019.PubMed/NCBI View Article : Google Scholar
|
|
57
|
Yu M: Metastasis stemming from circulating
tumor cell clusters. Trends Cell Biol. 29:275–276. 2019.PubMed/NCBI View Article : Google Scholar
|
|
58
|
Babaei G, Aziz SG and Jaghi NZZ: EMT,
cancer stem cells and autophagy; The three main axes of metastasis.
Biomed Pharmacother. 133(110909)2021.PubMed/NCBI View Article : Google Scholar
|
|
59
|
Kapeleris J, Zou H, Qi Y, Gu Y, Li J,
Schoning J, Monteiro MJ and Gu W: Cancer stemness contributes to
cluster formation of colon cancer cells and high metastatic
potentials. Clin Exp Pharmacol Physiol. 47:838–847. 2020.PubMed/NCBI View Article : Google Scholar
|
|
60
|
Martinez-Pena I, Hurtado P, Carmona-Ule N,
Abuin C, Davila-Ibanez AB, Sanchez L, Abal M, Chaachou A,
Hernández-Losa J, Cajal SRY, et al: Dissecting breast cancer
circulating tumor cells competence via modelling metastasis in
zebrafish. Int J Mol Sci. 22(9279)2022.PubMed/NCBI View Article : Google Scholar
|
|
61
|
Kawaguchi M, Dashzeveg N, Cao Y, Jia Y,
Liu X, Shen Y and Liu H: Extracellular Domains I and II of
cell-surface glycoprotein CD44 mediate its trans-homophilic
dimerization and tumor cluster aggregation. J Biol Chem.
295:2640–2649. 2020.PubMed/NCBI View Article : Google Scholar
|
|
62
|
Manupati K, Yeeravalli R, Kaushik K, Singh
D, Mehra B, Gangane N, Gupta A, Goswami K and Das A: Activation of
CD44-Lipoprotein lipase axis in breast cancer stem cells promotes
tumorigenesis. Biochim Biophys Acta Mol Basis Dis.
1867(166228)2021.PubMed/NCBI View Article : Google Scholar
|
|
63
|
Wang X, Sun Q, Liu Q, Wang C, Yao R and
Wang Y: CTC immune escape mediated by PD-L1. Med Hypotheses.
93:138–139. 2016.PubMed/NCBI View Article : Google Scholar
|
|
64
|
Liu Q, Liao Q and Zhao Y: Myeloid-derived
suppressor cells (MDSC) facilitate distant metastasis of
malignancies by shielding circulating tumor cells (CTC) from immune
surveillance. Med Hypotheses. 87:34–39. 2016.PubMed/NCBI View Article : Google Scholar
|
|
65
|
Lo HC, Xu Z, Kim IS, Pingel B, Aguirre S,
Kodali S, Liu J, Zhang W, Muscarella AM, Hein SM, et al: Resistance
to natural killer cell immunosurveillance confers a selective
advantage to polyclonal metastasis. Nat Cancer. 1:709–722.
2020.PubMed/NCBI View Article : Google Scholar
|
|
66
|
Szczerba BM, Castro-Giner F, Vetter M,
Krol I, Gkountela S, Landin J, Scheidmann MC, Donato C, Scherrer R,
Singer J, et al: Neutrophils escort circulating tumour cells to
enable cell cycle progression. Nature. 566:553–557. 2019.PubMed/NCBI View Article : Google Scholar
|
|
67
|
Luo L and He Y: Magnetically driven
microfluidics for isolation of circulating tumor cells. Cancer Med.
9:4207–4231. 2020.PubMed/NCBI View Article : Google Scholar
|
|
68
|
Sierra-Agudelo J, Rodriguez-Trujillo R and
Samitier J: Microfluidics for the isolation and detection of
circulating tumor cells. Adv Exp Med Biol. 1379:389–412.
2022.PubMed/NCBI View Article : Google Scholar
|
|
69
|
Khetani S, Mohammadi M and Nezhad AS:
Filter-based isolation, enrichment, and characterization of
circulating tumor cells. Biotechnol Bioeng. 115:2504–2529.
2018.PubMed/NCBI View Article : Google Scholar
|
|
70
|
Riethdorf S, O'Flaherty L, Hille C and
Pantel K: Clinical applications of the CellSearch platform in
cancer patients. Adv Drug Deliv Rev. 125:102–121. 2018.PubMed/NCBI View Article : Google Scholar
|
|
71
|
Ramos-Medina R, Lopez-Tarruella S, Del
Monte-Millan M, Massarrah T and Martin M: Technical challenges for
CTC implementation in breast cancer. Cancers (Basel).
13(4619)2021.PubMed/NCBI View Article : Google Scholar
|
|
72
|
Deng Z, Wu S, Wang Y and Shi D:
Circulating tumor cell isolation for cancer diagnosis and
prognosis. EBioMedicine. 83(104237)2022.PubMed/NCBI View Article : Google Scholar
|
|
73
|
Menyailo ME, Bokova UA, Ivanyuk EE,
Khozyainova AA and Denisov EV: Metastasis prevention: Focus on
metastatic circulating tumor cells. Mol Diagn Ther. 25:549–562.
2021.PubMed/NCBI View Article : Google Scholar
|
|
74
|
Krol I, Schwab FD, Carbone R, Ritter M,
Picocci S, De Marni ML, Stepien G, Franchi GM, Zanardi A, Rissoglio
MD, et al: Detection of clustered circulating tumour cells in early
breast cancer. Br J Cancer. 125:23–27. 2021.PubMed/NCBI View Article : Google Scholar
|
|
75
|
Deutsch TM, Riethdorf S, Fremd C, Feisst
M, Nees J, Fischer C, Hartkopf AD, Pantel K, Trumpp A, Schütz F, et
al: HER2-targeted therapy influences CTC status in metastatic
breast cancer. Breast Cancer Res Treat. 182:127–136.
2020.PubMed/NCBI View Article : Google Scholar
|
|
76
|
Goodman CR, Seagle BL, Friedl TWP, Rack B,
Lato K, Fink V, Cristofanilli M, Donnelly ED, Janni W, Shahabi S
and Strauss JB: Association of circulating tumor cell status with
benefit of radiotherapy and survival in early-stage breast cancer.
JAMA Oncol. 4(e180163)2018.PubMed/NCBI View Article : Google Scholar
|
|
77
|
Mostert B, Sieuwerts AM, Kraan J, Bolt-de
Vries J, van der Spoel P, van Galen A, Peeters DJ, Dirix LY,
Seynaeve CM, Jager A, et al: Gene expression profiles in
circulating tumor cells to predict prognosis in metastatic breast
cancer patients. Ann Oncol. 26:510–516. 2015.PubMed/NCBI View Article : Google Scholar
|
|
78
|
Bidard FC, Jacot W, Kiavue N, Dureau S,
Kadi A, Brain E, Bachelot T, Bourgeois H, Gonçalves A, Ladoire S,
et al: Efficacy of circulating tumor cell count-driven vs
clinician-driven first-line therapy choice in hormone
receptor-positive, ERBB2-Negative metastatic breast cancer: The
STIC CTC randomized clinical trial. JAMA Oncol. 7:34–41.
2021.PubMed/NCBI View Article : Google Scholar
|
|
79
|
Radovich M, Jiang G, Hancock BA, Chitambar
C, Nanda R, Falkson C, Lynce FC, Gallagher C, Isaacs C, Blaya M, et
al: Association of circulating tumor DNA and circulating tumor
cells after neoadjuvant chemotherapy with disease recurrence in
patients with triple-negative breast cancer: Preplanned secondary
analysis of the BRE12-158 randomized clinical trial. JAMA Oncol.
6:1410–1415. 2020.PubMed/NCBI View Article : Google Scholar
|
|
80
|
Zhang Y, Lv Y, Niu Y, Su H and Feng A:
Role of circulating tumor cell (CTC) monitoring in evaluating
prognosis of triple-negative breast cancer patients in China. Med
Sci Monit. 23:3071–3079. 2017.PubMed/NCBI View Article : Google Scholar
|
|
81
|
Ramirez JM, Fehm T, Orsini M, Cayrefourcq
L, Maudelonde T, Pantel K and Alix-Panabières C: Prognostic
relevance of viable circulating tumor cells detected by EPISPOT in
metastatic breast cancer patients. Clin Chem. 60:214–221.
2014.PubMed/NCBI View Article : Google Scholar
|
|
82
|
Bidard FC, Peeters DJ, Fehm T, Nole F,
Gisbert-Criado R, Mavroudis D, Grisanti S, Generali D, Garcia-Saenz
JA, Stebbing J, et al: Clinical validity of circulating tumour
cells in patients with metastatic breast cancer: A pooled analysis
of individual patient data. Lancet Oncol. 15:406–414.
2014.PubMed/NCBI View Article : Google Scholar
|
|
83
|
Guan X, Ma F, Li C, Wu S, Hu S, Huang J,
Sun X, Wang J, Luo Y, Cai R, et al: The prognostic and therapeutic
implications of circulating tumor cell phenotype detection based on
epithelial-mesenchymal transition markers in the first-line
chemotherapy of HER2-negative metastatic breast cancer. Cancer
Commun (Lond). 39(1)2019.PubMed/NCBI View Article : Google Scholar
|
|
84
|
Larsson AM, Jansson S, Bendahl PO, Levin
Tykjaer Jorgensen C, Loman N, Graffman C, Lundgren L, Aaltonen K
and Rydén L: Longitudinal enumeration and cluster evaluation of
circulating tumor cells improve prognostication for patients with
newly diagnosed metastatic breast cancer in a prospective
observational trial. Breast Cancer Res. 20(48)2018.PubMed/NCBI View Article : Google Scholar
|
|
85
|
Pang S, Li H, Xu S, Feng L, Ma X, Chu Y,
Zou B, Wang S and Zhou G: Circulating tumour cells at baseline and
late phase of treatment provide prognostic value in breast cancer.
Sci Rep. 11(13441)2021.PubMed/NCBI View Article : Google Scholar
|
|
86
|
Pierga JY, Bidard FC, Autret A, Petit T,
Andre F, Dalenc F, Levy C, Ferrero JM, Romieu G, Bonneterre J, et
al: Circulating tumour cells and pathological complete response:
independent prognostic factors in inflammatory breast cancer in a
pooled analysis of two multicentre phase II trials (BEVERLY-1 and
-2) of neoadjuvant chemotherapy combined with bevacizumab. Ann
Oncol. 28:103–109. 2017.PubMed/NCBI View Article : Google Scholar
|