|
1
|
Bray F, Ferlay J, Soerjomataram I, Siegel
RL, Torre LA and Jemal A: Global cancer statistics 2018: GLOBOCAN
estimates of incidence and mortality worldwide for 36 cancers in
185 countries. CA Cancer J Clin. 68:394–424. 2018.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Verhelst P-J, Dons F, Van Bever PJ,
Schoenaers J, Nanhekhan L and Politis C: Fibula free flap in head
and neck reconstruction: Identifying risk factors for flap failure
and analysis of postoperative complications in a low volume
setting. Craniomaxillofac Trauma Reconstr. 12:183–192.
2019.PubMed/NCBI View Article : Google Scholar
|
|
3
|
van Beek FE, Jansen F, Mak L,
Lissenberg-Witte BI, Buter J, Vergeer MR, Voortman J, Cuijpers P,
Leemans CR and Verdonck-de Leeuw IM: The course of symptoms of
anxiety and depression from time of diagnosis up to 2 years
follow-up in head and neck cancer patients treated with primary
(chemo)radiation. Oral Oncol. 102(104576)2020.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Hidalgo DA: Fibula free flap: A new method
of mandible reconstruction. Plast Reconstr Surg. 84:71–79.
1989.PubMed/NCBI
|
|
5
|
Swartz WM, Banis JC, Newton ED, Ramasastry
SS, Jones NF and Acland R: The osteocutaneous scapular flap for
mandibular and maxillary reconstruction. Plast Reconstr Surg.
77:530–545. 1986.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Petrovic I, Panchal H, Franca PDDS,
Hernandez M, McCarthy CC and Shah J: A Systematic review of
validated tools assessing functional and aesthetic outcomes
following fibula free flap reconstruction of the mandible. Head
Neck. 41(248)2019.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Ghai S, Sharma Y, Jain N, Satpathy M and
Pillai AK: Use of 3-D printing technologies in craniomaxillofacial
surgery: A review. Oral Maxillofac Surg. 22:249–259.
2018.PubMed/NCBI View Article : Google Scholar
|
|
8
|
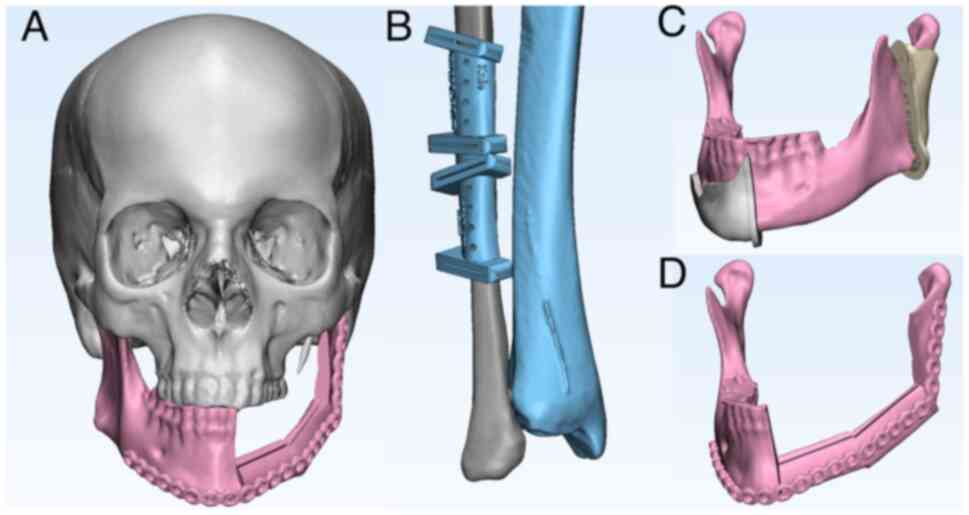
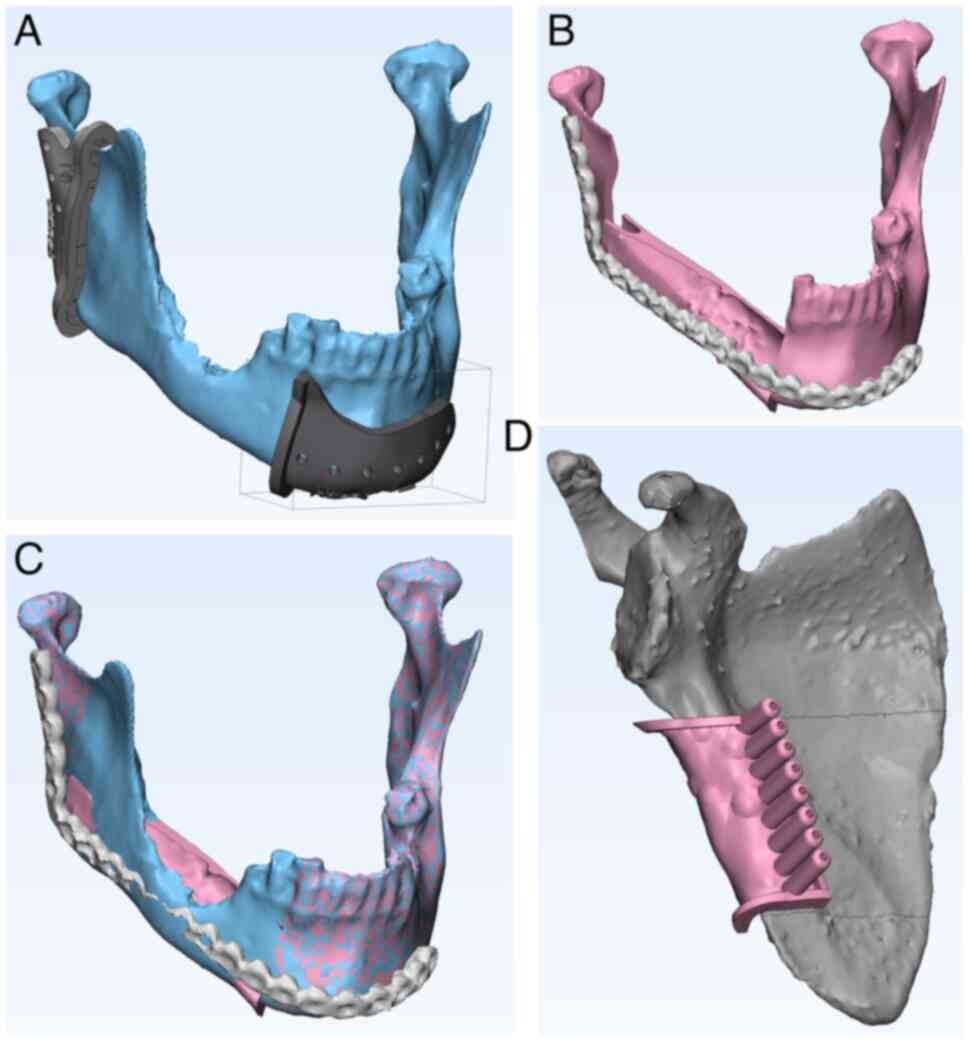
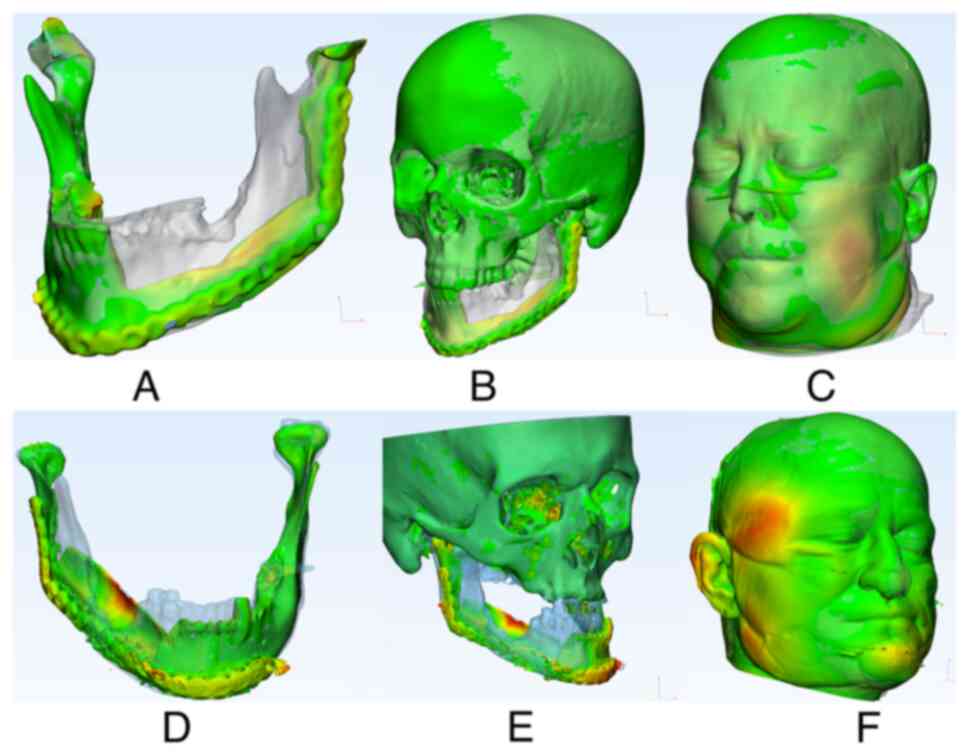
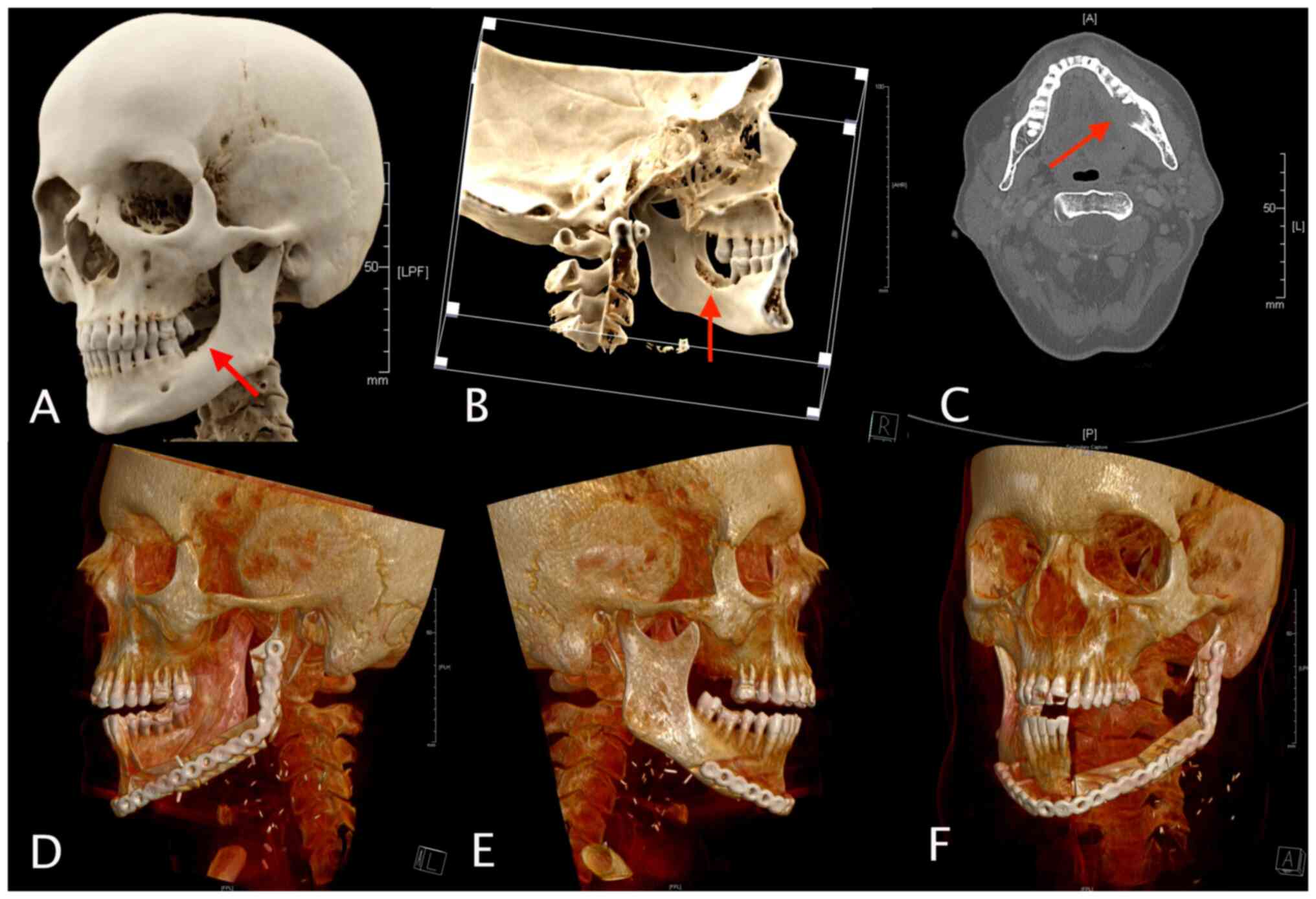
Ritschl LM, Kilbertus P, Grill FD, Schwarz
M, Weitz J, Nieberler M, Wolff KD and Fichter AM: In-house,
open-source 3D-software-based, CAD/CAM-planned mandibular
reconstructions in 20 consecutive free fibula flap cases: An
explorative cross-sectional study with three-dimensional
performance analysis. Front Oncol. 11(731336)2021.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Serrano C, van den Brink H, Pineau J,
Prognon P and Martelli N: Benefits of 3D printing applications in
jaw reconstruction: A systematic review and meta-analysis. J
Craniomaxillofac Surg. 47:1387–1397. 2019.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Nyirjesy SC, Heller M, von Windheim N,
Gingras A, Kang SY, Ozer E, Agrawal A, Old MO, Seim NB, Carrau RL,
et al: The role of computer aided design/computer assisted
manufacturing (CAD/CAM) and 3-dimensional printing in head and neck
oncologic surgery: A review and future directions. Oral Oncol.
132(105976)2022.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Berrone M, Crosetti E, Tos PL, Pentenero M
and Succo G: Fibular osteofasciocutaneous flap in computer-assisted
mandibular reconstruction: Technical aspects in oral malignancies.
Acta Otorhinolaryngol Ital. 36:469–478. 2016.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Sharma N, Aghlmandi S, Cao S, Kunz C,
Honigmann P and Thieringer FM: Quality characteristics and clinical
relevance of in-house 3D-printed customized polyetheretherketone
(PEEK) implants for craniofacial reconstruction. J Clin Med.
9(2818)2020.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Christensen R: ‘Ordinal-regression models
for ordinal data.’. R Package Version. 12–10. 2019.
|
|
14
|
Heinze G and Schemper M: A solution to the
problem of separation in logistic regression. Stat Med.
21:2409–2419. 2002.PubMed/NCBI View
Article : Google Scholar
|
|
15
|
Hoene G, Gruber RM, Leonhard JJ, Wiechens
B, Schminke B, Kauffmann P, Schliephake H and Brockmeyer P:
Combined quality of life and posttraumatic growth evaluation during
follow-up care of patients suffering from oral squamous cell
carcinoma. Mol Clin Oncol. 15(189)2021.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Iglesias-Martín F, Oliveros-López LG,
Fernández-Olavarría A, Serrera-Figallo MA, Gutiérrez-Corrales A,
Torres-Lagares D and Gutiérrez-Pérez JL: Advantages of surgical
simulation in the surgical reconstruction of oncological patients.
Med Oral Patol Oral Cir Bucal. 23:e596–e601. 2018.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Brown JS, Lowe D, Kanatas A and Schache A:
Mandibular reconstruction with vascularised bone flaps: A
systematic review over 25 years. Br J Oral Maxillofac Surg.
55:113–126. 2017.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Hollows P, McAndrew PG and Perini MG:
Delays in the referral and treatment of oral squamous cell
carcinoma. Br Dent J. 188:262–265. 2000.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Huang SH, Hahn E, Chiosea SI, Xu ZY, Li
JS, Shen L and O'Sullivan B: The role of adjuvant
(chemo-)radiotherapy in oral cancers in the contemporary era. Oral
Oncol. 102(104563)2020.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Lee H, Roh JL, Cho KJ, Choi SH, Nam SY and
Kim SY: Number of positive lymph nodes better predicts survival for
oral cavity cancer. J Surg Oncol. 119:675–682. 2019.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Kim J, Shin ES, Kim JE, Yoon SP and Kim
YS: Neck muscle atrophy and soft-tissue fibrosis after neck
dissection and postoperative radiotherapy for oral cancer. Radiat
Oncol J. 33:344–349. 2015.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Dean A, Alamillos F, Heredero S,
Redondo-Camacho A, Guler I and Sanjuan A: Fibula free flap in
maxillomandibular reconstruction. Factors related to osteosynthesis
plates' complications. J Craniomaxillofac Surg. 48:994–1003.
2020.PubMed/NCBI View Article : Google Scholar
|
|
23
|
López-Arcas JM, Arias J, Del Castillo JL,
Burgueño M, Navarro I, Morán MJ, Chamorro M and Martorell V: The
fibula osteomyocutaneous flap for mandible reconstruction: A
15-year experience. J Craniomaxillofac Surg. 68:2377–2384.
2010.PubMed/NCBI View Article : Google Scholar
|
|
24
|
van Gemert JTM, Abbink JH, van Es RJJ,
Rosenberg AJWP, Koole R and Van Cann EM: Early and late
complications in the reconstructed mandible with free fibula flaps.
J Surg Oncol. 117:773–780. 2018.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Al-Bustani S, Austin GK, Ambrose EC,
Miller J, Hackman TG and Halvorson EG: Miniplates versus
reconstruction bars for oncologic free fibula flap mandible
reconstruction. Ann Plast Surg. 77:314–317. 2016.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Wurm MC, Hagen J, Nkenke E, Neukam FW and
Schlittenbauer T: The fitting accuracy of pre-bend reconstruction
plates and their impact on the temporomandibular joint. J
Craniomaxillofac Surg. 47:53–59. 2019.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Rommel N, Kesting MR, Rohleder NH, Bauer
FMJ, Wolff KD and Weitz J: Mandible reconstruction with free fibula
flaps: Outcome of a cost-effective individual planning concept
compared with virtual surgical planning. J Craniomaxillofac Surg.
45:1246–1250. 2017.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Tarsitano A, Battaglia S, Crimi S, Ciocca
L, Scotti R and Marchetti C: Is a computer-assisted design and
computer-assisted manufacturing method for mandibular
reconstruction economically viable? J Craniomaxillofac Surg.
44:795–799. 2016.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Barr ML, Haveles CS, Rezzadeh KS, Nolan
IT, Castro R, Lee JC, Steinbacher D and Pfaff MJ: Virtual surgical
planning for mandibular reconstruction with the fibula free flap: A
systematic review and meta-analysis. Ann Plast Surg. 84:117–122.
2020.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Geusens J, Sun Y, Luebbers HT, Bila M,
Darche V and Politis C: Accuracy of Computer-aided
design/computer-aided manufacturing-assisted mandibular
reconstruction with a fibula free flap. J Craniofac Surg.
30:2319–2323. 2019.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Schepers RH, Raghoebar GM, Vissink A,
Stenekes MW, Kraeima J, Roodenburg JL, Reintsema H and Witjes MJ:
Accuracy of fibula reconstruction using patient-specific CAD/CAM
reconstruction plates and dental implants: A new modality for
functional reconstruction of mandibular defects. J Craniomaxillofac
Surg. 43:649–657. 2015.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Moe J, Foss J, Herster R, Powell C, Helman
J, Ward BB and VanKoevering K: An in-house computer-aided design
and computer-aided manufacturing workflow for maxillofacial free
flap reconstruction is associated with a low cost and high
accuracy. J Craniomaxillofac Surg. 79:227–236. 2021.PubMed/NCBI View Article : Google Scholar
|