Introduction
Conjunctival melanoma is a relatively rare ocular
surface malignancy leading to recurrence and subsequent
melanoma-related death; however, vascular configurations in tumor
tissues have not been fully analyzed. In head and neck melanoma,
not only tumor morphology but also rich vascularization and
lymphatic vessels may promote hematogeneous and lymph node
metastasis, and subsequent mortality (1). In conjunctival melanoma,
tumor-associated lymphangiogenesis has an important role in tumor
growth, lymph node metastasis and mortality (2). However, the role of intratumoral
microvessels in conjunctival melanoma remains largely unknown. It
is indisputable that high intratumoral microvessel density could
correlate with less tumor cell apoptosis and a subsequently more
aggressive nature, such as local recurrence or metastasis of
malignancies (3,4). We previously demonstrated that
conjunctival melanoma could show hypo-vascularity compared with
adjacent non-cancerous conjunctiva (5). Conjunctival melanoma is likely to
involve vascular abnormalities such as intralesional hemorrhage and
visible intrinsic tumor vessels with increased dye leakage compared
with benign tumors, which could reflect a defective endothelial
barrier function (6). Here, we
report a rare case of persistent bleeding caused by conjunctival
melanoma containing abundant vascular channels and propose a novel
variant of conjunctival melanoma. The study adheres to the tenets
of the Declaration of Helsinki.
Case report
Case description
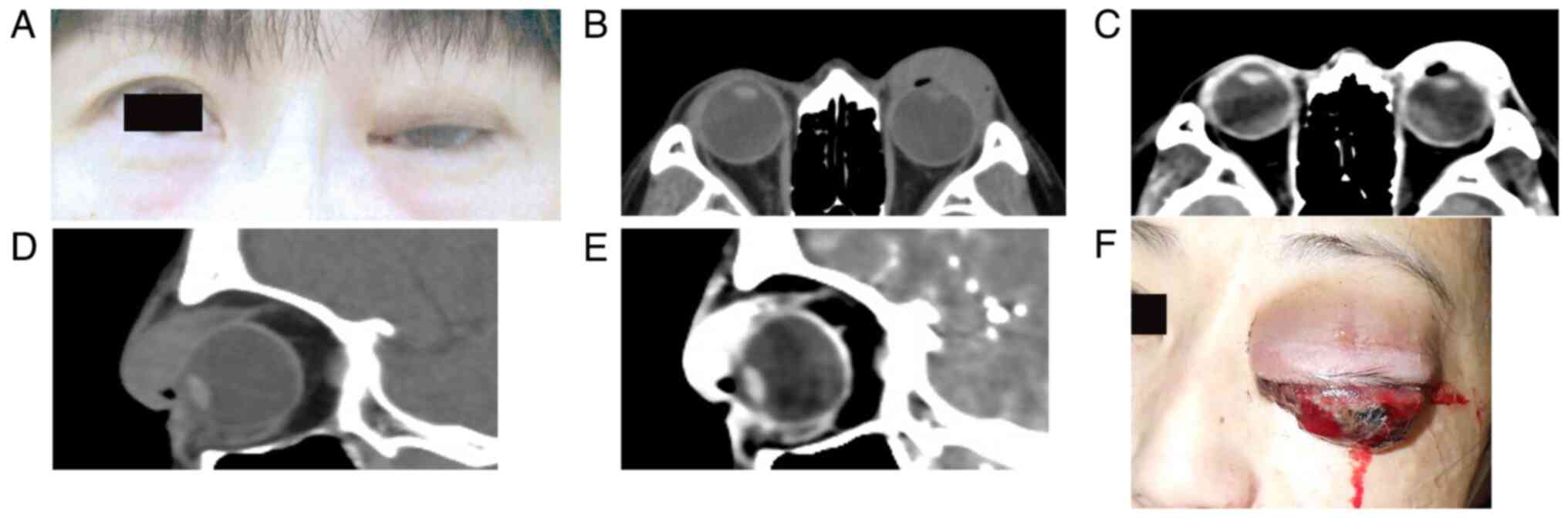
A 44-year-old Japanese woman presented at her local
clinic with a left upper eyelid nodule measuring about 2 fingers
broad in February 2023. The patient was healthy without any
remarkable medical history. The ophthalmologist at a nearby clinic
attempted to aspirate the tumor, but only some blood was collected,
and thus, the patient was observed without any biopsy of the
lesion. The nodule gradually enlarged and grew away from the eyelid
conjunctiva over 2 months, so the patient was referred for plastic
surgery at a nearby hospital in April 2023. There was a pigmented
conjunctival mass in the upper palpebral conjunctiva (Fig. 1A). Computed tomography (CT) showed
a large eyelid tumor invading the anterior orbit (Fig. 1B and D). Enhanced CT demonstrated marked
enhancement in the left eyelid in the artery phase, indicating
hemangioma (Fig. 1C and E), while there were no lesions in the
deep orbit. Therefore, the plastic surgeon followed up the patient
based on the radiological report. Whole-body CT with enhancements
(data not shown) revealed no enhancement in the body except for the
left periocular region. The conjunctival mass further enlarged,
where bleeding was noted in May 2023. The surgeon conducted a
transcutaneous biopsy of the eyelid mass. In the following week,
the patient accidentally suffered blunt trauma to her face and
continuous bleeding from the tumor occurred. Doctors in the
emergency room attempted hemostasis by diathermy and suture, but
the bleeding could not be stopped. Although no pathological
diagnosis had been made, the patient was referred to Hokkaido
University Hospital (Sapporo, Japan) in June 2023. At this initial
presentation, the left eyelid showed marked swelling with
persistent bleeding (Fig. 1F). The
eyelid had acquired a reddish coloration without any pain or
tenderness. A large elastic, hard mass was palpable beneath the
entire eyelid skin. The surface of the tumor was admixed with
pigmentation and fresh bleeding, with reddish elevation. The visual
acuity, intraocular pressure and fundus could not be fully examined
because the mass lesion blocked the ocular tissues. The
conjunctival mass was clinically diagnosed as giant conjunctival
melanoma exclusively based on clinical findings of an elastic hard
mass with pigmentation. The patient was taken to the operating room
and emergent orbital exenteration was conducted about 2 h after
arrival at our out-patient ward following the obtainment of
informed consent. Just before the orbital exenteration, the
patient's consciousness was clear, the heart rate was normal at
69/min, the body temperature was normal at 36.7˚C, blood pressure
was normal (117/80 mmHg) and oxygen saturation was 98%, whereas a
blood test revealed anemia, showing a low number of red blood cells
(3.68x1012/l; reference value,
4.35-5.55x1012/l), hemoglobin (9.9 g/dl; reference
value, 13.7-16.8 g/dl) and hematocrit (31.6%; reference value,
40.7-50.1%). After removal, the persistent bleeding resolved. The
pathology report of biopsy tissue taken by the plastic surgeon
indicated the presence of numerous atypical epithelioid cells with
high cellularity. The nuclei were round with clear nucleoli. There
were necrotic foci and pigmentation within the tumor tissues. The
atypical cells were positive for melanocytic markers, human
melanoma antigen (HMB45) (monoclonal; pre-diluted; cat. no. 413851;
Nichirei Corp.) and Melan A (monoclonal; pre-diluted; cat. no.
413381; Nichirei Corp.), but negative for epithelial markers,
AE1/AE3 (monoclonal; pre-diluted; cat. no. 760-2135; Roche
Diagnostics) and cytokeratin (CAM5.2; monoclonal; pre-diluted; cat.
no. 349205; BD Bioscience) and stromal and endothelial cell marker
CD34 (monoclonal; pre-diluted; cat. no. 413111; Nichirei Corp.).
Those findings allowed for a pathological diagnosis of malignant
melanoma, which was conveyed to our hospital from the initial
external hospital after the exenteration. H&E staining and
immunohistochemistry was performed according to standard
procedures.
In June 2023, positron emission tomography-CT (data
now shown) revealed no whole-body enhancement, including ocular
regions. In July 2023, a subcutaneous mass lesion was found in the
posterior head (data not shown). In August 2023, the left
preauricular lymph nodes were enlarged and a biopsy was conducted.
The pathological report was consistent with metastatic malignant
melanoma. A subsequent whole-body CT depicted metastatic lesions in
the left orbit, lung and liver, as well as systemic bone metastases
(data not shown). Nivolumab and ipilimumab were initiated 3 months
after the exenteration. In October 2023, brain metastasis were
noted on CT (data not shown). Sadly, the patient died in March of
the following year.
Pathological findings of total excised
tumor
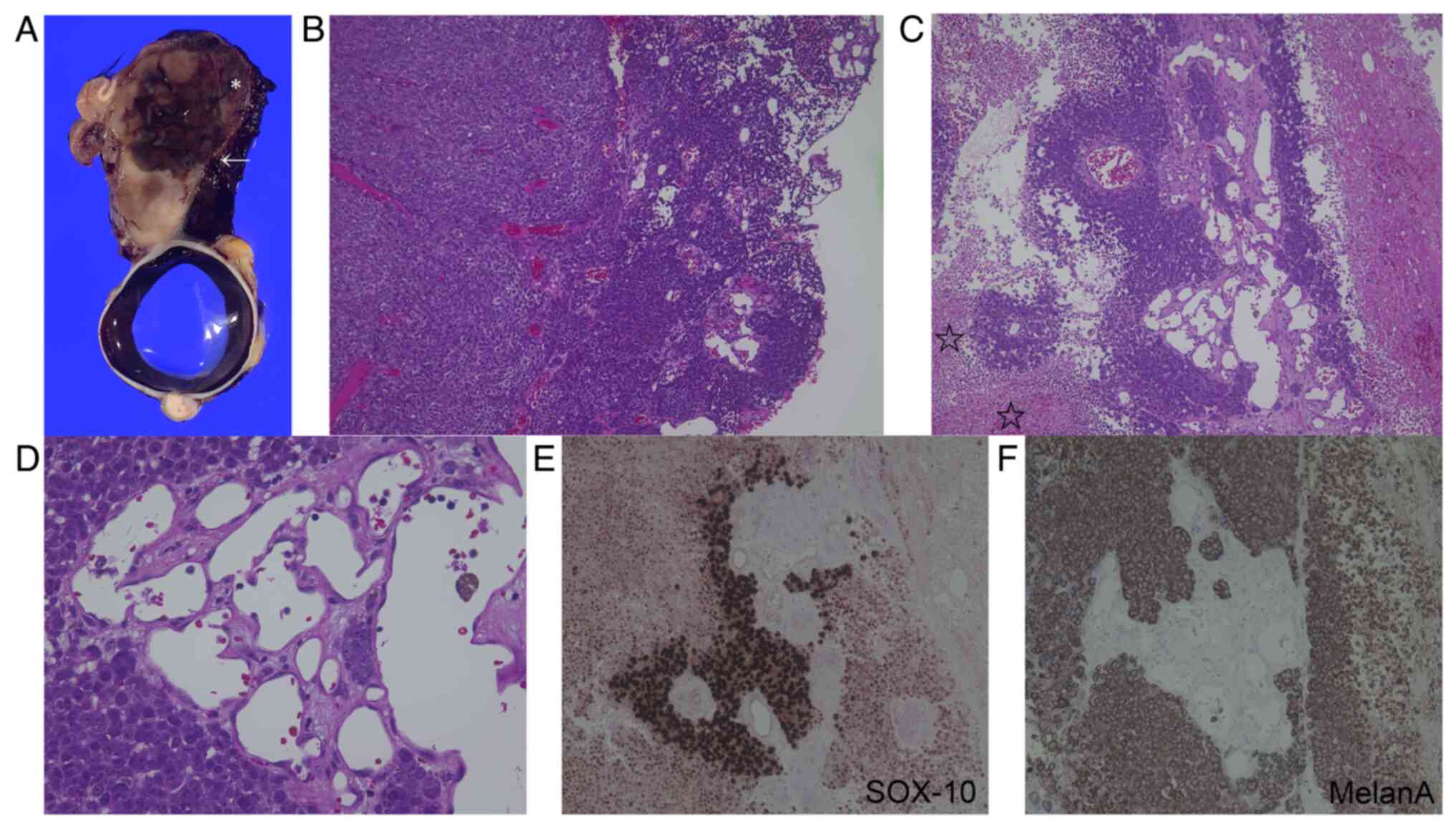
The excised tumor, measuring 30x35x45 mm, originated
from the palpebral conjunctiva with protrusion of the eyelid skin
(Fig. 2A). Regarding the
histological findings of the tumor region indicated by an asterisk
in Fig. 2A, the tumor cells
diffusely proliferated in the upper eyelid with less necrosis
(Fig. 2B). There was abundant
microvascular formation on the conjunctival side. Regarding the
histological findings of the tumor region shown by an asterisk in
Fig. 2A consistent with bleeding
sites and by an arrow close to the bleeding site, not only viable
tumor-cell proliferation (Fig.
2B), but also necrosis (Fig.
2C, stars) with hematoma were noted (Fig. 2C). The tumor was made up of
polygonal, atypical, large cells with marked nuclear atypia. A
variety of atypical epithelioid tumor cells with prominent nucleoli
were intermingled. At a high magnification closed to the bleeding
site (Fig. 2A, arrow), there were
small-to-large vascular channels made up of endothelial cells
forming various vascular lumens (Fig.
2D). Immunohistochemical analysis revealed that the tumor cells
were positive for SOX10 (Fig. 2E),
Melan A (Fig. 2F), S100 and HMB45,
leading to the diagnosis of malignant melanoma. Based on the 8th
American Joint Committee on Cancer classification (7), the melanoma was pathologically
classified as pT2b.
Discussion
The current study presented 2 novel
clinicopathological findings in giant conjunctival melanoma. The
first was persistent bleeding from the tumor as a clinical finding.
Although there was no clear definition of ‘giant’ regarding the
size of conjunctival melanoma, several case reports in the
literature have described giant conjunctival melanomas (8-11).
Most patients previously diagnosed with a giant conjunctival
melanoma, as in a case report of a patient presenting with an
enlarged conjunctival pigmented mass (8), and rarely with hemorrhage, which
could be removed by extensive surgical resection, together with
cryopexy or radiotherapy (8-11).
In addition, if tumor tissues are totally removed by local
resection with extensive eyelid/conjunctival reconstruction,
adjuvant local chemotherapy with mitomycin C or interferon alpha-2b
could be effective following surgery (12,13).
However, to the best of our knowledge, there is no previous report
on persistent bleeding from giant melanoma. CT findings
demonstrated marked enhancements in the tumor mimicking hemangioma,
although the lack of quantification of the marked enhancement
observed in the CT scan is a potential limitation of the present
study. To our knowledge, there are currently no reliable guidelines
for bleeding associated with conjunctival melanoma. In the case of
the present study, persistent bleeding was clinically caused by the
surface of the tumor tissue, but the orbital was not increased
pressure, since there were no lesions in the deep orbit on CT.
Persistent bleeding arising in giant conjunctival melanoma may be
challenging. One of the associated complications is likely to be
anemia, which seriously affects patients' life. Furthermore, the
procedure of stopping bleeding is not established. In the present
case, local hemostasis or suture at the bleeding site could not
completely resolve the problem. Therefore, complete tumor resection
with extensive eyelid reconstruction or orbital exenteration was
mandatory to stop the persistent bleeding after the first episode.
By contrast, orbital decompression with lateral orbitotomy would
not be effective because the cause of bleeding was not increased
orbital pressure. In this case, since the tumor was large, the area
of tumor cell invasion onto the ocular surface could not be
evaluated. Furthermore, because CT also indicated tumor cell
invasion to the anterior orbit, orbital exenteration was eventually
chosen as a treatment option in order to remove all tumor
tissues.
The second novel finding was that the tumor
histopathologically contained a variety of small-to-large vascular
channels, which were consistent with marked enhancements on CT. In
addition, hemangioma-like collections of intratumoral microvessels
were intermingled within the tumor tissue at the bleeding site.
These findings are likely to have caused the persistent bleeding
clinically observed. Three reports on giant conjunctival melanoma
mentioned pathological findings in addition to histological
diagnoses. Histopathology of giant conjunctival melanoma
demonstrated that tumor cells were classified as the epithelioid
cell-type (8,9). Tumor tissues presented with
ulceration on the surface (9), and
tumor cells were dispersed in fibrin and sites of hemorrhage
(8), being similar to the
histopathology of the present case. Supit et al (11) demonstrated that tumor cells invaded
the retrobulbar vasculature and fat tissue. However, there were no
reports on hemangioma-like abundant vascular channels within tumor
tissues. Of note, the intratumoral vascular configurations have
remained to be fully understood in conjunctival melanoma. A
previous study by our group demonstrated that CD34-positive
endothelial cells were less marked in melanoma tissues than in
non-cancerous adjacent conjunctiva in the same patients (5). In addition, Tuomaala et al
(14) clarified that intratumoral
microvessel density was not associated with recurrence, suggesting
that research on vascular configurations in conjunctival melanoma
has not fully progressed. We would herein like to propose a novel
variant of conjunctival melanoma with rich vascularization,
clinically causing relentless bleeding.
In the present case, the primary diagnosis of the
eyelid tumor was hemangioma. Although conjunctival melanoma is
rare, ophthalmologists and plastic surgeons should pay attention to
clinical findings of the subcutaneous eyelid mass, revealing an
elastic, hard mass in the present case. On the other hand,
hemangioma should present with an elastic, soft mass. In addition,
the clinical response to surgical procedures such as puncture of
the cystic lesion, leading to immediate enlargements of the
elevated lesions, should be taken into consideration. If the
response is poor and mass lesions grow rapidly, they should
consider the possibility of malignancy; also in the present case,
pathological confirmation should have been obtained sooner.
Regarding CT findings in the present patient, the findings of
conjunctival melanoma may not be typical, showing enhancements
involving a lesion in the anterior orbit. In addition, after the
onset, no orbital MRI had been recorded; therefore, preoperative
orbital MRI examination would have aided the diagnosis and
treatment of the disease. If the primary physicians are aware of
the vascular-rich conjunctival melanoma, they may evaluate the
clinical findings as showing a malignant tumor.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
SK wrote the whole manuscript and substantially
contributed to the present study. KOH significantly contributed to
the pathological diagnosis. YS, MM and SI substantially contributed
to the drafting of the manuscript. All authors critically reviewed
and revised the manuscript draft and have read and approved the
final version for submission. SK and MM checked and confirmed the
authenticity of the raw data.
Ethics approval and consent to
participate
The present study adhered to the tenets of the
Declaration of Helsinki.
Patient consent for publication
The patient provided written, retrospective consent
for the publication of the clinical information and images
following detailed explanation of the purpose of the study and
understanding that no identifiable information was going to be
released.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Višnjić A, Kovačević P, Veličkov A,
Stojanović M and Mladenović S: Head and neck cutaneous melanoma:
5-year survival analysis in a Serbian university center. World J
Surg Oncol. 18(312)2020.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Heindl LM, Hofmann-Rummelt C, Adler W,
Bosch JJ, Holbach LM, Naumann GO, Kruse FE and Cursiefen C:
Tumor-associated lymphangiogenesis in the development of
conjunctival melanoma. Invest Ophthalmol Vis Sci. 52:7074–7083.
2011.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Kase S, Osaki M, Honjo S, Adachi H,
Tsujitani S, Kaibara N and Ito H: Expression of cyclo-oxygenase-2
is correlated with high intratumoral microvessel density and low
apoptotic index in human esophageal squamous cell carcinomas.
Virchows Arch. 442:129–135. 2003.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Pastushenko I, Vermeulen PB, Carapeto FJ,
Van den Eynden G, Rutten A, Ara M, Dirix LY and Van Laere S: Blood
microvessel density, lymphatic microvessel density and lymphatic
invasion in predicting melanoma metastases: Systematic review and
meta-analysis. Br J Dermatol. 170:66–77. 2014.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Kase S, Kikuchi I and Ishida S: Expression
of VEGF in human conjunctival melanoma analyzed with
immunohistochemistry. Clin Ophthalmol. 12:2363–2367.
2018.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Palme C, Wanner A, Romano V, Franchi A,
Haas G, Kaye SB and Steger B: Indocyanine green angiographic
assessment of conjunctival melanocytic disorders. Cornea.
40:1519–1524. 2021.PubMed/NCBI View Article : Google Scholar
|
|
7
|
American Joint Committee on Cancer (AJCC):
AJCC cancer staging manual. Conjunctival melanoma. 8th edition.
Springer, New York, NY, pp795-803, 2017.
|
|
8
|
Matsuo T, Yamasaki O, Tanaka T, Katsui K
and Waki T: Proton beam therapy followed by pembrolizumab for giant
ocular surface conjunctival malignant melanoma: A case report. Mol
Clin Oncol. 16(12)2022.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Cekic SP, Kovacevic PT and Krstic MS:
Giant conjunctival melanoma treated with excision and primary
reconstruction using a partial thickness skin graft. Niger J Clin
Pract. 26:1204–1207. 2023.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Malik KPS, Dadeya S, Gulliani BP and Gupta
VS: Favourable outcome of giant malignant melanoma of the
conjunctiva despite poor prognostic features. Can J Ophthalmol.
38:397–400. 2003.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Supit T, Pujisriyani Subiyakto, Nugroho T,
Fitrikasari A and Najatullah : Giant conjunctival melanoma in
a paranoid schizophrenic man: A case report. Ann Med Surg (Lond).
62:391–394. 2021.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Kikuchi I, Kase S, Ishijima K and Ishida
S: Long-term follow-up of conjunctival melanoma treated with
topical interferon alpha-2b eye drops as adjunctive therapy
following surgical resection. Graefes Arch Clin Exp Ophthalmol.
255:2271–2276. 2017.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Nuessle S, Auw-Haedrich C, Jiang J,
Boehringer D and Reinhard T: Real-life data of adjuvant IFN-α2b and
MMC in conjunctival melanocytic lesions. Graefes Arch Clin Exp
Ophthalmol. 261:1159–1166. 2023.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Tuomaala S, Toivonen P, Al-Jamal R and
Kivelä T: Prognostic significance of histopathology of primary
conjunctival melanoma in Caucasians. Curr Eye Res. 32:939–952.
2007.PubMed/NCBI View Article : Google Scholar
|