Introduction
Metastatic carcinoma in the lung generally presents
with multiple nodular shadows. Metastatic carcinoma may present
with ground glass opacity (GGO), usually with diffuse form, on
chest computed tomography (CT). Diffuse GGO represents lymphatic
and/or vascular spread of carcinoma in the lung (1). Focal GGO, which is localized or
nodular form on chest CT, is uncommon in metastatic carcinoma.
Since various lung diseases such as interstitial fibrosis,
inflammation and primary lung adenocarcinoma present with GGO, it
is difficult to reach an accurate diagnosis based solely on
radiological findings. Thus, in a case with past history of
carcinoma, pathological assessment of focal GGO by biopsy or
partial resection is necessary to determine whether the lesion is
primary or metastatic carcinoma. The assessment is also critical to
decide appropriate treatment.
We herein present a case of metastatic carcinoma
presenting with focal GGO. A definite diagnosis of metastatic
prostate cancer was reached by CT-assisted percutaneous needle
biopsy and histological and immunohistochemical examinations. We
present characteristic histological and immunohistochemical
features of the case. We also reviewed a literature and found cases
of metastatic cancer, presenting with focal GGO (2-10),
and three cases were metastatic prostate cancer. It is of note two
out of three cases were associated with pulmonary tumor thrombotic
microangiopathy (PTTM), which rapidly progresses and is fatal
(11). The vascular pathology
needs to be assessed in biopsy specimen. The histological and
clinical features of PTTM, which are necessary for immediate
diagnosis, are also reviewed.
Case report
A 75-year-old man, who had a medical history of
metachronous prostate and gastric cancers, presented at Kashiwa
Kousei General Hospital, Kashiwa, Japan in September 2023 for the
follow-up examination of the cancers. He was diagnosed as prostate
cancer in another hospital 12 years before. Multiple bone
metastases were detected in the spine. The histology of biopsy
specimen of the prostate was adenocarcinoma with Gleason score 4+4.
The patient had been treated with androgen deprivation therapy
(ADT) for 12 years. The patient also received pelvic irradiation.
Bone metastases appeared to be stable by ADT. However, a gradual
increase was observed in the level of prostate-specific antigen
(PSA). Seven months before, the patient underwent subtotal
gastrectomy for multiple gastric cancers, which were detected in a
health examination in Kashiwa Kousei General Hospital. There were
three gastric cancers in the resected stomach. The main cancer was
well-differentiated adenocarcinoma with focal moderately
differentiated adenocarcinoma, and carcinoma cells invaded the
submucosa. Neither blood nor lymphatic invasion was observed. The
two other cancers were well-differentiated adenocarcinomas that
were confined to the mucosa. Lymph node metastasis was not
found.
Red and white blood cell counts were
4.09x106/µl and 4.1x103/µl, respectively. His
platelet count was 69x103/µl. Serum levels of
carcinoembryonic antigen and CA19-9 were within normal limits. His
PSA level was elevated to 7.62 ng/ml. His fibrinogen level was 283
ng/dl and fibrinogen degradation products (FDP) were below the
detection level. Echo cardiogram showed no abnormalities. The
patient did not have dyspnea or respiratory discomfort. Pulmonary
function tests were normal.
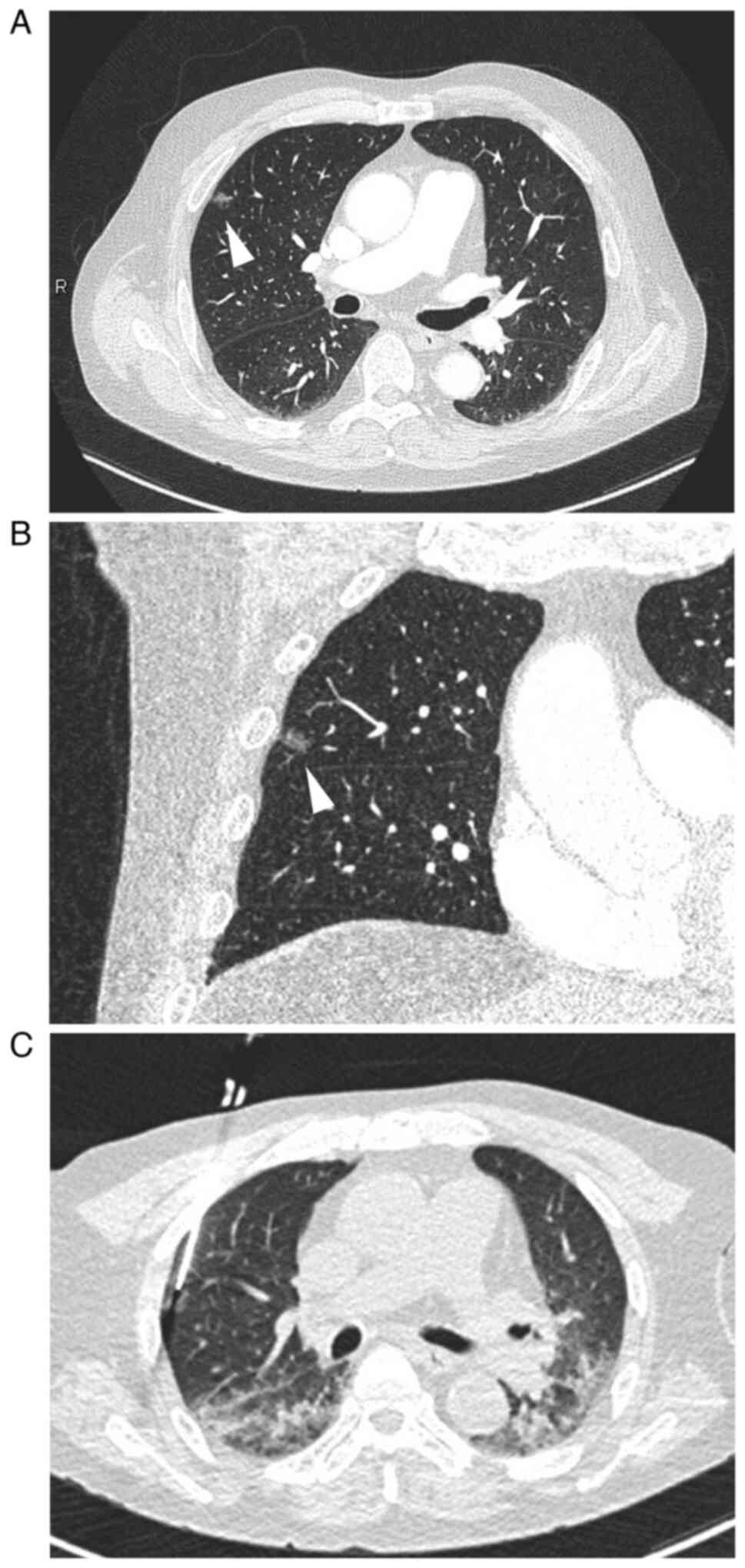
Chest CT revealed a focal GGO with a minimal solid
area, measuring 11 mm in diameter, in the periphery of the right
upper lobe (Fig. 1A and B). Pulmonary vessels and bronchioles were
not involved. Since primary lung adenocarcinoma was suspected,
CT-assisted percutaneous needle biopsy was performed (Fig. 1C).
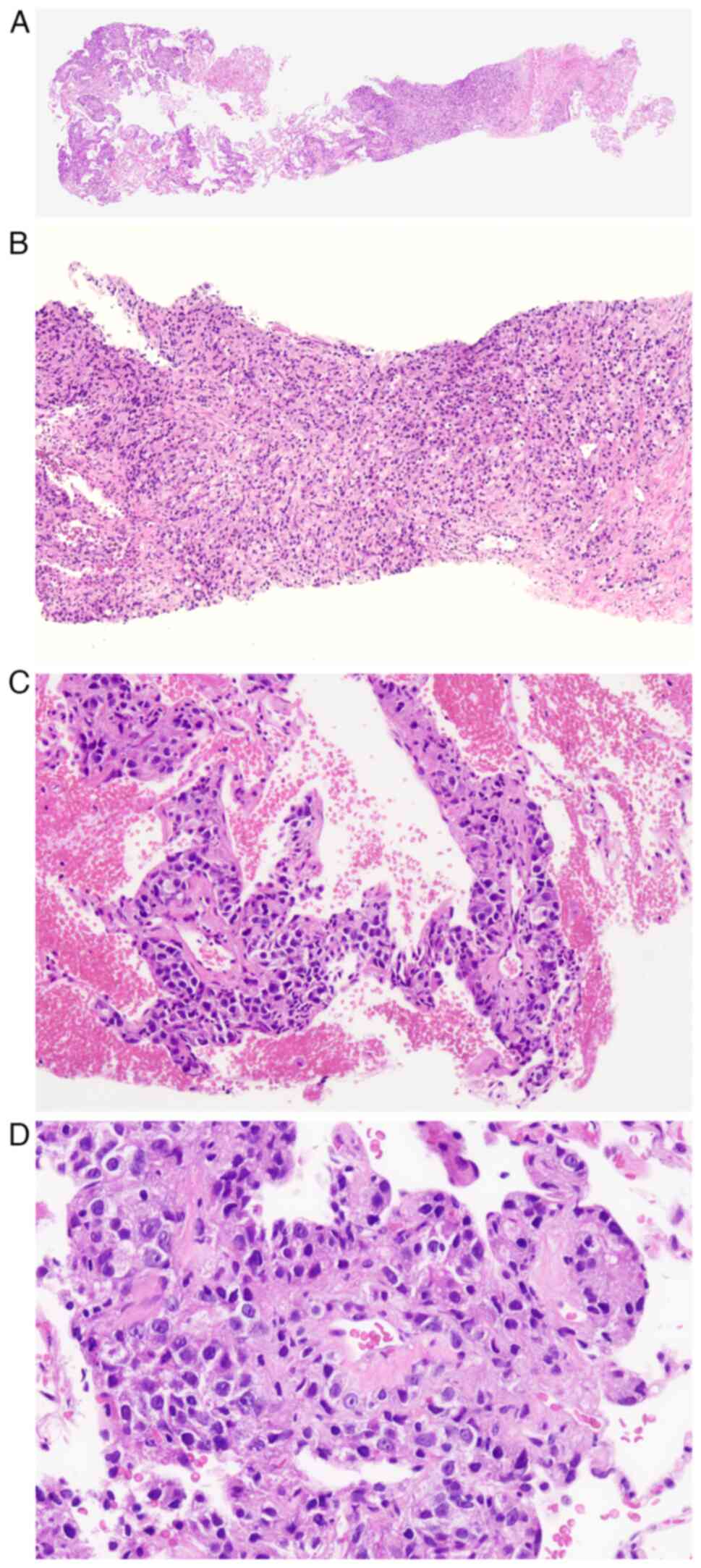
The biopsy specimen showed the proliferation of
atypical cells in fibrous tissue and the alveolar septa (Fig. 2A). In fibrous tissue, atypical
cells proliferated in sheet-like, trabecular, and vague glandular
patterns, suggesting that the lesion was moderately to poorly
differentiated adenocarcinoma (Fig.
2B). The surrounding alveolar wall was thickened by the
invasion of the poorly differentiated component of adenocarcinoma
into the interstitial space (Fig.
2B). Neither the lepidic growth of carcinoma cells within the
alveolar space nor invasion into the alveolar space was observed. A
tumor thrombus was not found in the blood or lymphatic vessels
(Fig. 2C), and there was no
stenosis or re-canalization of vessels. The perivascular
infiltration of macrophages and fibrocellular intimal proliferation
were not present.
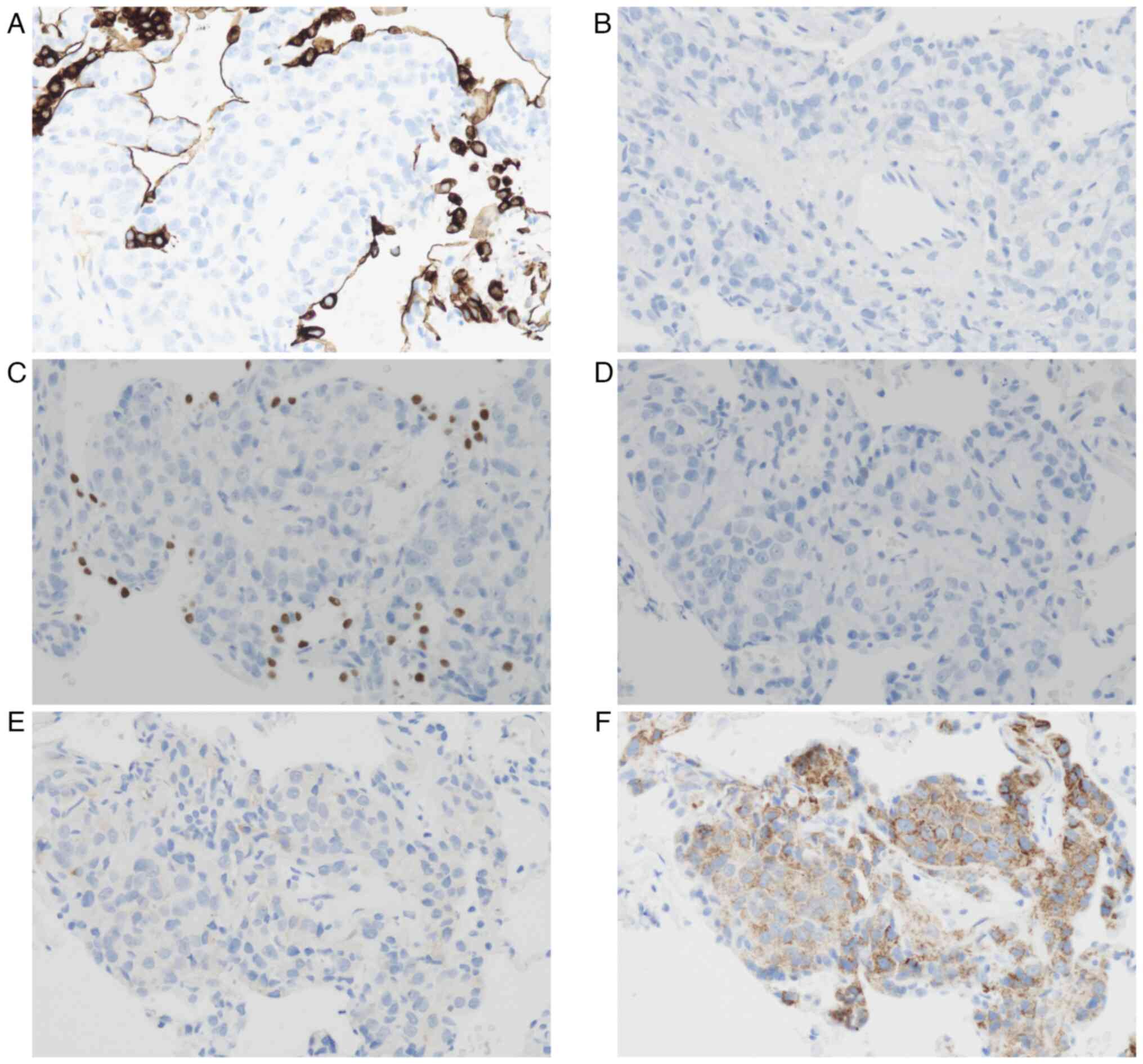
The phenotype of carcinoma cells was examined by
immunohistochemistry (IHC). Carcinoma cells were negative for
cytokeratin 7 (CK7) and CK20 (Fig.
3A and B) as well as thyroid
transcription factor-1 (TTF1) and CDX2 (Fig. 3C and D). Therefore, primary lung adenocarcinoma
and metastatic gastric cancer were considered to be unlikely.
Carcinoma cells showed a faint positive reaction with PSA (Fig. 3E) and strong positive reaction with
P504S (Fig. 3F). Based on these
findings, the patient was diagnosed with metastatic carcinoma from
prostate cancer. IHC with CK7 and TTF1 also clearly showed the
subepithelial proliferation of carcinoma cells (Fig. 3A and C).
After the diagnosis, ADT was continued, and the
patient is being followed up with careful observations. The
condition has remained stable, and new lesions were not detected in
the lungs 4 months since the diagnosis. Furthermore, there have
been no abnormalities in laboratory data.
Discussion
Metastatic carcinoma and malignant neoplasms
generally present as nodular shadows in the lungs; however, GGO may
be encountered in cases of lung metastasis (1). Diffuse and patchy GGO are caused by
diffuse thickening of the alveolar wall due to lymphangitic
carcinomatosis or PTTM, and the most frequent primary site of
carcinoma is the gastrointestinal tract. Focal GGO is rarely found
in metastatic carcinoma and malignant neoplasms, but has been
documented in cases of malignant melanoma (2-4),
malignant phyllodes tumor (5),
tongue cancer (6), thyroid cancer
(7), and prostate cancer (8-10),
including the present case (Table
I). Since it was not feasible to distinguish metastatic lesions
from primary lung adenocarcinoma based solely on radiological
findings, a diagnosis was made by a histological examination of
partially resected lung or biopsy specimens in the reported cases.
In the present case, which had a previous history of metachronous
prostate and gastric cancers, CT-assisted percutaneous needle
biopsy was performed for a definitive diagnosis of the lesion.
 | Table IReported cases of metastatic neoplasms
presenting with focal ground glass opacity. |
Table I
Reported cases of metastatic neoplasms
presenting with focal ground glass opacity.
| Author | Age, years | Sex | Size, mm | Specimen | Histology | (Refs.) |
|---|
| Malignant
melanoma | | | | | | |
|
Kang MJ | 56 | M | 11 | VATS | Subepithelial
proliferation of melanoma cells | (2) |
|
Okita R | 56 | F | 28 | VATS | Subepithelial
proliferation of melanoma cells | (3) |
|
Mizuuchi
H | 57 | M | 10 | WR | Proliferation in a
‘lepidic-like’ fashion | (4) |
| Malignant phyllodes
tumor | | | | | | |
|
Nakamura
S | 71 | F | 21 | VATS | Subepithelial
proliferation of neoplastic cells | (5) |
| Tongue cancer | | | | | | |
|
Haro A | 22 | M | 24 | WR | Invasion and
destruction of alveoli and hemorrhage | (6) |
| Thyroid cancer | | | | | | |
|
Ryuko T | 68 | M | 8 | VATS | Lepidic growth of
carcinoma cells | (7) |
| Prostate cancer | | | | | | |
|
Lubin
DJ | 62 | M | 14 | Resection | Lymphatic and
perilymphatic growth of carcinoma cells | (8) |
|
Osaki Y | 67 | M | ND | Autopsy | PTTM | (9) |
|
Katayama
S | 81 | M | Micronodular | TBLB/Autopsy | PTTM | (10) |
|
Present
case | 75 | M | 11 | PNB | Subepithelial
proliferation of carcinoma cells | - |
In biopsy specimens, it is important to confirm
whether the lesion is primary lung adenocarcinoma. A benign lesion
of interstitial pneumonia and other benign lesions are also
carefully differentiated. If metastatic adenocarcinoma is
suspected, the primary site needs to be identified by IHC with
specific markers. In the present case, carcinoma cells were
negative for CK7 and TTF1, suggesting that primary lung
adenocarcinoma was unlikely. Furthermore, a negative reaction for
CDX2 indicated that gastric cancer was unlikely. The confirmation
of metastatic prostate cancer was reached by positive reactions for
PSA and P504S. The majority of prostate cancers are negative for
CK7 and CK20(12). The expression
of PSA may be attenuated by long-term ADT (13).
GGO is caused by various pathological conditions,
such as interstitial fibrosis, inflammatory cell infiltration,
thrombosis, and the lepidic growth of carcinoma cells (1). In the present case, GGO was
attributed to thickening of the alveolar walls due to the extension
of carcinoma cells beneath alveolar epithelial cells. This
extension was evident by IHC, and proliferating carcinoma cells
were covered with alveolar epithelial cells, which were positive
for CK7 and TTF1 (Fig. 3A and
C). The subepithelial growth of
carcinoma cells is similar to reported cases of malignant melanoma
(2-4)
and malignant phyllodes tumor (5).
Lepidic growth similar to primary lung adenocarcinoma was
previously documented in a case of metastatic thyroid cancer
(7), and focal GGO was caused by
the invasion and destruction of alveoli and hemorrhage in a case of
metastatic tongue cancer (6).
Careful attention of reported cases of metastatic
prostate cancer with focal GGO is needed (Table I). Two of the three cases were
associated with PTTM (9,10), while one was associated with
lymphangitic carcinomatosis (8).
These conditions generally present with diffuse GGO. The clinical
course of PTTM is rapid and fatal; therefore, an immediate
diagnosis is essential. Respiratory failure, pulmonary
hypertension, an elevated D-dimer level, and thrombocytopenia
indicate PTTM in cases with a previous history of carcinoma
(11). PTTM may be diagnosed using
biopsy specimens. The pathological features of PTTM are a tumor
thrombus, fibrocellular intimal proliferation, and the
recanalization of vessels. The perivascular infiltration of
macrophages may also be present because the inflammatory process
plays an important role in the pathogenesis of PTTM (14,15).
In the present case, these histological changes were not observed
in the biopsy specimen. Respiratory failure was absent and there
was neither a decrease in the platelet count nor an elevation in
FDP. Although the patient's condition was stable, he needs to be
followed up with careful attention to laboratory data and
radiological findings.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used during the present study are
available from the corresponding author upon reasonable
request.
Authors' contributions
RW, TY, KI, SU, NM, and HN participated in the
diagnosis and treatment of the patient and wrote the first draft of
this manuscript. RW and HN confirm the authenticity of all the raw
data. All authors have read and approved the final manuscript.
Ethics approval and consent to
participate
Ethics approval for the study was obtained from the
Ethics Committee of Kashiwa Kousei General Hospital (approval no.
240025) dated February 26, 2024.
Patient consent for publication
Written informed consent was obtained from the
patient to publish this case report and any accompanying
images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Seo JB, Im JG, Goo JM, Chung MJ and Kim
MY: Atypical pulmonary metastases: Spectrum of radiologic findings.
Radiographics. 21:403–417. 2001.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Kang MJ, Kim MA, Park CM, Lee CH, Goo JM
and Lee HJ: Ground-glass nodules found in two patients with
malignant melanomas: Different growth rate and different histology.
Clin Imaging. 34:396–399. 2010.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Okita R, Yamashita M, Nakata M, Teramoto
N, Bessho A and Mogami H: Multiple ground-glass opacity in
metastasis of malignant melanoma diagnosed by lung biopsy. Ann
Thorac Surg. 79:e1–e2. 2005.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Mizuuchi H, Suda K, Kitahara H, Shimamatsu
S, Kohno M, Okamoto T and Maehara Y: Solitary pulmonary metastasis
from malignant melanoma of the bulbar conjunctiva presenting as a
pulmonary ground glass nodule: Report of a case. Thorac Cancer.
6:97–100. 2015.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Nakamura S, Goto T, Nara S, Kawahara Y,
Yashiro S, Kano S, Hosokawa Y and Kamada H: Pure ground glass
opacity (GGO) on chest CT: A rare presentation of lung metastasis
of malignant phyllodes tumor. Breast Cancer. 27:1187–1190.
2020.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Haro A, Wakasu S, Takada K, Osoegawa A,
Kamitani T, Tagawa T and Mori M: Pulmonary metastasis presenting as
a ground glass opacity-like lesion with a thin-walled cavity: A
case report. Int J Surg Case Rep. 60:287–290. 2019.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Ryuko T, Sano Y, Kitazawa R, Otani S,
Sakao N and Mori Y: Lung metastasis from thyroid carcinoma showing
a pure ground-glass nodule. Ann Thorac Surg. 114:e253–e256.
2022.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Lubin DJ, Holden SB, Rettig MB, Reiter RE,
King CR, Lee JM, Wallace DW and Calais J: Prostate cancer pulmonary
metastasis presenting as a ground-glass pulmonary nodule on
68Ga-PSMA-11 PET/CT. Clin Nucl Med. 44:e353–e356. 2019.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Osaki Y, Taoka R, Miyauchi Y and Sugimoto
M: Docetaxel chemotherapy temporarily improved pulmonary tumor
thrombotic microangiopathy induced by prostate cancer secreting
carcinoembryonic antigen and carbohydrate antigen 19-9: A case
report. Urol Case Rep. 29(101098)2020.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Katayama S, Takenaka T, Nakamura A, Sako
S, Bessho A and Ohara N: Pulmonary tumor thrombotic microangiopathy
induced by prostate cancer. Acta Med Okayama. 72:309–313.
2018.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Godbole RH, Saggar R and Kamangar N:
Pulmonary tumor thrombotic microangiopathy: A systematic review.
Pulm Circ. 9:1–13. 2019.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Dum D, Menz A, Völkel C, De Wispelaere N,
Hinsch A, Gorbokon N, Lennartz M, Luebke AM, Hube-Magg C, Kluth M,
et al: Cytokeratin 7 and cytokeratin 20 expression in cancer: A
tissue microarray study on 15,424 cancers. Exp Mol Pathol.
126(104762)2022.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Ogreid P, Berner A, Dahl O, Rettedal E and
Fossa SD: Tissue prostate-specific antigen and androgen receptor
immunoreactivity in prostate cancer biopsies before, during and
after neo-adjuvant androgen deprivation followed by radiotherapy.
Eur Urol. 36:116–122. 1999.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Mantovani A, Allavena P, Sica A and
Balkwill F: Cancer-related inflammation. Nature. 454:436–444.
2008.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Price LC, Wells AU and Wort SJ: Pulmonary
tumour thrombotic microangiopathy. Curr Opin Pulm Med. 22:421–428.
2016.PubMed/NCBI View Article : Google Scholar
|