Introduction
Epidermal inclusion cysts (EICs) are benign nodules
often misnamed as sebaceous cysts because they are filled with
keratin (protein) rather than sebum (oil). They are non-cancerous
nodules that develop due to entrapped epidermal cells (1). These cysts typically appear on the
scalp, face, neck, trunk, and back (1-3).
They rarely occur within lymph nodes, termed nodal epidermal
inclusion cysts (NEICs). These have been reported in the pelvic,
abdominal, mediastinal, and axillary regions (4). Epidermal inclusion cysts can occur at
any age however they are more common between the third and fourth
decades of life and predominantly affect males (1). Cutaneous cysts are classified into
true cysts and pseudocysts: True cysts are either lined by
stratified or non-stratified squamous epithelium, while pseudocysts
lack an epithelial lining (1,2). The
presence of an epidermal cyst within an axillary lymph node is an
infrequent occurrence.
The present study aimed to report a case of an EIC
within an axillary lymph node, incidentally discovered during the
histopathological study of a sentinel axillary lymph node biopsy in
a patient with invasive ductal carcinoma of the breast.
Case report
Patient information
A 55-year-old woman, gravida six and para six,
presented with a two-week history of a right breast mass. The
patient had no notable medical history apart from a total
thyroidectomy performed 6 years ago. Family history was positive
for both breast and thyroid cancer. Written informed consent was
obtained from the patient for the participation in the present
study, for the publication of the present case report and for any
accompanying images.
Clinical findings
On the same day of presentation, examination
revealed a small, firm, fixed, and painless lump in the upper outer
quadrant of the right breast, while no palpable lymphadenopathy or
lymph node abnormalities in the axillary region and no skin surface
changes, erythema, discharge, or systematic symptoms were
observed.
Diagnostic approach
Laboratory tests were conducted on the same day and
they were within the normal ranges. The following day, a breast
ultrasound (U/S) was conducted and revealed a small, irregular, and
hypoechoic mass measuring 7x6 mm at 10 o'clock in the posterior
depth of the right breast. Axillary sonography revealed no abnormal
lymph nodes (BIRADS score U6) and core needle biopsy of the mass
confirmed the diagnosis of invasive ductal carcinoma.
Therapeutic intervention
After 1 week of the patient's visit to the hospital,
wide local excision of the lump was performed with an axillary
lymph node sentinel biopsy. Gross examination revealed a 1.3-cm
poorly defined, firm, white, spiculated mass within the breast. The
axillary lymph nodes, with two stained and one unstained, appeared
entirely normal. The tissue samples underwent fixation in formalin
and embedding in paraffin. Sections of 4-µm thickness were then cut
using a microtome and stained using conventional hematoxylin and
eosin stain from MilliporeSigma. This staining procedure occurred
at room temperature over a duration of 65 min, utilizing a
Tissue-Tek Prisma Plus Automated slide stainer from Sakura Finetek
Europe B.V. Examination of the stained sections was conducted using
an Olympus BX-51 microscope equipped with a camera adaptor (Olympus
U-TV0.5XC-3; Olympus Corporation) to capture images. Microscopic
examination revealed a unifocal invasive ductal carcinoma of no
specific type, moderately differentiated, without lymph vascular
invasion, associated with low-grade ductal carcinoma in situ
within the tumor boundary. All three lymph nodes were tumor-free.
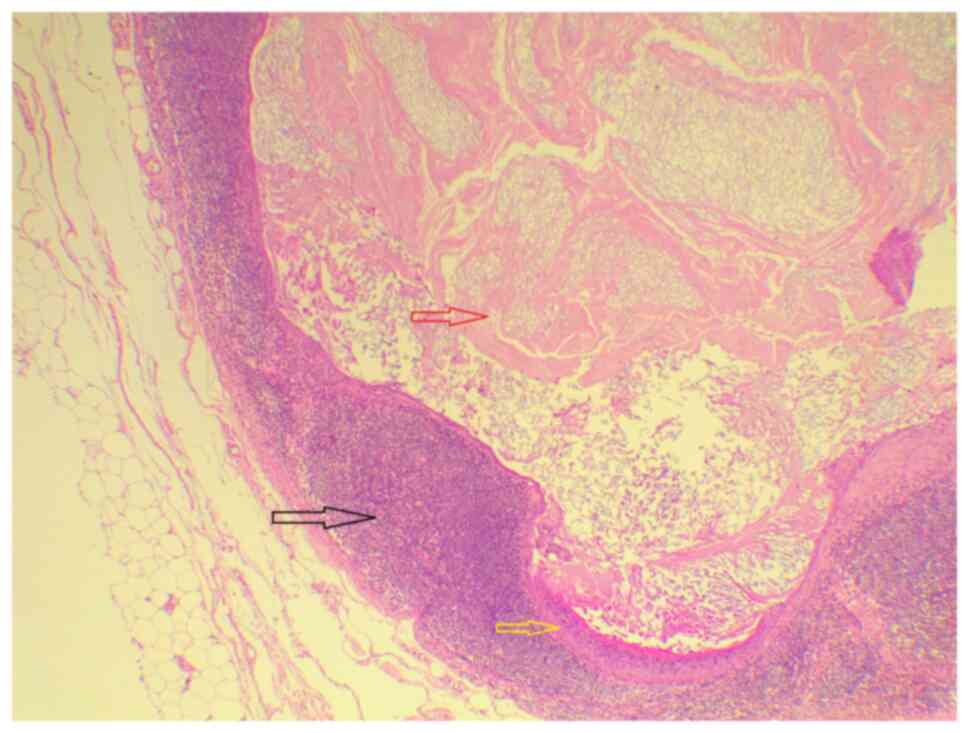
Notably, one the stained lymph nodes, however, contained a
unilocular cyst filled with laminated keratin and lined by
stratified squamous epithelium with a prominent granular layer and
a surrounding giant cell reaction (Fig. 1). These findings were consistent
with an intranodal EIC that had no relation to the invasive ductal
carcinoma within the ipsilateral breast.
Follow-up and outcome
The post-operative period was uneventful, and the
patient was scheduled for follow-up.
Discussion
Epidermal inclusion cysts, referred to by various
names such as epidermal cysts, sebaceous cysts, or infundibular
cysts, are non-cancerous sacs that develop due to the overgrowth of
skin cells within the dermal or subcutaneous layers, resulting in
the creation of a cyst filled with keratin (5,6).
These cysts can manifest in various locations across the body,
typically appearing as nodules directly beneath the skin surface,
and often exhibiting a visible central punctum. Epidermal cysts
primarily contain keratin rather than sebum within their centers.
The cysts do not originate from sebaceous glands; hence, they are
distinct from sebaceous cysts. While the terms ‘sebaceous’ and
‘epidermoid’ cysts should not be used interchangeably, in clinical
settings, this distinction is often overlooked (7).
The formation of an EIC typically involves a
combination of factors such as trauma, epithelial proliferation, or
minimal inflammation. Additionally, since EICs are often
asymptomatic and slow-growing, patients may not readily associate
the lesion with any previous trauma they may have experienced
(8). In the present case report,
the patient did not report any history of trauma or surgical
procedure in the region of the cyst.
Benign inclusions within lymph nodes were initially
documented by Ries in 1897, who categorized them into three groups:
Epithelial, nevomelanocytic, and decidual (9). Fellegara et al (10) further classified nodal epithelial
inclusions into glandular, squamous, and mixed types. The lymph
nodes most commonly affected vary depending on the type of
heterotopic inclusion. For instance, axillary nodes often contain
breast tissue and nevus cells, while cervical nodes may harbor
salivary glands or thyroid tissue. Pelvic and retroperitoneal nodes
may exhibit decidual tissue, intestinal glands, or mesothelial
cells. The origin of these epithelial inclusions remains a subject
of debate, with proposed theories including embryogenic,
implantation (iatrogenic), and metaplastic origins (11).
Complications associated with EICs include rupture,
inflammatory alterations, or the formation of abscesses, which can
pose challenges in achieving an accurate imaging diagnosis. In rare
instances (~2% of cases), malignant transformation into squamous
cell carcinoma within the EIC wall has been reported. Suspicion of
malignant degeneration should arise if solid nodules are detected
alongside the cyst wall (5). In
the present study, clinical signs of infection or malignant change
were absent.
Ultrasonography is prioritized as the primary
imaging method for assessing superficial soft tissue masses,
including those within the skin, due to its high-resolution
capabilities, absence of radiation, cost-effectiveness, and
widespread availability. This makes it preferable over other
modalities such as computed tomography or magnetic resonance
imaging. When assessing palpable lesions in the axilla, ultrasound
serves to identify and pinpoint the lesion, distinguishing between
lymph nodes and soft tissue masses that might require preoperative
tissue confirmation. In cases reported in reputable scientific
literature from non-predatory journals where ultrasound reveals
characteristic or distinctive features, a precise sonographic
diagnosis can be achieved without the need of a biopsy, potentially
averting further unnecessary examinations (5,12).
During ultrasonography, an EIC might exhibit a solid and
well-defined structure, appearing complex or heterogeneous. In
certain instances, it may display a distinctive concentric pattern
resembling onion rings, with alternating hypoechoic and hyperechoic
layers (13). In a study by
Abu-Mandeel et al (3),
which involved a 41-year-old patient, the ultrasound revealed a
hypo-echoic subcutaneous mass in the right axilla with internal
foci corresponding to calcifications consistent with the present
study, in which U/S of the breast and axilla revealed a small,
irregular, hypoechoic mass measuring 7x6 mm within the breast with
no abnormalities in the axillary lymph nodes.
Due to its wide prevalence, notable advancements
have been made in diagnosing and treating breast cancer across
sexes. Despite this, several critical clinical and scientific
challenges persist regarding prevention, diagnosis, prognosis,
recurrence, and treatment options. These challenges are further
highlighted by the occasional coexistence of benign EIC with breast
malignancies (2,14). Typically, small, uncomplicated
cysts do not require treatment. However, if removal is desired, it
can be achieved through a straightforward surgical excision,
ensuring the complete removal of the cyst along with its intact
wall (10). Benign epithelial
inclusion cysts can occur in patients with or without associated
breast pathology and, rarely, they are discovered within lymph
nodes alongside metastatic breast carcinoma. Fisher et al
(15) documented a case involving
a 55-year-old woman diagnosed with infiltrating ductal carcinoma.
During axillary dissection, two lymph nodes were extracted,
confirming metastatic carcinoma and associated epithelial inclusion
cysts. In a study reported in the literature, a histopathological
examination of a sample from a 41-year-old patient, stained with
hematoxylin and eosin, revealed depiction of the cyst wall,
presence of squamous epithelial lining, and accumulation of
laminated keratin layers (3).
Additionally, in a study which reported multiple bilateral EICs, a
biopsy revealed a cyst with a lining of multiple layers of squamous
epithelial cells and a cavity filled with keratin (16). In line with these studies, in the
current case, EIC was diagnosed incidentally in the sentinel lymph
node biopsy of a case with invasive ductal carcinoma of the breast;
three lymph nodes were isolated, two of which were stained (with
the methylene blue dye used for the sentinel biopsy procedure), and
all were free from tumors. Notably, one of the stained lymph nodes,
however, revealed a keratinous EIC with a giant cell reaction.
The coexistence of benign EICs with breast
malignancies presents diagnostic challenges for pathologists,
radiologists and clinicians. Pathologists should be vigilant in
histopathological examination to identify incidental EICs within
lymph nodes, necessitating thorough communication with clinicians.
Radiologists play a pivotal role in recognizing the sonographic
features of EICs during ultrasound evaluation, aiding in accurate
diagnosis and treatment planning. Clinicians should consider the
potential presence of concurrent benign lesions such as EICs when
interpreting diagnostic findings, emphasizing multidisciplinary
collaboration to ensure comprehensive patient care and optimal
outcomes. Integration of these recommendations into clinical
practice can enhance diagnostic accuracy and improve patient
management in breast cancer cases. A limitation of the present
study is the absence of ultrasound imaging. Additionally, although
a small, firm, fixed, and painless lump in the upper outer quadrant
of the right breast was revealed upon examination, representative
images of this mass are unavailable. Regrettably, due to the lack
of captured ultrasonographic images at the time of examination and
the early stages of electronic medical record adoption in the
authors' region, technical challenges are still faced, resulting in
some images being unretrievable.
In conclusion, it was deemed valuable to document
this rare instance of an EIC found within an axillary lymph node to
raise awareness among pathologists regarding this unusual benign
condition within lymph nodes. Recognizing this rare entity can help
prevent misdiagnosis of a malignant lesion, particularly metastatic
carcinoma in this context, thus avoiding unnecessary
treatments.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
AMS was a major contributor to the conception of the
present study, as well as to the literature search for related
studies. RSA, HOB and ROM were involved in the literature review,
study design, and writing the manuscript, as well as the follow-up
of the patient. SSO, AAQ, HOA and FHK were involved in the
literature review, the design of the present study, the critical
revision of the manuscript, and the processing of the figure. FHK
and AAQ confirm the authenticity of all the raw data. AMA and RMA
were the pathologists who performed the histopathological
diagnosis. LRAP was the radiologist who assessed the case. All
authors have read and approved the final version of the
manuscript.
Ethics approval and consent to
participate
In Sulaymaniyah, Iraq, ethical approval is not
required for case studies with <3 cases. Written informed
consent was obtained from the patient for participation in the
present study.
Patient consent for publication
Written informed consent was obtained from the
patient for the publication of the present case report and any
accompanying images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Zito P and Schar FC: Epidermoid (Sebaceous
Cyst). StatPearls StatPearls Publishing, Treasure Island, FL,
2019.
|
|
2
|
Hoang VT, Trinh CT, Nguyen CH, Chansomphou
V, Chansomphou V and Tran TTT: Overview of Epidermal cyst. Eur J
Radiol Open. 6:291–301. 2019.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Abu-Mandeel E, Saadeh A, Rababaa H and
Al-Share MS: Epidermal inclusion cyst of the axilla with
calcifications. Radiol Case Rep. 18:784–787. 2022.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Sigei AC, Bartow BB and Wheeler Y:
Sentinel lymph node involvement by epithelial inclusions mimicking
metastatic carcinoma: A diagnostic pitfall. Am J Case Rep.
21(e926094)2020.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Lee JY: Giant epidermal inclusion cyst of
the axilla: A case report with diagnostic ultrasound imaging
features. Radiol Case Rep. 17:64–67. 2021.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Abdullah AS, Ahmed AG, Mohammed SN, Qadir
AA, Bapir NM and Fatah GM: Benign Tumor Publication in One Year
(2022): A Cross-Sectional Study. Barw Med J. 1:20–25. 2023.
|
|
7
|
Weir CB and St Hilaire NJ: Epidermal
Inclusion Cyst. In: StatPearls. StatPearls Publishing, Treasure
Island, FL, 2023.
|
|
8
|
Kini YK, Kharkar VR, Rudagi BM and
Kalburge JV: An unusual occurrence of epidermoid cyst in the buccal
mucosa: A case report with review of literature. J Maxillofac Oral
Surg. 12:90–93. 2013.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Spinardi JR, Goncalves IRD, La Falce TS,
Fregnani JHTG, Barros MD and Macea JR: Benign inclusions in lymph
nodes. Int J Morphol. 25:625–629. 2007.
|
|
10
|
Fellegara G, Carcangiu ML and Rosai J:
Benign epithelial inclusions in axillary lymph nodes: Report of 18
cases and review of the literature. Am J Surg Pathol. 35:1123–1133.
2011.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Bahadur S, Pujani M and Jetley S:
Epithelial inclusion cyst in a cervical lymph node: Report of a
rare entity at an uncommon location. Ann Med Health Sci Res.
6:137–138. 2016.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Abdullah HO, Abdalla BA, Kakamad FH, Ahmed
JO, Baba HO, Hassan MN, Bapir R, Rahim HM, Omar DA, Kakamad SH, et
al: Predatory Publishing Lists: A Review on the Ongoing Battle
Against Fraudulent Actions. Barw Med J. 2:26–30. 2024.
|
|
13
|
Sreeramulu PN, Khan NA, Sreenivasan D and
Gopinath K: Epidermal Cyst in the Breast: A Diagnostic Dilemma.
Indian J Surg Oncol. 8:417–419. 2017.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Mingomataj E, Krasniqi M, Dedushi K,
Sergeevich KA, Kust D and Qadir AA: Cancer Publications in One Year
(2023): A Cross-Sectional Study. Barw Med J. 2:3–11. 2024.
|
|
15
|
Fisher CJ, Hill S and Millis RR: Benign
lymph node inclusions mimicking metastatic carcinoma. J Clin
Pathol. 47:245–247. 1994.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Hunter NB, Rousseau M, Nelson EE and
Rashid RM: The First Report of Multiple, Bilateral Axillary
Epidermal Inclusion Cysts. Cureus. 16(e55640)2024.PubMed/NCBI View Article : Google Scholar
|