Introduction
In total, ~90% of thyroid malignancies are papillary
thyroid carcinomas (PTCs), the most prevalent type of thyroid
carcinoma (1). Tall cell,
follicular and classical variations are the most prevalent types
(2). Several other rare variations
have also been reported, such as those with diffuse sclerosing,
solid, oncocytic, columnar, cribriform, morular, and clear cell
characteristics. Tall cell, follicular, diffuse sclerosing, solid,
and columnar cell variants have a poorer prognosis than other
variants (3,4).
The Warthin-like variant of PTC (WLPTC), considered
a subtype of the oncocytic variant of PTC, is a rare subtype of
papillary carcinoma constituting ~0.2-1.9% of all cases (5). Since this subtype was initially
identified in 1995, <200 instances of WLPTC have been documented
in the English literature (6).
WLPTC resembles a Warthin tumor of the salivary gland.
Histologically, the tumor demonstrates the presence of papillae
lined by oncocytic cells with typical nuclear features of PTC and
has prominent lymphocytic stroma in fibrovascular cores (7). Immunohistochemically, the BRAFV600
mutation was revealed in 75% of WLPTC, which is a mutation that
plays a role in the pathogenesis of classical PTC. Other
immunohistochemical markers detected in WLPTC are HBME-1,
Galectin-3, Cyclin D1 and Cytokeratin 19 (CK19); however, these
markers do not play a significant role in differential pathological
diagnosis (8). The prognosis,
clinical findings and demographic parameters are comparable with
those of classical papillary carcinoma. In contrast to the
classical variant, WLPTC usually manifests at a younger age and has
a higher female prevalence (9,10).
The present case report aims to raise awareness about the
clinicopathologic features of WLPTC.
Case presentation
A 40-year-old female patient was presented to the
outpatient clinic with complaints of fatigue and facial swelling.
The patient had a history of three thyroid carcinomas in
second-degree relatives. The laboratory results revealed
subclinical hypothyroidism [TSH: 7.8 mIU/l (range: 0.34-5.6 mIU/l),
FT3: 3.31 ng/dl (range: 2.6-4.37 ng/dl) and FT4: 0.7 ng/dl (range:
0.61-1.12 ng/dl)] with elevated levels of anti-thyroid peroxidase
antibody [Anti-TPO: 816 IU/ml (range: 0-34 IU/ml)]. Neck
ultrasonography (USG) revealed thyroiditis and multiple nodules
with microcalcifications. The largest nodules were a 6x4 mm
isoechoic-heterogeneous nodule in the right lobe and a 15x7 mm
hypoechoic nodule in the left lobe. The evaluation of the bilateral
central and lateral compartments revealed no pathological lymph
nodes. A fine-needle aspiration (FNA) biopsy was performed for
moderately suspicious nodule features. Histopathological assessment
revealed an atypia of undetermined significance (AUS) for the left
lobe nodule, and benign cytological findings were reported for the
right lobe nodule. In addition to the patient's history and
findings, total thyroidectomy was recommended on the basis of
patient preference. The patient underwent total thyroidectomy, and
she was discharged on postoperative day one with no postoperative
complications. Prophylactic central lymph node dissection was not
performed because no pathological lymph node was detected on
preoperative USG.
The thyroidectomy sample was first examined
macroscopically. Three nodules were found in the inferior pole of
the left thyroid lobe, and they were measured at 9, 3 and 5 mm.
Another 3-mm nodule was described in the superior pole of the left
lobe. A 6x4 mm nodule was described in the inferior pole of the
right lobe. Histopathological assessment of the left lobe revealed
three multifocal papillary microcarcinoma lesions, two non-invasive
follicular tumor papillary-like lesions, and a follicular adenoma.
The 6x4-mm nodule in the right lobe was also identified as a
papillary microcarcinoma. This lesion was reported as a
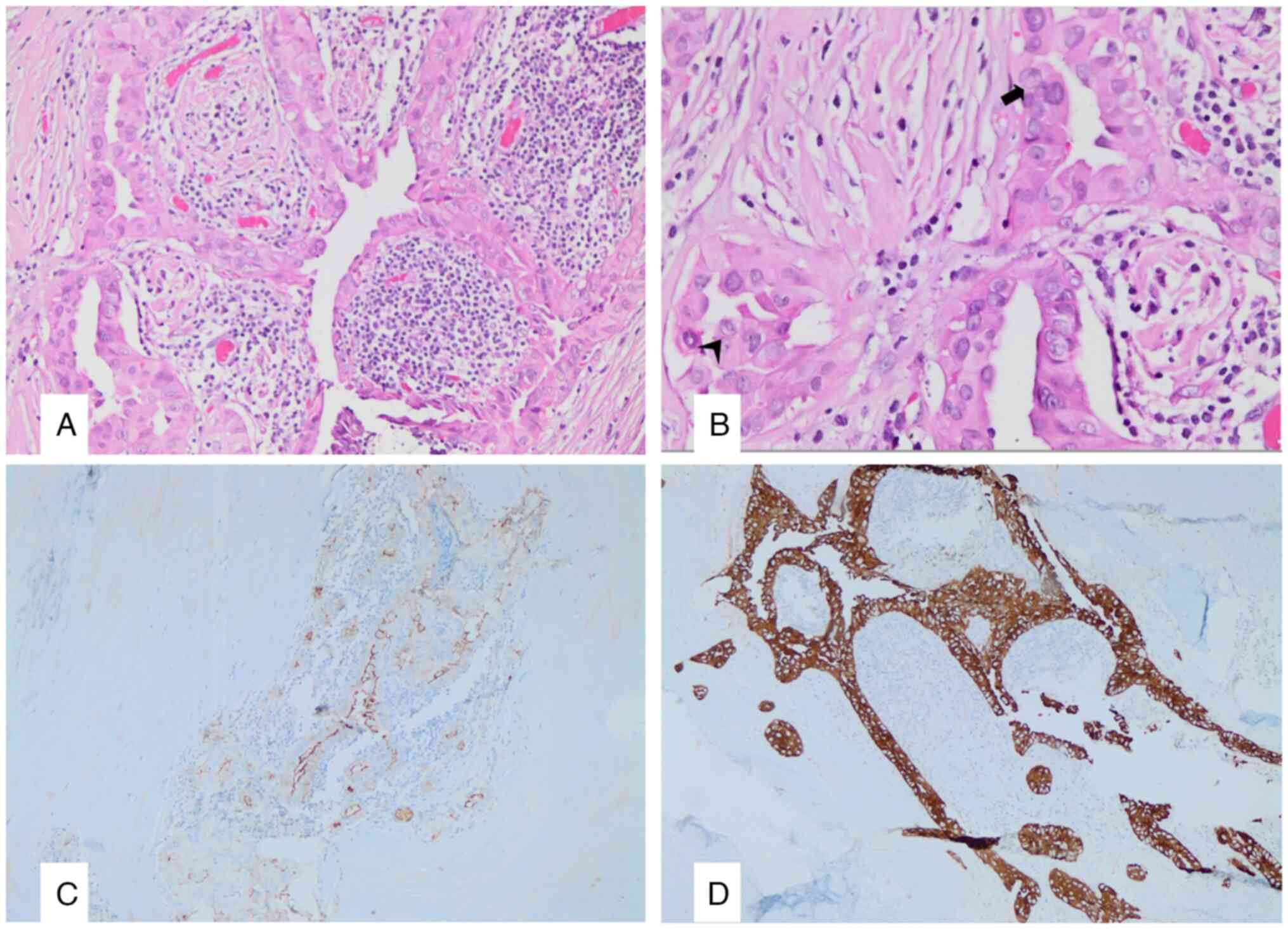
warthin-like subtype of papillary carcinoma (Fig. 1A-D), whereas the papillary
microcarcinoma foci in the left lobe were reported as an invasive
subtype of follicular-type papillary microcarcinoma.
The thyroidectomy specimen was sampled after 18 h of
fixation in 10% buffered formaldehyde solution at room temperature
(25˚C). Following tissue processing overnight, formalin-fixed
paraffin-embedded (FFPE) tissue blocks were prepared. Tissue
sections of 2 µm thickness prepared from FFPE blocks were taken
onto positively charged slides. All stages, including
deparaffinization and antigen retrieval processes, were performed
in Ventana Benchmark Ultra. As a secondary antibody, a detection
kit was used, containing non-biotin horseradish peroxidase,
hydrogen peroxide substrate, and 3,3'-diaminobenzidine
tetra-hydroxy-chloride (DAB) chromogen (UltraView Universal DAB
Detection Kit; Roche Tissue Diagnostics). Mayer's haematoxylin and
bluing reagent were used for counterstaining. Detailed information
about the antibodies used during immunohistochemistry is included
in Table I. Microscopic evaluation
was performed at x4, x100 and x400 magnifications.
 | Table IAntibodies used during
immunohistochemistry. |
Table I
Antibodies used during
immunohistochemistry.
| Antibody | Supplier | Clone or cat.
no. | Dilution | Incubation
period | Temperature |
|---|
| CK19 | Thermo Fisher
Scientific, Inc. | A53-B/A2.26 | 1/100 | 32 min | 56 |
| HBME-1 | Thermo Fisher
Scientific, Inc. | HBME-1 | 1/50 | 60 min | 56 |
| Galectin-3 | Biocare Medical,
LLC | Monoclonal | 1/100 | 32 min | 56 |
| Ki-67 | Roche Tissue
Diagnostics | 30-9 | Ready-to-use | 36 min | 56 |
In immunohistochemistry, this lesion was HMBE-1,
Cytokeratin-19 and Galectin-3 positive, and the Ki-67 proliferation
index was 2%. BRAF mutation was not studied. Capsule invasion was
detected in one tumor focused in the right lobe and one in the left
lobe. There were no signs of angioinvasion or lymphatic invasion.
The thyroid tissue was compatible with Hashimoto's thyroiditis.
According to the AJCC 8th edition, the pathological
stage was determined to be pT1a-Stage 1(11). Surveillance was recommended on the
basis of the patient's clinical and pathological findings. The
patient remained disease-free 8 months after surgery.
Discussion
WLPTC is a rare oncocytic variant of PTC. Its
demographic and clinical features resemble those of other
differentiated thyroid carcinomas, especially classic PTC, which
coexist with Hashimoto's thyroiditis. Similar to classic PTC, WLPTC
affects women more commonly than men, and the most frequently
affected age group is 30-50 years-old. Patients usually present
with a painless mass in the neck (9,10,12,13).
USG of the neck usually reveals a solid, hypoechoic nodule with
heterogeneous parenchyma in the background. However, it may be
misdiagnosed as a benign nodule or focal thyroiditis with USG
(14).
There are no specific clinical or radiological
findings for diagnosing WLPTC; FNA biopsy may also result in
inconclusive findings. Histopathological assessment of the
thyroidectomy material is crucial for a definitive diagnosis
(7). The differential diagnosis of
WLPTC includes Hashimoto's thyroiditis, Hurthle cell neoplasm,
classical PTC arising in a thyroiditis background, tall cell
variant, and the oxyphilic variant of PTC. Differential diagnosis
is crucial, as some mimickers have more aggressive and unfavourable
outcomes than WLPTC does. WLPTC rarely exhibits lymph node
metastasis and extrathyroidal extension, thus demonstrating a low
recurrence rate and a favourable outcome (9,12,13).
In the present case, the patient, who was a
40-year-old female, did not have a palpable mass on her neck and
her only symptom was fatigue. A nodule that was eventually
diagnosed as WLPTC was defined as a 6x4 mm isoechoic-heterogeneous
nodule with microcalcifications on neck USG. USG also revealed
coexisting thyroiditis, which is considered to be a common feature
among patients with WLPTC. The FNA biopsy of the nodule revealed
benign cytological findings. Immunohistochemical studies were not
performed in FNA biopsy material.
Total thyroidectomy was recommended for patients
with multiple thyroid nodules with microcalcifications, one of whom
had been diagnosed with AUS, and a positive family history of
thyroid carcinoma. Left hemithyroidectomy or immunohistochemical
studies could have been performed as the patient's FNA biopsy
revealed AUS only for the left lobe nodule. In this case, WLPTC in
the right lobe would not have been diagnosed, and this could have
led to a delay in treatment, also requiring a second surgery with a
higher risk of complications. Another option would be a second FNA
biopsy of the right lobe nodule, due to the incompatibility of
pathological and radiological findings. This also could have
resulted in a false negative and caused a delay in treatment. In
the present case, family history of thyroid carcinoma,
ultrasonographic image of microcalcifications and the patient's
preference have led to total thyroidectomy without another FNA
biopsy.
Even though there were no malignant findings in the
cytological assessment, the definitive pathological assessment
revealed four lesions of invasive thyroid carcinoma. The present
case was unique in that three other foci of papillary
microcarcinoma and a follicular adenoma coexisted with WLPTC.
In the present case, WLPTC could not have been
diagnosed by FNA biopsy assessment before surgery; the right lobe
nodule was misdiagnosed as benign with FNA biopsy and cytological
evaluation. Moreover, neck USG did not reveal strong malignant
features other than microcalcifications. This finding may support
the idea that radiology and FNA biopsy alone are insufficient for
the differential diagnosis of WLPTC.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
All listed authors meet the ICMJE criteria. The
authors attest that all authors contributed significantly to the
creation of the present study, each having fulfilled criteria as
established by the ICMJE. SA, BD and ME conceptualized the present
study. SA, BD, MHT, NA and ME performed the methodology. SA, BD,
MHT, NA and ME investigated and analyzed the data. SA, BD, MHT, NA
and ME wrote and prepared the original draft of the manuscript. SA,
BD, MHT, NA and ME wrote reviewed and edtited the te manuscript.
SA, BD, ME acquired the funds and obtained the resources. ME
supervised the present study. All authors read and approved the
final version of the manuscript. Data authentication is not
applicable.
Ethics approval and consent to
participate
All procedures that were performed were in
accordance with the ethical standards of the responsible committee
on human experimentation (institutional and national) and with the
Helsinki Declaration of 1975, as revised in 2008. Patient consent
for participation was obtained.
Patient consent for publication
Written informed consent to publish potentially
identifying information, such as details of the case and associated
images, was obtained from the patient.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Kitahara CM and Schneider AB: Epidemiology
of thyroid cancer. Cancer Epidemiol Biomarkers Prev. 31:1284–1297.
2022.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Lloyd RV, Buehler D and Khanafshar E:
Papillary thyroid carcinoma variants. Head Neck Pathol. 5:51–56.
2011.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Coca-Pelaz A, Shah JP, Hernandez-Prera JC,
Ghossein RA, Rodrigo JP, Hartl DM, Olsen KD, Shaha AR, Zafereo M,
Suarez C, et al: Papillary thyroid cancer-aggressive variants and
impact on management: A narrative review. Adv Ther. 37:3112–3128.
2020.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Hu J, Wang F, Xue W and Jiang Y: Papillary
thyroid carcinoma with nodular fasciitis-like stroma-an unusual
variant with distinctive histopathology: A case report. World J
Clin Cases. 11:5797–5803. 2023.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Hu D and Wang L: Warthin-like variant of
papillary thyroid carcinoma: A new entity. Asian J Surg.
45:2592–2593. 2022.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Wajahat M, Jeelani T, Gupta K and Bashir
N: Warthin like papillary carcinoma-A rare variant of papillary
carcinoma thyroid. Hum Pathol Case Rep. 13:21–23. 2018.
|
|
7
|
Erşen A, Durak MG, Canda T, Sevinc AI,
Saydam S and Koçdor MA: Warthin-like papillary carcinoma of the
thyroid: A case series and review of the literature. Turk Patoloji
Derg. 29:150–155. 2013.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Fonseca D, Arya SS, Lahari GG and Rao C:
Warthin like variant of papillary carcinoma thyroid with BRAF
mutation. Indian J Otolaryngol Head Neck Surg. 74 (Suppl
3):S6213–S6215. 2022.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Paliogiannis P, Attene F, Trogu F and
Trignano M: Warthin-like papillary carcinoma of the thyroid gland:
Case report and review of the literature. Case Rep Oncol Med.
2012(689291)2012.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Lam KY, Lo CY and Wei WI: Warthin
tumor-like variant of papillary thyroid carcinoma: A case with
dedifferentiation (anaplastic changes) and aggressive biological
behavior. Endocr Pathol. 16:83–89. 2005.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Tuttle RM, Haugen B and Perrier ND:
Updated American joint committee on cancer/tumor-node-metastasis
staging system for differentiated and anaplastic thyroid cancer
(eighth edition): What changed and why? Thyroid. 27:751–756.
2017.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Kumar T, Nigam JS, Tewari P and Jha CK:
Warthin-like variant of papillary thyroid carcinoma: An uncommon
variant. Cureus. 12(e12350)2020.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Missaoui AM, Hamza F, Belabed W, Mellouli
M, Maaloul M, Charfi S, Jardak I, Sellami-Boudawara T, Rekik N and
Abid M: Warthin-like papillary thyroid carcinoma: A case report and
comprehensive review of the literature. Front Endocrinol
(Lausanne). 14(1210943)2023.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Kim GR, Shin JH, Hahn SY, Ko EY and Oh YL:
Ultrasonographic features and clinical characteristics of
warthin-like variant of papillary thyroid carcinoma. Endocr J.
63:329–335. 2016.PubMed/NCBI View Article : Google Scholar
|