Introduction
Esophageal cancer is one of the most important
cancer types in the gastrointestinal tract. It is more prevalent in
the Asian continent, including Thailand (1,2).
Unfortunately, the majority of patients with esophageal cancer are
asymptomatic in the early stages and the diagnosis is often made at
an advanced stage. This leads to a poor prognosis, notably in
patients with malnutrition, who have a lower survival rate
(3,4). Esophageal cancer can cause metabolic
changes that lead to anoxia and cachexia, in addition to worsening
dysphagia (5-7).
Nutrition plays a crucial role in any type of treatment and
staging, particularly for esophageal cancer. Therefore, it is even
more essential to pay attention to nutrition when dealing with this
type of cancer (3,7,8).
Enteral nutrition is the preferred method of
providing nutrition for patients who can consume food orally or
through a feeding tube (3,7-12).
In cases of T4b esophageal cancer, feeding is done by passing food
through the narrowed esophagus caused by the cancer. There are two
main methods for delivering the food: Prepyloric (or gastric) and
postpyloric (or jejunum). The prepyloric methods currently in use
include nasogastric tube feeding, percutaneous endoscopic
gastrostomy (PEG), surgical gastrostomy and esophageal stent.
However, there is a lack of comparison between the effectiveness of
each method. Different factors can be used to monitor nutritional
status, which may vary depending on the type of cancer. For
instance, weight plays a crucial role in tracking nutritional
status in patients with esophageal cancer (9). Monitoring weight changes is a
straightforward and non-invasive approach that can be employed in
clinical settings. The aim of the present study was to compare
various enteral nutrition techniques and assess the efficacy of
weight changes in patients who have advanced esophageal cancer.
Materials and methods
Study design and patients
A study was conducted retrospectively on patients
who were referred to the Department of Surgery at Thammasat
University Hospital in Pathum Thani, Thailand, for esophageal
cancer treatment between January 2012 and December 2022. The
patients were treated in accordance with the guidelines set by the
National Comprehensive Cancer Network (13) and the Japan Esophageal Society
(14,15). The present study included patients
aged 18 years or older with stage T4b esophageal cancer and
squamous cell carcinoma confirmed by pathology. All enrolled
patients received enteral nutrition via methods such as nasogastric
tube (NG), esophageal stent, PEG, or open gastrostomy (OG).
Patients were excluded if they had no treatment plan due to
impending death, or if their Eastern Cooperative Oncology Group
Performance Status Score was ≥4. Patients who received parenteral
nutrition, had other causes of malnutrition, or altered their
enteral method were also excluded from the study. The institutional
ethics review committees approved the study. The following
reference number was provided by the institutional review board and
the Human Ethics Committee of Thammasat University (Faculty of
Medicine): MTU-EC-SU-0-262/65.
Data collection
The present study included the collection of various
data including baseline characteristics, comorbidities, body mass
index (BMI), route of enteral nutrition, tolerable enteral
nutrition, total calories per day and mode of treatment.
Malnutrition was defined as having a BMI <18.5 kg/m2
or unintentional weight loss exceeding 10% at any time or exceeding
5% over the last 3 months combined with either a BMI <20
kg/m2 if the patient was <70 years of age or <22
kg/m2 if the patient was 70 years of age or older, based
on the European Society for Clinical Nutrition and Metabolism
guidelines. The present study recorded the patient's body weight at
0-, 1-, 3- and 6-month follow-up visits. In addition, the one-year
survival data were also collected.
Statistical analysis
The statistical analysis of data is presented as the
mean ± standard error of the mean. The analysis was carried out
using various statistical tests such as the χ2 test for
categorical data, and unpaired t-test and one-way ANOVA for
continuous data. The analysis was carried out using Fisher's exact
test if >20% of the expected counts in the cells of the analyzed
contingency table were 5 or fewer. The Bonferroni multiple
comparison test was performed in the event of a significant result
according to one-way ANOVA. Bonferroni correction was applied after
Fisher's exact tests and χ2 tests for multiple
comparisons. The weight changes of all four groups were assessed at
1-, 3- and 6-month follow-up periods using the Kruskal-Wallis test
for non-parametric continuous data and Dunn's pairwise comparison
between two groups. The data were analyzed using Stata/MP 18.0 for
Mac (StataCorp LP). A P<0.05 was considered to indicate a
significant difference.
Results
Out of 192 patients with esophageal cancer who were
screened, only 58 were enrolled in the present study. Among the
enrolled patients, 11 (18.97%) received enteral nutrition through
the NG route, 4 (6.9%) received an esophageal stent with an oral
route, 18 (31.03%) received OG, and 25 (43.1%) received PEG.
Table I provides the baseline
characteristics of patients with advanced esophageal cancer. On
average, the patients were 61.85 years old and 86.21% of them were
male. The patients had similar tolerable enteral nutrition and
total calorie intake per day. All patients, except for those in the
esophageal stent group who received chemotherapy, underwent
chemoradiation. Following the improvement in their enteral
nutrition status, the one-year survival rate of these patients was
55.17%.
 | Table ICharacteristics of patients with
advanced esophageal cancer receiving enteral nutrition methods,
including nasogastric tube, esophageal stent, open gastrostomy and
percutaneous endoscopic gastrostomy. |
Table I
Characteristics of patients with
advanced esophageal cancer receiving enteral nutrition methods,
including nasogastric tube, esophageal stent, open gastrostomy and
percutaneous endoscopic gastrostomy.
| | Enteral nutrition
methods | |
|---|
| Characteristics | NG (n=11) | ES (n=4) | OG (n=18) | PEG (n=25) | P-value |
|---|
| Mean age ± SD,
years | 60.64±5.54 | 61.00±6.22 | 61.94±11.66 | 62.44±10.76 | 0.083a |
| Sex, n (%) | | | | | 0.697 |
|
Male | 9 (81.82) | 3 (75.00) | 16 (88.89) | 22 (88.00) | |
|
Female | 2 (18.18) | 1 (25.00) | 2 (11.11) | 3 (12.00) | |
| Comorbidities, n
(%) | | | | | |
|
Hypertension | 2 (18.18) | 1 (25.00) | 4 (22.22) | 9 (36.00) | 0.586 |
|
Diabetes | 1 (9.09) | 0 (0.00) | 2 (11.11) | 6 (24.00) | 0.235 |
|
Dyslipidemia | 1 (9.09) | 0 (0.00) | 2 (11.11) | 6 (24.00) | 0.235 |
|
Coronary
artery disease | 1 (9.09) | 0 (0.00) | 0 (0.00) | 0 (0.00) | 0.259 |
|
Atrial
fibrillation | 1 (9.09) | 0 (0.00) | 0 (0.00) | 0 (0.00) | 0.259 |
|
Tuberculosis | 3 (27.27) | 1 (25.00) | 3 (16.67) | 3 (12.00) | 0.599 |
|
Chronic
obstructive | 1 (9.09) | 1 (25.00) | 0 (0) | 8 (32.00) | 0.041; |
|
pulmonary
disease | | | | |
>0.999b;
>0.999c;
>0.999d;
>0.999e;
>0.999f;
>0.999g |
|
Cirrhosis | 0 (0.00) | 0 (0.00) | 2 (11.11) | 0 (0.00) | 0.260 |
|
Chronic
kidney disease | 0 (0.00) | 0 (0.00) | 2 (11.11) | 0 (0.00) | 0.260 |
|
Head and
neck cancer | 1 (9.09) | 0 (0.00) | 1 (5.56) | 1 (4.00) | 0.825 |
|
Other | 0 (0.00) | 1 (25.00) | 1 (5.56) | 0 (0.00) | 0.107 |
| Mean weight 1 year
before diagnosis ± SD, kg | 54.45±5.52 | 58.75±5.44 | 56.06±8.84 | 59.96±6.79 | 0.361a |
| Mean weight before
enteral nutrition methods ± SD, kg | 42.31±5.24 | 44.75±6.65 | 40.07±7.76 | 43.99±3.77 | 0.018a; >0.999b; >0.999c; >0.999d; 0.872e; >0.999f; 0.186g |
| Weight loss, % | 22.34±5.41 | 23.85±8.00 | 28.88±6.21 | 23.23±7.83 | 0.529a |
| Mean height ± SD,
cm | 161.27±4.36 | 163.25±5.38 | 163.17±4.30 | 164.08±8.94 | 0.730a |
| Mean BMI ± SD,
kg/m2 | 16.28±2.05 | 16.74±1.69 | 15.01±2.52 | 17.12±1.78 | 0.469a |
| Mean tolerable
enteral nutrition total calories per day ± SD, calorie |
1,654.55±249.45 |
1,472.50±166.41 |
1,757.78±540.89 |
1,760.04±299.53 | 0.006a; >0.999b; >0.999c; >0.999d; >0.999e; >0.999f; >0.999g |
| Mean albumin ± SD,
g/dl | 2.96±0.28 | 2.85±0.19 | 2.79±0.61 | 2.99±0.36 | 0.011a; >0.999b; >0.999c; >0.999d; >0.999e; >0.999f; 0.784g |
| Treatment, n
(%) | | | | | |
|
Radiation | 0 (0.00) | 0 (0.00) | 2 (11.11) | 1 (4.00) | 0.665 |
|
Chemoradiation | 9 (81.82) | 0 (0.00) | 13 (72.22) | 22 (88.00) | 0.002;
0.003b;
>0.999c;
>0.999d;
0.007e;
<0.001f;
>0.999g |
|
Chemotherapy | 2 (18.18) | 4 (100.00) | 3 (16.67) | 2 (8.00) | <0.001;
0.001b;
>0.999c;
>0.999d;
<0.001e;
<0.001f;
>0.999g |
| 1-year survival, n
(%) | 6 (54.55) | 2 (50.00) | 9 (50.00) | 15 (60.00) | 0.924 |
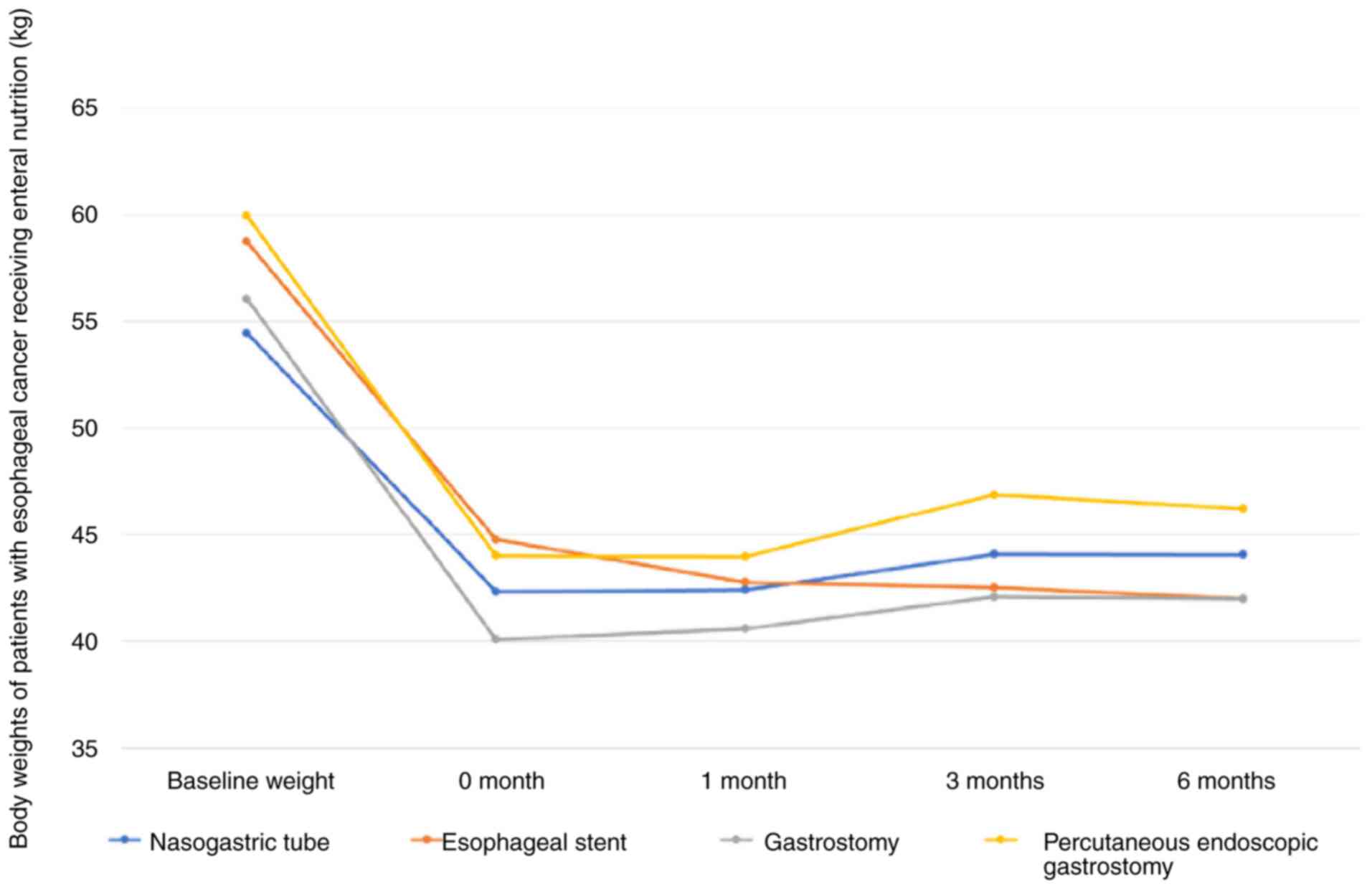
During the study, each patient's weight was
monitored at the beginning and subsequently at 1-, 3-, and 6-month
follow-up periods. All patients were monitored for 6 months.
Fig. 1 illustrates the trend of
their body weight throughout the study. Prior to receiving enteral
nutrition, the average weight of all patients one year before
diagnosis was 57.62±7.41 kg; this value was altered to 42.51.5±8.56
kg. Following administration of enteral nutrition, the average body
weight was 42.52±6.16 kg in the 1st month, which was improved to
44.55±6.61 kg in the 3rd month and reached a plateau at ~44.21±6.13
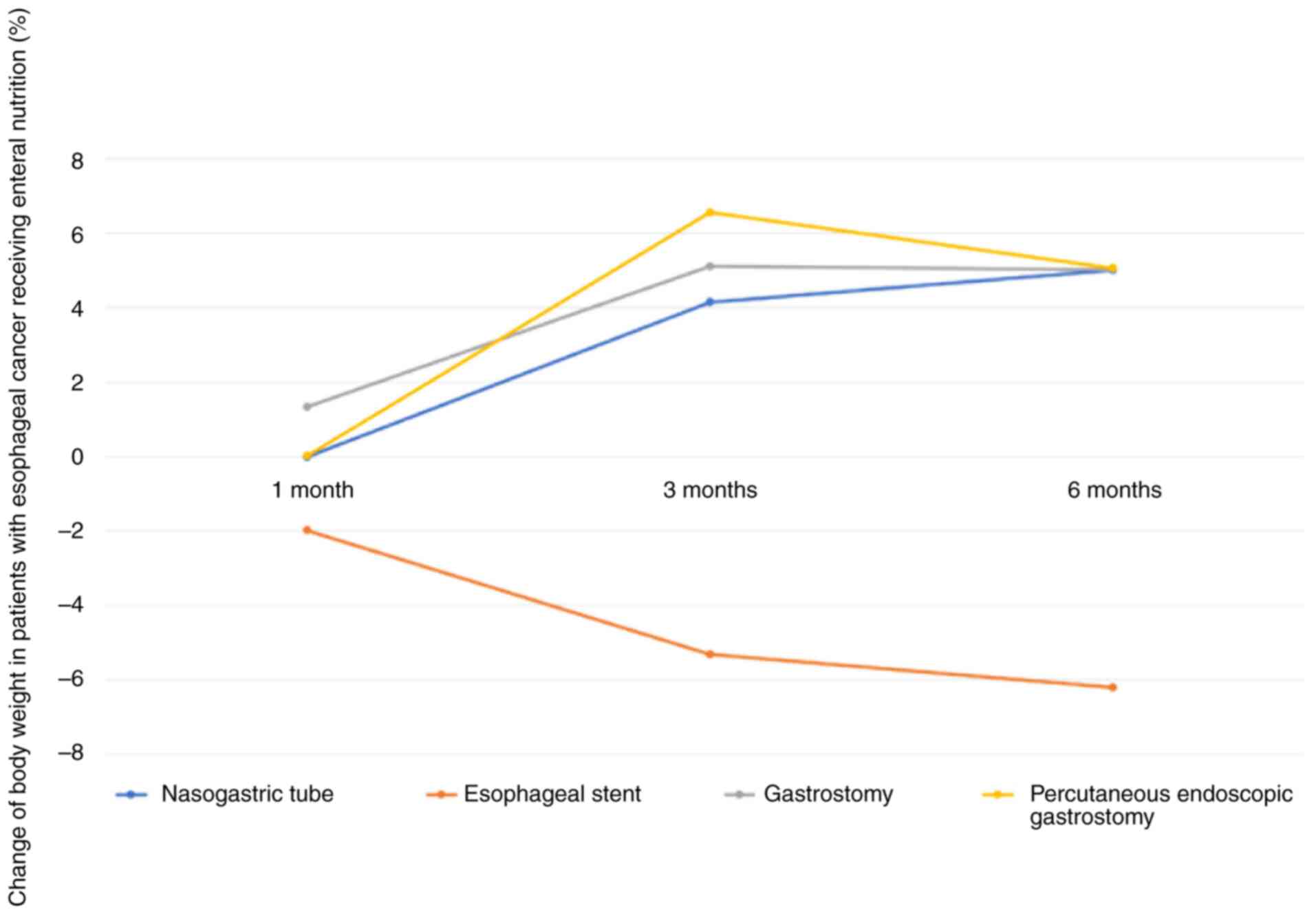
kg in the 6th month. Fig. 2
demonstrated the percentage change in body weight in patients with
esophageal cancer who received enteral nutrition via each method.
The weight change of patients with advanced esophageal cancer who
received enteral nutrition at the 3-month follow-up period
indicated significant weight improvement in the NG tube, OG and PEG
group compared with that of the esophageal stent group (P=0.027,
P=0.009 and P=0.001, respectively). No significant difference was
noted between the NG tube, OG and PEG methods. There were
statistically significant differences in the mean weight change
between the NG and OG methods as well as OG and ES methods at the
1-month follow-up (P=0.044 and P=0.047, respectively). At the
6-month follow-up, ES methods demonstrated statistically
significant difference compared with the NG, OG and PEG methods
(P=0.023, P=0.024 and P=0.010, respectively). Table II provides information on detailed
comparisons.
 | Table IIWeight changes of patients with
advanced esophageal cancer receiving enteral nutrition methods,
including NG, esophageal stent, OG and PEG, at the 1-, 3- and
6-month follow-ups. |
Table II
Weight changes of patients with
advanced esophageal cancer receiving enteral nutrition methods,
including NG, esophageal stent, OG and PEG, at the 1-, 3- and
6-month follow-ups.
| | 1-month
follow-up | 3-month
follow-up | 6-month
follow-up |
|---|
| | | P-value
(P=0.404a) | | P-value
(P=0.020a,b) | | P-value
(P=0.146a) |
|---|
| Enteral nutrition
methods | Mean weight change
± SD, kg | NG vs. | ES vs. | OG vs. | Mean weight change
± SD, kg | NG vs. | ES vs. | OG vs. | Mean weight change
± SD, kg | NG vs. | ES vs. | OG vs. |
|---|
| NG | 0.08±2.82 | | | | 1.76±2.88 | | | | 1.73±5.47 | | | |
| ES | -2.00±2.58 | 0.067 | | | -2.25±2.6 | 0.027b | | | -2.50±3.70 | 0.023b | | |
| OG | 0.49±2.51 | 0.044b | 0.047b | | 1.99±2.36 | 0.326 | 0.009b | | 19.00±1.12 | 0.420 | 0.024b | |
| PEG | -0.06±1.36 | 0.378 | 0.079 | 0.296 | 2.88±2.05 | 0.078 | 0.001b | 0.136 | 2.22±2.06 | 0.414 | 0.010b | 0.307 |
Discussion
Dysphagia, or difficulty in swallowing, is a
significant symptom that affects both swallowing function and
nutrition. It can be indicative of conditions such as esophageal
cancer or external pressure on the esophagus, such as from enlarged
lymph nodes (13). Advanced
esophageal cancer is a significant healthcare issue noted
worldwide, particularly in developing countries, such as Thailand
(1,2). In the institution in which the
present study was performed, a previous study demonstrated that
53.8% of patients exhibited stage 4 cancer (4). Tumors can severely impact swallowing
and cause dysphagia, particularly in cases of T4 staging. The
systemic effects of cancer can also lead to malnutrition, causing
further health deterioration and distress for patients. Patients
with T4b esophageal cancer often have large mass effects that
affect oral intake and have invaded vital nearby organs; in this
clinical status, surgery is not recommended (14-16).
Therefore, it was decided that research should be conducted on this
group of patients with esophageal cancer.
It is crucial to take into account various factors
related to the nutritional status of patients with advanced
esophageal cancer, notably their weight, in order to ensure their
quality of life, regardless of the treatment method used (8,9,17-21).
Weighing of the patients is a simple and effective method that can
be easily implemented in clinical practice. Even if the patients
are unable to stand, their weight can still be measured using
specialized weight machines or by subtracting the weight of their
wheelchair using wheelchair scales. In addition, blood chemistry
values can also be employed to determine the patient's nutritional
status; however, this is an invasive method that may not be
comfortable for the patient.
Nutritional support for patients with advanced
esophageal cancer requires consideration of various factors,
including indications, suitability based on disease staging and
cost. There is no one-size-fits-all approach, as each method has
its own advantages and disadvantages that must be evaluated on a
case-by-case basis. It is important to note that all enteral
nutrition methods are classified based on feeding sites in the
stomach or prepyloric feeding route. One such method is the NG
tube, which involves the use of a pediatric endoscopy with a small
diameter and guidewire to pass through the narrowing of the
esophageal lumen caused by cancer. While this method is relatively
inexpensive, patients may find it uncomfortable to have a nasal
tube in their nose and throat and it may impact their self-image
from the perception of others (22). An additional method is the
esophageal stent, which allows for oral intake without the
requirement for tubes or wounds from the procedure. However, this
method requires a technical skill and may be more expensive
compared with other methods (23,24).
Surgical gastrostomy is a feeding technique that has
been in use for a long time. It involves making an opening in the
stomach through surgery. However, this procedure carries the risk
of complications and abdominal wounds. An innovative method called
PEG uses an endoscope to insert the feeding tube. This technique
has been developed to minimize the disadvantages associated with
surgical gastrostomy. PEG causes lower number of complications and
reduced pain and results in a shorter hospital stay. A special
technique of PEG has been developed called the push technique,
which is used for patients with esophageal cancer. This technique
has no risk of cancer seeding to the stroma of the gastrostomy
site. All of the patients in the present study were treated by this
technique. However, the success of PEG depends on technical
practices and experiences, as well as the cost of PEG kits. In
addition, if the endoscope is unable to pass through the mass and
luminal narrowing in the stomach, an open gastrostomy is still
required in such cases. Ultimately, the selection of the method
should be based on the individual disease and patient factors
and/or circumstances of each disease status (11,12).
According to the findings of the present study, the
majority of the participants exhibited malnourished status. In
patients with advanced esophageal cancer, enteral nutrition
exhibited a modest impact on body weight during the initial month
of the study. However, it indicated an inclination towards
enhancing body weight in the first 3 months following treatment,
and the improvement persisted for the subsequent 6 months of
follow-up.
No significant difference was noted in the body
weight change between the NG, OG and PEG methods. However, when
analyzed with an esophageal stent, three of these methods
demonstrated significant improvement in weight. One possible reason
for this difference is that all patients in the stent group were
treated with chemotherapy, whereas patients who were treated with
other enteral nutrition methods mostly received chemoradiation. The
present study relates to a previous publication, which indicates
that stents did not prevent weight loss or malnutrition (25,26).
By contrast, certain studies have determined that esophageal stents
could relieve dysphagia and maintain the nutritional status
(27,28). Moreover, the number of stents was
very small and further studies in the future will probably provide
better answers and evidence on this point. Furthermore, the
one-year survival in these patients with enteral nutritional
support was 55.17%; in the present study, the range was between
29-76% compared with the one-year overall survival noted in the
previous reports (29).
The study's limitation was that it was a
single-center and retrospective analysis. The study's conclusion
revealed that enteral nutrition can support weight improvement in
patients with advanced esophageal cancer. Methods, such as NG,
gastrostomy and PEG feeding tubes have been proven to be safe and
effective options.
In our study, a trend of weight improvement was
observed within 3 months of initiating nutritional support with
weight maintenance noted at the 6-month follow-up. Further research
is required with multi-center, randomization and blinding
protocols, as well as larger population numbers, to confirm the
definitive evidence of enteral nutritional options and their
effectiveness in treating patients with advanced esophageal
cancer.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
PM and BC confirm the authenticity of all the raw
data. PM and BC contributed to data analysis, drafting and revising
the article, have agreed on the journal to which the article was
submitted, and agree to be accountable for all aspects of the work.
Both authors have read and approved the final manuscript.
Ethics approval and consent to
participate
The institutional ethics review committees approved
the study before participation, and it passed the institutional
review board and the ethical research process of the Human Ethics
Committee of Thammasat University, Amphur Klongluang, Pathum Thani,
Thailand (Faculty of Medicine; approval no. MTU-EC-SU-0-262/65).
The requirement for informed consent from all patients included in
the present study was waived due to the retrospective design.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Morgan E, Soerjomataram I, Rumgay H,
Coleman HG, Thrift AP, Vignat J, Laversanne M, Ferlay J and Arnold
M: The global landscape of esophageal squamous cell carcinoma and
esophageal adenocarcinoma incidence and mortality in 2020 and
projections to 2040: New estimates from GLOBOCAN 2020.
Gastroenterology. 163:649–658. 2022.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Zhu H, Wang Z, Deng B, Mo M, Wang H, Chen
K, Wu H, Ye T, Wang B, Ai D, et al: Epidemiological landscape of
esophageal cancer in Asia: Results from GLOBOCAN 2020. Thorac
Cancer. 14:992–1003. 2023.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Sunpaweravong S, Benjhawaleemas P,
Karnjanawanichkul O, Yolsuriyanwong K, Ruangsin S, Laohawiriyakamol
S and Chaipetch O: Randomized controlled trial of intravenous
sedation vs general anesthesia for esophageal dilation with
percutaneous endoscopic gastrostomy in esophageal cancer patients.
Surg Endosc. 37:5109–5113. 2023.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Nun-Anan P and Vilaichone RK: Late stage
and grave prognosis of esophageal cancer in Thailand. Asian Pac J
Cancer Prev. 16:1747–1749. 2015.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Ispoglou T, McCullough D, Windle A, Nair
S, Cox N, White H, Burke D, Kanatas A and Prokopidis K: Addressing
cancer anorexia-cachexia in older patients: Potential therapeutic
strategies and molecular pathways. Clin Nutr. 43:552–566.
2024.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Garutti M, Noto C, Pastò B, Cucciniello L,
Alajmo M, Casirati A, Pedrazzoli P, Caccialanza R and Puglisi F:
Nutritional management of oncological symptoms: A comprehensive
review. Nutrients. 15(5068)2023.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Li Y, Pond G, Van Osch A, Reed R, Ung Y,
Cheng S, Menjak I, Doherty M, Moglica E and Taggar AS: Enhancing
nutrition support for esophageal cancer patients: Understanding
factors influencing feeding tube utilization. Nutr Cancer.
76:271–278. 2024.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Akagündüz DD and Türker PF: Nutritional
support in older patients with esophageal cancer undergoing
chemoradiotherapy. Nutr Cancer. 74:3634–3639. 2022.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Salas S, Cottet V, Dossus L, Fassier P,
Ginhac J, Latino-Martel P, Romieu I, Schneider S, Srour B,
Touillaud M, et al: Nutritional Factors during and after cancer:
Impacts on survival and quality of life. Nutrients.
14(2958)2022.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Muscaritoli M, Arends J, Bachmann P,
Baracos V, Barthelemy N, Bertz H, Bozzetti F, Hütterer E, Isenring
E, Kaasa S, et al: ESPEN practical guideline: Clinical nutrition in
cancer. Clin Nutr. 40:2898–2913. 2021.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Mahawongkajit P, Techagumpuch A,
Limpavitayaporn P, Kanlerd A, Sriussadaporn E, Juntong J, Tongyoo A
and Mingmalairak C: Comparison of introducer percutaneous
endoscopic gastrostomy with open gastrostomy in advanced esophageal
cancer patients. Dysphagia. 35:117–120. 2020.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Mahawongkajit P and Techagumpuch A:
Gastrostomy in patients with previous abdominal surgery: A
comparative study between the laparoscopy-assisted introducer
percutaneous endoscopic gastrostomy versus open gastrostomy in
advanced esophageal cancer. Dysphagia. 36:67–72. 2021.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Neacşu F, Vârban AŞ, Simion G, Şurghie R,
Pătraşcu OM, Sajin M, Dumitru M and Vrînceanu D: Lung cancer
mimickers-a case series of seven patients and review of the
literature. Rom J Morphol Embryol. 62:697–704. 2021.PubMed/NCBI View Article : Google Scholar
|
|
14
|
National Comprehensive Cancer Network.
NCCN clinical practice guidelines in oncology: Esophageal and
Esophagogastric junction Cancers, version 4[Internet]. Fort
Washington, PA: National Comprehensive Cancer Network; 2023.
https://www.nccn.org/professionals/physician_gls/pdf/esophageal.pdf.
Accessed Jan 2, 2024.
|
|
15
|
Kitagawa Y, Ishihara R, Ishikawa H, Ito Y,
Oyama T, Oyama T, Kato K, Kato H, Kawakubo H, Kawachi H, et al:
Esophageal cancer practice guidelines 2022 edited by the Japan
esophageal society: Part 1. Esophagus. 20:343–372. 2023.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Kitagawa Y, Ishihara R, Ishikawa H, Ito Y,
Oyama T, Oyama T, Kato K, Kato H, Kawakubo H, Kawachi H, et al:
Esophageal cancer practice guidelines 2022 edited by the Japan
esophageal society: Part 2. Esophagus. 20:373–389. 2023.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Cederholm T, Bosaeus I, Barazzoni R, Bauer
J, Van Gossum A, Klek S, Muscaritoli M, Nyulasi I, Ockenga J,
Schneider SM, et al: Diagnostic criteria for malnutrition-An ESPEN
consensus statement. Clin Nutr. 34:335–340. 2015.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Quyen TC, Angkatavanich J, Thuan TV, Xuan
VV, Tuyen LD and Tu DA: Nutrition assessment and its relationship
with performance and Glasgow prognostic scores in Vietnamese
patients with esophageal cancer. Asia Pac J Clin Nutr. 26:49–58.
2017.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Wiwitkeyoonwong J, Jiarpinitnun C,
Hiranyatheb P and Ngamphaiboon N: Impact of weight loss on patients
with locally advanced esophageal and esophagogastric junction
cancers treated with chemoradiotherapy. Asian Pac J Cancer Prev.
22:3847–3855. 2021.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Wang X, Liu X, Gu Z, Li X and Shu Y:
Experiences and requirements in nutritional management of patients
with esophageal cancer: A systematic review and qualitative
meta-synthesis. Support Care Cancer. 31(633)2023.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Ai X, Zhang P, Xie X, Qiu B, Zhu Y, Zhao
L, Xi M, Wu Y, Guo S, Guo J, et al: Efficacy and cost-effectiveness
analysis of pretreatment percutaneous endoscopic gastrostomy in
unresectable locally advanced esophageal cancer patients treated
with concurrent chemoradiotherapy (GASTO 1059). Cancer Med.
12:15000–15010. 2023.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Lin CH, Liu NJ, Lee CS, Tang JH, Wei KL,
Yang C, Sung KF, Cheng CL, Chiu CT and Chen PC: Nasogastric feeding
tube placement in patients with esophageal cancer: Application of
ultrathin transnasal endoscopy. Gastrointest Endosc. 64:104–107.
2006.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Sasso JGRJ, de Moura DTH, Proença IM,
Junior ESDM, Ribeiro IB, Sánchez-Luna SA, Cheng S, Bestetti AM, Kum
AST, Bernardo WM and de Moura EGH: Anti-reflux versus conventional
self-expanding metal stents in the palliation of esophageal cancer:
A systematic review and meta-analysis. Endosc Int Open.
10:E1406–E1416. 2022.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Chandan S, Mohan BP, Khan SR, Bhogal N,
Canakis A, Bilal M, Dhaliwal AS, Aziz M, Mashiana HS, Singh S, et
al: Clinical efficacy and safety of palliative esophageal stenting
without fluoroscopy: A systematic review and meta-analysis. Endosc
Int Open. 8:E944–E952. 2020.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Mão-de-Ferro S, Serrano M, Ferreira S,
Rosa I, Lage P, Alexandre DP, Freire J, Mirones L, Casaca R,
Bettencourt A and Pereira AD: Stents in patients with esophageal
cancer before chemoradiotherapy: High risk of complications and no
impact on the nutritional status. Eur J Clin Nutr. 70:409–410.
2016.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Yu FJ, Shih HY, Wu CY, Chuang YS, Lee JY,
Li HP, Fang PT, Tsai DL, Chou SH and Wu IC: Enteral nutrition and
quality of life in patients undergoing chemoradiotherapy for
esophageal carcinoma: A comparison of nasogastric tube, esophageal
stent, and ostomy tube feeding. Gastrointest Endosc. 88:21–31.
2018.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Siddiqui AA, Glynn C, Loren D and Kowalski
T: Self-expanding plastic esophageal stents versus jejunostomy
tubes for the maintenance of nutrition during neoadjuvant
chemoradiation therapy in patients with esophageal cancer: A
retrospective study. Dis Esophagus. 22:216–222. 2009.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Smith ZL, Gonzaga JE, Haasler GB, Gore EM
and Dua KS: Self-expanding metal stents improve swallowing and
maintain nutrition during neoadjuvant therapy for esophageal
cancer. Dig Dis Sci. 62:1647–1656. 2017.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Bardol T, Ferre L, Aouinti S, Dupuy M,
Assenat E, Fabre JM, Picot MC and Souche R: Survival after
multimodal treatment including surgery for metastatic esophageal
cancer: A systematic review. Cancers (Basel).
14(3956)2022.PubMed/NCBI View Article : Google Scholar
|