Introduction
Breast cancer is the most common malignancy in women
(1), negatively affecting women's
health, and distant metastasis is the main factor affecting
prognosis (2). The most common
sites of distant breast cancer metastasis are the lung, liver, bone
and brain. Luminal breast cancer is most likely to metastasize
first to bone. Furthermore, among the breast cancer types,
HR−/HER2+ tumors have the highest rates of
liver metastasis, and HR+/HER2- tumors have
the highest rates of lung metastasis. The brain has been previously
reported to be a preferred site of metastasis in patients with
triple-negative cancers (3).
However, metastasis to the female reproductive system is less
common, but when breast cancer does metastasize to the reproductive
system, it is most commonly observed in the ovaries. The small size
of the uterus, limited blood flow to the distal region, and
abundant fibrous tissue within the uterus collectively create an
environment that is not conducive to the spread of malignant tumors
(4). Consequently, uterine
metastatic cancer represents <10% of female reproductive system
metastases (5). The metastatic
patterns of lobular and ductal invasive breast cancer differ,
although it is not explicitly known why this is the case. Invasive
lobular carcinoma (ILC) metastasis usually involves the peritoneum,
gastrointestinal tract and ovaries, whereas invasive ductal
carcinoma (IDC) more commonly involves the lungs and pleura
(6). The results of prior studies
based on tumor registry data have demonstrated that ILC
metastasizes to gynecologic organs in ~4.5% of cases, whereas IDC
metastasizes to these organs in 0.8% of cases (7). Currently, the number of reported
cases of breast cancer metastasis to the reproductive tract, both
domestically and internationally, is limited. Therefore, additional
data are needed to enhance our understanding of this phenomenon. In
the present study, two cases of breast cancer combined with
reproductive system metastasis and a synthesis of the clinical
characteristics of this disease are presented on the basis of the
previous literature. The characteristics of the patients are shown
in Table I.
 | Table IPatient characteristics. |
Table I
Patient characteristics.
| | Age PT (year) | Age met (year) | Time PT- Mets
(months) | Histology | Stage | Her-2 | ER | PR | Pt Treatment | Endocrine
therapy | Met Symptoms | Other site | Met Treatment |
|---|
| Case 1 | 53 | 54 | 9 | IDC | IA | 3+ | - | - | Surgery,
Chemotherapy, Radiotherapy, Targeted therapy | - | Vaginal bleeding | - | - |
| Case 2 | 32 | 36 | 38 | IDC (Mixed) | IIIC | + | + | + | Surgery,
Chemotherapy, Radiotherapy, Targeted therapy | Exemestane
Leuprolide | - | - | - |
Case presentation
Patient 1
A 54-year-old female patient underwent local
excision of the primary tumor in the left breast and axillary
sentinel lymph node biopsy at Peking Union Medical College Hospital
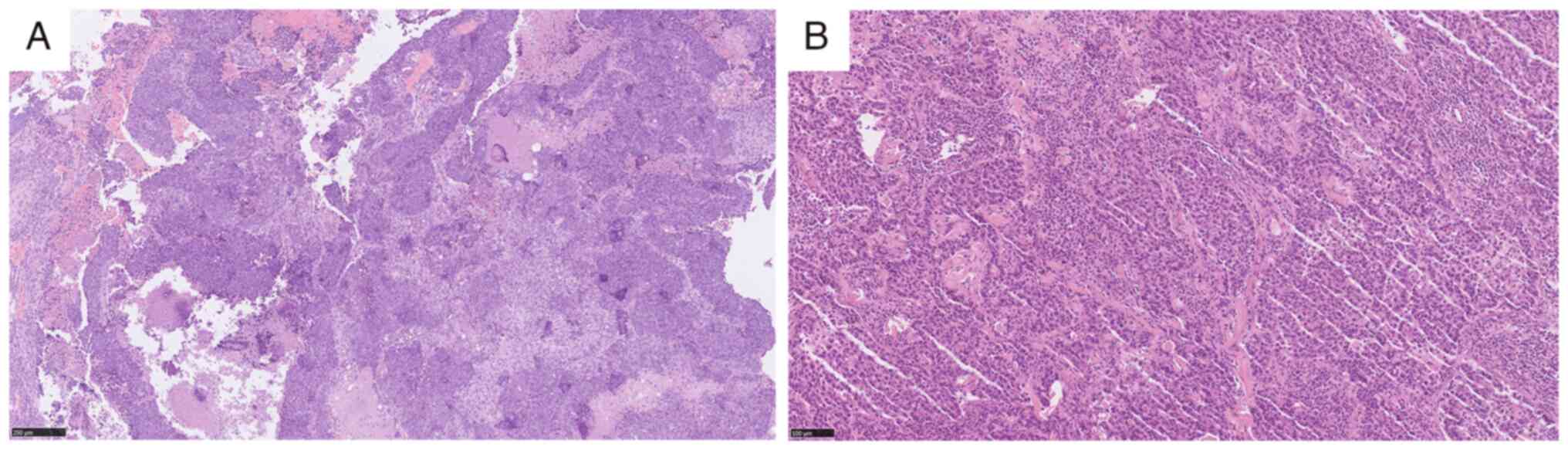
(Beijing, China) in February 2023. The postoperative pathological
diagnosis was IDC of no special type that was poorly differentiated
(Fig. 1A), with no evidence of
metastasis in the sentinel lymph nodes. Immunohistochemical
analysis (Paraffin-embedded, light microscope) revealed the
presence of HER2 protein (3+), a negative result for estrogen
receptor (ER) and progesterone receptor (PR), and a Ki-67 index of
60%. Accordingly, the patient was diagnosed with invasive carcinoma
in the left breast, stage IA, human epidermal growth factor
receptor 2 (Her-2) overexpression type. Following surgical
intervention, the patient underwent six cycles of chemotherapy
comprising 120 mg docetaxel, 600 mg carboplatin and
trastuzumab-targeted therapy. Additionally, the patient underwent a
course of adjuvant radiotherapy to the left breast with 42.4 Gy in
16 treatment fractions followed by a boost to her lumpectomy cavity
with 10.6 Gy in 4 fractions. During the radiotherapy course, the
patient developed minor vaginal bleeding without accompanying
clinical symptoms such as abdominal pain. Initially, the patient
did not seek medical attention for this symptom. However, the
volume of bleeding subsequently increased. On gynecological
ultrasound, the endometrial assessment revealed a thickness of 11
mm, with heterogeneous echogenicity but no evidence of focal
thickening, and the myometrium and adnexa were unremarkable.
Magnetic resonance imaging indicated the possibility of a
hysteromyoma, with CA125 at 14.2 U/ml and CA19-9 at 21.1 U/ml.
Therefore, she underwent a dilatation and curettage (D&C)
biopsy for histological diagnosis of the endometrium. Postoperative
pathology revealed that the lumps of neoplastic cells suggested
poorly differentiated carcinoma and, in combination with the
immunohistochemistry results and medical history, metastatic
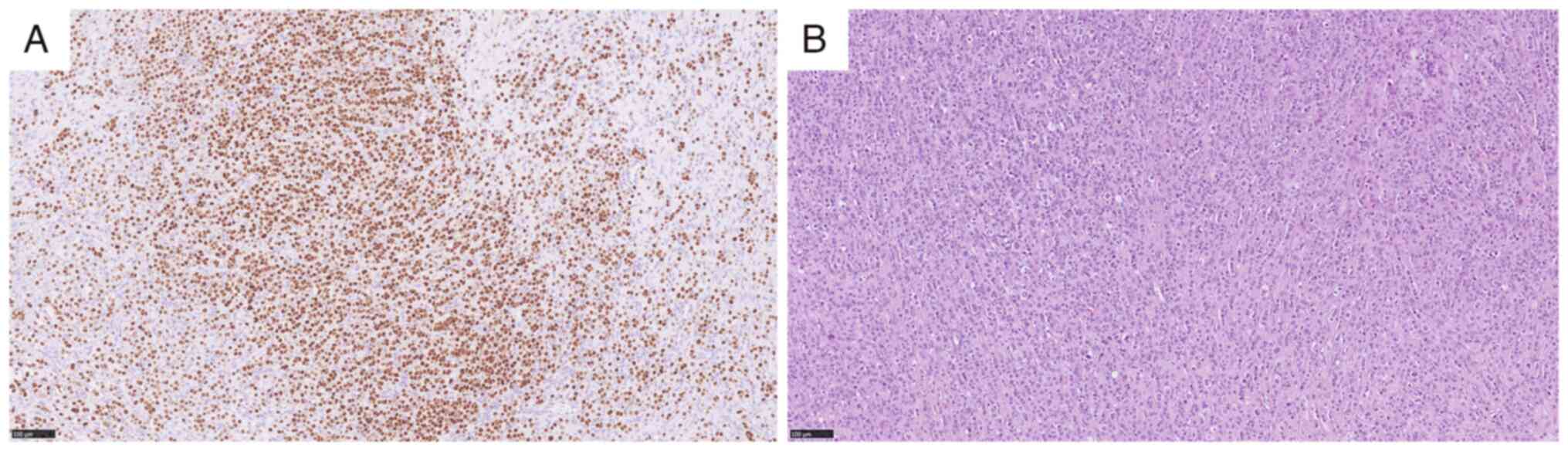
invasive breast carcinoma of no special type (Fig. 1B). Immunohistochemistry revealed ER
(-), PR (-) and Ki-67 (index 70%). The immunohistochemical analysis
revealed positive staining for E-cadherin; partial positivity for
CEA and CK5; and negative staining for GCDFP-15, P63, P16 and
vimentin. The positron emission tomography/computed tomography
(PET/CT) exam was refined on 13 November 2023 and confirmed a
heterogeneous increase in metabolic activity in the uterine body
and cervix, the nature of which has yet to be determined. The
patient subsequently underwent hysterectomy and bilateral
salpingo-oophorectomy laparoscopically at our institution.
Postoperative pathology suggested chronic cervicitis and
endometritis, which were subsequently treated with oral
capecitabine for chemotherapy.
Patient 2
A 36-year-old woman was admitted to Peking Union
Medical College Hospital (Beijing, China). In December 2020, she
underwent right modified radical mastectomy. The pathological
examination of the tumor revealed a mixed nonspecial type and ILC,
intermediate differentiation, with lymph node metastasis (15/15 in
the axilla, 5/5 at the third station) (Fig. 2A). Immunohistochemical analysis
revealed the presence of ER protein in moderate quantities (90%),
PR protein in moderate quantities (80%), Her-2 protein in the 1+
category, Ki-67 protein in the 70% category, and androgen receptor
(AR) protein in high quantities (80%). The patient was diagnosed
with mixed invasive breast cancer, stage III C, luminal B type.
After the surgical procedure, the patient was administered a course
of epirubicin and cyclophosphamide for a total of four cycles,
followed by four cycles of paclitaxel. Intensity-modulated
radiotherapy was initiated for the right chest wall and the region
of the supraclavicular and axillary lymph nodes, with 50 Gy in 25
treatment fractions. The patient was subsequently treated with
exemestane and leuprolide. On 6 February 2024, when the patient
revisited the institution for breast cancer, a gynecological
ultrasound revealed the presence of a hypoechoic mass in the right
adnexal area (4.0x3.8 cm), as well as a hyperechoic lesion in the
left ovary (2.1x2.1 cm). The CA-125 level was 99.2 U/ml, while the
CA-153 level was 123.3 U/ml. At this time, the patient did not
exhibit any abnormal vaginal bleeding or abdominal pain, nor were
there other notable clinical symptoms. A professor of gynecology in
our hospital suggested surgical treatment. On 26 February 2024, the
patient underwent hysterectomy and bilateral salpingo-oophorectomy,
high ligation of the ovarian vessels, and pelvic adhesion lysis
laparoscopically at our hospital. The pathological examination
revealed that the heterotypic cells infiltrated the fallopian tube
and ovarian tissue (right side), which was consistent with
metastatic breast cancer. The endometrium was observed to be in the
proliferative stage in the uterus, heterotypic cells were observed
in the uterine wall, and metastatic cancer was not excluded
(Fig. 2B). The results of the
immunohistochemical analysis were as follows: ER (moderate
positive, 95%), PR (moderate positive, 20%), Her-2 (2+), Ki-67
(index 30%), E-cadherin (membranous+), GATA3 (+), TRPS1 (+), PAX
(-), AE1/AE3 (+), AR (strongly positive, 95%), P120 (cytoplasmic+),
and β-catenin (membranous and cytoplasmic+). Fluorescence in
situ hybridization revealed HER2(-) cells (data not shown).
After the surgical procedure, the patient was administered
abemaciclib and fulvestrant for endocrine therapy.
Discussion
In 2022, the incidence rates of breast cancer
(23.8%) far exceeded those of other cancers in women, followed by
lung cancer (9.4%). Breast cancer is the most common cancer in
women and has a high mortality rate. The incidence and mortality of
breast cancer are significantly influenced by demographic
characteristics and geographical factors. White European and
American women exhibit the highest incidence rates, ~130 per
100,000 individuals; however, women of African descent experience a
higher mortality rate, which may be related to disparities in
healthcare resources. By contrast, the incidence of breast cancer
is relatively low among Asian women, although it has increased
rapidly in recent years (Table
II). The highest incidence rates were observed in France,
Australia/New Zealand, North America and Northern Europe, where
they are ~4-fold higher than those reported in South-Central Asia
and Middle Africa (8). Among the
pathological breast cancer subtypes, IDC accounts for >70% of
cases, and ILC accounts for 5-15% of cases; however, the latter is
the most common pathological type of metastatic breast cancer
(9). In their study, Wang et
al (10) analyzed 18,322
patients with metastatic breast cancer and reported that bone
metastasis accounted for 39.8% of metastasis cases, followed by
lung (10.94%), liver (7.34%) and brain metastasis (1.51%).
Metastases of extragenital malignancies to the reproductive system
are rare, most commonly in the digestive system (37.6%), followed
by breast cancer, which often involves the ovaries (75.8%) and
vagina (13.4%), followed by the endometrium (4.7%), cervix (3.3%)
and salpinx (0.7%) (5,11). Since the cervix is composed mainly
of fibrous muscle tissue with a limited blood supply and only
incoming lymphatic drainage, metastasis to the cervix is extremely
rare (12).
 | Table IIIncidence and mortality rates of
breast cancer across different ethnic groups. |
Table II
Incidence and mortality rates of
breast cancer across different ethnic groups.
| Ethnicity | Incidence rate (per
100,000) | Mortality rate (per
100,000) | Hazard ratio (95%
confidence interval) | Risk Factor
characteristics |
|---|
| Caucasian (European-
American) | 132.5 | 19.8 | 1.0 (Reference) | High hormone
replacement therapy usage rate (25%), Late childbirth (average
first birth age of 28 years) |
| African American | 126.7 | 28.3 | 1.12 (1.05-1.19) | High proportion of
triple-negative breast cancer (21% vs. 10% in Caucasians), High
rate of medical treatment delay (34% delayed for more than 3
months) |
| Asian American | 89.4 | 11.2 | 0.68 (0.63-0.73) | Protective effect of
traditional diet (high intake of beans), But the incidence rate
increases by an average of 3.5% annually due to Westernized
lifestyle |
| Hispanic | 92.1 | 14.3 | 0.83 (0.78-0.89) | High proportion of
obesity-related breast cancer (38% with BMI>30), Lower screening
rate than Caucasians (65% vs. 73%) |
| Ashkenazi Jewish | 215.0 | 24.5 | 2.1 (1.9-2.3) | High BRCA1/2 mutation
carrier rate of 2.5% (0.2% in the general population), 28% of
early-onset cancer under the age of 50 |
The timing of the occurrence of reproductive system
metastasis in patients with breast cancer is inconsistent, and the
precise mechanism of reproductive system metastasis remains
unclear. At present, the literature on breast cancer metastasis to
the reproductive system both domestically and internationally is
composed primarily of case reports. The most frequently observed
presentation of metastasis is vaginal bleeding (13). Additionally, the diagnosis of
asymptomatic metastases among these patients is incidental, and
asymptomatic metastasis is more likely to be overlooked than
metastasis with abnormal vaginal bleeding symptoms. Despite the
presence of uterine lesions, as evidenced on gynecological
ultrasound or CT, there was no previous history of gynecological
disease or current symptoms among these patients. Consequently, no
further diagnosis was made. Metastatic uterine malignant tumors are
frequently misdiagnosed as uterine fibroids or primary uterine
malignant tumors on imaging, particularly following tamoxifen
treatment. Endocrine medication is associated with a 5-30%
incidence of increased endometrial thickness, a 26-60% incidence of
endometrial polyps, and an endometrial cancer (EC) incidence of
0.8-8%, all of which are 2-7 times greater than those of the
general population (14).
Furthermore, international researchers have discovered that in
individuals receiving endocrine therapy following breast cancer
surgery, age is a risk factor for the development of EC.
Premenopausal patients account for ~52% of endometrial disease
cases, and EC is more common in patients older than 35 years
(15). Patients are advised to
receive routine examinations. Because the symptoms of endometrial
alterations can be mistaken for those of other gynecological
disorders, there is a chance of misdiagnosis even though the actual
incidence of EC caused by endocrine therapy is low, at 0.1-0.2%
(16). In such cases, a
differential diagnosis of endocrine drug-induced primary EC is
essential (17). Mazur et
al (5) reported that ~42% of
metastatic cervical tumors are incorrectly identified as primary
cervical tumors. Nevertheless, importantly, some metastases are
detected prior to or concurrently with the primary tumor (18,19).
A pathological biopsy is typically the most rigorous criterion for
differentiating a primary mass from a secondary mass that has
metastasized beyond the reproductive tract. In cases of highly
suspicious but difficult to differentiate findings on the basis of
the imaging presentation, accurate immunohistochemistry is needed.
It is therefore of particular importance to consider the
contributions of pathology and immunology.
GATA3 is one of six members of the GATA family of
transcription factors. It plays a specific role in regulating
mammary gland morphogenesis and the differentiation of luminal
epithelial cells in the breast (20,21).
The expression rates of GATA-3 in IDC and ILC are 91 and 100%,
respectively, whereas in EC, the expression rate is only 2%.
Furthermore, GATA-3 is not expressed in cervical adenocarcinoma or
ovarian mucinous carcinoma (22,23).
In the present study, Patient 2 had GATA3 expression in the
reproductive system tissues and a history of breast cancer.
Therefore, in such cases, breast cancer metastasis to the
reproductive system has to be strongly considered.
Treatment and prognosis
In patients with breast cancer metastasis to the
reproductive tract, the disease prognosis is typically poor, and
there is currently no uniform diagnosis or treatment plan. In some
studies, it has been indicated that palliative hysterectomy and
bilateral salpingo-oophorectomy were suggested as effective forms
of castration therapy; however, the evidence supporting this is
inconclusive with respect to survival outcomes. In other studies,
systemic chemotherapy was suggested to be more efficacious when it
is administered alone. Despite the generally poor prognosis among
this group of patients, some patients achieve complete remission
and remain disease-free for extended periods, with survival
exceeding 20 years in some patients (24).
The present article presents two cases. In Patient
1, metastasis occurred in the uterine body and cervix, with
abnormal vaginal bleeding as the initial symptoms. The patient was
diagnosed at an early stage, with metastasis already present. In
this patient, metastasis occurred when the primary tumor was in an
early stage, almost at the same time as the primary tumor, and
there was no metastasis to the lymph nodes or other sites, which is
quite rare and has not been reported previously. The patient is
currently undergoing regular follow-up, with no evidence of tumor
recurrence or metastasis to other sites. In Patient 2, metastasis
to the common ovary and uterus occurred, with no clinical symptoms.
However, high echogenicity in the adnexa was observed on
ultrasound. The disease was staged as an advanced stage malignancy,
with an ILC component, and the pathological examination of the
metastatic lesion indicated that it was primarily a metastasis of
the ILC component. The GATA3 result was positive, whereas the PAX8
result was negative. Immunohistochemistry provided clear evidence
that the tumor had originated in the breast, thus providing a means
of distinguishing it from primary ovarian cancer. The patient
underwent surgical intervention in conjunction with endocrine
therapy, and the current status remained stable with regular
follow-up.
In summary, although breast cancer metastasis to the
reproductive system is rare, for patients with breast cancer,
regular gynecological ultrasound should be performed during
follow-up, even in the absence of clinical symptoms. Caution should
be exercised in the event of the occurrence of metastatic tumors in
the reproductive tract, particularly in patients with late-stage
infiltrating lobular carcinoma and a history of similar drug
treatments, such as tamoxifen. GATA-3 and other immunohistochemical
markers are helpful in differentiating primary reproductive system
tumors. At present, there is no consensus regarding the optimal
treatment approach for these patients; the most important issue in
clinical studies is the low number of patients because this type of
metastasis is uncommon. It is considered that once more related
cases are reported both domestically and internationally, a
meta-analysis will be the next step, and on the basis of the
findings of the meta-analysis, the best course of treatment can be
chosen.
Acknowledgements
Not applicable.
Funding
Funding: The present study was supported by the National Key
R&D Program of China (Ministry of Science and Technology; grant
no. 2023YFC2411504).
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
LHL, CXY and HXR contributed to the study conception
and design. CXY prepared material and performed data analysis. LHL
wrote the first draft of the manuscript. All authors commented on
previous versions of the manuscript. HXR and CXY confirm the
authenticity of all the raw data. All authors read and approved the
final version of the manuscript.
Ethics approval and consent to
participate
The case report was approved (approval no. K24C3535)
by the Ethics Committee of Peking Union Medical College Hospital
Chinese Academy of Medical Sciences & Peking Union Medical
College (Beijing, China). Written informed consent was obtained by
the patients prior to registration.
Patient consent for publication
Patient consent for publication of relevant data was
provided by the patients.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Katsura C, Ogunmwonyi I, Kankam HK and
Saha S: Breast cancer: Presentation, investigation and management.
Br J Hosp Med (Lond). 83:1–7. 2022.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Criscitiello C and Corti C: Breast cancer
genetics: Diagnostics and treatment. Genes (Basel).
13(1593)2022.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Wang R, Zhu Y, Liu X, Liao X, He J and Niu
L: The Clinicopathological features and survival outcomes of
patients with different metastatic sites in stage IV breast cancer.
BMC Cancer. 19(1091)2019.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Pérez-Montiel D, Serrano-Olvera A, Salazar
LC, Cetina-Pérez L, Candelaria M, Coronel J, Montalvo LA and de
León DC: Adenocarcinoma metastatic to the uterine cervix: A case
series. J Obstet Gynaecol Res. 38:541–549. 2012.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Mazur MT, Hsueh S and Gersell DJ:
Metastases to the female genital tract-Analysis of 325 case.
Cancer. 53:1978–1984. 1984.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Mathew A, Rajagopal PS, Villgran V, Sandhu
GS, Jankowitz RC, Jacob M, Rosenzweig M, Oesterreich S and Brufsky
A: Distinct pattern of metastases in patients with invasive lobular
carcinoma of the breast. Geburtsh Frauenheilk. 77:660–666.
2017.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Waks AG, Lennon J, Yadav BS, Hwang H,
dSchapirael Carmen M, Johnson NB, Reynolds K, Schapira L, Gilman PB
and Overmoyer B: Metastasis to the cervix uteri 15 years after
treatment of lobular carcinoma of the breast. Semin Oncol.
42:e81–e94. 2015.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Bray F, Laversanne M, Sung H, Ferlay J,
Siegel RL, Soerjomataram I and Jemal A: Global cancer statistics
2022: GLOBOCAN estimates of incidence and mortality worldwide for
36 cancers in 185 countries. CA Cancer J Clin. 74:229–263.
2024.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Martinez V and Azzopardi JG: Invasive
lobular carcinoma of the breast: Incidence and variants.
Histopathology. 3:467–488. 1979.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Wang R, Zhu Y, Liu X, Liao X, He J and Niu
L: The clinicopathological features and survival outcomes of
patients with different metastatic sites in stage IV breast cancer.
BMC Cancer. 19(1091)2019.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Rahmani M, Nili F and Tabibian E:
Endometrial metastasis from ductal breast carcinoma: A case report
with literature review. Am J Case Rep. 19:494–499. 2018.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Lokadasan R, Ratheesan K, Sukumaran R and
Nair SP: Metastatic lobular carcinoma of breast mimics primary
cervix carcinoma: Two case reports and a review of the literature.
Ecancermedicalscience. 9(571)2015.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Enling L, Liqun W, Yanmei Z, et al:
Clinical study on endometrial lesions induced by tamoxifen in
postoperative breast cancer patients. Chin J Mod Med. 23:106–108.
2013.
|
|
14
|
Early Breast Cancer Trialists'
Collaborative Group (EBCTCG). Aromatase inhibitors versus tamoxifen
in early breast cancer: Patient-level meta-analysis of the
randomised trials. Lancet. 386:1341–1352. 2015.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Ghanavati M, Khorshidi Y, Shadnoush M,
Akbari ME, Ardehali SH, Chavarri-Guerra Y, Akbari A,
Barragan-Carrillo R, Amlashi MA, Javid Z, et al: Tamoxifen use and
risk of endometrial cancer in breast cancer patients: A systematic
review and dose-response meta-analysis. Cancer Rep.
6(e1806)2023.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Committee Opinion No. 601. Tamoxifen and
uterine cancer. American College of Obstetricians and
Gynecologists. Obstet Gynecol. 123:1394–1397. 2014.
|
|
17
|
Singh P, Patro SS, Singhal T, Parida GK
and Agrawal K: Uterine metastasis presenting as abnormal uterine
bleeding in a case of primary breast cancer identified on
18F-FDG PET/CT. J Nucl Med Technol. 51:333–334.
2023.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Colak E, Erinanc OH and Ozdemir D:
Diagnosis of micropapillary carcinoma of the breast by endometrial
biopsy in a postmenopausal patient with abnormal uterine bleeding.
Ann Ital Chir. 10:2021.PubMed/NCBI
|
|
19
|
Arif SH, Mohammed AA and Mohammed FR:
Metastatic invasive lobular carcinoma of the breast to the
endometrium presenting with abnormal uterine bleeding; Case report.
Ann Med Surg (Lond). 51:41–43. 2020.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Ren M, Cai X, Jia L, Bai Q, Zhu X, Hu X,
Wang Q, Luo Z and Zhou X: Comprehensive analysis of cancer of
unknown primary and recommendation of a histological and
immunohisto-chemical diagnostic strategy from China. BMC Cancer.
23(1175)2023.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Asch-Kendrick R and Cimino-Mathews A: The
role of GATA3 in breast carcinomas: A review. Hum Pathol. 48:37–47.
2016.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Jingping Y, Juan W, Xinxin Y, et al: The
pathological diagnostic value of GATA3, MGB, and GCDFP-15 in breast
cancer. Chin J Endocr Surg. 14:94–99. 2020.
|
|
23
|
Rao M, Khade S, Chaudhary R, Singh P,
Yadav G, Elhence P, Nalwa A, Sharma R and Goel AD: Comparison of
GATA-3, mammaglobin and GCDFP-15 expression in primary, metastatic
and triple negative breast carcinomas: An Indian scenario. Asian
Pac J Cancer Prev. 24:509–515. 2023.PubMed/NCBI View Article : Google Scholar
|
|
24
|
O'Shaughnessy J: Extending survival with
chemotherapy in metastatic breast cancer. Oncologist. 10
(Suppl):S20–S29. 2005.PubMed/NCBI View Article : Google Scholar
|