Introduction
The anterior cerebral artery (ACA) and its divisions
enclose symptomatically critical differentiations. Anatomical
variations of the distal ACA that are irregularly detected can be
separated into three main groups, namely azygos, bihemispheric and
median ACA variations (1). The
azygos ACA appears after the fusion of the two A2 sections, which
pass through the medial wall of the brain and separate under the
genus (2-7).
In addition, when one of the two A2 divisions is hypoplastic, the
contralateral artery separates to irrigate the hemispheres at the
same time. This structure is known as a bihemispheric ACA (6,8,9). When an additional third distal ACA
branch appears, running to the distal medial surface of one or both
hemispheres, this anatomical variant is named median ACA (8,10-12).
The acquaintance with the ACA structure is essential for
neurosurgeons and radiologists in the identification and managing
pathological injuries, although avoiding lesions such as aneurysm
development and low irrigation, leading to cerebral ischemia
(13).
As the number of available studies on the prevalence
of the ACA anatomical variations are limited, the present
systematic review and meta-analysis aimed to determine the precise
incidence of these variants. In addition, with the comparative
description between cadaveric (autopsy) and imaging cases, more
accurate results can be extracted from the prevalence presentation
of the distal ACA variants.
Data and methods
Literature search strategy
The present meta-analysis examined the relative
studies involving intracranial ACA variations imaging vs. autopsy
evaluation throughout electronic records, counting the Cochrane
Library, PubMed (until December, 2023), Embase (until December,
2023), and MEDLINE (until December, 2023). For the study protocol
establishment and plan, the Preferred Reporting Items for
Systematic Reviews and Meta-Analyses (PRISMA) guidelines were
applied. The key words ‘anterior cerebral artery’, ‘Anatomy A1’,
‘Anatomy A2’, ‘anterior cerebral artery variations’ and ‘anterior
cerebral artery anomalies’ were used.
Selection of studies
For the evaluation of the risk of bias, the Cochrane
Collaboration tool was applied by two authors (GF and AGB) for each
article. The evaluation included random sequence generation and
allocation concealment. The assessed results were classified
according to the percentage of the risk into low, high or unclear.
In the case of a discrepancy, a different investigator with
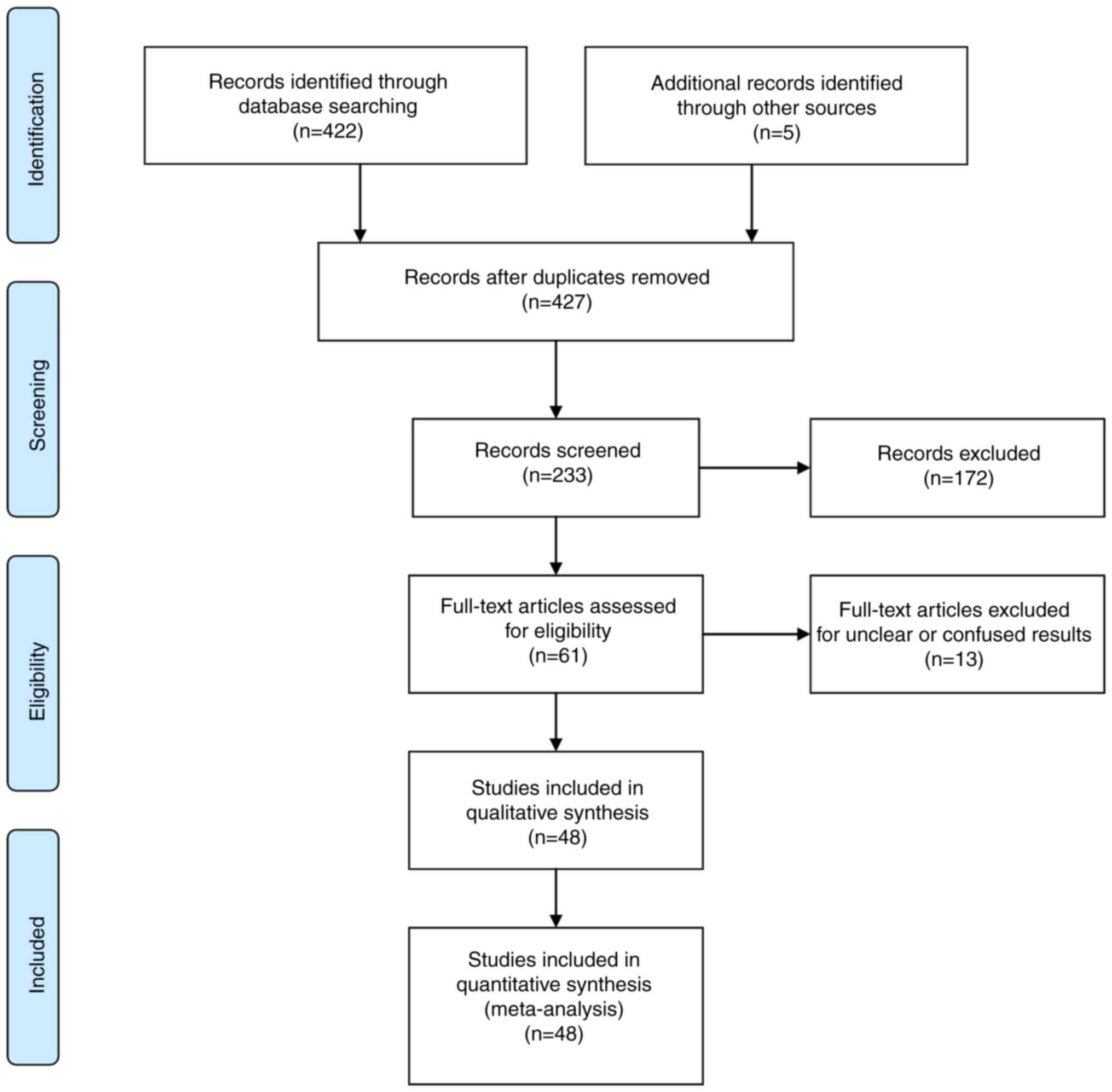
authority provided the concluding solution. The flow chart of the
data extraction procedure is presented in Fig. 1.
Screening
The following exclusion criteria were used:
Duplicate articles and those without clear results were excluded
from the final article pool. Bibliographic fields, such as title,
abstract and investigators were noticeable through the screening.
The final article pool excluded duplicate articles and those with
no clear results. Records were identified through database
searching (n=422 articles) and an additional search through
additional bases also identified articles (n=5). Documentations
after duplicates were eliminated (n=427). The records were screened
(n=233), and records were ruled out (n=172). Full-text articles
were evaluated for inclusion criteria (n=61) and eliminated for
unclear or confusing results (n=13). The remaining articles were
included in the qualitative procedure (n=48). The inclusion
criteria were the following: i) Included relative studies involving
intracranial ACA variations imaging vs. autopsy evaluation; ii)
were primary research articles; and iii) studies published in the
English language.
Extraction process
The following entities were extracted from the
selected studies: Estimations of associations between different ACA
variations, sample sizes and sample characteristics, the prevalence
of each ACA variation, and comparisons between imaging and autopsy
data. A total of 48 articles were independently found to fulfill
the criteria. There is no test to evaluate the export agreement.
The extraction procedures are usual compromises and depend on a
large sample of patients (>24.949 patients in the 48 included
studies).
For the primary research question, the present study
used PICOS criteria (population, intervention, comparison, outcomes
and study), to determine eligibility into the article pool. The
complete information of these studies is presented in Table I.
 | Table IDetermined prevalence of anatomical
characteristics based on study type (autopsy or imaging). |
Table I
Determined prevalence of anatomical
characteristics based on study type (autopsy or imaging).
| A, Autopsy |
|---|
| Author(s), year of
publication | Study design | Total no. of
patients, n=24, 949 (100%) | Azygos ACA,
n=127/22, 429 (0.6%) | Bihemishperic ACA,
n=109/1, 811 (6.0%) | Median ACA,
n=319/6, 706 (4.7%) | (Refs.) |
|---|
| Windle et
al, 1888 | Retro | 200 | 6 | 0 | 9 | (15) |
| Fawcett and
Blachford, 1905 | Retro | 700 | 0 | 0 | 23 | (16) |
| Jain, 1964 | Retro | 300 | 0 | 0 | 26 | (18) |
| Fisher, 1965 | Retro | 414 | 7 | 0 | 0 | (19) |
| LeMay and Gooding,
1966 | Retro | 107 | 4 | 0 | 0 | (20) |
| Ring and
Waddington, 1968 | Retro | 25 | 0 | 2 | 0 | (22) |
| Dunker and Harris,
1976 | Retro | 20 | 2 | 0 | 0 | (23) |
| Ozaki et al,
1977 | Retro | 146 | 0 | 0 | 21 | (25) |
| Perlmutter and
Rhoton, 1978 | Retro | 25 | 0 | 16 | 0 | (26) |
| Tulleken, 1978 | Retro | 75 | 1 | 0 | 8 | (24) |
| Kayembe et
al, 1984 | Retro | 44 | 0 | 0 | 10 | (29) |
| Gomes et al,
1986 | Retro | 30 | 1 | 0 | 1 | (30) |
| Marinković et
al, 1990 | Retro | 22 | 0 | 0 | 2 | (31) |
| Ogawa et al,
1990 | Retro | 206 | 0 | 0 | 27 | (32) |
| Nathal et
al, 1992 | Retro | 134 | 0 | 0 | 5 | (33) |
| van der Zwan et
al, 1992 | Retro | 25 | 0 | 2 | 0 | (34) |
| Serizawa et
al, 1997 | Retro | 30 | 1 | 0 | 2 | (37) |
| Stefani et
al, 2000 | Retro | 38 | 1 | 0 | 3 | (12) |
| Avci et al,
2001 | Retro | 25 | 1 | 0 | 1 | (38) |
| Kulenović et
al, 2003 | Retro | 100 | 0 | 0 | 1 | (39) |
| Paul and Mishra,
2004 | Retro | 50 | 0 | 1 | 0 | (40) |
| Ugur et al,
2005 | Retro | 20 | 1 | 1 | 0 | (41) |
| Tao et al,
2006 | Retro | 45 | 0 | 0 | 1 | (42) |
| Ugur et al,
2006 | Retro | 50 | 2 | 0 | 0 | (44) |
| Kahilogullari et
al, 2008 | Retro | 30 | 0 | 0 | 10 | (46) |
| Kapoor et
al, 2008 | Retro | 1,000 | 9 | 0 | 23 | (10) |
| Nordon and
Rodrigues, 2012 | Retro | 50 | 0 | 0 | 3 | (49) |
| Swetha, 2012 | Retro | 70 | 0 | 0 | 1 | (50) |
| Gunnal et
al, 2013 | Retro | 39 | 0 | 7 | 1 | (51) |
| Kedia et al,
2013 | Retro | 500 | 9 | 1 | 1 | (5) |
| Cilliers et
al, 2018 | Retro | 30 | 0 | 0 | 5 | (54) |
| B, Imaging |
| Author(s), year of
publication | Study design | Total no. of
patients, n=24, 949 (100%) | Azygos ACA,
n=127/22, 429 (0.6%) | Bihemishperic ACA,
n=109/1, 811 (6.0%) | Median ACA,
n=319/6, 706 (4.7%) | (Refs.) |
| Baptista et
al, 1963 | Retro | 381 | 1 | 45 | 50 | (17) |
| Wollschlaeger et
al, 1967 | Retro | 291 | 3 | 0 | 0 | (21) |
| Huber et al,
1980 | Retro | 7,782 | 17 | 0 | 0 | (27) |
| Kwak et al,
1980 | Retro | 296 | 0 | 0 | 13 | (28) |
| Sanders et
al, 1993 | Retro | 5,190 | 2 | 0 | 0 | (35) |
| Macchi et
al, 1996 | Retro | 100 | 2 | 0 | 9 | (36) |
| Uchino et
al, 2006 | Retro | 891 | 18 | 0 | 27 | (43) |
| Bharatha et
al, 2008 | Retro | 504 | 1 | | 0 | (45) |
| Lehecka et
al, 2008 | Retro | 101 | 4 | 15 | 4 | (6) |
| Saidi et al,
2008 | Retro | 72 | 0 | 4 | 0 | (47) |
| Nowinski et
al, 2009 | Retro | 96 | 0 | 0 | 0 | (7) |
| Zurada et
al, 2010 | Retro | 115 | 2 | 0 | 3 | (48) |
| Stefani et
al, 2013 | Retro | 15 | 0 | 2 | 1 | (53) |
| Hamidi et
al, 2013 | Retro | 112 | 5 | 9 | 5 | (52) |
| Kovač et al,
2014 | Retro | 455 | 7 | 4 | 10 | (13) |
| Wan-Yin et
al, 2014 | Retro | 3,572 | 14 | 0 | 0 | (55) |
| López-Sala et
al, 2020 | Retro | 426 | 6 | 0 | 22 | (56) |
Secondary research question(s) were associated with
the study design and method (imaging or autopsy).
Expectations and hypotheses
It was hypothesized that there is a difference
between autopsy and imaging studies concerning the prevalence of
ACA variations. The variables used were azygos ACA, bihemispheric
ACA and median ACA. All prospective and retrospective studies that
evaluated these modalities were included. By contrast, reviews,
editorials, pediatric cases, case reports, uncertain methods, or
one of the two modalities separately from that article pool were
excluded. Moreover, in order to reduce the risk of bias in the
contained studies, the Newcastle-Ottawa Scale (NOS) was applied as
a quality evaluation measurement (Table
II) (14).
 | Table IINewcastle-Ottawa Scale (NOS) quality
assessment of final article pool. |
Table II
Newcastle-Ottawa Scale (NOS) quality
assessment of final article pool.
| A, Autopsy |
|---|
| | Newcastle-Ottawa
Scale | |
|---|
| Author(s), year of
publication | Study design | Selection | Comparability | Exposure | Total scores | (Refs.) |
|---|
| Windle et
al, 1888 | Retro | 3 | 3 | 3 | 9 | (15) |
| Fawcett and
Blachford, 1905 | Retro | 3 | 3 | 3 | 9 | (16) |
| Jain, 1964 | Retro | 3 | 3 | 3 | 9 | (18) |
| Fisher, 1965 | Retro | 3 | 3 | 3 | 9 | (19) |
| Lemay and Gooding,
1966 | Retro | 3 | 3 | 3 | 9 | (20) |
| Ring and
Waddington, 1968 | Retro | 3 | 3 | 3 | 9 | (22) |
| Dunker and Harris,
1976 | Retro | 2 | 2 | 3 | 7 | (23) |
| Ozaki et al,
1977 | Retro | 2 | 2 | 3 | 7 | (25) |
| Perlmutter and
Rhoton, 1978 | Retro | 2 | 3 | 3 | 8 | (26) |
| Tulleken, 1978 | Retro | 3 | 3 | 3 | 9 | (24) |
| Kayembe et
al, 1984 | Retro | 3 | 3 | 3 | 9 | (29) |
| Gomes et al,
1986 | Retro | 3 | 3 | 3 | 9 | (30) |
| Marinković et
al, 1990 | Retro | 3 | 3 | 3 | 9 | (31) |
| Ogawa et al,
1990 | Retro | 3 | 3 | 3 | 9 | (32) |
| Nathal et
al, 1992 | Retro | 3 | 3 | 3 | 9 | (33) |
| van der Zwan et
al, 1992 | Retro | 3 | 3 | 3 | 9 | (34) |
| Serizawa et
al, 1997 | Retro | 3 | 3 | 3 | 9 | (37) |
| Stefani et
al, 2000 | Retro | 3 | 3 | 3 | 9 | (12) |
| Avci et al,
2001 | Retro | 3 | 3 | 3 | 9 | (38) |
| Kulenović et
al, 2003 | Retro | 3 | 3 | 3 | 9 | (39) |
| Paul and Mishra,
2004 | Retro | 3 | 3 | 3 | 9 | (40) |
| Ugur et al,
2005 | Retro | 3 | 2 | 3 | 8 | (41) |
| Tao et al,
2006 | Retro | 3 | 3 | 2 | 8 | (42) |
| Ugur et al,
2006 | Retro | 3 | 3 | 3 | 9 | (44) |
| Kahilogullari et
al, 2008 | Retro | 3 | 3 | 3 | 9 | (46) |
| Kapoor et
al, 2008 | Retro | 3 | 3 | 3 | 9 | (10) |
| Nordon and
Rodrigues, 2012 | Retro | 3 | 3 | 3 | 9 | (49) |
| Swetha, 2012 | Retro | 3 | 3 | 3 | 9 | (50) |
| Gunnal et
al, 2013 | Retro | 3 | 3 | 3 | 9 | (51) |
| Kedia et al,
2013 | Retro | 3 | 3 | 3 | 9 | (5) |
| Cilliers et
al, 2018 | Retro | 3 | 3 | 3 | 9 | (54) |
| B, Imaging |
| | Newcastle-Ottawa
Scale | |
| Author(s), year of
publication | Study design | Selection | Comparability | Exposure | Total scores | (Refs.) |
| Baptista et
al, 1963 | Retro | 3 | 2 | 3 | 8 | (17) |
| Wollschlaeger et
al, 1967 | Retro | 3 | 3 | 3 | 9 | (21) |
| Huber et al,
1980 | Retro | 3 | 3 | 3 | 9 | (27) |
| Kwak et al,
1980 | Retro | 3 | 3 | 3 | 9 | (28) |
| Sanders et
al, 1993 | Retro | 3 | 3 | 3 | 9 | (35) |
| Macchi et
al, 1996 | Retro | 3 | 3 | 3 | 9 | (36) |
| Uchino et
al, 2006 | Retro | 3 | 3 | 3 | 9 | (43) |
| Bharatha et
al, 2008 | Retro | 3 | 3 | 3 | 9 | (45) |
| Lehecka et
al, 2008 | Retro | 3 | 3 | 3 | 9 | (6) |
| Saidi et al,
2008 | Retro | 3 | 3 | 3 | 9 | (47) |
| Nowinski et
al, 2009 | Retro | 3 | 3 | 3 | 9 | (7) |
| Zurada et
al, 2010 | Retro | 3 | 3 | 3 | 9 | (48) |
| Stefani et
al, 2013 | Retro | 3 | 3 | 3 | 9 | (53) |
| Hamidi et
al, 2013 | Retro | 3 | 3 | 3 | 9 | (52) |
| Kovač et al,
2014 | Retro | 3 | 3 | 3 | 9 | (13) |
| Wan-Yin et
al, 2014 | Retro | 3 | 3 | 3 | 9 | (55) |
| López-Sala et
al, 2020 | Retro | 3 | 3 | 3 | 9 | (56) |
Statistical analysis
A random- and fixed-effects form meta-analysis was
used to evaluate the proportion estimate for every outcome
independently, as the I2 statistic was used to calculate
the heterogeneity. A value of I2 in an amount <50%
was considered as low heterogeneity, and an amount >50% was
considered as high heterogeneity. The consequences were illustrated
on forest plots. The Egger's regression test was used for the
calculation of the risk of publication bias. The statistical
package R We applied for all statistical analyses (R: Language and
Environment, 2010). A value of P<0.05 was considered to indicate
a statistically significant difference.
Results
In total, 48 articles (5-7,10,12,13,15,16-56)
fulfilled the eligibility criteria. The entire number of
participants was 24,949 [20,399 (81.7%) in imaging and 4,550
(18.3%) in autopsy observed groups]. The study sample was based on
48 articles (5-7,10,12,13,15,16-56)
(Table I) and all of these articles
were retrospective.
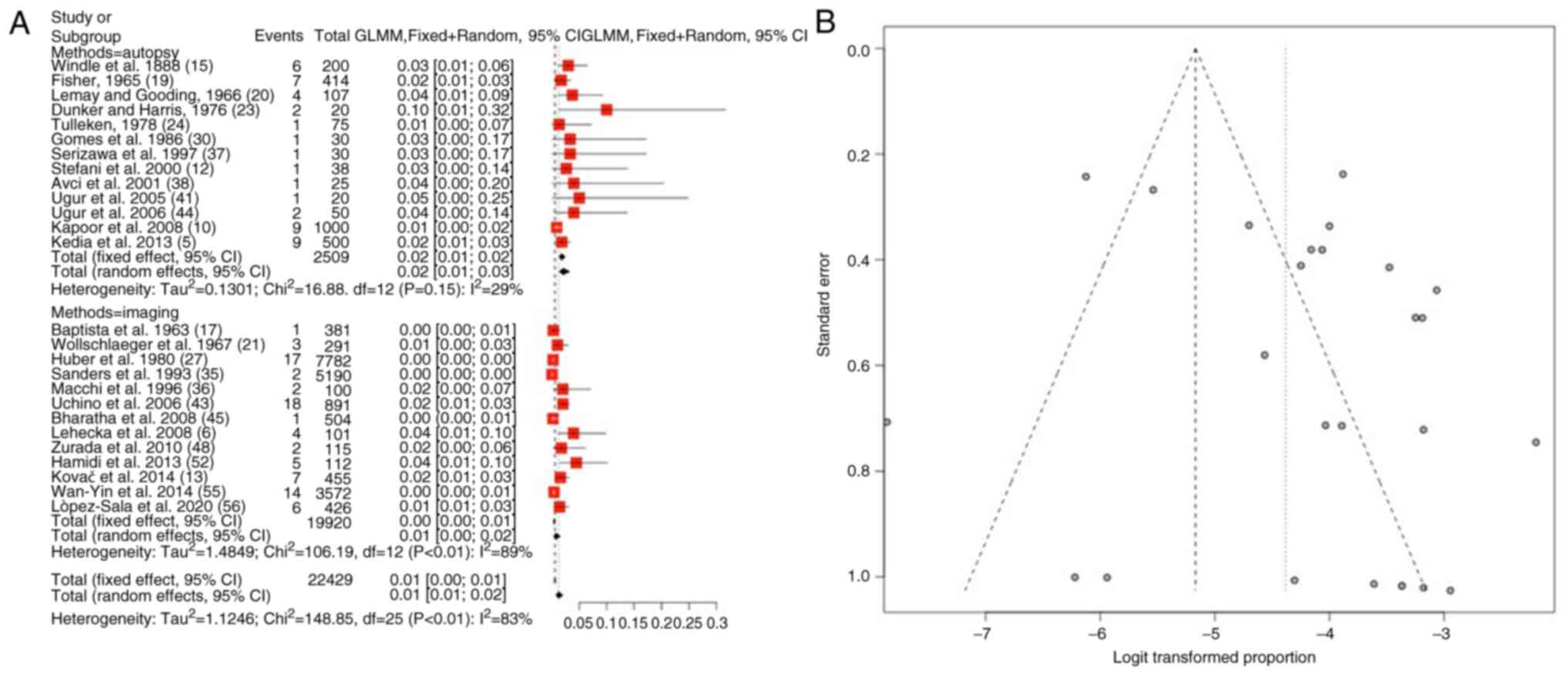
Azygos ACA variations
Information regarding azygos ACA variations was
available in 26 articles (5,6,10,12,13,15,17,19-21,23,24,27,30,35-38,41,43-45,48,52,55,56).
The total number of patients was 22,429 [19,920 (88.8%) in imaging
and 2,509 (11.2%) in autopsy observed groups]. The prevalence of
azygos ACA was 1.5% (mean) (95% CI, 0.01-0.02, P<0.01) (Table III and Fig. 2A). The heterogeneity was extensive
(I2=83%). When examining the funnel plot, it was
established that there was a significant publication bias
(P<0.01; Fig. 2B). No significant
differences were found between the prevalence established in
autopsy (2%) and imaging (1%) studies (Table III).
 | Table IIIParameters for the results of the
meta-analysis. |
Table III
Parameters for the results of the
meta-analysis.
| | Groups | Overall effect | Heterogeneity | Prevalence (%) |
|---|
| Parameters | Included Trials
(n=48) | Imaging | Autopsy | Effect
estimate | 95% CI | I2
(%) | P-value | Imaging | Autopsy |
|---|
| Azygos | 26 | 19920 | 2509 | 0.01 | (0.01-0.02) | 83 | <0.01 | 2 | 1 |
| Bihemishperic | 13 | 1136 | 675 | 0.01 | (0.03-0.12) | 89 | <0.01 | 7.5 | 11 |
| Median | 32 | 2892 | 3814 | 0.05 | (0.04-0.07) | 85 | <0.01 | 5 | 6 |
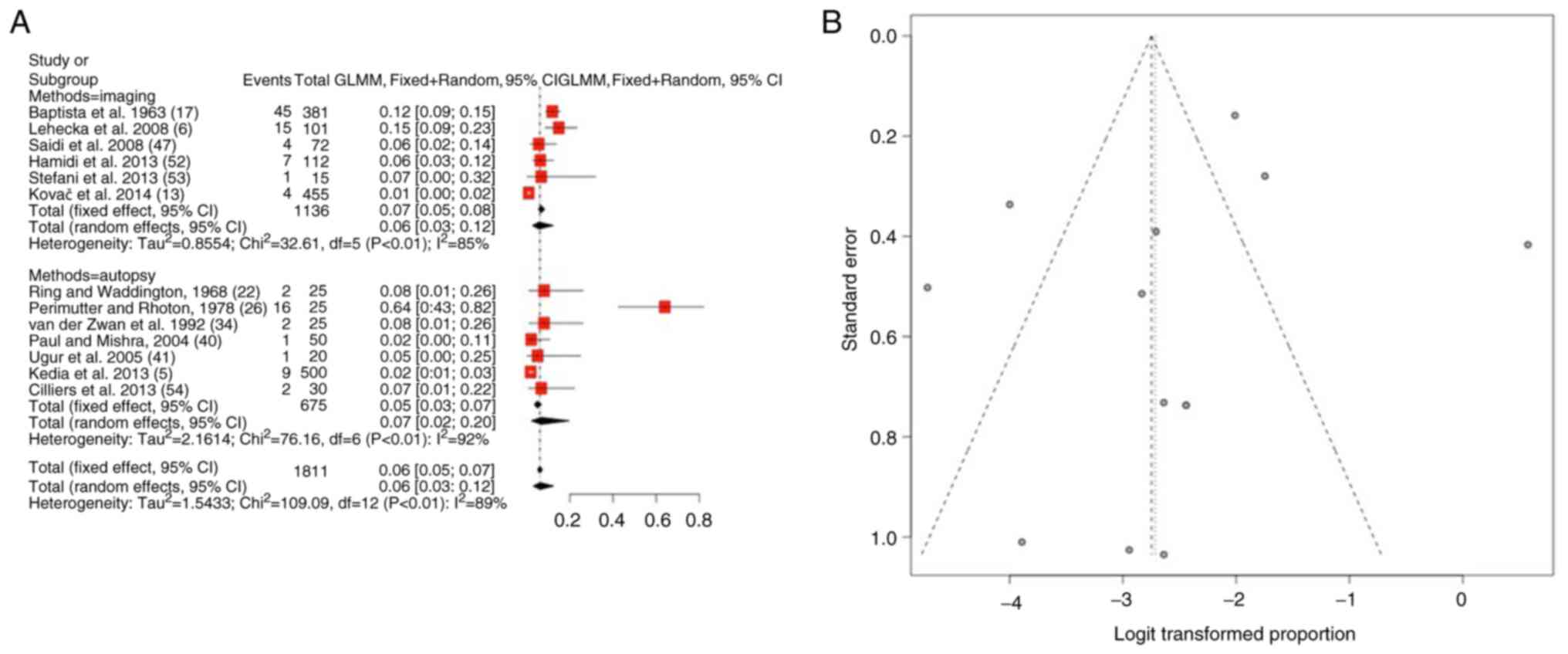
Bihemishperic ACA variations
As regards bihemispheric ACA variations, information
was available in 13 articles (5,6,13,17,22,26,34,40,41,47,52-54).
The total number of patients was 1,811 [1,136 (62.7%) in imaging
and 675 (37.3%) in autopsy-observed groups]. The prevalence of
bihemishperic ACA was 7.5% (mean) (95% CI, 0.03-0.12) (Table III and Fig. 3A). The heterogeneity was significant
(I2=89%). When examining the funnel plot, it was
established that there was a high publication bias (P<0.01)
(Fig. 3B). No statistically
significant differences were found between the prevalence of
autopsy (11%) and imaging (7.5%) studies (Table III).
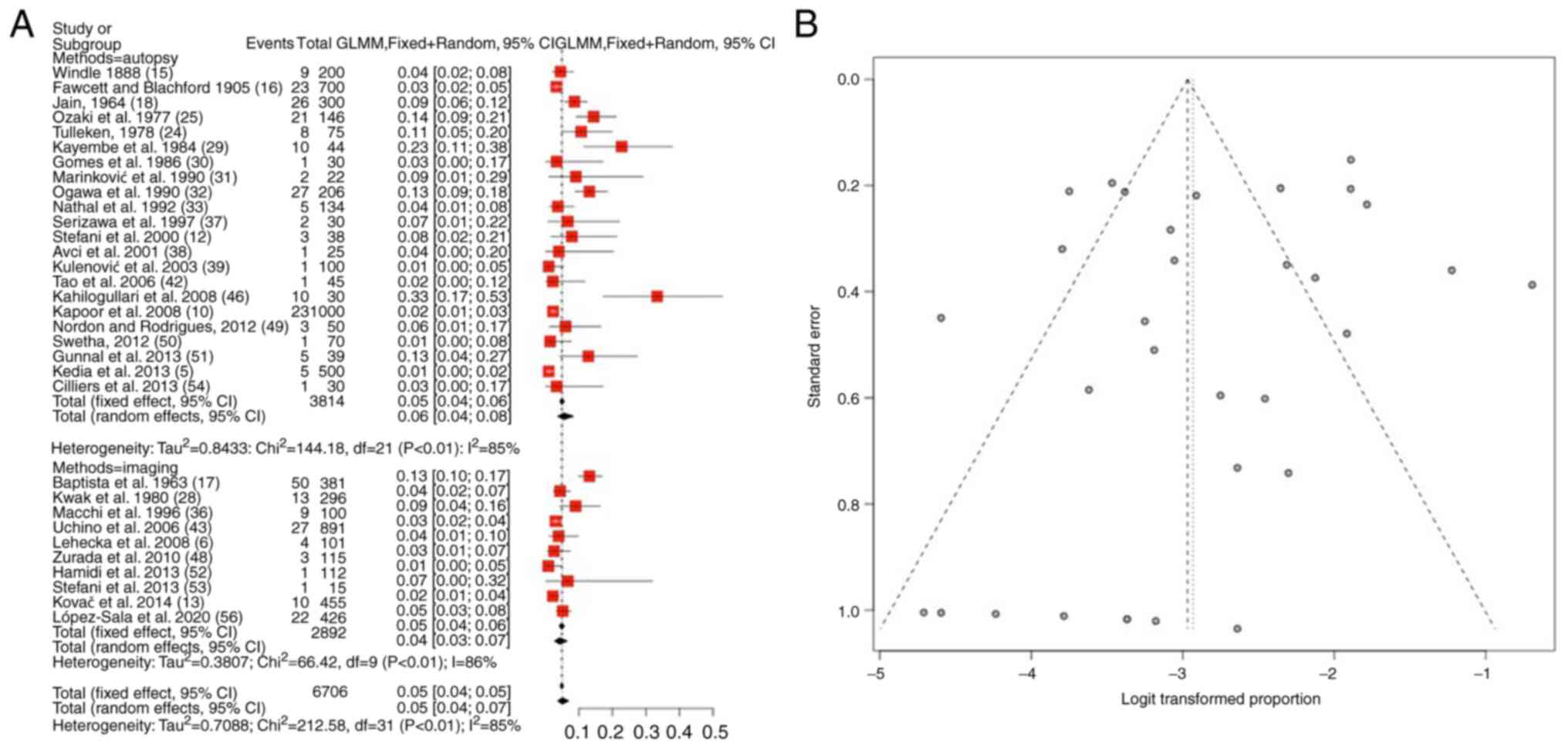
Median ACA variations
As regards, median ACA variations, information was
available in 32 articles (5,6,10,12,13,15-18,24,25,28-33,36-39,42,43,46,48-54,56).
The total number of patients was 6,706 [2,892 (43.1%) in imaging
and 3,814 (56.9%) in autopsy observed groups]. The prevalence of
the median ACA variant was 5.5% (mean) (95% CI, 0.04-0.07,
P<0.01) (Table III and Fig. 4A). The heterogeneity was considerable
(I2=85%). When examining the funnel plot, it was
established that there was a high publication bias (P<0.01)
(Fig. 4B). No considerable
differences were found between the prevalence evaluated in imaging
(5%) and autopsy (6%) articles (Table
III).
Discussion
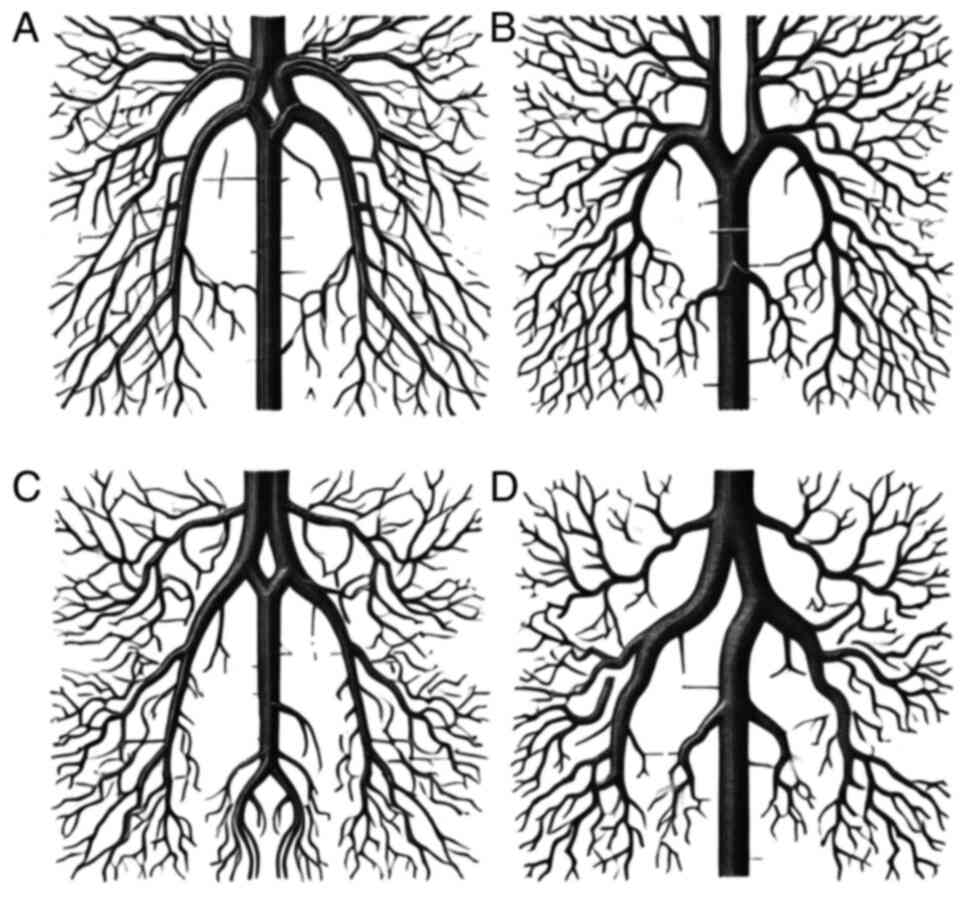
Anatomical variations of the distal ACA that are
irregularly detected can be separated into three main groups,
namely azygos, bihemispheric and median ACA variations (1) (Fig. 5).
Concerning the topography and morphology, the azygous ACA variation
reveals a particular midline vessel created from the connection of
bilateral A1 segments next to the typical locality of the anterior
communicating artery (A-comm) (20).
Thus, mainly the A-comm is mislaid or hypoplastic, and the formed
midline vessel passes through the inter-hemispheric fissure,
supplying the medial hemispheres with blood (20). The clinical interest of the azygous
ACA is that its appearance consists of pathologies leading to
infarcts or aneurysms (57,58). According to the literature, the
occurrence of an azygous ACA is 0.3% (2,59). The
present meta-analysis revealed that the prevalence of azygos ACA
was 1.5% [autopsy (2%) and imaging (1%)].
Another moderately comparable anatomic modification
is the bihemispheric ACA, where one of the two contralateral A1
segments is hypoplastic (59). Thus,
the bihemispheric ACA feeds the two pericallosal regions equally
with blood and its one-sided callosomarginal region (59). A with the azygos ACA, the
bihemispheric ACA variation is connected with a number of
pathologies, such as infarcts and aneurysms, in the regions where
it supplies (59,60). In the literature, the prevalence of
the bihemispheric ACA variation was found to be 0.20-8.0% (5,27). The
present meta-analysis demonstrated that the prevalence of
bihemishperic ACA was 7.5%, and no significant differences were
found between the prevalence in autopsy (11%) and imaging (7.5%)
studies.
Strongly related to the azygos ACA is an additional
variant where a median ACA is detected, and the third distal ACA
appearance divisions to the distal medial region of one or both
hemispheres (8,10,11).
This variation may be the result of a hypoplastic ACA and the
persistent expansion of the median artery of the corpus callosum
(61). The literature demonstrates a
wide range in the prevalence of median ACA between 1.0 and 35.0%
(5,48). The present study revealed that the
median ACA variant was 5.5%, and there were no notable differences
between the prevalence evaluated in imaging (5%) and autopsy (6%)
articles.
The present meta-analysis had certain limitations
that should be mentioned. The main inadequacy was that its
retrospective character was associated with potential
miscalculations in assembling and understanding the records from
the medical history.
In conclusion, the variations of the ACA's provide
significant blood supply to anatomically valuable regions, such as
the corpus callosum, or frontal lobe and basal ganglia. In
addition, the pathologies behind their appearance, such as infarcts
or aneurysm development, are critical. Thus, the knowledge of the
ACA variations in prevalence may aid clinicians in managing
aneurysms or tumors and other surgical procedures involving these
regions, providing a strong justification for more extensive
prospective clinical investigations.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
GF and VEG conceptualized the study. VEG, CG, AGB,
OF, KM, GF, NT, PS and KNF analyzed the data, and wrote and
prepared the draft of the manuscript. VEG and GF provided critical
revisions. All authors contributed to manuscript revision, and have
read and approved the final version of the manuscript. GF and VEG
confirm the authenticity of all the raw data.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
Use of artificial intelligence tools
During the preparation of this work, AI tools were
used to improve the readability and language of the manuscript or
to generate images, and subsequently, the authors revised and
edited the content produced by the AI tools as necessary, taking
full responsibility for the ultimate content of the present
manuscript.
References
|
1
|
Jinkins JR: 2000 Atlas of Neuroradiologic
Embryology, Anatomy, and Variants. Lippincott Williams and Wilkins,
PA, 2000.
|
|
2
|
Burbank NS and Morris PP: Unique anomalous
origin of the left anterior cerebral artery. AJNR Am J Neuroradiol.
26:2533–2535. 2005.PubMed/NCBI
|
|
3
|
Cavalcanti DD, Albuquerque FC, Silva BF,
Spetzler RF and Preul MC: The anatomy of the callosomarginal
artery: Applications to microsurgery and endovascular surgery.
Neurosurgery. 66:602–610. 2010.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Hussain Z, Corkill RA, Kuker W and Byrne
JV: Distal aneurysms of the unpaired ACA: Embryologic and
therapeutic aspects. Neuroradiology. 47:209–214. 2005.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Kedia S, Daisy S, Mukherjee KK, Salunke P,
Srinivasa R and Narain MS: Microsurgical anatomy of the anterior
cerebral artery in Indian cadavers. Neurol India. 61:117–121.
2013.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Lehecka M, Dashti R, Hernesniemi J,
Niemelä M, Koivisto T, Ronkainen A, Rinne J and Jääskeläinen J:
Microneurosurgical management of aneurysms at the A2 segment of
anterior cerebral artery (proximal pericallosal artery) and its
frontobasal branches. Surg Neurol. 70:232–246. 2008.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Nowinski WL, Thirunavuukarasuu A, Volkau
I, Marchenko Y, Aminah B, Puspitasari F and Runge VM: A
three-dimensional interactive atlas of cerebral arterial variants.
Neuroinformatics. 7:255–264. 2009.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Dimmick SJ and Faulder KC: Normal variants
of the cerebral circulation at multidetector CT angiography.
Radiographics. 29:1027–1043. 2009.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Parmar H, Sitoh YY and Hui F: Normal
variants of the intracranial circulation demonstrated by MR
angiography at 3T. Eur J Radiol. 56:220–228. 2005.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Kapoor K, Singh B and Dewan LI: Variations
in the configuration of the circle of Willis. Anat Sci Int.
83:96–106. 2008.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Niederberger E, Gauvrit JY, Morandi X,
Carsin-Nicol B, Gauthier T and Ferré JC: Anatomic variants of the
anterior part of the cerebral arterial circle at multidetector
computed tomography angiography. J Neuroradiol. 37:139–147.
2010.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Stefani MA, Schneider FL, Marrone AC,
Severino AG, Jackowski AP and Wallace MC: Anatomic variations of
anterior cerebral artery cortical branches. Clin Anat. 13:231–236.
2000.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Kovač JD, Stanković A, Stanković D, Kovač
B and Šaranović D: Intracranial arterial variations: A
comprehensive evaluation using CT angiography. Med Sci Monit.
20:420–427. 2014.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Wells GA, Shea B, O'Connell D, Peterson J,
Welch V, Losos M and Tugwell P: The Newcastle-Ottawa scale (NOS)
for assessing the quality of nonrandomised studies in
meta-analyses. 2014. Available from: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp.
|
|
15
|
Windle BC: The arteries forming the circle
of Willis. J Anat Physiol. 22 (Pt 2):289–293. 1888.PubMed/NCBI
|
|
16
|
Fawcett E and Blachford JV: The circle of
Willis: An examination of 700 specimens. J Anat Physiol. 40 (Pt
1):63.2–70. 1905.PubMed/NCBI
|
|
17
|
Baptista AG: Studies on the arteries of
the brain. ii. The anterior cerebral artery: Some anatomic features
and their clinical implications. Neurology. 13:825–835.
1963.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Jain KK: Some observations on the anatomy
of the middle cerebral artery. Can J Surg. 7:134–139.
1964.PubMed/NCBI
|
|
19
|
Fisher CM: The Circle of Willis:
Anatomical Variations. Annals of Vasc Dis. 2:99–105. 1965.
|
|
20
|
LeMay M and Gooding CA: The clinical
significance of the azygos anterior cerebral artery (A.C.A.). Am J
Roentgenol Radium Ther Nucl Med. 98:602–610. 1966.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Wollschlaeger G, Wollschlaeger PB, Lucas
FV and Lopez VF: Experience and result with postmortem cerebral
angiography performed as routine procedure of the autopsy. Am J
Roentgenol Radium Ther Nucl Med. 101:68–87. 1967.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Ring BA and Waddington MM:
Roentgenographic anatomy of the pericallosal arteries. Am J
Roentgenol Radium Ther Nucl Med. 104:109–118. 1968.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Dunker RO and Harris AB: Surgical anatomy
of the proximal anterior cerebral artery. J Neurosurg. 44:359–367.
1976.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Tulleken CA: A study of the anatomy of the
anterior communicating artery with the aid of the operating
microscope. Clin Neurol Neurosurg. 80:169–173. 1978.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Ozaki T, Handa H, Tomimoto K and Hazama F:
Anatomical variations of the arterial system of the base of the
brain. Nihon Geka Hokan. 46:3–17. 1977.PubMed/NCBI
|
|
26
|
Perlmutter D and Rhoton AL Jr:
Microsurgical anatomy of the distal anterior cerebral artery. J
Neurosurg. 49:204–228. 1978.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Huber P, Braun J, Hirschmann D and Agyeman
JF: Incidence of berry aneurysms of the unpaired pericallosal
artery: Angiographic study. Neuroradiology. 19:143–147.
1980.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Kwak R, Niizuma H, Hatanaka M and Suzuki
J: Anterior communicating artery aneurysms with associated
anomalies. J Neurosurg. 52:162–164. 1980.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Kayembe KN, Sasahara M and Hazama F:
Cerebral aneurysms and variations in the circle of Willis. Stroke.
15:846–850. 1984.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Gomes FB, Dujovny M, Umansky F, Berman SK,
Diaz FG, Ausman JI, Mirchandani HG and Ray WJ: Microanatomy of the
anterior cerebral artery. Surg Neurol. 26:129–141. 1986.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Marinković S, Milisavljević M and
Marinković Z: Branches of the anterior communicating artery.
Microsurgical anatomy. Acta Neurochir (Wien). 106:78–85.
1990.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Ogawa A, Suzuki M, Sakurai Y and Yoshimoto
T: Vascular anomalies associated with aneurysms of the anterior
communicating artery: Microsurgical observations. J Neurosurg.
72:706–709. 1990.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Nathal E, Yasui N, Sampei T and Suzuki A:
Intraoperative anatomical studies in patients with aneurysms of the
anterior communicating artery complex. J Neurosurg. 76:629–634.
1992.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Van der Zwan A, Hillen B, Tulleken CA,
Dujovny M and Dragovic L: Variability of the territories of the
major cerebral arteries. J Neurosurg. 77:927–940. 1992.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Sanders WP, Sorek PA and Mehta BA:
Fenestration of intracranial arteries with special attention to
associated aneurysms and other anomalies. AJNR Am J Neuroradiol.
14:675–680. 1993.PubMed/NCBI
|
|
36
|
Macchi C, Catini C, Federico C, Gulisano
M, Pacini P, Cecchi F, Corcos L and Brizzi E: Magnetic resonance
angiographic evaluation of circulus arteriosus cerebri (circle of
Willis): A morphologic study in 100 human healthy subjects. Ital J
Anat Embryol. 101:115–123. 1996.PubMed/NCBI
|
|
37
|
Serizawa T, Saeki N and Yamaura A:
Microsurgical anatomy and clinical significance of the anterior
communicating artery and its perforating branches. Neurosurgery.
40:1211–1216. 1997.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Avci E, Fossett D, Erdogan A, Egemen N,
Attar A and Aslan M: Perforating branches of the anomalous anterior
communicating complex. Clin Neurol Neurosurg. 103:19–22.
2001.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Kulenović A, Dilberović F and Ovcina F:
Variation in the flow and branching of the anterior and middle
cerebral arteries. Med Arh. 57:3–5. 2003.PubMed/NCBI
|
|
40
|
Paul S and Mishra S: Variations of the
anterior cerebral artery in human cadavers: A dissection study. J
Anat Soc India. 53:15–16. 2004.
|
|
41
|
Ugur HC, Kahilogullari G, Coscarella E,
Unlu A, Tekdemir I, Morcos JJ, Elhan A and Baskaya MK: Arterial
vascularization of primary motor cortex (precentral gyrus). Surg
Neurol. 64 (Suppl 2):S48–S52. 2005.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Tao X, Yu XJ, Bhattarai B, Li TH, Jin H,
Wei GW, Ming JS, Ren W and Jiong C: Microsurgical anatomy of the
anterior communicating artery complex in adult Chinese heads. Surg
Neurol. 65:155–161. 2006.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Uchino A, Nomiyama K, Takase Y and Kudo S:
Anterior cerebral artery variations detected by MR angiography.
Neuroradiology. 48:647–652. 2006.PubMed/NCBI View Article : Google Scholar
|
|
44
|
Ugur HC, Kahilogullari G, Esmer AF, Comert
A, Odabasi AB, Tekdemir I, Elhan A and Kanpolat Y: A neurosurgical
view of anatomical variations of the distal anterior cerebral
artery: An anatomical study. J Neurosurg. 104:278–284.
2006.PubMed/NCBI View Article : Google Scholar
|
|
45
|
Bharatha A, Aviv RI, White J, Fox AJ and
Symons SP: Intracranial arterial fenestrations: Frequency on CT
angiography and association with other vascular lesions. Surg
Radiol Anat. 30:397–401. 2008.PubMed/NCBI View Article : Google Scholar
|
|
46
|
Kahilogullari G, Comert A, Arslan M, Esmer
AF, Tuccar E, Elhan A, Tubbs RS and Ugur HC: Callosal branches of
the anterior cerebral artery: An anatomical report. Clin Anat.
21:383–388. 2008.PubMed/NCBI View Article : Google Scholar
|
|
47
|
Saidi H, Kitunguu PK and Ogeng'O JA:
Variant anatomy of the anterior cerebral artery in adult brains.
Afr J Neurol Scie. 27:97–105. 2008.
|
|
48
|
Zurada A, Gielecki J, Tubbs RS, Loukas M,
Cohen-Gadol AA, Chlebiej M, Maksymowicz W, Nowak D, Zawiliński J
and Michalak M: Three-dimensional morphometry of the A2 segment of
the anterior cerebral artery with neurosurgical relevance. Clin
Anat. 23:759–769. 2010.PubMed/NCBI View Article : Google Scholar
|
|
49
|
Nordon DG and Rodrigues OF: Variations in
the brain circulation-the circle of Willis. J Morphol Sci.
29:243–247. 2012.
|
|
50
|
Swetha B: Anatomic features of distal
anterior cerebral artery supply on corpus callosum: A detailed
study on 140 cerebral hemispheres. J Neurol Sci (Turkish).
29:46–56. 2012.
|
|
51
|
Gunnal S: Variations of anterior cerebral
artery in human cadavers. Neurology Asia. 18:249–259. 2013.
|
|
52
|
Hamidi C, Bükte Y, Hattapoğlu S, Ekici F,
Tekbaş G, Önder H, Gümüş H and Bilici A: Display with 64-detector
MDCT angiography of cerebral vascular variations. Surg Radiol Anat.
35:729–736. 2013.PubMed/NCBI View Article : Google Scholar
|
|
53
|
Stefani MA, Schneider FL, Marrone ACH and
Severino AG: Influence of the gender on cerebral vascular diameters
observed during the magnetic resonance angiographic examination of
willis circle. Braz Arch Biol Technol. 56:45–52. 2013.
|
|
54
|
Cilliers K, Vorster W and Page BJ: The
anatomical variation of the circulus arteriosus cerebri in a
cadaver cohort representing the population dynamics of the Western
Cape. Br J Neurosurg. 32:61–67. 2018.PubMed/NCBI View Article : Google Scholar
|
|
55
|
Wan-Yin S, Ming-Hua L, Bin-Xian G,
Yong-Dong L and Hua-Qiao T: Azygous anterior cerebral artery and
associated aneurysms: Detection and identification using
3-dimensional time-of-flight magnetic resonance angiography. J
Neuroimaging. 24:18–22. 2014.PubMed/NCBI View Article : Google Scholar
|
|
56
|
López-Sala P, Alberdi N, Mendigaña M,
Bacaicoa MC and Cabada T: Anatomical variants of anterior
communicating artery complex. A study by computerized tomographic
angiography. J Clin Neurosci. 80:182–187. 2020.PubMed/NCBI View Article : Google Scholar
|
|
57
|
Nutik S and Dilenge D: Carotid-anterior
cerebral artery anastomosis. Case report. J Neurosurg. 44:378–382.
1976.PubMed/NCBI View Article : Google Scholar
|
|
58
|
Huh JS, Park SK, Shin JJ and Kim TH:
Saccular aneurysm of the azygos anterior cerebral artery: Three
case reports. J Korean Neurosurg Soc. 42:342–345. 2007.PubMed/NCBI View Article : Google Scholar
|
|
59
|
Tahir RA, Haider S, Kole M, Griffith B and
Marin H: Anterior cerebral artery: Variant anatomy and pathology. J
Vasc Interv Neurol. 10:16–22. 2019.PubMed/NCBI
|
|
60
|
Lasjaunias P, Brugge KG and Berenstein A:
Surgical neuroangiography. Vol 3. Springer, Berlin, 2006.
|
|
61
|
Pekcevik Y, Hasbay E and Oncel D: Colloid
cyst of the third ventricle associated with anterior cerebral
artery trifurcation and agenesis of the corpus callosum: Findings
on MRI and CT angiography. Pediatr Radiol. 42:1130–1133.
2012.PubMed/NCBI View Article : Google Scholar
|