Introduction
Birth asphyxia and hypoxic ischemic syndrome a very
consequential illnesses that are linked to elevated rates of infant
mortality and significant neurological consequences (1). The syndrome is a topic of contention in
scientific literature, with numerous writers attempting to enhance
its definition throughout time, resulting in increased precision,
but also in increased complexity. The prevalence of neonatal
asphyxia has experienced a significant increase in recent years,
including a spectrum of severity from moderate to severe
manifestations. Consequently, it has emerged as a fundamental
challenge encountered within neonatology units (2). The phrase ‘birth asphyxia’ is employed
to describe a situation in which a baby exhibits poor Apgar scores,
notable metabolic acidosis detected in umbilical cord blood
samples, and a modified neurological examination (with or without
EEG correspondence) in the absence of any indications of other
etiologies of encephalopathy (3).
Asphyxia during the perinatal period leads to the
formation of hypoxic cerebral lesions, which have a marked impact
on the cognitive, neurological and motor development of neonates.
Defining the etiology of hypoxia is crucial for effectively
treating the cause and achieving a positive outcome.
The etiology of hypoxic ischemic syndrome at birth
is multifactorial, with both intrapartum and antenatal factors.
When affected, each link of the pathological chain causes the onset
of a mild or more severe form, thereby the need to investigate the
most accessible parts of the process. The diagnosis of hypoxic
ischemic encephalopathy is made on clinical criteria (Sarnat
classification), as well as on laboratory tests (evidence of
metabolic acidosis, multiple organ damage) and brain imaging (EEG
and MRI) (4). The treatment of
hypoxic ischemic encephalopathy should be prompt to overcome the
onset of permanent neurological sequelae. It has been extensively
studied over the last decade, leading to the identification of
extensive neuroprotective strategies, such as controlled
hypothermia or the use of several molecules, such as erythropoietin
and other molecules still under investigation (5).
The identification of pathogenic processes occurring
during gestation has been demonstrated by the study of placental
pathology. The prompt identification of the hypoxic-ischemic lesion
is crucial in the context of encephalopathy to facilitate timely
intervention. Despite extensive research conducted on maternal risk
factors and birth events associated with prenatal hypoxia or
cerebral palsy, there are a limited number of studies available
that have established direct associations between placental
histological signs and neurological impairment (6).
The histological analysis of the placenta is often
conducted primarily in instances of challenging births, to identify
distinct alterations that are linked to a higher incidence of
infant mortality. In recent years, there has been a growing
scientific interest in investigating the association between the
diagnosis of hypoxic ischemic encephalopathy and abnormalities in
the placenta. The Amsterdam Placental Workshop Group Criteria were
formulated in 2016 to establish a uniform categorization system for
placental lesions (7).
Perinatal asphyxia is linked to placental
abnormalities that affect blood flow to the fetus. The identified
lesions on the umbilical cord included issues, such as damaged
velamentous vessels, cord rupture, hypercoiled chords and cord
hematoma. Additionally, there were instances of chorioamnionitis
accompanied by fetal vasculitis and fetal vascular malperfusion
(8,9).
In the present study, it was hypothesized that by
carefully examining a single ‘key’ component, such as the placenta,
the identification of etiological associations between placental
abnormalities and the occurrence of birth asphyxia would be
possible. In order to provide a rapid tool for stratifying the
probable future evolution of newborns, the present study aimed to
identify and characterize particular macroscopic and microscopic
placental damage in hypoxic neonates.
Subjects and methods
Subject information
An observational, prospective, non-interventional
study was undertaken at the ‘Filantropia’ Clinical Hospital in
Bucharest, Romania, spanning a duration of 3 years from 2020 to
2022. The research was conducted with the requisite authorization
from the Ethics Council of ‘Filantropia’ Clinical Hospital and
according to the privacy protocols established for the
participating patients. Prior to the inclusion of the mother and
newborn in the study, the parents or legal guardians provided their
signature on an informed consent agreement. The research was
carried out following the principles outlined in the Declaration of
Helsinki on Human Rights.
Relevant maternal information, including the social,
medical and family history of the mother, was gathered in
conjunction with data about the newborn. These data encompassed
various aspects, such as fetal heartbeat during labor, gestational
age, delivery type, birth weight and sex. Additionally, data from
the clinical examination of the newborns, including changes
associated with perinatal hypoxia and Apgar score, were also
provided. In addition, laboratory findings were documented,
including hemograms, metabolic parameters, pH and acid-base balance
parameters, all of which were collected in a dynamic manner.
However, the database was updated with placental histopathology
examination data, including both micro- and macroscopic images.
Examination procedures
The investigation involved a macroscopic examination
of the placenta, umbilical cord and membranes. The macroscopic
lesions were from predefined categories: In the case of the
placenta, weight and appearance; in the case of the umbilical cord,
length and appearance, insertion; and in the case of the membranes,
color and appearance. The weight of the placenta was measured
within the initial hour following delivery, after the removal of
the membranes and umbilical cord. The assessment of the umbilical
cord encompassed various aspects, such as its length, the location
of its insertion about the center or borders of the placenta, the
existence or absence of a hypercoiled (≥3 coils per 10 cm) or
hypocoiled (1 coil per 10 cm) look, and the identification of a
single umbilical artery. The membranes were described as having an
opaque look and colour and were inserted in a circumvallate or
circummarginal manner.
An experienced pathologist conducted the placental
examination. On fresh placenta sections, the microscopic
examination was performed before they were embedded in paraffin and
stained with hematoxylin and eosin (with Mayer's hematoxylin
solution, supplied by Merck, for a duration of 15 min at room
temperature). A total of five samples (1.5-2-cm-thick) were
obtained for microscopic examination: One from the membranes, one
from the umbilical cord and three from the placental parenchyma. In
the cases in which the placenta examination could not be conducted
immediately after birth, the samples were refrigerated at 4˚C, for
a maxim period of 24 h. During the examination, the microscope used
was Zeiss Axioscope 5 and the images were captured with Zeiss
Axiocam 208 (Zeiss AG). The classification included the primary six
pre-established classifications of injuries, according to the
Amsterdam Criteria: Maternal vascular malperfusion, fetal vascular
malperfusion, chronic villitis of unknown etiology, delayed villous
maturation, chorioamnionitis and abruption. The following
abnormalities were associated with maternal vascular malperfusion:
Placental hypoplasia (weight below the 10th percentile for
gestational age), villi abnormalities (hypoplasia, increased fibrin
deposits at villous levels, necrosis) and placental infarction.
Fetal vascular malperfusion includes both segmental
and generalized alterations, which can appear as thrombosis with or
without occlusive thrombi, avascular villi, intramural fibrin
deposits in the major veins and stromal-vascular karyorrhexis.
Chronic villitis of unknown etiology that associates vascular
obstruction, and avascular villi was diagnosed as the presence of
inflammation that affects >30% of the distal villi. Delayed
villous maturation is represented by villous maturation
inappropriately immature for gestational age across the peripheral
villi, which includes at least 30% of a section. The defining
characteristic of chorioamnionitis is the presence of inflammatory
cells inside the layers of chorion membranes. This condition is
sometimes accompanied by necrosis and acute vasculitis at certain
levels of the umbilical cord and chorion. The clinical
manifestation of abruptio placentae was characterized by the
observation of retroplacental hemorrhage. Placentas with distinct
lesions across the six categories were excluded from the analysis.
The Zeiss Axioscope 5 microscope (Zeiss AG) was used to analyze all
placental samples.
Study groups and criteria
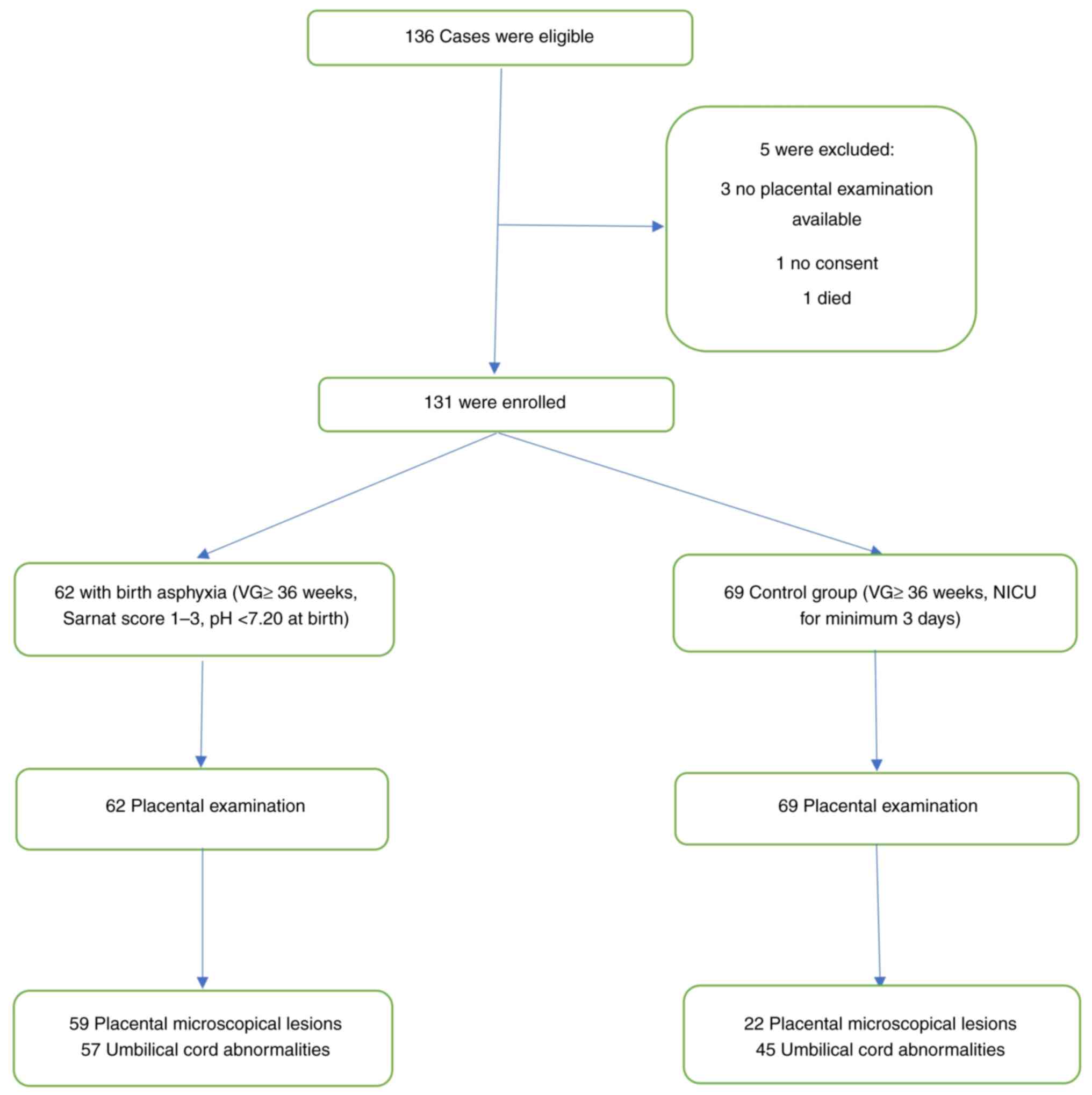
The study group included 62 newborns who had
perinatal asphyxia, with a gestational age >36 weeks and a
diagnosis of hypoxia at birth (mild, moderate and severe). The
exclusion criteria were the following: Patients who had viral
intrauterine infections, congenital abnormalities, chromosomal
anomalies and twin pregnancies. The control group consisted of 69
newborns with a gestational age >36 weeks who required neonatal
intensive care for a minimum of 3 days for any other pathology,
excluding hypoxia. The exclusion criteria for the control group
were the following: Congenital abnormalities, chromosomal anomalies
or were unable to undergo placental examination. Placental
examinations were conducted in all patients. The diagnosis of birth
asphyxia in newborns was established with a comprehensive
neurological clinical examination and subsequently categorized
using the Sarnat score, which ranged from 1 (mild) to 3 (severe).
The blood collected from the clamped umbilical cord immediately
after birth had a pH value <7.20. A complete acid-base study was
conducted on the collected blood samples, including measurements of
pH, pCO2, pO2 and base deficit. Patients who
were excluded from the study did not match the specified inclusion
criteria. All data are summarized in Fig. 1.
Statistical analysis
SPSS 25.0 for Windows (IBM Corp.) was used to
statistically analyze the recorded data. The Chi-squared test or an
unpaired t-test were employed for independent sample analyses,
whereas Mann-Whitney tests were used to analyze non-parametric
variables. Fisher's test was also applied for each variable that
had a count of ≤5. A value of P<0.05 was considered to indicate
a statistically significant difference.
Results
A total of 136 patients who met the inclusion
criteria were enrolled; 5 patients were excluded. In addition, 36
(27.48%) of the patients were males. The incidence of cesarean
section was found to be 28.24%, with a total of 37 neonates being
born with emergency cesarean section.
Cardiotocography (CTG) was used to continuously
monitor the mothers during labor. The recorded changes included
fetal bradycardia, fetal tachycardia and variability. Of note,
60.3% (78 pregnancies) exhibited CTG abnormalities, with 51
pregnancies (82.3%) in the asphyxia group (P=0.01) and 27
pregnancies (39.1%) in the control group. Tachycardia was observed
in 18 cases (29.0%) (P=0.01) and bradycardia (P=0.01) in 23
neonates (37.1%) with asphyxia. In addition, lower variability was
observed in 10 neonates (16.1%) with hypoxia (P=NS). Within the
control group, 12 cases (17.4%) experienced fetal bradycardia, 7
cases (10.1%) experienced fetal tachycardia, and 8 cases (11.6%)
exhibited lower variability.
Complicated pregnancies accounted for a substantial
portion of the cases, specifically 92 (70.2%). Among the 62
neonates with asphyxia, 56 (90.3%) were born from pregnancies with
complications (P=0.01), whereas in the control group, only 36
(52.2%) had problems. Out of the numerous medical conditions
related to pregnancy, 25 cases (19.0%) were attributed to
pregnancy-induced hypertension, with 18 cases (29.0%) occurring
within the study group (P=0.01). Gestational diabetes was present
in 33 (25.2%) cases. Among these, 16 (25.8%) neonates had asphyxia
(P=NS), while 17 (24.6%) were in the control group. In addition,
there were 14 cases (10.7%) of preeclampsia; in the study group,
there were 11 (17.7%) cases (P=0.02), while in the control group,
there were 3 (4.3%). Additionally, pregnancy cholestasis was
present in 20 cases (15.3%), 11 (17.7%) with asphyxia (P=NS), and 9
(13.0%) in the control group. In addition, 5 (3.8%) patients were
under psychiatric treatment at the time of birth, 4 (6.4%) from the
study group (P=NS), and 1 (1.4%) from the control group. The
features of the patients are presented in Table I.
 | Table IPatients characteristics. |
Table I
Patients characteristics.
| Characteristic | Birth asphyxia
(n=62) | Control (n=69) | P-value |
|---|
| Gestational age
(weeks) | 37.83±1.4 | 36.58±3.1 | NS |
| Birth weight (g) | 3,030.95±602.62 | 2,743.33±891.20 | 0.02 |
| Cesarean section, n
(%) | | | 0.01 |
|
Yes | 25 (40.3%) | 12 (17.4%) | |
|
No | 37 (59.7%) | 57 (82.5%) | |
| Median ventilation
duration (days) | 3.90±3.03 | 2.57±2.76 | 0.01 |
| Length of hospital
stay (days) | 17.26±11.7 | 13.38±7.2 | 0.03 |
| Male sex, n (%) | | | 0.03 |
|
Yes | 22 (35.5%) | 14 (20.3%) | |
|
No | 40 (64.5%) | 55 (79.7%) | |
| CTG abnormalities, n
(%) | | | 0.01 |
|
Yes | 51 (82.3%) | 27 (39.1%) | |
|
No | 11 (17. 7%) | 42 (60.9%) | |
| Tachycardia, n
(%) | | | 0.01 |
|
Yes | 18 (29.0%) | 7 (10.1%) | |
|
No | 44 (71.0%) | 62 (89.9%) | |
| Bradycardia, n
(%) | | | 0.01 |
|
Yes | 23 (37.1%) | 12 (17.4%) | |
|
No | 39 (62.9%) | 57 (82.5%) | |
| Lower variability,
n (%) | | | NS |
|
Yes | 10 (16.1%) | 8 (11.6%) | |
|
No | 52 (83.9%) | 61 (88.4%) | |
| Complicated
pregnancies, n (%) | | | 0.01 |
|
Yes | 56 (90.3%) | 36 (52.2%) | |
|
No | 6 (9.7%) | 33 (47.8%) | |
| Pregnancy-induced
hypertension, n (%) | | | 0.01 |
|
Yes | 18 (29.0%) | 7 (10.1%) | |
|
No | 44 (71.0%) | 62 (89.9%) | |
| Gestational
diabetes, n (%) | | | NS |
|
Yes | 16 (25.8%) | 17 (24.6%) | |
|
No | 46 (74.2%) | 52 (75.4%) | |
| Preeclampsia, n
(%) | | | 0.02 |
|
Yes | 11 (17.7%) | 3 (4.3%) | |
|
No | 51 (82.3%) | 66 (95.7%) | |
| Pregnancy
cholestasis, n (%) | | | NS |
|
Yes | 11 (17.7%) | 9 (13.0%) | |
|
No | 51 (82.3%) | 60 (87.0%) | |
| Under psychiatric
treatment, n (%) | | | NS |
|
Yes | 4 (6.4%) | 1(1.4%) | |
|
No | 58 (93.6%) | 68 (98.6%) | |
| Fetal growth
restriction, n (%) | | | NS |
|
Yes | 21 (33.9%) | 16 (23.2%) | |
|
No | 41 (66.1%) | 53 (76.8%) | |
| APGAR at 5 min | 4.92±1.5 | 5.94±1.42 | 0.01 |
| Umbilical cord
pH | 7.05±0.09 | 7.23±0.07 | 0.01 |
| Umbilical cord
pCO2 (mmHg) | 64.2±0.07 | 48.5±0.05 | 0.01 |
| Umbilical cord base
deficit (mmol/l) | -13.4±0.04 | -5.0±0.02 | 0.01 |
| pH at 1 h of
life | 7.12±0.07 | 7.27±0.02 | 0.01 |
| pCO2
(mmH) at 1 h of life | 56.5±0.04 | 40.4±0.03 | 0.01 |
| Base deficit
(mmol/l) at 1 h of life | -8.2±0.03 | -2.3±0.06 | 0.02 |
| SARNAT 1,
percentage | 23.5% | 0 | |
| SARNAT 2,
percentage | 26.5% | 0 | |
| SARNAT 3,
percentage | 13.6% | 0 | |
Additionally, it is important to note that the
control group consisted of neonates who had been diagnosed with
transient tachypnea of the newborn 27 (38%), early neonatal sepsis
15 (23%), hypoglycemia 14 (20%), pneumonia 9 (14%) and meconium
aspiration syndrome 4 (5%).
Newborns with perinatal asphyxia exhibited a lower
umbilical cord pH value, measuring 7.05 (P=0.01). Additionally,
they had a smaller umbilical cord base deficit of -13.4 mmol/l
(P=0.01), a higher umbilical cord pCO2 of 64.2 mmHg
(P=0.01) and greater median ventilation days (P=0.01). It is
important to note that the duration of hospital stay was
significantly longer in individuals with asphyxia compared to the
control group, with a P-value of.03 (Table I).
The macroscopic examination records of the placenta
contained a number of indicators, such as placental weight,
membrane aspect, appearance and implantation of the umbilical cord.
The birth asphyxia group exhibited a significantly increased
placental weight compared to the control group (P=0.01).
Furthermore, 57 neonates (91.9%) with hypoxia exhibited umbilical
cord anomalies, including: Umbilical knot, 10 neonates (16.1%);
unique umbilical artery, 23 neonates (37.1%); abnormal insertion,
18 neonates (29%); hypercoiled, 4 neonates (6.5%); and hypocoiled,
2 neonates (3.2%). Furthermore, the occurrence of perinatal hypoxia
was found to be linked with alterations in the umbilical cord,
namely the presence of knots (P=0.01) and the existence of a
distinct umbilical artery (P=0.01). These data are presented in
Table II.
 | Table IIPlacental macroscopic examination
data and umbilical cord abnormalities. |
Table II
Placental macroscopic examination
data and umbilical cord abnormalities.
| Parameter | Birth asphyxia
(n=62) | Control (n=69) | P-value |
|---|
| Placental weight
(g) | 453.62±87.58 | 405.52±138.43 | 0.01 |
| Umbilical knot, n
(%) | | | 0.01 |
|
Yes | 10 (16.1%) | 2 (2.9%) | |
|
No | 52 (83.9%) | 67 (97.1%) | |
| Unique umbilical
artery, n (%) | | | 0.01 |
|
Yes | 23 (37.1%) | 12 (17.4%) | |
|
No | 39 (62.9%) | 57 (82.6%) | |
| Insertion anomalies
of the umbilical cord, n (%) | | | NS |
|
Yes | 18 (29.0%) | 24 (34.8%) | |
|
No | 44 (71.0%) | 45 (65.2%) | |
| Hypercoiled, n
(%) | | | NS |
|
Yes | 4 (6.5%) | 7 (10.1%) | |
|
No | 58 (93.5%) | 62 (89.9%) | |
| Hypocoiled, n
(%) | | | NS |
|
Yes | 2 (3.2%) | 5 (7.2%) | |
|
No | 60 (96.8%) | 62 (89.8%) | |
| Normal, n (%) | | | 0.01 |
|
Yes | 5 (8.1%) | 19 (27.5%) | |
|
No | 57 (91.9%) | 50 (72.5%) | |
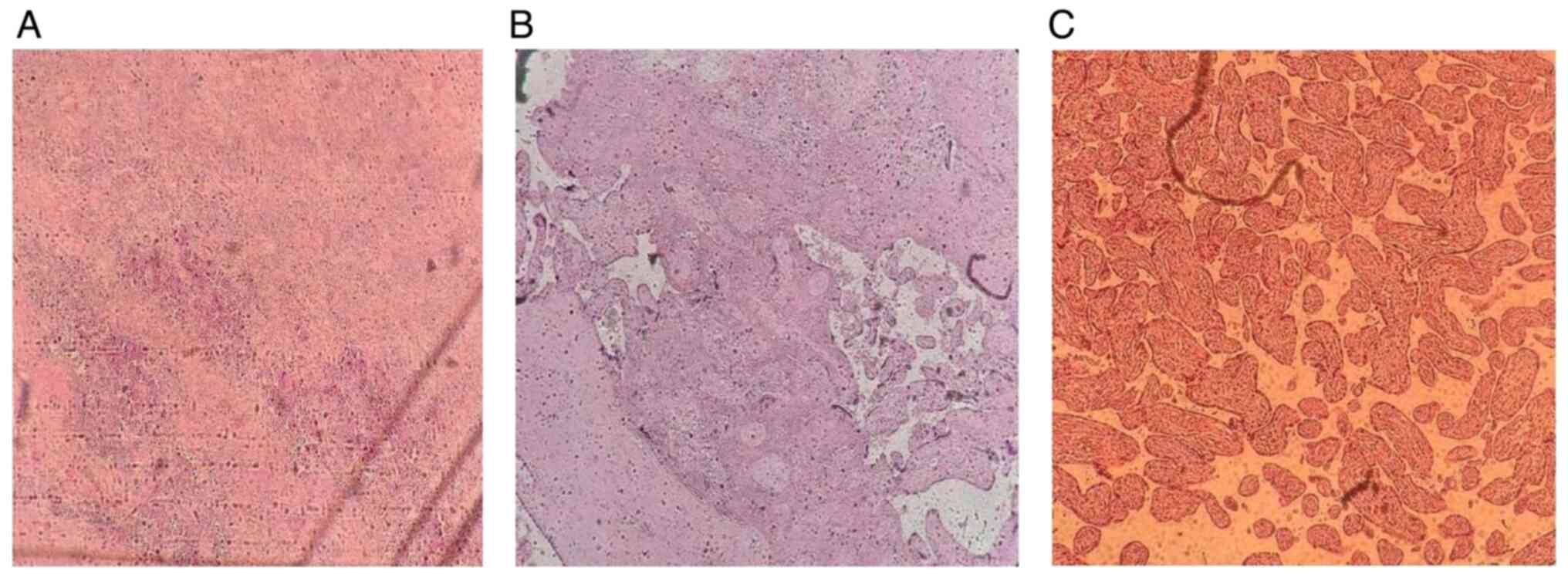
Placental microscopic changes were observed in 81
(61.8%) of cases, while 50 (38.2%) were normal. The most commonly
identified lesions in birth asphyxia were chronic from the maternal
vascular malperfusion [15 (24.2%)] and fetal vascular malperfusion
[11 (17.7%)] class. In the control group, the normal aspect was
predominant. Furthermore, the group with perinatal asphyxia
exhibited a higher prevalence of chronic villitis of unknown
causes, with 10 cases (16.2%) out of the 62 cases, compared with
the control group with 3 cases (4.2%) out of the 69 cases. In
instances of delayed villous maturation, similar findings were
observed, with 12 cases (19.4%) out of 62 and 4 cases (5.6%) out of
69 cases. These results highlight a statistical association between
these lesions and the occurrence of hypoxic lesions at birth,
chronic villitis of unknown cause (P=0.01), and delayed villous
maturation (P=0.01) (Table III).
Some of the identified lesions are illustrated in Fig. 2.
 | Table IIIPlacental microscopic lesions. |
Table III
Placental microscopic lesions.
| Placental
lesions | Birth asphyxia
(n=62) (%) | Control (n=69)
(%) | P-value |
|---|
| MVM, n (%) | | | 0.01 |
|
Yes | 15 (24.2) | 4 (5.8) | |
|
No | 47 (75.8) | 65 (94.2) | |
| FVM, n (%) | | | 0.01 |
|
Yes | 11 (17.7) | 2 (2.9) | |
|
No | 51 (82.3) | 67 (97.1) | |
| VUE, n (%) | | | 0.03 |
|
Yes | 10 (16.1) | 3 (4.3) | |
|
No | 52 (83.9) | 66 (65.7) | |
| Delayed villous
maturation, n (%) | | | 0.03 |
|
Yes | 12 (19.4) | 4 (5.8) | |
|
No | 50 (80.6) | 65 (94.2) | |
| Chorioamnionitis, n
(%) | | | NS |
|
Yes | 5 (8.1) | 9 (13.0) | |
|
No | 57 (91.9) | 60 (87.0) | |
| Abruption, n
(%) | | | 0.05 |
|
Yes | 6 (9.7) | 1 (1.4) | |
|
No | 56 (81.3) | 68 (98.6) | |
| No lesions, n
(%) | | | 0.01 |
|
Yes | 3 (4.8) | 47 (68.1) | |
|
No | 59 (95.2) | 22 (31.9) | |
Out of the total 7 cases of abruption, 6 (9.6%)
cases were assigned to the study group, while 1 (1.4%) case was
assigned to the control group. Due to its small number, the data
did not demonstrate a strong significant statistical association
between the two variables (P=0.05). In addition, there were no
differences in the two groups regarding chorioamnionitis (P=NS).
These data are presented in Table
III.
A few other lesions were excluded during the
placental histopathological examination as they could not be
classified based on the criteria, and the placental
histopathological examination (0.7%) did not reveal any
chorangiosis. Moreover, in the instance of the presence of multiple
simultaneous lesions [3 cases (2.2%)], they were classified
according to the extent of the most extensive lesions
(>30%).
The analysis of placental changes in relation to the
severity of hypoxia revealed significant associations between
maternal (P=0.01) or fetal (P=0.01) vascular malperfusion type
lesions and severe perinatal asphyxia. In cases of moderate
asphyxia, both fetal vascular malperfusion (P=0.01) lesions, and
abruptio-type (P=0.02) lesions were observed. Additionally, the
presence of chronic villitis of unknown etiology (P=0.01) and
delayed villous maturation (P=0.01) type lesions were associated
with mild perinatal asphyxia. Table
IV provides a summary of all the statistical associations that
have been found between the identified placental lesions and the
degree of prenatal hypoxia.
 | Table IVPlacental microscopic lesions in
those with mild, moderate and severe asphyxia, and the
controls. |
Table IV
Placental microscopic lesions in
those with mild, moderate and severe asphyxia, and the
controls.
| A, Those with mild
asphyxia vs. the controls |
|---|
| Placental
lesions | Mild asphyxia
(n=23) (%) | Control (n=69)
(%) | P-value |
|---|
| MVM, n (%) | | | NS |
|
Yes | 1 (4.3) | 4 (5.8) | |
|
No | 22 (95.7) | 65 (94.2) | |
| FVM, n (%) | | | NS |
|
Yes | 0 (0) | 2 (2.9) | |
|
No | 23(100) | 67 (97.1) | |
| VUE, n (%) | | | 0.01 |
|
Yes | 7 (30.4) | 3 (4.3) | |
|
No | 16 (69.6) | 66 (65.7) | |
| Delayed villous
maturation, n (%) | | | 0.01 |
|
Yes | 10 (43.5) | 4 (5.8) | |
|
No | 13 (56.5) | 65 (94.2) | |
| Chorioamnionitis, n
(%) | | | |
|
Yes | 1 (4.3) | 9 (13.0) | |
|
No | 22 (95.7) | 60 (87.0) | |
| Abruption, n
(%) | | | NS |
|
Yes | 1 (4.3) | 1 (1.4) | |
|
No | 22 (95.7) | 68 (98.6) | |
| Normal, n (%) | | | 0.01 |
|
Yes | 3 (13.0) | 47 (68.1) | |
|
No | 20 (87.0) | 22 (31.9) | |
| B, Those with
moderate asphyxia vs. the controls |
| Placental
lesions | Moderate asphyxia
(n=16) (%) | Control (n=69)
(%) | P-value |
| MVM, n (%) | | | NS |
|
Yes | 3 (18.8) | 4 (5.8) | |
|
No | 13 (81.2) | 65 (94.2) | |
| FVM, n (%) | | | 0.01 |
|
Yes | 4 (25.0) | 2 (2.9) | |
|
No | 12(75) | 67 (97.1) | |
| VUE, n (%) | | | NS |
|
Yes | 2 (12.5) | 3 (4.3) | |
|
No | 14 (87.5) | 66 (65.7) | |
| Delayed villous
maturation, n (%) | | | NS |
|
Yes | 2 (12.5) | 4 (5.8) | |
|
No | 14 (87.5) | 65 (94.2) | |
| Chorioamnionitis, n
(%) | | | NS |
|
Yes | 2 (12.5) | 9 (13.0) | |
|
No | 14 (87.5) | 60 (87.0) | |
| Abruption, n
(%) | | | 0.02 |
|
Yes | 3 (18.8) | 1 (1.4) | |
|
No | 13 (81.2) | 68 (98.6) | |
| Normal, n (%) | | | 0.01 |
|
Yes | 0 (0) | 47 (68.1) | |
|
No | 16(100) | 22 (31.9) | |
| C, Those with
severe asphyxia vs. the controls |
| Placental
lesions | Severe asphyxia
(n=23) (%) | Control (n=69)
(%) | P-value |
| MVM, n (%) | | | 0.01 |
|
Yes | 11 (47.8) | 4 (5.8) | |
|
No | 12 (52.2) | 65 (94.2) | |
| FVM, n (%) | | | 0.01 |
|
Yes | 7 (30.4) | 2 (2.9) | |
|
No | 16 (69.6) | 67 (97.1) | |
| VUE, n (%) | | | NS |
|
Yes | 1 (4.3) | 3 (4.3) | |
|
No | 22 (95.7) | 66 (65.7) | |
| Delayed villous
maturation, n (%) | | | NS |
|
Yes | 0 (0) | 4 (5.8) | |
|
No | 23(100) | 65 (94.2) | |
| Chorioamnionitis, n
(%) | | | NS |
|
Yes | 2 (8.7) | 9 (13.0) | |
|
No | 21 (91.3) | 60 (87.0) | |
| Abruption, n
(%) | | | NS |
|
Yes | 2 (8.7) | 1 (1.4) | |
|
No | 21 (91.3) | 68 (98.6) | |
| Normal, n (%) | | | 0.01 |
|
Yes | 0 (0) | 47 (68.1) | |
|
No | 23(100) | 22 (31.9) | |
Discussion
The present study emphasized that a careful
examination of both the umbilical cord and the placenta is critical
to a better understanding of the multifactorial etiology of
perinatal asphyxia. Based on the findings of the present study, the
presence of both placental changes and the presence of hypoxic
lesions at birth were associated with the presence of placental
changes, as well as the umbilical cord.
The results highlight the importance of a placental
examination in birth asphyxia, as also revealed by other studies,
such as the study by Nielsen et al (10). Previous studies have revealed that
both macroscopic and microscopic examinations are associated with
hypoxic brain lesions (11-13).
In the present study, the most common placental microscopic changes
in perinatal asphyxia were from the maternal and fetal vascular
malperfusion categories, unlike the control group where the
majority of the placentas were normal. According to the
classification of placental lesions, it can be concluded that the
factors that determined the appearance of hypoxic lesions were
chronic; these results were similar to those in the study by
Bingham et al (14).
The results presented herein support the statement
that hypoxic ischemic lesions are associated with both macro- and
microscopic placental lesions and changes in the umbilical cord. As
previously mentioned by Wintermark et al (9), the following pathological lesions of
the umbilical cord were highlighted in the present study:
Circumvallated membranes, single umbilical artery, hypo/hypercoiled
and abnormal insertions. These lesions from the umbilical cord and
membranes have been shown to be associated with fetal or perinatal
mortality in previous studies (15-17).
In the present study, they were associated with newborns with birth
asphyxia (P=0.01).
The macroscopic examination of the placentas, as
well as in other scientific studies, did not present significant
changes (18). Lachapelle et
al (19) demonstrated that the
weight of the placenta and the ratio between birth weight and
placenta proved to be a valuable factor. As observed in the present
study, placental weight tended to be greater in newborns who had
developing brain lesions, particularly in those with an extended
lesion that caused hypoxic ischemic encephalopathy (P=0.01). The
underlying mechanisms responsible for the augmentation of placental
weight remain unknown. Placental hypertrophy during pregnancy may
potentially serve as a protective mechanism for the fetus against
stressful events in utero, which increases the risk of
perinatal depression following hazardous events during labor and
birth. This predisposition is primarily associated with the
incidence of significant brain damage.
Other researchers have observed associations between
the velamentous and marginal insertion of the umbilical cord into
the placenta with the presence of hypoxic ischemic encephalopathy
(20). These changes in the
umbilical cord can cause acute injuries during labor or chronic
circulatory obstruction, both of which can lead to birth asphyxia.
Nomiyama et al (21)
demonstrated the utility of Doppler imaging in the context of
normal second-trimester sonography to identify cord insertion,
particularly velamentous insertion. The rapid examination,
characterized by a high level of precision, aids in the
identification of pregnancies that are at risk. In the present
study, the results were strongly associated with a single umbilical
artery of the umbilical cord and birth asphyxia due to compromised
blood flow through the umbilical vessels (P=0.01).
Redline (22) pointed
out that placental lesions are the only explanation for asphyxia in
some cases. Redline (22) identified
the presence of placental pathological lesions in >90% of
infants who subsequently developed cerebral palsy. The present
study identified a statistically significant association between
the presence of placental changes and the diagnosis of birth
asphyxia (P=0.01). Redline (22)
also demonstrated the association between placental vasculopathy
and umbilical arterial pH under 7.10, which causes thrombotic
events and mortality.
Due to the extensive lesions encountered in the
histopathological examination, in the present study, the Amsterdam
standardized classification was used to make the changes associated
with hypoxic ischemic encephalopathy as specific as possible. Other
classifying systems of placental injuries are used by other authors
in their publications. For example, Chang et al (23) classified the lesions into
inflammatory, vascular and other, while others have made more
detailed classifications with 10 to 16 subgroups of
histopathological lesions (20). In
the present study, only six main groups were selected; the other
lesions that could not be classified were very few and
insignificant. Each lesion was categorized according to the
Amsterdam Criteria (7) and included
six large categories: Maternal vascular malperfusion, fetal
vascular malperfusion, chorioamnionitis, chronic villitis of
unknown aetiology, delayed villous maturation and abruption
placenta. In the analyzed placentas, although several concomitant
lesions were present, the division was performed after the dominant
lesion from the pre-specific Amsterdam group.
Furthermore, in the present study, the most common
microscopic placental lesions associated with the hypoxic-ischemic
syndrome were in the category of maternal and fetal placental
malperfusion, being labelled as chronic lesions predominant with
the damage of villi (infarction, fibrin depositions and necrosis).
Badawi et al (24),
emphasized that fetal vascular malperfusion lesions present in
newborns can cause both acute neonatal lesions and long-term damage
through cord compression. Such lesions emphasize the multitude of
ways of the etiology of hypoxic lesions. The results of the present
study revealed an association between the presence of fetal
vascular malperfusion-type lesions and the presence of perinatal
asphyxia (P=0.01).
In addition, the present study identified a strong
association between the presence of placental infarction and the
occurrence of severe asphyxia, as in other research (25). The connection between placental
vascular changes and the etiology of hypoxia at birth was a large
research subject and has been shown to be associated with an
increased risk of cerebral palsy (26). The results of the present study
revealed a strong statistical association between maternal vascular
malperfusion lesions and birth asphyxia (P=0.01), both moderate and
severe.
The presence of vascular lesions increases the
vulnerability of the fetus during labor, leading to hypoxic lesions
at birth. Furthermore, these results underscore the presence of a
persistent thrombotic mechanism occurring inside the fetal and
placental blood vessels, which demonstrate a close interconnection.
There is a positive association between hypoxia and the occurrence
of clots inside the fetoplacental circulation. The findings of the
present study align with those of Redline (22), who emphasized a statistically
significant correlation between prenatal vascular malperfusion and
hypoxic-ischemic encephalopathy.
The association between villous destruction, caused
by chronic villitis of unknown etiology (P=0.01) or delayed villous
maturation (P=0.01), and mild forms of the disease is not
unexpected. This is due to the fact that these mechanisms
contribute to the gradual development of lesions by activating
stress-adaptive mechanisms in the fetus before birth. Consequently,
the infant presents a reduced level of hypoxia and a better
response at birth.
In contrast to the study by Wintermark et al
(9), who reported an association
between chorioamnionitis and brain injury, the results of the
present study did not show any such association. This can be
explained by the good protective function of the brain in acute
injuries. Additionally, Strunk et al (27) found that the risk of late-onset
sepsis for infants exposed to histological chorioamnionitis
decreased. Although the present study included newborns with
gestational ages <32 weeks, it is notable that the neonates were
at term.
Previous research has established a connection
between placental abruption and cerebral palsy (28). Although the diagnosis of placental
abruption is primarily clinical, a histopathological examination
has revealed the presence of retroplacental hematoma. Following the
findings of Bingham et al (14), the appearance of retroplacental
hematoma did not demonstrate a statistically significant
association with the occurrence of ischemic hypoxic syndrome at
birth. In addition, the present study did not reveal a significant
association between the two factors.
Recent research, in accordance with the latest ISUOG
guidelines, highlights the significance of evaluating the placenta
and umbilical cord during the ultrasound examination in the third
trimester of pregnancy (29).
Therefore, the data collected regarding the position of the
placenta and its specific type (such as previa or accreta) can
determine the mode of delivery and the level of urgency in
finishing the pregnancy, subsequently reducing the rate of
perinatal mortality.
Furthermore, placenta previa increases the risk of
umbilical cord abnormalities, such as velamentous cord insertion,
marginal insertion and vasa previa. These conditions can be
detected through an ultrasound examination during the third
trimester of pregnancy. The umbilical cord abnormalities observed
in the present study were associated with neonatal hypoxia (P=0.01)
(30).
The present study stands out from the vast
literature as, contrary to the numerous studies that have been
published in the past, the particularity of the present study lies
in the clear diagnostic criteria for perinatal asphyxia and a
standardized classification of placental lesions. A notable
strength of the present study is that we were able to identify
placental lesions in a group of patients who had a clear diagnosis
of birth asphyxia, as well as that we were able to categorize
placental lesions according to Amsterdam criteria and that we
identified a large number of lesions on the examined placenta. The
limitations of the present study are linked to the relatively
limited number of patients included, the unblinded nature of the
single pathologist responsible for the placental examination, and
the absence of brain imaging for newborns with hypoxic-ischemic
syndrome.
In conclusion, the present study demonstrates that
birth asphyxia is associated with micro- and macroscopic placental
lesions, as well as abnormalities of the umbilical cord. In
addition, the weight of the placenta tends to be greater in
newborns with hypoxia at birth. Furthermore, the placental
histopathological examination illustrating changes in both maternal
and fetal vascular malperfusion is associated with the presence of
hypoxic syndrome at birth.
Moreover, the categorization of patients based on
the manifestation of the disease enabled us to emphasize that the
less severe versions are linked to the existence of persistent
villous inflammation and the postponement of delayed villous
maturation. Furthermore, it has been observed that the presence of
maternal and fetal vascular malperfusion-type lesions is related to
moderate and severe types of hypoxic lesions.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
IG, ACA, AIT and MD were involved in the
conceptualization of the study. ACA, VD, OMP and AM were involved
in the study methodology. ACA and LC were involved in the
histological examination. ACA, VD and MD were involved in obtaining
the informed consent from the patients. ACA, AB and SCȘ worked with
the database from which the patients' medical records were
obtained. PB and AJI were involved in the statistical analysis.
ACA, OMP and AIT were involved in the writing and editing of the
manuscript. VD and AIT confirm the authenticity of all the raw
data. All authors have read and agreed to publish the final version
of the manuscript.
Ethics approval and consent to
participate
The research was conducted with the approval of the
Ethics Council of ‘Filantropia’ Clinical Hospital (no. 5266/2020).
All the patient legal representatives signed the informed consent
forms for the participation of the patients in the study, according
to the privacy protocols of the hospital.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Ambalavanan N, Carlo WA, Shankaran S, Bann
CM, Emrich SL, Higgins RD, Tyson JE, O'Shea TM, Laptook AR,
Ehrenkranz RA, et al: Predicting outcomes of neonates diagnosed
with hypoxic-ischemic encephalopathy. Pediatrics. 118:2084–2093.
2006.
|
|
2
|
Volpe JJ: Neurology of the newborn.
Edition 5. Saunders, PA, 2008.
|
|
3
|
Avroy AA, Fanaroff JM and Klaus MH: Care
of the high-risk neonate. Edition 6. Saunders, PA, 2013.
|
|
4
|
Higgins RD, Raju TN, Perlman J, Azzopardi
DV, Blackmon LR, Clark RH, Edwards AD, Ferriero DM, Gluckman PD,
Gunn AJ, et al: Hypothermia and perinatal asphyxia: Executive
summary of the national institute of child health and human
development workshop. J Pediatr. 148:170–175. 2006.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Executive summary: Neonatal encephalopathy
and neurologic outcome, second edition. Report of the American
College of Obstetricians and Gynecologists' Task Force on Neonatal
Encephalopathy. Obstet Gynecol. 123:896–901. 2014.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Redline RW: Placental pathology: A
systematic approach with clinical correlations. Placenta. 29
(Suppl):S86–S91. 2008.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Khong TY, Mooney EE, Ariel I, Balmus NC,
Boyd TK, Brundler MA, Derricott H, Evans MJ, Faye-Petersen OM,
Gillan JE, et al: Sampling and definitions of placental lesions:
Amsterdam placental workshop group consensus statement. Arch Pathol
Lab Med. 140:698–713. 2016.PubMed/NCBI View Article : Google Scholar
|
|
8
|
de Laat MW, Franx A, Bots ML, Visser GH
and Nikkels PG: Umbilical coiling index in normal and complicated
pregnancies. Obstet Gynecol. 107:1049–1055. 2006.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Wintermark P, Boyd T, Gregas MC, Labrecque
M and Hansen A: Placental pathology in asphyxiated newborns meeting
the criteria for therapeutic hypothermia. Am J Obstet Gynecol.
203(579)2010.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Nielsen LF, Schendel D, Grove J, Hvidtjørn
D, Jacobsson B, Josiassen T, Vestergaard M, Uldall P and Thorsen P:
Asphyxia-related risk factors and their timing in spastic cerebral
palsy. BJOG. 115:1518–1528. 2008.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Fox A, Doyle E, Geary M and Hayes B:
Placental pathology and neonatal encephalopathy. Int J Gynaecol
Obstet. 160:22–27. 2023.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Redline RW: Disorders of placental
circulation and the fetal brain. Clin Perinatol. 36:549–559.
2009.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Chang KT: Examination of the placenta:
Medico-legal implications. Semin Fetal Neonatal Med. 19:279–284.
2014.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Bingham A, Gundogan F, Rand K and Laptook
AR: Placental findings among newborns with hypoxic ischemic
encephalopathy. J Perinatol. 39:563–570. 2019.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Parast MM, Crum CP and Boyd TK: Placental
histologic criteria for umbilical blood flow restriction in
unexplained stillbirth. Hum Pathol. 39:948–953. 2008.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Tantbirojn P, Saleemuddin A, Sirois K,
Crum CP, Boyd TK, Tworoger S and Parast MM: Gross abnormalities of
the umbilical cord: Related placental histology and clinical
significance. Placenta. 30:1083–1088. 2009.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Kidokoro H, Anderson PJ, Doyle LW,
Woodward LJ, Neil JJ and Inder TE: Brain injury and altered brain
growth in preterm infants: Predictors and prognosis. Pediatrics.
134:e444–e453. 2014.PubMed/NCBI View Article : Google Scholar
|
|
18
|
de Regnier RA: Placental windows into
neonatal encephalopathy. J Pediatr. 202(3)2018.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Lachapelle J, Chen M, Oskoui M, Ali N,
Brown R and Wintermark P: Placental pathology in asphyxiated
newborns treated with therapeutic hypothermia. J Neonatal Perinatal
Med. 8:33–40. 2015.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Nasiell J, Papadogiannakis N, Lof E,
Elofsson F and Hallberg B: Hypoxic ischemic encephalopathy in
newborns linked to placental and umbilical cord abnormalities. J
Matern Fetal Neonatal Med. 29:721–726. 2016.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Nomiyama M, Toyota Y and Kawano H:
Antenatal diagnosis of velamentous umbilical cord insertion and
vasa previa with color Doppler imaging. Ultrasound Obstet Gynecol.
12:426–429. 1998.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Redline RW: Severe fetal placental
vascular lesions in term infants with neurologic impairment. Am J
Obstetr Gynecol. 192:452–457. 2005.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Chang T, Reyes C, Teng J, Placette J,
Massaro AN and Nelson KB: Neonatal encephalopathy, sentinel events,
and the placenta. J Neonatal Perinatal Med. 5:41–48. 2012.
|
|
24
|
Badawi N, Kurinczuk JJ, Keogh JM,
Alessandri LM, O'Sullivan F, Burton PR, Pemberton PJ and Stanley
FJ: Intrapartum risk factors for newborn encephalopathy: The
Western Australian case-control study. BMJ. 317:1554–1558.
1998.PubMed/NCBI View Article : Google Scholar
|
|
25
|
McDonald DG, Kelehan P, McMenamin JB,
Gorman WA, Madden D, Tobbia IN and Mooney EE: Placental fetal
thrombotic vasculopathy is associated with neonatal encephalopathy.
Hum Pathol. 35:875–880. 2004.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Mir IN, Johnson-Welch SF, Nelson DB, Brown
LS, Rosenfeld CR and Chalak LF: Placental pathology is associated
with severity of neonatal encephalopathy and adverse developmental
outcomes following hypothermia. Am J Obstet Gynecol.
213(849)2015.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Strunk T, Doherty D, Jacques A, Simmer K,
Richmond P, Kohan R, Charles A and Burgner D: Histologic
chorioamnionitis is associated with reduced risk of late-onset
sepsis in preterm infants. Pediatrics. 129:e134–e141.
2012.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Thorngren-Jerneck K and Herbst A:
Perinatal factors associated with cerebral palsy in children born
in Sweden. Obstet Gynecol. 108:1499–1505. 2006.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Khalil A, Sotiriadis A, D'Antonio F, Da
Silva Costa F, Odibo A, Prefumo F, Papageorghiou AT and Salomon LJ:
ISUOG practice guidelines: Performance of third-trimester obstetric
ultrasound scan. Ultrasound Obstet Gynecol. 63:131–147.
2024.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Jauniaux ERM, Alfirevic Z, Bhide AG,
Belfort MA, Burton GJ, Collins SL, Dornan S, Jurkovic D, Kayem G,
Kingdom J, et al: Diagnosis and management: Green-top guideline no.
27a. BJOG. 126:e1–e48. 2019.PubMed/NCBI View Article : Google Scholar
|