Introduction
Intervertebral disc degeneration (IDD) is one of the
most common clinical entities and the leading etiological
contributor to low-back pain and other disc disorders (1). The progression of disc degeneration
is associated with a significant decrease in the levels of
proteoglycans (PGs) and water, as well as an increase in the levels
of type I collagen in the nucleus pulposus (NP) with the
simultaneous decrease in type II collagen levels (2–4).
Thus, a poor nutritional environment as a result of dehydration in
the discs is a major cause of degeneration of the intervertebral
discs. As a result of their ease of use, minimally invasive
properties and efficient correction of metabolic derangement,
protein growth factor injections administered into degenerative
discs have become an alternative treatment strategy to conservative
therapy and reconstructive surgery for the treatment of symptomatic
IDD (5).
Hepatocyte growth factor (HGF) was initially
identified as a mitogen of hepatocytes and promotes the
regeneration and repair of the kidney, lung and several other
tissues (6–8). In terms of its clinical application,
human HGF plasmid DNA has been used in the treatment of critical
limb ischemia (9,10). Given its therapeutic effects and
good safety profile observed in animal experiments and clinical
trials, we hypothesized that HGF therapy is capable of retarding
IDD. To the best of our knowledge, no studies examining the
therapeutic effects of HGF in degenerative discs have been
previously conducted. In the present study, a rat tail IDD model
induced by needle puncture was used due to its convenience,
minimally invasive properties and cost-effectiveness (11). The triblock
poly(lactide-co-glycolide)-poly(ethyleneglycol)-poly(lactide-co-glycolide;
PLGA-PEG-PLGA) polymer was used as the drug vehicle due to its
optimal properties, including biodegradability, thermosensitivity
and allowing a prolonged duration of drug exposure. We performed
magnetic resonance imaging (MRI), histological and
immunohistochemical assessments in a rat tail IDD model, which
demonstrated that HGF retards the process of IDD by stimulating
antifibrosis in degenerative discs.
Materials and methods
Reagents and antibodies
Recombinant human HGF was purchased from HumanZyme
Inc. (Chicago, IL, USA). Rabbit polyclonal type I and type II
collagen, bone morphogenetic protein-2 (BMP-2) and secondary goat
polyclonal fluorescein isothiocyanate (FITC)-conjugated antibodies
were purchased from Abcam (Cambridge, MA, USA). PLGA-PEG-PLGA was
synthesized at our laboratory (Fudan University, Shanghai,
China).
Animals
Thirty male Sprague-Dawley rats (each weighing
200–250 g) were used in this study. The animals were housed with
free access to commercial rodent chow and water. The temperature
was maintained at 24°C and the light schedule consisted of 12 h of
daylight starting at 8:00 a.m. and 12 h of darkness starting at
8:00 p.m. The humidity was maintained at 50%. All of the
experiments were performed according to the guidelines for the
ethical treatment of animals approved by the Laboratory Animal
Ethics Committee of Fudan University (Shanghai, China).
Surgical procedure
The rat tail segments were divided into 4 groups:
the sham-operated control segments, stab injury-only segments, gel
alone-treated segments and HGF-treated segments. The animals were
anesthetized using a combination of 10 mg/kg xylazine and 60 mg/kg
ketamine hydrochloride administered intraperitoneally. A total of
10 rat tails were prepared for drug treatment. For the MRI
assessment, the caudal segments 5/6 and 7/8 from the same rat tail
were interchangeably used for the gel alone treatment and HGF
treatment. After identifying the level of the caudal segments by
fluoroscopy, a puncture was made parallel to the endplates through
the annulus fibrosus (AF) into the NP by a syringe needle
(21-gauge) (12). The needle was
then rotated by 180° and held for 5 sec. During the puncture,
fluoroscopy was used to ensure that the needle reached the center
of the NP (11). The caudal
segments 6/7 were left undisturbed as contrast segments for MRI.
For the stab injury-only segments, an additional 10 rat tails
underwent the same surgical procedure randomly at the level of
caudal segments 5/6 or 7/8 in order to correspond to the
drug-treated segments described above. The remaining 10 rat tails
were used to prepare the sham-operated control segments, for which
only a small incision was made in the tail skin.
Four weeks following needle puncture, the
PLGA-PEG-PLGA gel loaded with HGF or the gel alone was slowly
injected into the NP of the respective caudal segments of the rat
tail. Recombinant human HGF (HumanZyme Inc.) was added to a 30%
(w/v) aqueous solution of PLGA-PEG-PLGA and homogenized at 9,600 ×
g for 30 sec at room temperature to form a homogeneous clear
solution (HGF, 5 μg/ml) (13). To
avoid injury leading to disc degeneration, a micro-syringe attached
to a 31-gauge needle (Hamilton Bonaduz AG, Bonaduz, Switzerland)
was used and the injection volume was 2 μl (14,15).
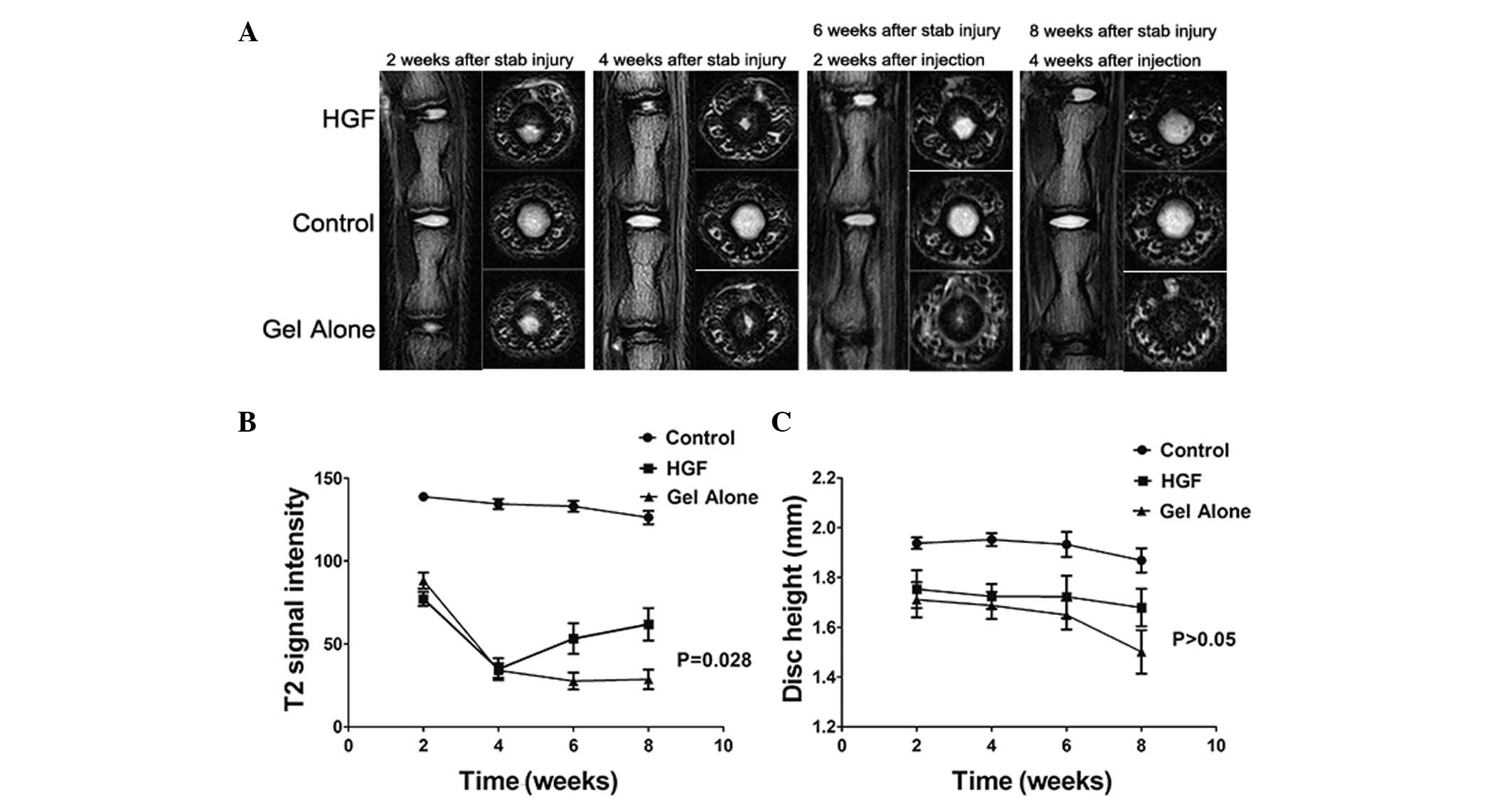
MRI evaluation
The effect of stab injury and HGF treatment on disc
degeneration was evaluated using a Siemens Trio Tim 3.0T MR scanner
(Siemens Medical Solutions, Erlangen, Germany) at 2 and 4 weeks
following stab injury, and at 2 and 4 weeks following drug
injection. The animals were laid prone and the tails were
straightened in the MR scanner. Serial T2-weighted sagittal and
transverse images covering the entire experimental disc area were
obtained using the following parameter settings: repetition time,
6150 msec; echo time, 80 msec; field of view, 60×35 mm and slice
thickness, 0.8 mm. T2-weighted signal intensity and disc height
were measured using the Image J software (The National Institutes
of Health, Bethesda, MD, USA). Image assessments were conducted by
two independent, blinded and experienced observers. The data were
presented as the mean of the two evaluations.
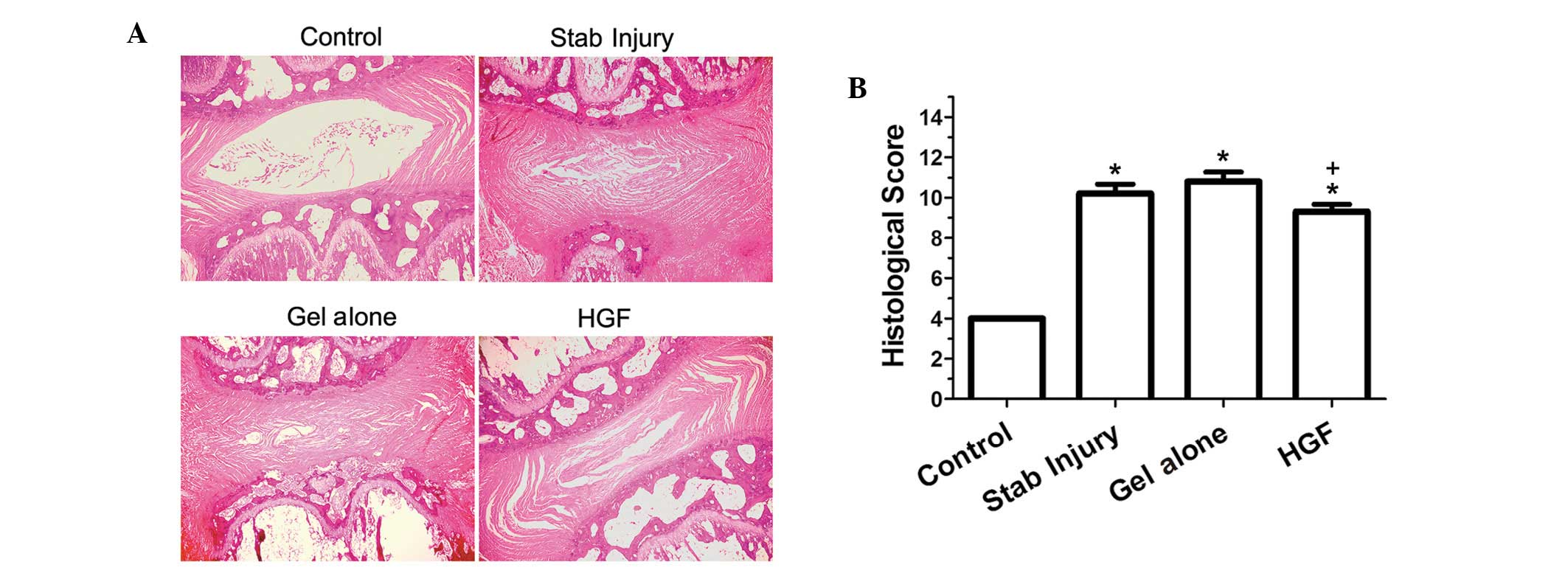
Histological evaluation
At 4 weeks following drug injection, all of the rats
were euthanized and the segments were harvested for histological
examination. The discs were fixed and decalcified, and then
processed for paraffin embedding and sectioning. Sagittal sections
(5 μm) were obtained and stained with hematoxylin and eosin
(H&E). Histological images were analyzed using the Olympus BX51
microscope (Olympus, Center Valley, PA, USA). The extent of disc
degeneration was graded using a semi-quantitative method as
described previously by Masuda et al(16). The assessment was conducted by two
independent, blinded and experienced observers. The data were
presented as the mean of the two evaluations.
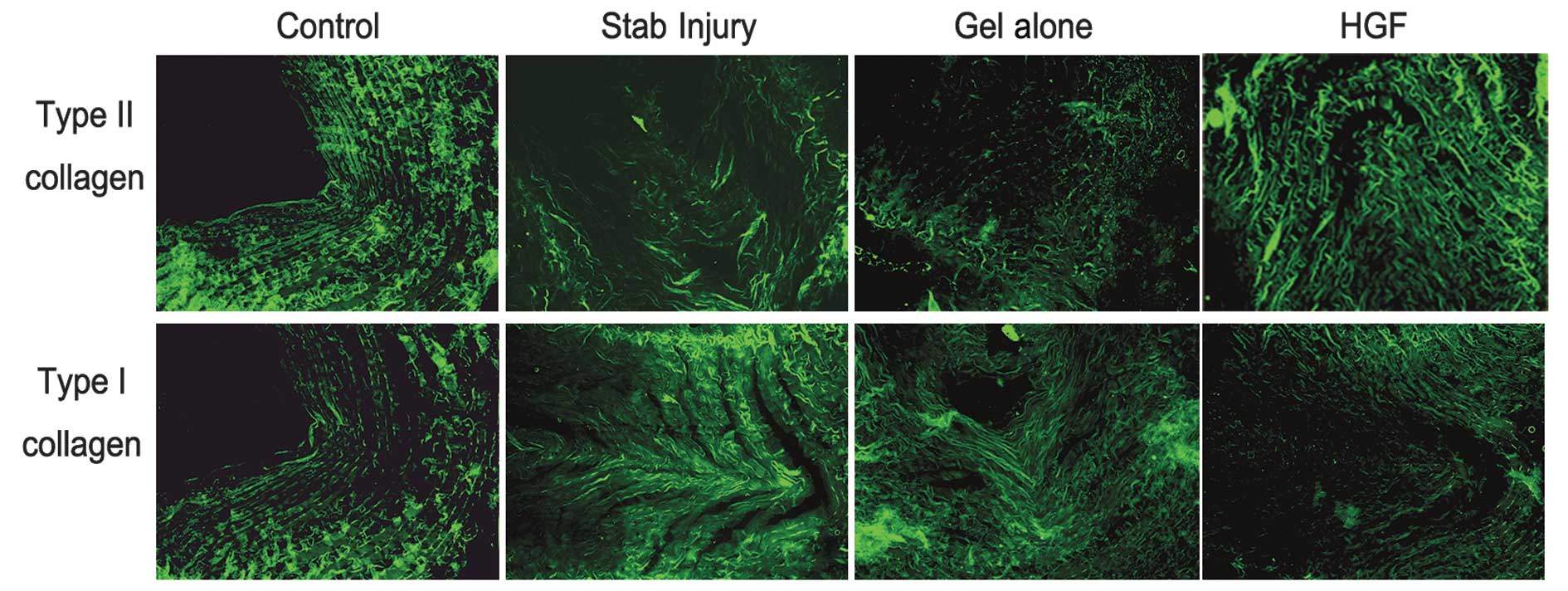
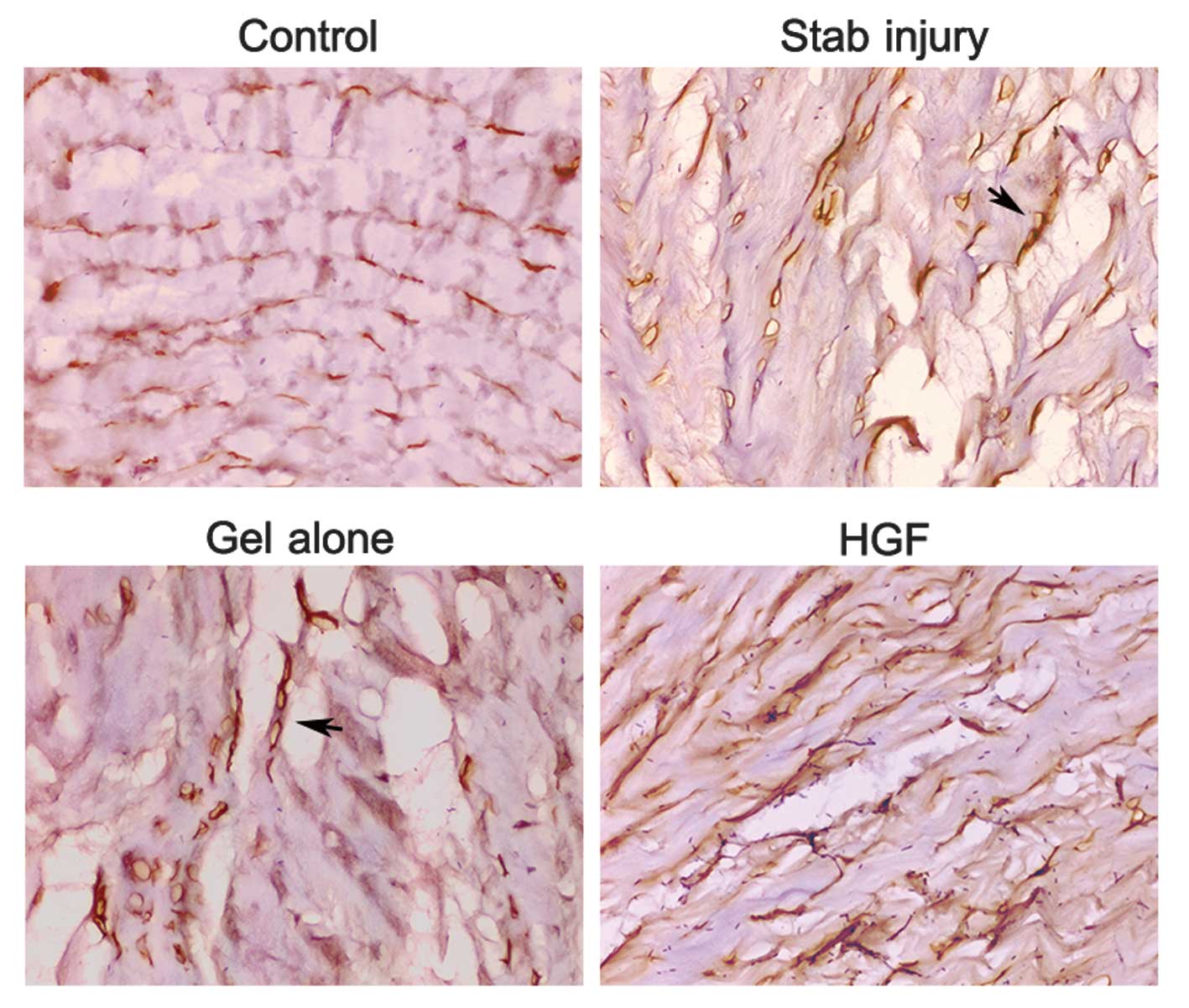
Immunohistochemical examination
For the immunohistochemical examination, the
sections were stained with rabbit anti-type I and type II collagen,
and anti-BMP-2 antibodies (Abcam). Paraffin-embedded sections were
deparaffinized and rehydrated, immersed in a retrieval solution (10
mmol/l citrate, pH 6.0) and then placed in a microwave for 10 min.
Endogenous peroxidase activity was blocked using 3% hydrogen
peroxide for 10 min. Non-specific binding sites were blocked using
1% bovine serum albumin for 30 min at room temperature. The
sections were incubated with the primary antibody at 4°C overnight
and then with the FITC-conjugated secondary antibody for 30 min at
room temperature. The diaminobenzidine detection method was used to
visualize the BMP-2 protein expression (11) and the sections were counterstained
using hematoxylin.
Statistical analysis
The SPSS version 17.0 software (SPSS, Inc., Chicago,
IL, USA) was used for all statistical analyses. Data were expressed
as the mean ± standard error. The Kruskal-Wallis test was used to
analyze the differences in the T2 signal intensities and in the
histological scores of the discs. One-way ANOVA was used to analyze
the differences in disc height. P<0.05 was considered to
indicate a statistically significant result.
Results
MRI assessment
The T2 signal intensity was decreased in the gel
alone-treated and HGF-treated segments at 2 and 4 weeks following
stab injury. However, the signal intensity in the HGF-treated
segments was increased at 4 weeks following drug injection compared
with the gel alone-treated segments, and the difference was
statistically significant (P=0.028; Fig. 1A and B). The degree of disc height
reduction in the HGF-treated segments was smaller compared with the
gel alone-treated segments at 2 and 4 weeks following drug
injection; however, the difference was not statistically
significant (P>0.05; Fig.
1C).
Histological changes and scores
H&E staining demonstrated an intact
circumferential AF in the sham-operated control segments and the
border between the AF and the NP was clear. The NP occupied the
majority of the disc area. In the stab injury-only and gel
alone-treated segments, ruptured and serpentine-patterned fibers
were observed in the AF. Furthermore, the border between the AF and
NP was interrupted and unclear, and exhibited features of severe
degeneration. However, the AF and the border between the AF and the
NP in the HGF-treated segments appeared more regular compared with
those observed in the stab-injury only and gel alone-treated
segments (Fig. 2A). Statistical
analysis demonstrated that the histological score of the
HGF-treated segments was significantly lower compared with the gel
alone-treated segments (P=0.025; Fig.
2B).
Immunohistochemical evaluation
Immunofluorescence studies revealed that the
staining for type II collagen was stronger in the HGF-treated
segments compared with the other experimental segments. By
contrast, the staining was weaker in the stab-injury only and gel
alone-treated segments when compared with the sham-operated control
segments. By contrast, type I collagen staining appeared strongly
positive in the stab-injury only and gel alone-treated segments
when compared with the sham-operated control segments. However, in
the HGF-treated segments, type I collagen was almost exclusively
observed in the outer layer of the AF (Fig. 3).
The expression levels of BMP-2 were detected by
immunohistochemical staining (Fig.
4). The BMP-2 expression levels were negligible in the
sham-operated control segments. Conversely, the BMP-2 expression
levels were notably increased in the AF cells of the HGF-treated
segments. By contrast, only the disrupted border in the AF
demonstrated a strong positive staining for BMP-2 expression in the
stab injury-only and gel alone-treated segments (Fig. 4).
Discussion
When evaluating the degree of disc degeneration, the
two most important clinical parameters to consider are the values
of T2-weighted signal intensity and disc height, which are measured
by MRI. Therefore, we evaluated MR scans in order to assess disc
degeneration intravitally and continuously in vivo. The
signal intensity of the T2-weighted images and disc height on the
MR scans represented the water content and the NP volume in the
intervertebral discs, and the loss of water content and NP volume
were associated with a reduction in the levels of PGs in the NP,
contributing to the decrease in the T2-weighted signal intensity
and disc height. Thus, disc regeneration leads to an increased
signal intensity of the T2-weighted image and disc height (17,18).
Our results demonstrated that degenerative changes in discs induced
by stab injury were recovered following HGF injection. The
T2-weighted signal intensity of the HGF-treated segments was
significantly stronger than that of the gel alone-treated segments
at 4 weeks following drug injection. Although the differences in
disc height between the HGF-treated and gel alone-treated segments
was not statistically significant following drug injection, our
results demonstrated a trend towards HGF treatment retarding the
reduction of disc height.
During degeneration, discs become less elastic,
consequently inhibiting their ability to absorb and dissipate
spinal forces. The increase in type I collagen levels along with
the corresponding decrease in type II collagen and PG levels in the
disc matrix has been identified as a factor that causes the poor
nutritional environment and inferior mechanical properties of
degenerated discs (19). In
samples of human lumbar intervertebral discs, type II collagen
levels were demonstrated to be present at normal levels in the NP
and in the inner layer of the AF; however, the levels were reduced
in advanced degenerative discs. In addition, type I collagen levels
were demonstrated to be present at normal levels in the AF and
degenerative NP (2). In a rabbit
annular stab-injury model, aggrecan and type IIa collagen mRNA
levels were decreased and were unable to be restored to normal
levels, whereas type Ia collagen mRNA levels gradually increased
throughout the course of degeneration (20). Our results demonstrated that in
degenerative discs treated with HGF, the levels of type I collagen
synthesis in the NP were suppressed; however, changes in the levels
of synthesis of intrinsic type I collagen in the outer layer of the
AF were not observed, and type II collagen levels in the NP were
restored. Our results indicate that HGF treatment provides an
optimum method to maintain the normal ECM components and mechanical
properties of discs.
The expression of endogenous growth factors in cells
is required for degenerative disc repair. In degenerative disc
models, the decreased expression of the BMP-2 gene may represent a
failed reparative response to injury (20,21).
In an external-compression degenerative disc model,
immunohistochemical evaluation of the compressed discs demonstrated
a loss of the annular architecture and a significant reduction in
the number of BMP-2-positive cells, whereas gene expression
analysis showed a significant upregulation of BMP-2 (22). In a rabbit annular stab-injury
model, there was a relative decrease in BMP-2 mRNA levels, followed
by a consequent increase close to the preoperative levels (20). In a prospective, randomized
controlled animal study, injection of the BMP-2 gene delayed
degenerative changes in a rabbit disc puncture model (23). Our results demonstrated that the
number of BMP-2-positive cells in the AF increased following
treatment with HGF, whereas a strong positive staining of BMP-2 was
only observed in cells at the disrupted border in the AF of
stab-injury only and gel alone-treated segments, suggesting that
HGF promotes BMP-2-induced repair in degenerative discs. In
addition, an in vitro study using rat disc cells
demonstrated the effect of BMP-2 on type II collagen and aggrecan
mRNA expression levels (24).
These findings suggest that the upregulation of BMP-2 in
HGF-treated segments may have stimulated type II collagen and
aggrecan synthesis observed in our study. However, the correlation
between HGF and BMPs, and the precise role of each protein in
degenerative disc repair requires further elucidation.
In conclusion, the present study has demonstrated
that HGF-loaded PLGA-PEG-PLGA gel injected into the degenerative
discs of rat tail models retards disc degeneration, as revealed by
MRI, histological and immunohistochemical evaluation. The study
provides an alternative biological method to achieve antifibrosis
in the NP to induce disc repair. Considering the differences
between the rat tail spine and the human lumbar spine, additional
studies using a different animal model that closely resembles the
characteristics of the human lumbar spine are required in order to
evaluate the biological effects of HGF in degenerative discs.
References
|
1
|
Andersson GB: Epidemiological features of
chronic low-back pain. Lancet. 354:581–585. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Nerlich AG, Boos N, Wiest I and Aebi M:
Immunolocalization of major interstitial collagen types in human
lumbar intervertebral discs of various ages. Virchows Arch.
432:67–76. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Zhao CQ, Wang LM, Jiang LS and Dai LY: The
cell biology of intervertebral disc aging and degeneration. Ageing
Res Rev. 6:247–261. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Bernick S, Walker JM and Paule WJ: Age
changes to the anulus fibrosus in human intervertebral discs. Spine
(Phila Pa 1976). 16:520–524. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Masuda K, Oegema TR Jr and An HS: Growth
factors and treatment of intervertebral disc degeneration. Spine
(Phila Pa 1976). 29:2757–2769. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Matsumoto K and Nakamura T: Hepatocyte
growth factor: molecular structure, roles in liver regeneration,
and other biological functions. Crit Rev Oncog. 3:27–54. 1992.
|
|
7
|
Mizuno S and Nakamura T: Hepatocyte growth
factor: a regenerative drug for acute hepatitis and liver
cirrhosis. Regen Med. 2:161–170. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Mizuno S, Matsumoto K and Nakamura T: HGF
as a renotrophic and anti-fibrotic regulator in chronic renal
disease. Front Biosci. 13:7072–7086. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Shigematsu H, Yasuda K, Iwai T, et al:
Randomized, double-blind, placebo-controlled clinical trial of
hepatocyte growth factor plasmid for critical limb ischemia. Gene
Ther. 17:1152–1161. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Powell RJ, Simons M, Mendelsohn FO, et al:
Results of a double-blind, placebo-controlled study to assess the
safety of intramuscular injection of hepatocyte growth factor
plasmid to improve limb perfusion in patients with critical limb
ischemia. Circulation. 118:58–65. 2008. View Article : Google Scholar
|
|
11
|
Zhang H, La Marca F, Hollister SJ,
Goldstein SA and Lin CY: Developing consistently reproducible
intervertebral disc degeneration at rat caudal spine by using
needle puncture. J Neurosurg Spine. 10:522–530. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Hsieh AH, Hwang D, Ryan DA, Freeman AK and
Kim H: Degenerative anular changes induced by puncture are
associated with insufficiency of disc biomechanical function. Spine
(Phila Pa 1976). 34:998–1005. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Chen S and Singh J: Controlled release of
growth hormone from thermosensitive triblock copolymer systems: In
vitro and in vivo evaluation. Int J Pharm. 352:58–65. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Jeong JH, Lee JH, Jin ES, Min JK, Jeon SR
and Choi KH: Regeneration of intervertebral discs in a rat disc
degeneration model by implanted adipose-tissue-derived stromal
cells. Acta Neurochir (Wien). 152:1771–1777. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Mao HJ, Chen QX, Han B, et al: The effect
of injection volume on disc degeneration in a rat tail model. Spine
(Phila Pa 1976). 36:E1062–E1069. 2011.PubMed/NCBI
|
|
16
|
Masuda K, Aota Y, Muehleman C, et al: A
novel rabbit model of mild, reproducible disc degeneration by an
anulus needle puncture: correlation between the degree of disc
injury and radiological and histological appearances of disc
degeneration. Spine (Phila Pa 1976). 30:5–14. 2005.
|
|
17
|
Roberts N, Gratin C and Whitehouse GH: MRI
analysis of lumbar intervertebral disc height in young and older
populations. J Magn Reson Imaging. 7:880–886. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Schiebler ML, Camerino VJ, Fallon MD,
Zlatkin MB, Grenier N and Kressel HY: In vivo and ex vivo magnetic
resonance imaging evaluation of early disc degeneration with
histopathologic correlation. Spine (Phila Pa 1976). 16:635–640.
1991. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Ruan DK, Xin H, Zhang C, et al:
Experimental intervertebral disc regeneration with
tissue-engineered composite in a canine model. Tissue Engineering
Part A. 16:2381–2389. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Sobajima S, Shimer AL, Chadderdon RC, et
al: Quantitative analysis of gene expression in a rabbit model of
intervertebral disc degeneration by real-time polymerase chain
reaction. Spine J. 5:14–23. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Sowa G, Vadalà G, Studer R, et al:
Characterization of intervertebral disc aging: longitudinal
analysis of a rabbit model by magnetic resonance imaging,
histology, and gene expression. Spine (Phila Pa 1976).
33:1821–1828. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Guehring T, Omlor GW, Lorenz H, et al:
Stimulation of gene expression and loss of anular architecture
caused by experimental disc degeneration - an in vivo animal study.
Spine (Phila Pa 1976). 30:2510–2515. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Leckie SK, Bechara BP, Hartman RA, et al:
Injection of AAV2-BMP2 and AAV2-TIMP1 into the nucleus pulposus
slows the course of intervertebral disc degeneration in an in vivo
rabbit model. Spine J. 12:7–20. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Li J, Yoon ST and Hutton WC: Effect of
bone morphogenetic protein-2 (BMP-2) on matrix production, other
BMPs, and BMP receptors in rat intervertebral disc cells. J Spinal
Disord Tech. 17:423–428. 2004. View Article : Google Scholar : PubMed/NCBI
|