Introduction
According to the World Health Organization,
hypertension affects one billion people worldwide and is a major
risk factor for inducing all forms of cardiovascular disease,
exerting a similar effect in both women and men (1,2).
Hypertension is a risk factor for death and ischemic events after
the occurrence of acute coronary syndrome (ACS) (3–6).
Cardiovascular disease is the most frequent cause of mortality in
both genders; however, in the past 20 years, cardiovascular
mortality has decreased in men but increased in women (7,8).
Demographic statistics reveal that hypertension is more common in
men than women at a younger age, but in the 45–54 year age group,
it is more prevalent in women. Hypertension is estimated to affect
over a quarter of all women in the USA and this increases markedly
with age; only ~3–4% of women <35 years have hypertension, but
75% of women >75 years are affected (9). Despite this, 19% of women with
hypertension do not recognize that is a risk factor for
cardiovascular disease, and as many as 75% may not be adequately
treated (10,11). In addition to being a risk factor
for epicardial coronary disease, hypertension leads to
microcirculatory dysfunction, which disproportionately affects
women, with significant morbidity (12–16).
Materials and methods
Patient selection
A total of 12 tertiary hospitals across China
participated in the Chinese registry of acute coronary events
(CRACE) trial. The selected patients represented populations with
different demographic characteristics. Data collection began with
1,301 ACS patients between January 2001 and October 2003.
At each hospital, a trained coordinator collected
data on the following, using a standard case report form: patient
demographic and clinical characteristics, medical history, duration
of pre-hospital delay, symptoms, electrocardiographic findings, use
of cardiac medications and interventional procedures, and
hospital-associated outcomes. A standardized set of definitions for
patient-related variables and clinical diagnosis were used.
Inclusion and exclusion criteria
Patients needed to be at least 18 years old, alive
at the time of presentation, hospitalized with a presumed diagnosis
of ACS and have at least one of the following: electrocardiographic
changes consistent with ACS, elevated serum biochemical markers for
cardiac necrosis or documented evidence of coronary artery disease
(CAD). To qualify, the ACS must not have been precipitated or
accompanied by a significant comorbidity such as trauma or surgery.
Where informed consent could not be obtained, patients were
excluded from the study (5).
Quality control
The 12 triple class hospitals involved in this study
are teaching hospitals affiliated with medical universities in
different regions of China. To eliminate patient selection bias,
each hospital enrolled the first 5 ACS patients to be hospitalized
each month. Completed case report forms were faxed to the data
management organization, where they were reviewed for completeness
and clinical validity. Resulting queries were referred back to the
originating site before the forms were processed. The data were
scanned into an electronic database and checked manually prior to
statistical analysis.
Statistical analysis
Statistical analyses were performed using SPSS 11.0
for PC. Values were expressed as the means ± SD for continuous
variables. Comparisons between different groups were made using a
two-tailed Student’s t-test for continuous variables and by
Pearson’s Chi-square test and Fisher’s exact test for binary
variables. Differences were considered to indicate statistical
significance when P<0.05.
Results
Patient population
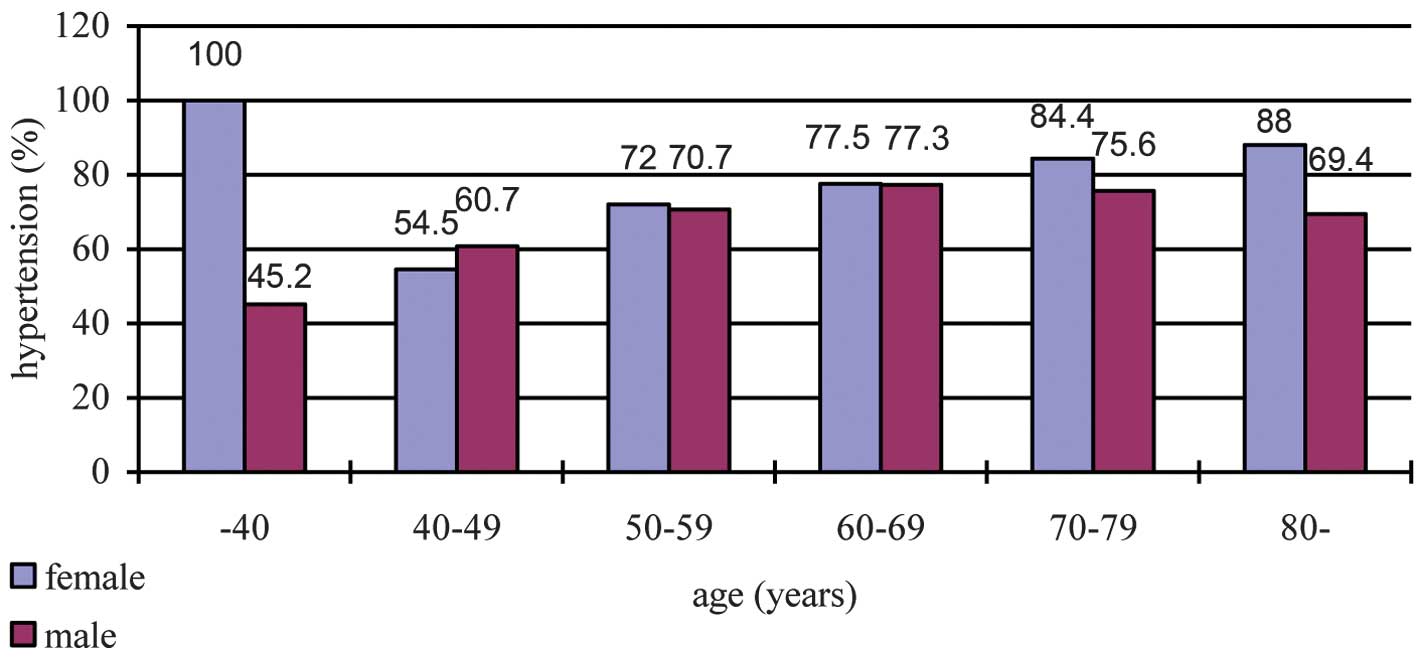
In the CRACE trial the prevalence of hypertension
was 66.4% among female patients with ACS and 56.8% among male
patients. Fig. 1 shows the
prevalence of hypertension of different age groups. Unlike
observations in unselected populations, among the ACS patients in
this study, the prevalence of hypertension was greater among women
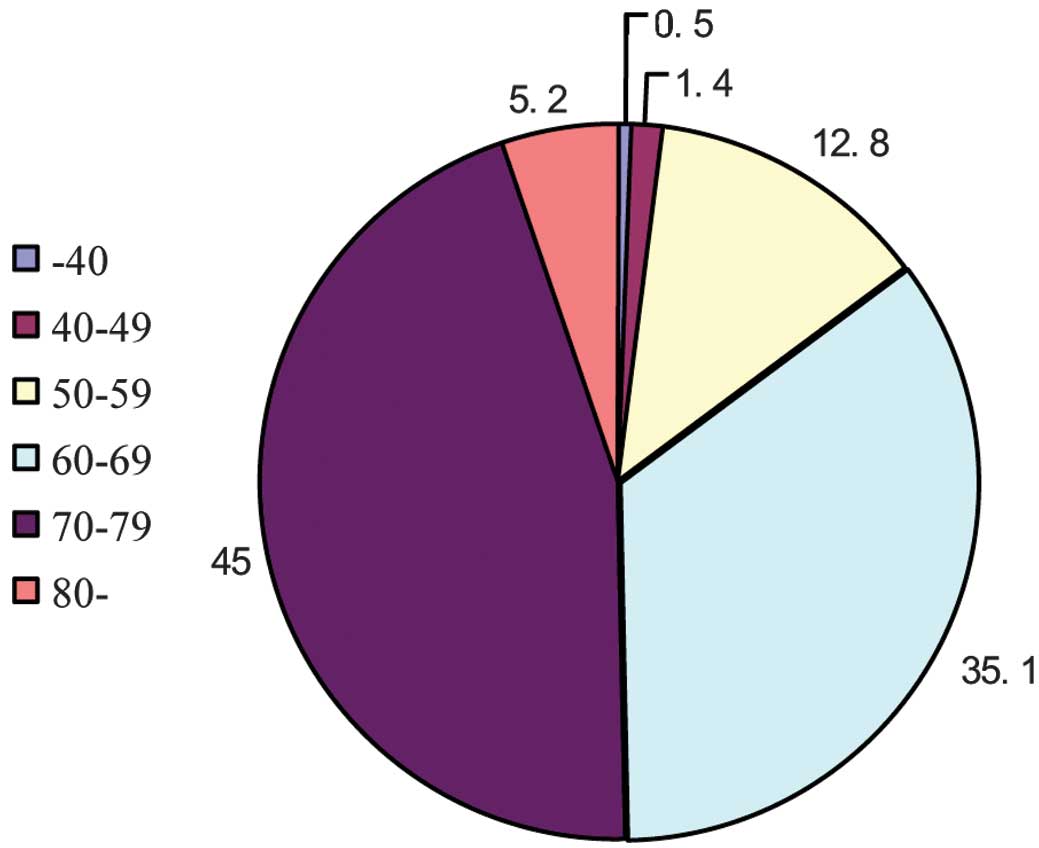
than among men for each decile of age. As shown in Fig. 2, the age distribution among
hypertensive women was skewed toward older ages, but age was found
to be more regularly distributed among hypertensive men. Overall,
for both genders, patients with hypertension were older and more
often had diabetes, hypercholesterolemia, prior incidence of
myocardial infarction (MI), prior incidence of stroke, and history
of congestive heart failure. Additionally, female patients were
more likely to present with MI rather than unstable angina pectoris
(UAP) compared to female patients without hypertension (Table I).
 | Table IBaseline characteristics of patients
with and without hypertension. |
Table I
Baseline characteristics of patients
with and without hypertension.
| Hypertension | No hypertension |
|---|
|
|
|
|---|
| Characteristics | Female (n=211) | Male (n=558) | Female (n=107) | (Male n=425) |
|---|
| Demographics |
| Age, mean ± SD | 68.17±8.49 | 62.85±10.43 | 65.38±8.48 | 60.43±12.06 |
| History and risk
factors (%) |
| Diabetes
mellitus | 34.1 | 21.9 | 24.3 | 14.4 |
|
Hypercholesterolemia | 36.5 | 32.6 | 22.4 | 22.8 |
| Current cigarette
smoking | 6.6 | 66.3 | 6.5 | 66.1 |
| Prior MI | 13.3 | 14.9 | 11.2 | 13.4 |
| Prior stroke | 12.3 | 12.2 | 3.7 | 6.4 |
| Congestive heart
failure | 8.5 | 6.5 | 7.5 | 4.7 |
| Prior PCI | 6.2 | 3.6 | 0.9 | 2.8 |
| Prior CABG | 0 | 0.7 | 0.9 | 0 |
| Clinical
presentation |
| BMI,
kg/m2 | 24.74±3.76 | 25.15±7.12 | 25.07±3.09 | 24.61±5.97 |
| Killip ≥III | 10.4 | 11.3 | 11.2 | 14.6 |
| Creatinine
clearance, ml/min | 74.57±44.59 | 80.70±57.69 | 80.43±52.5 | 80.83±50.81 |
| SBP, mmHg | 137.32±22.96 | 136.22±26.64 | 126.98±23.12 | 118.32±19.68 |
| DBP, mmHg | 79.61±15.85 | 81.58±15.19 | 75.99±14.07 | 72.97±13.67 |
| Type of ischemic
events (%) |
| STEMI | 41.2 | 45 | 34.6 | 53.2 |
| NSTEMI | 19.4 | 16.8 | 15.9 | 15.3 |
| UAP | 39.3 | 38.2 | 49.5 | 31.5 |
When comparing men and women with hypertension, the
women were older, had lower estimated creatinine clearance, and
were more likely to have diabetes, hypercholesterolemia and prior
congestive heart failure (Table
I). They tended to smoke less and were less likely to have had
a prior incidence of MI or to present with MI as their index event.
Median SBP at presentation was higher (1 mmHg) among women with
hypertension than men, despite the use of significantly more
antihypertensive medications (Table
I).
Antihypertensive medication use
As shown in Table
II, more female ACS patients with hypertension were well
controlled than male patients. The use of diuretics and β-blockers
was found to be higher in hypertensive women, yet no difference was
found with regards to the use of angiotensin-converting enzyme
inhibitors (ACEI) and calcium channel blockers (CCBs) between the
two groups. The use of all medications including ACEI, β-blockers,
CCBs and diuretics increased in both genders during management of
the presenting ACS, but, when discharged, hypertensive men (77.2%)
were more likely to have been receiving β-blockers than women
(69.2%). Although at discharge, the rate of diuretic use increased
by ~20% in both genders, hypertensive women were more likely to
have been receiving diuretics (28.4%) compared to men (22%). ACEI
use increased by ~60% (absolute increase) in both women and men as
a result of ACS treatment, but use remained similar between the
genders, and the same phenomenon was observed in the use of
CCBs.
 | Table IIUse of antihypertensive medications
among people with hypertension before and after presentation with
ACS. |
Table II
Use of antihypertensive medications
among people with hypertension before and after presentation with
ACS.
| Female (n=211) | Male (n=558) | P-value |
|---|
| BP control at
admission (%) |
| SBP <140
mmHg | 61.1 | 64.2 | |
| DBP <90 mmHg | 82 | 78 | |
| Before presentation
(%) |
| ACE inhibitors | 22.7 | 21.5 | 0.671 |
| β-blocker | 17.5 | 14.9 | 0.029 |
| CCBs | 15.2 | 14.7 | 0.801 |
| Diuretics | 4.3 | 3.9 | 0.004 |
| At discharge (%) |
| ACE inhibitors | 85.8 | 87.5 | 0.524 |
| β-blocker | 69.2 | 77.2 | 0.013 |
| CCBs | 35.1 | 34.6 | 0.878 |
| Diuretics | 28.4 | 22 | 0.020 |
Outcomes among hypertensive women and
men
Men with hypertension were more likely to receive
reperfusion therapies during hospitalization than hypertensive
women (Table III). Although no
difference was found regarding the in-hospital death rate between
genders, female patients experienced more in-hospital composite
endpoints, including recurrent angina and congestive heart failure.
Despite their higher rate of adverse clinical outcomes,
hypertensive women were less likely to receive evidence-based
medication to treat their acute coronary event than men (for women
and men, respectively: β-blocker, 69.2 vs. 77.2%; ACEI, 85.8 vs.
87.5%).
 | Table IIIReperfusion therapies and outcomes
between in-hospital female and male ACS patients with
hypertension. |
Table III
Reperfusion therapies and outcomes
between in-hospital female and male ACS patients with
hypertension.
| Outcomes | Female (n=211) | Male (n=558) | P-value |
|---|
| Reperfusion
therapies (%) | | | <0.0001 |
| No
reperfusion | 48.8 | 31.4 | |
| PCI | 44.1 | 54.3 | |
| Thrombolysis | 2.8 | 6.5 | |
| Othersa | 4.3 | 7.8 | |
| In-hospital MACCEs
(%) |
| MI within 24
h | 4.7 | 3.4 | 0.08 |
| Recurrent
angina | 27 | 15.4 | <0.0001 |
| Congestive heart
failure | 16.1 | 10.8 | 0.008 |
| Stroke | 0.9 | 0.6 | 0.156 |
| Bleeding | 1.4 | 1.1 | 0.585 |
| Discharge status
(%) | | | 0.669 |
| Death | 3.8 | 3.6 | |
| Go home | 23.3 | 21.9 | |
Discussion
Among patients with ACS in the CRACE trial, >50%
had hypertension, and it was found to be more prevalent among
women. The association of hypertension with adverse clinical
outcomes in these patients was similar in both genders. Among the
studied patients with hypertension, ~40% had failed to maintain
their blood pressure at a safe level at the beginning of the
study.
As expected, the overall prevalence of hypertension
among ACS patients was higher than that which had been reported in
the general population. Contrary to observations made regarding the
general population, in which the prevalence of hypertension is
greater among men than among women at younger ages and the opposite
is observed at older ages, we found that the prevalence of
hypertension among ACS patients was greater in women than in men in
every decile of age. We cannot find a reasonable explanation for
this finding, but we suspect that an overall greater burden of risk
factors is required to overcome the protective effect of the
premenopausal state on the development of CAD among younger women.
Alternatively, this may reflect a correlation with other medication
use (such as oral contraceptives) that influences both the
incidence of hypertension and the occurrence of ischemic events in
women compared with men (17).
In our study, hypertensive women were treated with
more antihypertensive agents than men, and the median SBP at
presentation in women was 1 mmHg higher. The effect of
antihypertensive agents on lowering blood pressure has yet to be
well studied in each gender, but previous studies have indicated
that differences in salt sensitivity, hormonal variation and
vascular reactivity may affect hypertension in women (18–21).
We observed that only 61% of women and 64% of men
with prevalent hypertension at presentation with ACS were well
controlled. Observations made from the NHANES III study may reflect
this finding in the general population in that NHANES III
demonstrated that only 70% of hypertensive participants were aware
of their diagnosis and that 31% of participants had controlled
hypertension (22). Even with
close monitoring in the setting of a large-scale randomized trial
of hypertension treatment, the 5-year follow-up data from ALLHAT
revealed that only 66% of participants achieved target levels of
hypertension control (23). In
conclusion, these figures emphasize the need for more active
management, particularly among high-risk ACS patients, and suggest
that factors other than blood pressure are important in preventing
the clinical consequences of hypertension. These additional factors
may be associated with the pleiotropic effects of many contemporary
antihypertensive medications.
Although the ALLHAT results suggest that diuretics
may be more beneficial to prevent primary coronary heart disease
than an ACEI, at the time of the SYMPHONY studies, the American
Heart Association prevention guidelines for women with hypertension
recommended the use of β-blockers and ACEI for risk factor
modification (24–26). Furthermore, the use of diuretics at
discharge after presentation with ACS remained greater in women
than in men, with β-blockers prescribed less often in women.
Although we adjusted for comorbid conditions (diabetes, heart
failure, and prior MI or bypass surgery) that may have influenced
the decision to use a given antihypertensive agent, we could not
account for possible unmeasured factors leading to this
association. For example, we noted that among the studied patients,
women had no epicardial CAD more often than men and more frequently
had preserved left ventricular function. This may be related to
gender differences in microcirculatory dysfunction associated with
hypertension and other comorbid diseases, resulting in a higher
incidence of women presenting with ACS despite having no epicardial
CAD (27–30), and it may account for
gender-related differences with regard to medication given upon
discharge.
Despite the higher prevalence of hypertension in
women than men with ACS in our study, cardiovascular outcomes were
similar after adjusting for age and comorbidities. Furthermore,
similar results were found in the overall population of the
SYMPHONY trials: the association of hypertension with adverse
clinical outcomes was similar in the two genders.
Thus, hypertensive female patients are a vital
target population for active evidence-based primary and secondary
risk factor modification. A study of the correlation between
gender, hypertension and outcomes in the NHANES III revealed that
preventable population-attributed risk of coronary heart disease
events was higher in women than men. From this observation, it was
estimated that optimal control of blood pressure could prevent more
than one-third of coronary heart disease events in men and more
than half of the events in women. We observed that hypertensive
women were less likely to receive evidence-based medications for
ACS during hospitalization than hypertensive men. This finding
suggests a need for continued education on the high risk of adverse
outcomes in hypertensive women presenting with ACS and the
importance of using therapies shown to attenuate that risk, such as
β-blockers and ACEI (1).
This study observed the differences in managing
hypertension between male and female ACS patients. As is inherent
in such analyses, selection bias may exist, and detailed data about
the duration and control of hypertension prior to admission were
not collected. Therefore, our observations, including age and
prevalence distributions, may not represent the entire population
of ACS patients, nor are they intended to reflect an unselected
population with hypertension. Results should be interpreted with
caution due to the fact that examinations of gender and
hypertension were not specified as a priori hypotheses in
the clinical trial design.
In conclusion, this study revealed gender-related
differences in the prevalence and treatment of hypertension among
patients with ACS. It demonstrated the relationship between gender,
hypertension and outcomes in this population and highlighted the
greater prevalence of hypertension between women and men with ACS
and suggests more active treatment is required for women with
hypertension.
References
|
1
|
World Health Organization. The world
health report 2002: reducing risks, promoting healthy life.
http://www.who.int/whr/2002.
Accessed January 2005
|
|
2
|
Yusuf S, Hawken S, Ounpuu S, et al: Effect
of potentially modifiable risk factors associated with myocardial
infarction in 52 countries (the INTERHEART study): case-control
study. Lancet. 364:937–952. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Lee KL, Woodlief LH, Topol EJ, et al:
Predictors of 30-day mortality in the era of reperfusion for acute
myocardial infarction. Results from an international trial of
41,021 patients GUSTO-I Investigators. Circulation. 91:1659–1668.
1995. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Newby LK, Bhapkar MV, White HD, et al:
Predictors of 90-day outcome in patients stabilized after acute
coronary syndromes. Eur Heart J. 24:172–181. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Antman EM, Cohen M, Bernink PJ, et al: The
TIMI risk score for unstable angina/non-ST elevation MI: a method
for prognostication and therapeutic decision making. JAMA.
284:835–842. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Pepine CJ, Handberg EM, Cooper-DeHoff RM,
et al: A calcium antagonist vs a non-calcium antagonist
hypertension treatment strategy for patients with coronary artery
disease. The International Verapamil-Trandolapril Study (INVEST): a
randomized controlled trial. JAMA. 290:2805–2816. 2003. View Article : Google Scholar
|
|
7
|
AHA, heart disease and stroke statistics -
2005 update. American Heart Association; Dallas, TX, USA: 2004
|
|
8
|
Chobanian AV, Bakris GL, Black HR, et al:
Seventh report of the Joint National Committee on Prevention,
Detection, Evaluation, and Treatment of High Blood Pressure.
Hypertension. 42:1206–1252. 2003. View Article : Google Scholar
|
|
9
|
Wolz M, Cutler J, Roccella EJ, et al:
Statement from the National High Blood Pressure Education Program:
prevalence of hypertension. Am J Hypertens. 13:103–104. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Vasan RS, Beiser A, Seshadri S, et al:
Residual lifetime risk for developing hypertension in middle-aged
women and men: The Framingham Heart Study. JAMA. 287:1003–1010.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Rosenthal T and Oparil S: Hypertension in
women. J Hum Hypertens. 14:691–704. 2000. View Article : Google Scholar
|
|
12
|
Reis SE, Holubkov R, Conrad Smith AJ, et
al: Coronary microvascular dysfunction is highly prevalent in women
with chest pain in the absence of coronary artery disease: results
from the NHLBI WISE study. Am Heart J. 141:735–741. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Rosengren A, Wallentin L, Gitt AK, et al:
Sex, age, and clinical presentation of acute coronary syndromes.
Eur Heart J. 25:663–670. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Gulli G, Cemin R, Pancera P, et al:
Evidence of parasympathetic impairment in some patients with
cardiac syndrome X. Cardiovasc Res. 52:208–216. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Iriarte M, Caso R, Murga N, et al:
Microvascular angina pectoris in hypertensive patients with left
ventricular hypertrophy and diagnostic value of exercise
thallium-201 scintigraphy. Am J Cardiol. 75:335–339. 1995.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Schwartzkopff B, Motz W, Frenzel H, et al:
Structural and functional alterations of the intramyocardial
coronary arterioles in patients with arterial hypertension.
Circulation. 88:993–1003. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Jaffe LS and Seely EW: The heterogeneity
of the blood pressure response to hormonal contraceptives. Curr
Opin Endocrinol Diabetes. 2:257–265. 1995. View Article : Google Scholar
|
|
18
|
Appel LJ, Champagne CM, Harsha DW, et al:
Effects of comprehensive lifestyle modification on blood pressure
control: main results of the PREMIER clinical trial. JAMA.
289:2083–2093. 2003.PubMed/NCBI
|
|
19
|
Staessen J, Bulpitt CJ, Fagard R, et al:
The influence of menopause on blood pressure. J Hum Hypertens.
3:427–433. 1989.
|
|
20
|
McIntyre M, Hamilton CA, Rees DD, et al:
Sex differences in the abundance of endothelial nitric oxide in a
model of genetic hypertension. Hypertension. 30:1517–1524. 1997.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Duvernoy C, Martin J, Briesmiester K, et
al: Myocardial blood flow and flow reserve in response to hormone
therapy in postmenopausal women with risk factors for coronary
disease. J Clin Endocrinol Metab. 89:2783–2788. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Hajjar I and Kotchen TA: Trends in
prevalence, awareness, treatment, and control of hypertension in
the United States, 1988–2000. JAMA. 290:199–206. 2003.
|
|
23
|
Cushman WC, Ford CE, Cutler JA, et al:
Success and predictors of blood pressure control in diverse North
American settings: the antihypertensive and lipid-lowering
treatment to prevent heart attack trial (ALLHAT). J Clin Hypertens
(Greenwich). 4:393–404. 2002.
|
|
24
|
Mosca L, Manson JE, Sutherland SE, et al:
Cardiovascular disease in women: a statement for healthcare
professionals from the American Heart Association. Writing Group.
Circulation. 96:2468–2482. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Mukherjee D, Fang J, Chetcuti S, et al:
Impact of combination evidence-based medical therapy on mortality
in patients with acute coronary syndromes. Circulation.
109:745–749. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Fox KA, Goodman SG, Anderson FA Jr, et al:
From guidelines to clinical practice: the impact of hospital and
geographical characteristics on temporal trends in the management
of acute coronary syndromes. The Global Registry of Acute Coronary
Events (GRACE). Eur Heart J. 24:1414–1424. 2003. View Article : Google Scholar
|
|
27
|
Hochman JS, McCabe CH, Stone PH, et al:
Outcome and profile of women and men presenting with acute coronary
syndromes: a report from TIMI IIIB. TIMI Investigators.
Thrombolysis in Myocardial Infarction. J Am Coll Cardiol.
30:141–148. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
The Global Use of Strategies to Open
Occluded Coronary Arteries (GUSTO) IIb Investigators. A comparison
of recombinant hirudin with heparin for the treatment of acute
coronary syndromes. N Engl J Med. 335:775–782. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Becker RC, Terrin M, Ross R, et al:
Comparison of clinical outcomes for women and men after acute
myocardial infarction. The Thrombolysis in Myocardial Infarction
Investigators. Ann Intern Med. 120:638–645. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Tunstall-Pedoe H, Morrison C, Woodward M,
et al: Sex differences in myocardial infarction and coronary deaths
in the Scottish MONICA population of Glasgow 1985 to 1991.
Presentation, diagnosis, treatment, and 28-day case fatality of
3991 events in men and 1551 events in women. Circulation.
93:1981–1992. 1996. View Article : Google Scholar
|