Introduction
With industrialization and the development of more
advanced forms of transportation, the incidence of spinal cord
injury (SCI) has increased. SCI is a significant cause of morbidity
and mortality (1). Spinal cord
injuries comprise damage that results in complete or partial loss
of sensation and/or motor control, and can therefore have a marked
effect on quality of life (2–4).
Current treatment options include surgery, medicine, such as
Ganglioside and Oxiracetam and physiotherapy, but no therapy is yet
available to completely restore function.
Increasing evidence has shown that brain
tissue-derived neural stem cells (NSCs) have the potential for
self-proliferation and multilineage differentiation under certain
conditions. NSCs are able to differentiate into a variety of cells
within the nervous system, indicating that they may be used for the
treatment of nerve injury (5).
However, NSC transplantation alone is not sufficient for spinal
cord repair, since the majority of the cells implanted into the
spinal cord have been shown to differentiate into a phenotype that
is restricted to glial lineages, and which rarely survive. The
microenvironment of the injured spinal cord is hypothesized to be
important in inducing the differentiation and survival of grafted
NSCs (6,7). In recent years, hypothermia (33–35°C)
has become an increasing focus of attention in research into the
treatment of SCI and brain injury, due to its neuroprotective
effects against secondary injury (8).
A large number of clinical studies have shown that
hypothermia effectively reduces secondary brain and SCI injury, and
also protects the central nervous system from injury. The
beneficial effects of hypothermia include reducing oxygen
consumption, decreasing free radical generation, delaying the
release of damaged neurotransmitters, reducing inflammation,
lowering metabolic demand and preventing the formation of cytotoxic
edema. Even a temperature reduction of 1–2°C has been demonstrated
to be protective against secondary neurological injury at the
cellular level in any organ or tissue (9–13).
In the present study, it was hypothesized that
hypothermia improves the differentiation and survival of engrafted
NSCs via its effects on the microenvironment of the injured spinal
cord. To investigate this hypothesis, the microenvironment was
modified by hypothermia, during transplantation of NSCs in a model
of SCI. The aim of this study was to investigate the effect of NSC
transplantation in combination with hypothermia on the recovery of
SCI in rats.
Materials and methods
Experimental animals and reagents
This study was approved by the Scientific Review
Committee and the Institutional Review board of Tianjin Medical
University (Tianjin, China) and all experimental procedures adhered
to the Helsinki Declaration. One 1-month-old Sprague Dawley (SD)
rat and 60 healthy female SD rats (200–250 g) were obtained from
the Chinese Academy of Medical Sciences Animal Laboratory (Beijing,
China). L-Dulbecco’s modified Eagle’s medium (L-DMEM) was obtained
from Gibco Life Technologies (Carlsbad, CA, USA). Fetal bovine
serum was obtained from GE Healthcare Life Sciences (Logan, UT,
USA). 0.01 mol/l phosphate-buffered saline (PBS) powder (pH 7.2)
was obtained from Fuzhou Maxim Biotech Inc. (Fuzhou, China).
Glutamate was obtained from Sigma-Aldrich (St. Louis, MO, USA).
Trypsin was obtained from Gibco Life Technologies. EDTA was
obtained from Tianjin Chemical Reagent No. 1 Plant (Tianjin,
China). Horseradish peroxidase (HRP) was obtained from Santa Cruz
Biotechnology, Inc. (Dallas, TX, USA). 5-bromo-deoxyuridine (Brdu)
was obtained from Takara Biotechnology, Inc. (Dalian, China).
Monoclonal mouse-anti-BrdU antibodies were obtained from Boehringer
Manheim (Ingelhemin am Rhein, Germany). Horse anti-mouse IgG
polyclonal antibodies conjugated to biotin were obtained from
Vector Laboratories, Inc. (Burlingame, CA, USA).
The one-month-old male SD rats were used to collect
BMSCs (n=5 rats per group). All the rats were sacrificed via
decapitation.
Rat bone marrow stem cell (BMSC)
cultivation
The one-month-old SD rats (irrespective of gender)
were sacrificed via decapitaton and disinfected using 75% alcohol
for ~10 min. Bilateral removal of tibias and femurs was conducted
under sterile conditions. Bone ends were removed, washed in L-DMEM
(1 ml) or stored in it or both, and prepared in single-cell
suspension at a density of 3×104 cells/ml. Cells were
inoculated into 100-ml culture flasks and placed into an incubation
box at 37°C, with 5% CO2 saturated humidity. The culture
liquid was replenished 24 h later and thereafter renewed every
three days. Nonadherent cells were removed, and adherent cells were
expanded until they reached confluence and processed through
sequential passages. The majority of contaminating hematopoietic
stem cells were lost after the first passage, and following the
second passage, cultures contained a morphologically homogenous
cell population, designated BMSCs. This was confirmed by
fluorescence-activated cell-sorting analysis, which demonstrated a
lack of expression of typical hematopoietic cell surface markers,
including CD45, CD34 and CD14, and positivity for CD71, CD105 and
CD44. Mesenchymal stem cells CD44, CD90, and CD105 were positively
expressed, while CD34 and CD45 were negatively expressed. Cells
between passages three and six were used for subsequent
experiments. They were labeled using a medium containing BrdU
(Takara Biotechnology, Dalian, China).
Establishment of animal models
A total of 60 female SD rats (200–250 g) were fed
standard animal feed (GB14924.2–2001) in the laboratory for 2 weeks
and then anesthetized with an intraperitoneal injection of 2.5%
ketamine 20 mg/kg (Hainan Kai-Pharmaceutical Co., Ltd., Hainan,
China). In the prone position, rats were fixed on the operating
table in order to enable preparation of skin specimens, which were
then thoroughly disinfected. T9 spinous processes were identified
and 2–3 cm of skin and subcutaneous tissue overlying this area were
incised along the posterior median line. Paraspinal muscles were
stripped and the T8–T9 spinous processes and lamina were exposed.
Using rat forceps, T8 and T9 spinous processes and lamina were
removed, exposing the dura mater. The right side of the spinal cord
was then cut. Paralysis of the right hind limb was considered to
indicate a successful model of SCI. Wounds were rinsed with
penicillin (Hainan Kai-Pharmaceutical Co., Ltd., Hainan, China) and
saline, and then sutured. Subsequently, the passage of urine was
encouraged twice per day, morning and evening, by squeezing the
rats’ bladders, until the micturition reflex was restored.
Animal grouping and mild hypothermia
treatment
An HP-V26 temperature meter (Beijing Zhongxiyuanda
Technology Co., Ltd., Beijing China) was used for continuous
monitoring of rat rectal temperature. The 45 rats in which a model
of acute SCI had been established, were randomly divided into three
groups: Group A, SCI control group; group B, single BMSC
transplantation group, in which rats were placed on the operating
table at room temperature with rectal temperature maintained at
(37±0.5)°C and at 6 h, a 1 ml BMSC (1×1010/l) suspension
was administered intravenously through the tail using a 1-ml
syringe; and group C, mild hypothermia and BMSC transplantation
group, in which rats were placed on an ice blanker machine (Zhuhai
Heima Medical Instrument Co., Ltd.), with rectal temperature
maintained at (34±0.5)°C, and at 6 h, a 1 ml BMSC
(1×1010/l) suspension was administered intravenously
into the tail using a 1-ml syringe. Then animals were fed in
separate cages.
Functional recovery evaluation
Following treatment, two forms of test were used to
assess functional recovery. Each test was observed by two
independent investigators.
Basso, Beattie and Bresnahan (BBB)
score
The open-field locomotion test assesses movement,
weight support and coordination. It was scored using the
standardized BBB locomotor scoring system (12). BBB scores range from 0 (flaccid
paralysis) to 21 (normal gait). Rats were acclimated to the test
environment (90 cm diameter plastic wading pool; 4 cm height) prior
to testing. The test was performed at 1, 2, 4, 6 and 8 weeks
post-SCI. The mean BBB score was calculated for each group.
Inclined plate test
An inclined plate surface was covered with a
6-mm-thick rubber pad and rats were placed in a direction of body
axis perpendicular to the longitudinal axis of the inclined plate.
The incline angle was gradually increased and rats were required to
stay in the inclined plate for at least 5 sec to record the maximum
angle achieved. The angle of incline was measured three times in
each rat, and the average value was obtained. The three groups were
measured at 1, 2, 4, 6 and 8 weeks post-SCI. The mean values for
each group at each time point were obtained.
Histological analysis
Four weeks following SCI, two rats were randomly
selected from each group for histological analysis. Dissected
spinal cord tissues were post-fixed for 3 h in 4% paraformaldehyde,
soaked overnight in 10% and then 30% sucrose, and cut into 15-mm
sagittal and parasagittal sections using a cryostat. Hematoxylin
and eosin staining, and 1% cresyl violet staining were conducted
for general histological examination.
Immunocytochemistry
Four weeks following SCI, two rats were randomly
selected from each group for immunocytochemistry analysis using
BrdU. This process required the pre-treatment of tissue sections to
denature DNA. All staining was conducted on free-floating 40-μm
sections. A monoclonal mouse-anti-BrdU antibody (1:100 dilution)
was used in combination with avidinbiotin complex and a
horse-anti-IgG-antibody conjugated with biotin (1:167 dilution).
Ten fields from each slice were randomly selected and viewed under
a high-power microscope (x200) (Metallurgical Microscope; Shanghai
Optical Instrument Production Company, Shanghai, China). The mean
number of theBrdU-positive cells in each field of vision was
calculated for each sample.
HRP retrograde neural tracing
Eight weeks following SCI, two rats were randomly
selected from each group for HRP retrograde neural tracing.
Following surgery, the spinal cord was exposed at T12 and 1 μl
aqueous suspension of 30% HRP (RZ>3.0, which represented the
enzyme purity) was injected 1 mm bilaterally to the spinal dorsal
vein. Following injection, the wound was closed and tissue samples
of the animals were maintained for 36 h prior to being perfused by
with buffer and then fixed with 1% paraformaldehyde and 1.25%
glutaraldehyde. Spinal cords were removed and stored in 20% sucrose
in 0.1 M PBS at 4°C overnight. The spinal cord was dissected and
ten fields from each slice were randomly selected in which to
calculate the HRP-labeled neurofibers under a high-power microscope
(x200). The mean was calculated for each group.
Electron microscopy (EM)
Eight weeks following SCI, two rats from each group
were randomly selected using a simple random sampling method on
pre-labeled rats. They were sacrificed and perfused intracardially
with saline, followed by 2% glutaraldehyde and 4% paraformaldehyde
in 0.1 M sodium cacodylate buffer (pH 7.4). Immediately following
perfusion, the spinal cords were removed and post-fixed in the same
medium (comprising a mixture of the primary and secondary antibody)
overnight at 4°C. The spinal cord segment at the injury epicenter
was sliced into 1-mm sections, post-fixed for 2 h in 1%
OsO4 in 0.1 M cacodylate buffer, dehydrated in graded
ethanol solutions and embedded in Epon-812 (Hyde Venture (Beijing)
Biotech Co., Ltd.). Plastic sections (1 μm) were cut and stained
with 1% toluidine blue prior to examination with a Nikon Eclipse
TE300 microscope (Tokyo, Japan) equipped with a Spot RT Color CCD
camera (Basler, Genmany). For EM, blocks were trimmed and sections
were cut at 100 nm, mounted on copper grids, stained with uranyl
acetate and lead citrate, and viewed with a JEOL Jem 1200 EX
transmission electron microscope (JEOL, Tokyo, Japan).
Statistical analysis
Data are expressed as the mean ± standard deviation
in this randomized control trial design. Analysis of variance was
performed using SPSS 16.0 statistical software (SPSS Inc., Chicago,
IL, USA). Two sample comparison was conducted using Dunnett’s
t-test. P<0.05 was considered to indicate a statistically
significant difference. All analyses were performed with SPSS
statistical software (version 16.0).
Results
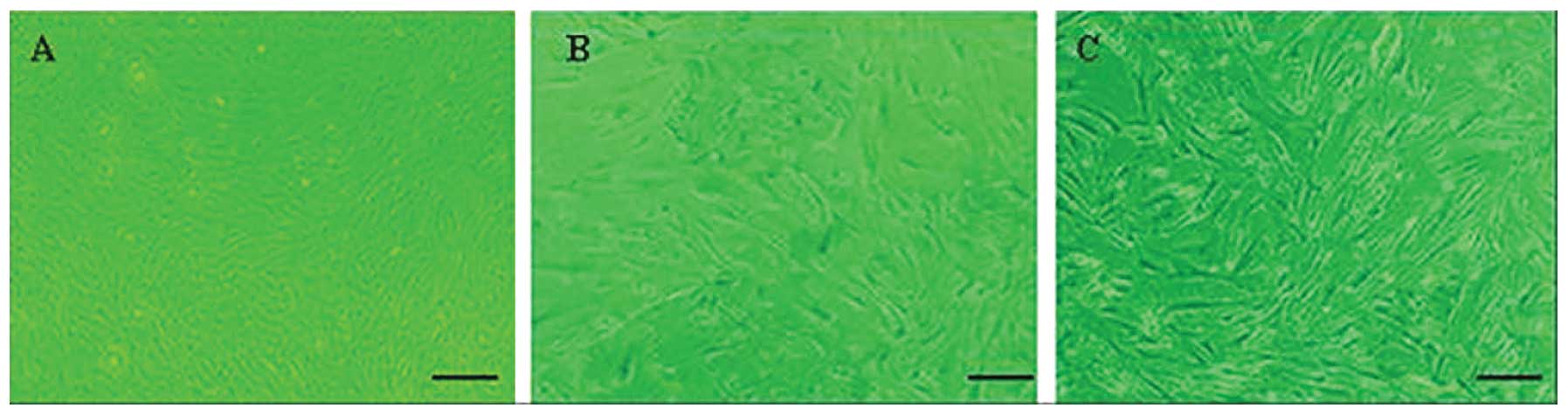
Morphology of NSCs
The number of bone marrow stromal cells and colonies
were significantly increased on the fifth day of culture. Cells at
passages 1–3 proliferated actively and the majority of cells
adhered to the monolayer, with various morphological forms,
including spindle-shaped, oval-shaped, flat-shaped, triangular and
irregular cell bodies. Cells exhibited strong refraction and
possessed >2 processes, some of which connected to each other,
showing nucleus and nucleolus. When the cells were confluent, they
were observed to grow in a parallel or spiral manner (Fig. 1).
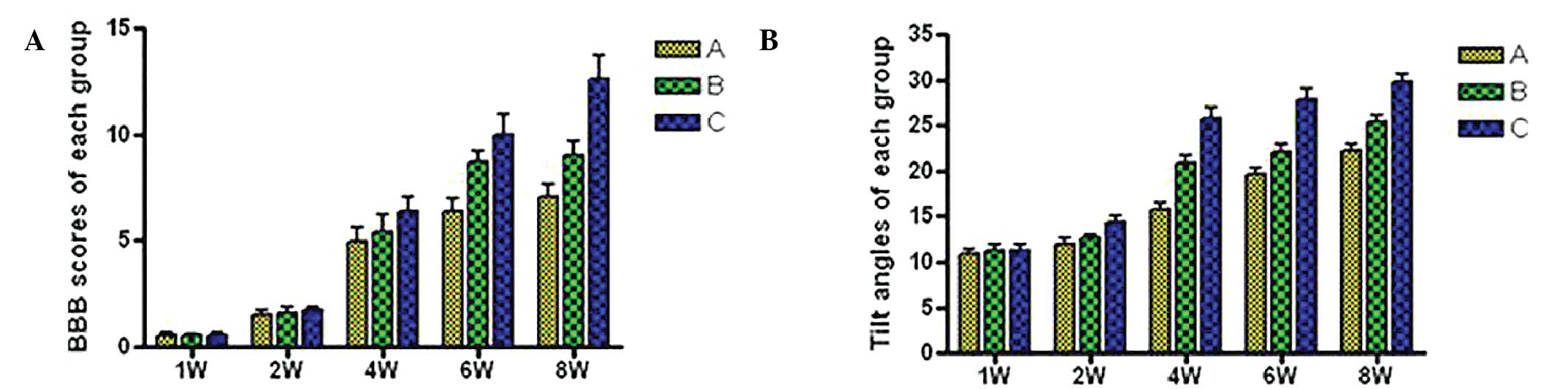
BBB scores
Following SCI, rats manifested full monoplegia with
no activity of the right hind limb or tail, and urinary dysfunction
but no dysfunction of defecation. The retraction to the puncture,
including the manifestation of the movement from contraction to
stretch of hind legs, began to emerge at 1 week post-injury. Hind
limb movement occurred at 2 weeks post-injury and became
increasingly evident at 4 weeks. Hind limbs demonstrated
coordination of activities at 6 weeks and urinary function was
partially restored, although there was still residual urine in the
bladder. The three groups exhibited the same changes following
injury. BBB scores in groups B and C were higher than those in
group A. At 4 weeks post-injury, group C scores were significantly
higher that those from group A (P<0.01) and group B (P<0.05;
Table I, Fig. 2A).
 | Table IBBB scores of each group at different
time points following spinal cord injury. |
Table I
BBB scores of each group at different
time points following spinal cord injury.
| BBB score |
|---|
|
|
|---|
| Group | 1 week | 2 weeks | 4 weeks | 6 weeks | 8 weeks |
|---|
| A | 0.54±0.15 | 1.49±0.28 |
4.97±0.68a |
6.39±0.59a |
7.03±0.61a |
| B | 0.53±0.12 | 1.62±0.23 |
5.42±0.83b |
8.68±0.52b |
9.04±0.62b |
| C | 0.54±0.11 | 1.73±0.14 |
6.39±0.67a,b |
9.98±0.64a,b |
12.62±0.73a,b |
Incline plate test
At 4 weeks post-injury, scores from group C were
significantly higher than those from group A (25.8±1.1 compared
with 15.7±0.8°, P<0.05) and from group B (25.8±1.1 compared with
20.9±0.9°, P<0.05). Scores from group B were also significantly
higher than those from group A (20.9±0.9 compared with 15.7±0.8,
P<0.05). At 6 weeks post-injury, there remained significant
differences between groups A and C (P<0.01) and between groups B
and C (P<0.05). These results suggest that mild hypothermia in
combination with NSC transplantation is superior to NSC
transplantation alone in terms of functional motor recovery
following SCI (Table II, Fig. 2B).
 | Table IITilt angles of each group at
different time points following spinal cord injury. |
Table II
Tilt angles of each group at
different time points following spinal cord injury.
| Tilt angle (°) |
|---|
|
|
|---|
| Group | 1 week | 2 weeks | 4 weeks | 6 weeks | 8 weeks |
|---|
| A | 10.8±0.5 | 12.0±0.6 |
15.7±0.8a |
19.6±0.8a |
22.2±0.8a |
| B | 11.2±0.7 | 12.6±0.4 |
20.9±0.9b |
22.1±0.9b |
25.4±0.7b |
| C | 11.3±0.6 | 14.4±0.7 |
25.8±1.1a,b |
27.8±1.2a,b |
29.7±1.0a,b |
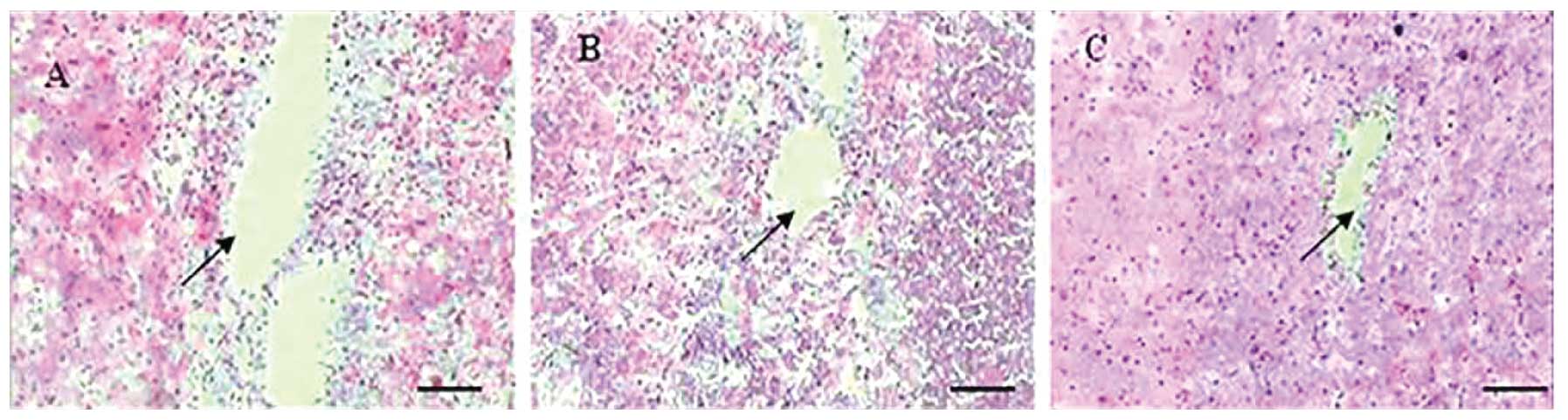
Histological analysis and
immunocytochemistry
At 4 weeks following injury, spinal cord tissue
damage, scarless healing and structural disorder were visible at
the affected site in group A, with a clear cavity formation
(Fig. 3A). In group B, astrocytes
aggregated at the edge of the affected site and formed scars at the
junction between the intact and damaged sections of the spinal
cord. The cavity in group B was smaller than in group A but larger
than in group C (Fig. 3B). In
group C, astrocytes underwent reactive hypertrophy, aggregated and
formed scars at the edge of the affected site. A number of cells
were spindle-shaped, with a dense network between processes. The
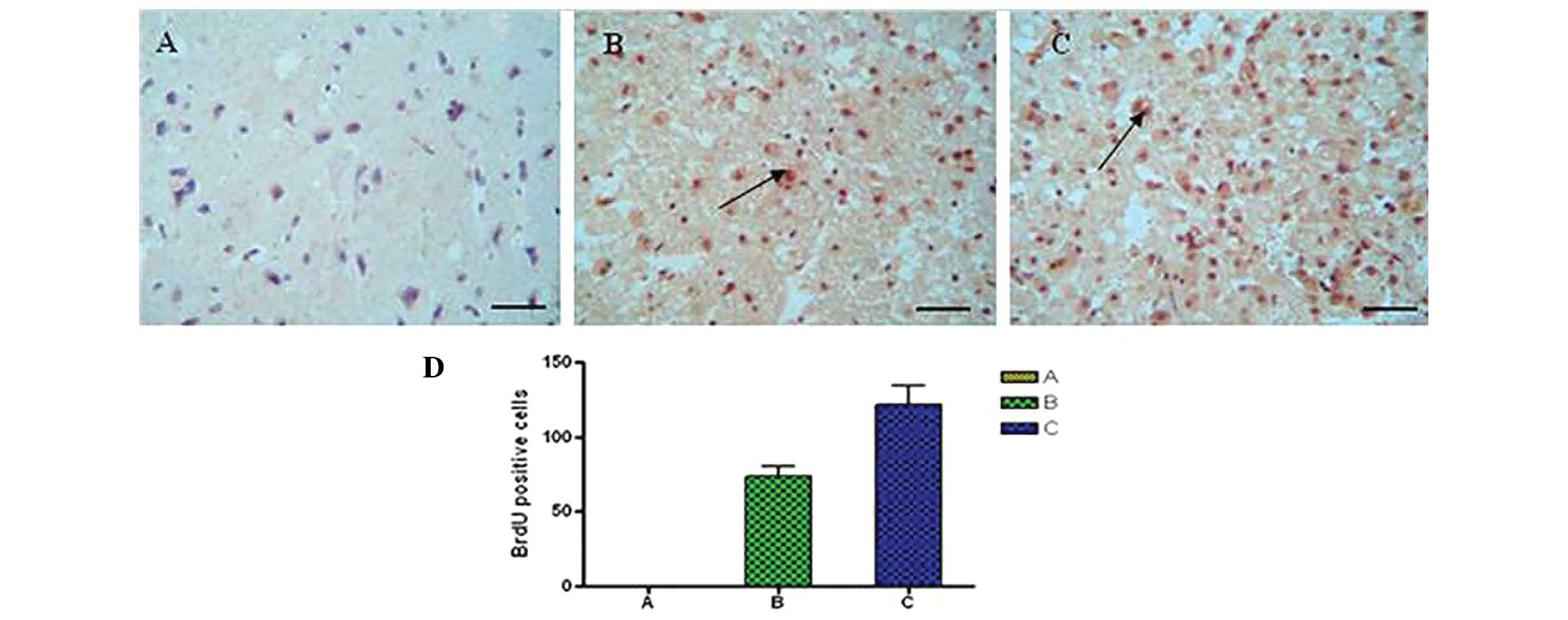
cavities were not visible in this group (Fig. 3C). Immunohistochemical staining
showed the number of BrdU-positive cells in tissues from the SCI
lesions (Fig. 4). Using analysis
of variance and Dunnett’s t-test, the number of BrdU-positive cells
in group C (Fig. 4C) was found to
be significantly increased compared with group B (Fig. 4B; P<0.05), and compared with
group A (Fig. 4A; P<0.01), at 4
weeks post-injury.
HRP retrograde nerve tracing
DAB color reaction was performed according to
manufacturer’s instructions (Shanghai ZiYi Co., Ltd.). A central
area of deeply-stained tissue and a surrounding area of less
strongly-stained tissue was observed at the injection site. In
group A, rats were injected with HRP through the lumbar
intumescentia. Two days after HRP injection, the HRP had been
transported in a retrograde direction for groups A and B. In
segments T8 and above few HRP-positively labeled nerve fibers were
observed (Fig. 5A). In group B,
HRP-positive nerve fibers were also observed, and there were fewer
fibers in group C, although more than in group A (Fig. 5B). Group C exhibited a large
quantity of HRP-positive granule-labeled nerve fibers in the spinal
cord (Fig. 5C). The number of
HRP-positive nerve fiber bundles in rat SCI tissues from each group
is shown in Fig. 5D). There were
significant differences among the three groups at 8 weeks
post-injury (P<0.01).
Transmission electron microscopy
Transmission electron microscopy results showed the
glial scar and a small number of myelinated nerve fibers in group
A, along with macrophage phagocytosis and degeneration, and
necrotic myelinated nerve fibers (Fig.
6A). A large number of myelinated and non-myelinated nerve
fibers were observed in group C, which had more axons and intact
myelin as compared with the other groups (Fig. 6B). The number of myelinated and
non-myelinated nerve fibers at the injury site in group B was
greater than that in group A and less than that in group C
(Fig. 6C).
Discussion
Central nervous system regeneration is a complex
area of theoretical research and clinical practice in the fields of
neuroscience and medicine, and an effective treatment for damage to
the nervous system has not yet been developed. Central nervous
system injury is primarily a result of trauma, including cerebral
cortex impairment or loss of function and paralysis as a result of
SCI (14–16). Recently, with the development of
stem cell research, NSC transplantation for the treatment of
neurological diseases has become a significant focus in medical
research (17–19). NSCs have a number of superior
qualities as compared to neurons, such as ease of harvesting,
well-developed methods for cell separation, culture, amplification
and exogenous gene transfection, and the feasibility of autologous
implantation following in vitro amplification or genetic
engineering modification, without encountering ethical issues or
immune rejection. NSC transplantation has been shown to effectively
treat nervous system injury in a previous study (20). Its mechanisms of action are
diverse. NSCs exhibit a high expansion potential, genetic stability
and a stable phenotype. They are easily collected and transported,
and are compatible with different delivery methods and formulations
(21). In addition, NSCs have two
other important characteristics: They are able to migrate to sites
of tissue injury and they have strong immunosuppressive properties
that can be exploited for successful autologous or heterologous
transplantation without the requirement for pharmacological
immunosuppression (22,23). NSCs are capable of differentiating
into neurons and astrocytes in vitro and in vivo
(24). Recently, NSC injection has
shown promising results in the treatment of amyotrophic lateral
sclerosis in humans (25). They
have been shown to improve neurological deficits and promote the
development of neuronal networks with functional synaptic
transmission, when transplanted into animal models of neurological
disorders, such as nerve dysfunction (26). NSCs have been observed to migrate
to injured tissues and to mediate functional recovery following
brain, spinal cord and peripheral nerve lesions (27).
In recent years, mild hypothermia (33–35°C) has
received increasing attention in the treatment of central nervous
system injury. A previous clinical study showed that mild
hypothermia effectively reduces secondary nerve injury and protects
against severe traumatic brain injury (28). The mechanisms underlying this
protective effect may include reducing the release of excitatory
amino acids, inhibiting calcium influx, regulating calmodulin
kinase II and protein kinase C activity, inhibiting the
inflammatory response following cerebral ischemia, suppressing
edema formation, reducing the oxygen metabolic rate, diminishing
the production of free radicals, and inhibiting necrosis and
neuronal apoptosis induced by mitochondrial release of cytochrome
c (29–31). In the present study, the effect of
mild hypothermia combined with NSC transplantation on SCI in rats
was investigated. The results showed that NSC transplantation
combined with mild hypothermia was superior to NSC transplantation
alone, in the treatment of SCI in rats, as evaluated by changes in
histology and functional recovery.
The synergistic effect of hypothermia and NSC
transplantation may be due to the fact that hypothermia improves
the microenvironment of the injured spinal cord. An important
mechanism underlying the neuroprotective effects of hypothermia is
a reduction or delay in metabolic consumption during the period of
stress experienced by the injured spinal cord (32–36).
The hemodynamic consequences of cooling the spinal cord are
important, as reductions in blood flow to critical levels caused by
profound cooling may have adverse effects on tissue preservation
and thus on functional outcome (37–39).
It is clear that the neurotransmitter response in various types of
SCI models may be temperature-dependent, but that attenuating other
injury cascade may be more important in subserving the beneficial
effects of hypothermia (40–43).
Alterations in blood-brain barrier permeability following ischemia
and trauma are an important vascular consequence that leads to the
passage of water, blood-borne exogenous substances and potential
neurotoxic agents across the vascular system and into the brain
parenchyma. Microvascular perturbations including blood-brain
barrier permeability, the formation of vasogenic edema and the
extravasation of circulating inflammatory cells may adversely
affect injury outcome. The effects of hypothermia on the
vasculature comprise an important mechanism contributing to the
beneficial effects of hypothermia (44–47).
There are also pronounced changes in calcium-dependent
intracellular signaling pathways following SCI. The neuronal
cytoskeleton is highly vulnerable to injury, resulting in beading
of dendrites and degeneration of axons, changes that are reversed
by hypothermia. This effect is likely to be mediated by the
inhibition of calpain activity, a calcium-dependent protease
(48–52). Attenuation of inflammation is one
of the major mechanisms by which hypothermia leads to beneficial
effects in SCI. The inflammatory response following SCI is known to
be significantly attenuated by hypothermia. In addition to
attenuating the disruption of the blood-brain barrier and the
extravasation of infiltrating inflammatory cells and neurotoxic
substances, the endogenous inflammatory response induced by SCI is
also reduced by hypothermia (53–55).
Evidence for apoptotic cell death has been demonstrated in various
models of SCI. Although neuronal necrosis is commonly observed in
injury models, evidence for apoptotic cell death in CNS injury has
also been documented using various histochemical and molecular
techniques. As with necrosis, apoptotic cell death appears to be
sensitive to post-injury hypothermic treatment strategies. Using
terminal deoxynucleotidetransferase-mediated dUTP-biotin nick end
labeling staining, DNA fragmentation has been found to be reduced
by hypothermia in SCI (56–59).
Recent studies have utilized various genetic markers in order to
evaluate the effects of temperature on molecular events associated
with SCI. Families of genes associated with inflammation, apoptosis
and other cell signaling cascades are known to be reduced or
elevated when brain temperature is lowered. The ability of
post-injury temperature to affect the acute and delayed genetic
responses to injury is important, as these genes may be important
in determining the proteomic response that results in secondary
injury (60–63).
In conclusion, NSC transplantation in combination
with mild hypothermia may promote the survival, proliferation,
differentiation and migration of the transplanted cells at the
injury site, as well as promoting the restoration of nerve function
in rats with SCI. This therapy provides novel strategies and
methods for the clinical treatment of SCI.
Acknowledgements
This study was sponsored by the Application Basis
and Front Technology Projects of Tianjin (Science and Technology
Foundation of Tianjin, No. 12JCYBJC18000.
References
|
1
|
Ku JH: The management of neurogenic
bladder and quality of life in spinal cord injury. BJU Int.
98:739–745. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Papadopoulos SM, Selden NR, Quint DJ,
Patel N, Gillespie B and Grube S: Immediate spinal cord
decompression for cervical spinal cord injury: feasibility and
outcome. J Trauma. 52:323–332. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Harrop JS, Sharan AD, Vaccaro AR and
Przybylski GJ: The cause of neurologic deterioration after acute
cervical spinal cord injury. Spine (Phila Pa 1976). 26:340–346.
2001. View Article : Google Scholar
|
|
4
|
Beck KD, Nguyen HX, Galvan MD, Salazar DL,
Woodruff TM and Anderson AJ: Quantitative analysis of cellular
inflammation after traumatic spinal cord injury: evidence for a
multiphasic inflammatory response in the acute to chronic
environment. Brain. 133:433–447. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Furuya T, Hashimoto M, Koda M, Okawa A,
Murata A, Takahashi K, Yamashita T and Yamazaki M: Treatment of rat
spinal cord injury with a Rho-kinase inhibitor and bone marrow
stromal cell transplantation. Brain Res. 1295:192–202. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Ohta M, Suzuki Y, Noda T, Ejiri Y, Dezawa
M, Kataoka K, Chou H, Ishikawa N, Matsumoto N, Iwashita Y, Mizuta
E, Kuno S and Ide C: Bone marrow stromal cells infused into the
cerebrospinal fluid promote functional recovery of the injured rat
spinal cord with reduced cavity formation. Exp Neurol. 187:266–278.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Gu Y, Wang J, Ding F, Hu N, Wang Y and Gu
X: Neurotrophic actions of bone marrow stromal cells on primary
culture of dorsal root ganglion tissues and neurons. J Mol
Neurosci. 40:332–341. 2010. View Article : Google Scholar
|
|
8
|
Nguyen HP, Zaroff JG, Bayman EO, et al:
Perioperative hypothermia (33 degrees C) does not increase the
occurrence of cardiovascular events in patients undergoing cerebral
aneurysm surgery: findings from the Intraoperative Hypothermia for
Aneurysm Surgery Trial. Anesthesiology. 113:327–342. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Kobbe P, Lichte P, Wellmann M, Hildebrand
F, Nast-Kolb D, Waydhas C and Oberbeck R: Impact of hypothermia on
the severely injured patient. Unfallchirurg. 112:1055–1061.
2009.(In German). View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Huang T, Solano J, He D, Loutfi M,
Dietrich WD and Kuluz JW: Traumatic injury activates MAP kinases in
astrocytes: mechanisms of hypothermia and hyperthermia. J
Neurotrauma. 26:1535–1545. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Dimar II Jr, Shields CB, Zhang YP, Burke
DA, Raque GH and Glassman SD: The role of directly applied
hypothermia in spinal cord injury. Spine (Phila Pa 1976).
25:2294–2302. 2000. View Article : Google Scholar
|
|
12
|
Kwon BK, Mann C, Sohn HM, Hilibrand AS,
Phillips FM, Wang JC and Fehlings MG: NASS Section on Biologics:
Hypothermia for spinal cord injury. Spine J. 8:859–874. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Dietrich WD, Atkins CM and Bramlett HM:
Protection in animal models of brain and spinal cord injury with
mild to moderate hypothermia. J Neurotrauma. 26:301–312. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Cao QL, Howard RM, Dennison JB and
Whittemore SR: Differentiation of engrafted neuronal-restricted
precursor cells is inhibited in the traumatically injured spinal
cord. Exp Neurol. 177:349–359. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Carvalho KA, Vialle EN, Moreira GH, Cunha
RC, Simeoni RB, Francisco JC, Guarita-Souza LC, Oliveira L, Zocche
L and Olandoski M: Functional outcome of bone marrow stem cells
(CD45(+)/CD34(−)) after cell therapy in chronic spinal cord injury
in Wistar rats. Transplant Proc. 40:845–846. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Sun Z, Wen Y, Mao Q, Hu L, Li H, Sun Z and
Wang D: Adenosine-triphosphate promoting repair of spinal cord
injury by activating mammalian target of rapamycin/signal
transducers and activators of transcription 3 signal pathway in
rats. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 24:165–171.
2010.(In Chinese). PubMed/NCBI
|
|
17
|
Bhang SH, Lee YE, Cho SW, Shim JW, Lee SH,
Choi CY, Chang JW and Kim BS: Basic fibroblast growth factor
promotes bone marrow stromal cell transplantation-mediated neural
regeneration in traumatic brain injury. Biochem Biophys Res Commun.
359:40–45. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Theus MH, Wei L, Cui L, Francis K, Hu X,
Keogh C and Yu SP: In vitro hypoxic preconditioning of embryonic
stem cells as a strategy of promoting cell survival and functional
benefits after transplantation into the ischemic rat brain. Exp
Neurol. 210:656–670. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Hwang DH, Shin HY, Kwon MJ, Choi JY, Ryu
BY and Kim BG: Survival of neural stem cell grafts in the lesioned
spinal cord is enhanced by a combination of treadmill locomotor
training via insulin-like growth factor-1 signaling. J Neurosci.
34:12788–12800. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Shen LH, Li Y, Gao Q, Savant-Bhonsale S
and Chopp M: Down-regulation of neurocan expression in reactive
astrocytes promotes axonal regeneration and facilitates the
neurorestorative effects of bone marrow stromal cells in the
ischemic rat brain. Glia. 56:1747–1754. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Giordano A, Galderisi U and Marino IR:
From the laboratory bench to the patient’s bedside: an update on
clinical trials with mesenchymal stem cells. J Cell Physiol.
211:27–35. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Le Blanc K and Pittenger M: Mesenchymal
stem cells: progress toward promise. Cytotherapy. 7:36–45. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Beggs KJ, Lyubimov A, Borneman JN,
Bartholomew A, Moseley A, Dodds R, Archambault MP, Smith AK and
McIntosh KR: Immunologic consequences of multiple, high-dose
administration of allogeneic mesenchymal stem cells to baboons.
Cell Transplant. 15:711–721. 2006. View Article : Google Scholar
|
|
24
|
Jori FP, Napolitano MA, Melone MA,
Cipollaro M, Cascino A, Altucci L, Peluso G, Giordano A and
Galderisi U: Molecular pathways involved in neural in vitro
differentiation of marrow stromal stem cells. J Cell Biochem.
94:645–655. 2005. View Article : Google Scholar
|
|
25
|
Mazzini L, Mareschi K, Ferrero I, Vassallo
E, Oliveri G, Nasuelli N, Oggioni GD, Testa L and Fagioli F: Stem
cell treatment in Amyotrophic Lateral Sclerosis. J Neurol Sci.
265:78–83. 2008. View Article : Google Scholar
|
|
26
|
Bae JS, Han HS, Youn DH, Carter JE, Modo
M, Schuchman EH and Jin HK: Bone marrow-derived mesenchymal stem
cells promote neuronal networks with functional synaptic
transmission after transplantation into mice with
neurodegeneration. Stem Cells. 25:1307–1316. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Chen G, Hu YR, Wan H, Xia L, Li JH, Yang
F, Qu X, Wang SG and Wang ZC: Functional recovery following
traumatic spinal cord injury mediated by a unique polymer scaffold
seeded with neural stem cells and Schwann cells. Chin Med J (Engl).
123:2424–2431. 2010.
|
|
28
|
Li XH, Chen Z, Xia Zhao, Liang HQ, Zhao
ML, Zhang S and Tu Y: Hypothermia in rats after traumatic brain
injury within the endogenous neural stem cell proliferation and
differentiation and its mechanism. Zhonghua Chuang Shang Za Zhi.
30:500–503. 2014.
|
|
29
|
Lyden PD, Krieger D, Yenari M and Dietrich
WD: Therapeutic hypothermia for acute stroke. Int J Stroke. 1:9–19.
2006. View Article : Google Scholar
|
|
30
|
Deng H, Han HS, Cheng D, Sun GH and Yenari
MA: Mild hypothermia inhibits inflammation after experimental
stroke and brain inflammation. Stroke. 34:2495–2501. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Schwab S, Georgiadis D, Berrouschot J,
Schellinger PD, Graffagnino C and Mayer SA: Feasibility and safety
of moderate hypothermia after massive hemispheric infarction.
Stroke. 32:2033–2035. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Tohyama Y, Sako K and Yonemasu Y:
Hypothermia attenuates hyperglycolysis in the periphery of ischemic
core in rat brain. Exp Brain Res. 122:333–338. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Kaibara T, Sutherland GR, Colbourne F and
Tyson RL: Hypothermia: depression of tricarboxylic acid cycle flux
and evidence for pentose phosphate shunt upregulation. J Neurosurg.
90:339–347. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Lo EH and Steinberg GK: Effects of
hypothermia on evoked potentials, magnetic resonance imaging, and
blood flow in focal ischemia in rabbits. Stroke. 23:889–893. 1992.
View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Sutton LN, Clark BJ, Norwood CR, Woodford
EJ and Welsh FA: Global cerebral ischemia in piglets under
conditions of mild and deep hypothermia. Stroke. 22:1567–1573.
1991. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Jiang JY, Liang YM, Luo QZ and Zhu C:
Effect of mild hypothermia on brain dialysate lactate after fluid
percussion brain injury in rodents. Neurosurgery. 54:713–718. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Rosomoff HL and Holaday DA: Cerebral blood
flow and cerebral oxygen consumption during hypothermia. Am J
Physiol. 179:85–88. 1954.PubMed/NCBI
|
|
38
|
Kuluz JW, Prado R, Chang J, Ginsberg MD,
Schleien CL and Busto R: Selective brain cooling increases cortical
cerebral blood flow in rats. Am J Physiol. 265:H824–H827.
1993.PubMed/NCBI
|
|
39
|
Hansebout RR, Lamont RN and Kamath MV: The
effects of local cooling on canine spinal cord blood flow. Can J
Neurol Sci. 12:83–87. 1985.PubMed/NCBI
|
|
40
|
Baker AJ, Zornow MH, Grafe MR, Scheller
MS, Skilling SR, Smullin DH and Larson AA: Hypothermia prevents
ischemia-induced increases in hippocampal glycine concentrations in
rabbits. Stroke. 22:666–673. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Rokkas CK, Cronin CS, Nitta T, Helfrich LR
Jr, Lobner DC, Choi DW and Kouchoukos NT: Profound systemic
hypothermia inhibits the release of neurotransmitter amino acids in
spinal cord ischemia. J Thorac Cardiovasc Surg. 110:27–35. 1995.
View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Zausinger S, Westermaier T, Plesnila N,
Steiger HJ and Schmid-Elsaesser R: Neuroprotection in transient
focal cerebral ischemia by combination drug therapy and mild
hypothermia: comparison with customary therapeutic regimen. Stroke.
34:1526–1532. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Zhu H, Meloni BP, Bojarski C, Knuckey MW
and Knuckey NW: Post-ischemic modest hypothermia (35 degrees C)
combined with intravenous magnesium is more effective at reducing
CA1 neuronal death than either treatment used alone following
global cerebral ischemia in rats. Exp Neurol. 193:361–368. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Dietrich WD, Busto R, Halley M and Valdes
I: The importance of brain temperature in alterations of the blood
brain barrier following cerebral ischemia. J Neuropathol Exp
Neurol. 49:486–497. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Huang ZG, Xue D, Preston E, Karbalai H and
Buchan AM: Biphasic opening of the blood-brain barrier following
transient focal ischemia: effects of hypothermia. Can J Neurol Sci.
26:298–304. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Arican N, Kaya M, Yorulmaz C, Kalayci R,
Ince H, Kucuk M, Fincanci SK and Elmas I: Effect of hypothermia on
blood-brain barrier permeability following traumatic brain injury
in chronically ethanol-treated rats. Int J Neurosci. 116:1249–1261.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Nagel S, Su Y, Horstmann S, Heiland S,
Gardner H, Koziol J, Martinez-Torres FJ and Wagner S: Minocycline
and hypothermia for reperfusion injury after focal cerebral
ischemia in the rat: effects on BBB breakdown and MMP expression in
the acute and subacute phase. Brain Res. 1188:198–206. 2008.
View Article : Google Scholar
|
|
48
|
Hu BR, Kamme F and Wieloch T: Alterations
of Ca2+/calmodulin-dependent protein kinase II and its
messenger RNA in the rat hippocampus following normo- and
hypothermic ischemia. Neuroscience. 68:1003–1016. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Churn SB, Taft WC, Billingsley MS, Blair
RE and DeLorenzo RJ: Temperature modulation of ischemic neuronal
death and inhibition of calcium/calmodulin-dependent protein kinase
II in gerbils. Stroke. 21:1715–1721. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Shimohata T, Zhao H and Steinberg GK:
Epsilon PKC may contribute to the protective effect of hypothermia
in a rat focal cerebral ischemia model. Stroke. 38:375–380. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Atkins CM, Oliva AA Jr, Alonso OF, Chen S,
Bramlett HM, Hu BR and Dietrich WD: Hypothermia treatment
potentiates ERK1/2 activation after traumatic brain injury. Eur J
Neurosci. 26:810–819. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Shimohata T, Zhao H, Sung JH, Sun G,
Mochly-Rosen D and Steinberg GK: Suppression of deltaPKC activation
after focal cerebral ischemia contributes to the protective effect
of hypothermia. J Cereb Blood Flow Metab. 27:1463–1475. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Ha KY and Kim YH: Neuroprotective effect
of moderate epidural hypothermia after spinal cord injury in rats.
Spine (Phila Pa 1976). 33:2059–2065. 2008. View Article : Google Scholar
|
|
54
|
Morino T, Ogata T, Takeba J and Yamamoto
H: Microglia inhibition is a target of mild hypothermic treatment
after the spinal cord injury. Spinal Cord. 46:425–431. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Fukui O, Kinugasa Y, Fukuda A, Fukuda H,
Tskitishvili E, Hayashi S, Song M, Kanagawa T, Hosono T, Shimoya K
and Murata Y: Post-ischemic hypothermia reduced IL-18 expression
and suppressed microglial activation in the immature brain. Brain
Res. 1121:35–45. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Brodhun M, Fritz H, Walter B,
Antonow-Schlorke I, Reinhart K, Zwiener U, Bauer R and Patt S:
Immunomorphological sequelae of severe brain injury induced by
fluid-percussion in juvenile pigs - effects of mild hypothermia.
Acta Neuropathol. 101:424–434. 2001.PubMed/NCBI
|
|
57
|
Zhao H, Yenari MA, Sapolsky RM and
Steinberg GK: Mild postischemic hypothermia prolongs the time
window for gene therapy by inhibiting cytochrome C release. Stroke.
35:572–577. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Zhao H, Yenari MA, Cheng D, Sapolsky RM
and Steinberg GK: Biphasic cytochrome c release after transient
global ischemia and its inhibition by hypothermia. J Cereb Blood
Flow Metab. 25:1119–1129. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Zhao H, Wang JQ, Shimohata T, Sun G,
Yenari MA, Sapolsky RM and Steinberg GK: Conditions of protection
by hypothermia and effects on apoptotic pathways in a rat model of
permanent middle cerebral artery occlusion. J Neurosurg.
107:636–641. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Shibuya S, Miyamoto O, Janjua NA, Itano T,
Mori S and Norimatsu H: Post-traumatic moderate systemic
hypothermia reduces TUNEL positive cells following spinal cord
injury in rat. Spinal Cord. 42:29–34. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Ohta H, Terao Y, Shintani Y and Kiyota Y:
Therapeutic time window of post-ischemic mild hypothermia and the
gene expression associated with the neuroprotection in rat focal
cerebral ischemia. Neurosci Res. 57:424–433. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Gressens P, Dingley J, Plaisant F, Porter
H, Schwendimann L, Verney C, Tooley J and Thoresen M: Analysis of
neuronal, glial, endothelial, axonal and apoptotic markers
following moderate therapeutic hypothermia and anesthesia in the
developing piglet brain. Brain Pathol. 18:10–20. 2008. View Article : Google Scholar
|
|
63
|
Kobayashi MS, Asai S, Ishikawa K, Nishida
Y, Nagata T and Takahashi Y: Global profiling of influence of
intra-ischemic brain temperature on gene expression in rat brain.
Brain Res Rev. 58:171–191. 2008. View Article : Google Scholar : PubMed/NCBI
|