Introduction
Severe acute pancreatitis (SAP) is a common acute
abdominal disease with rapid progression and high mortality rates
of ~20.8–36% (1,2), due to the lack of effective
treatments for SAP, its progression is often associated with local
or systemic inflammatory responses, and current treatment
strategies focus on ameliorating inflammatory cytokine activation
(3,4).
During the progression of SAP-induced systemic
inflammatory response syndrome, the release of high levels of
inflammatory mediators triggers the synthesis and release of
anti-inflammatory cytokines. Anti-inflammatory cytokines inhibit
pathogenic inflammation, however, they also precipitate the
systemic suppression of immune functions, particularly cellular
immunity directed against exogenous pathogens, resulting in the
development of compensatory anti-inflammatory response syndrome
(5). The precise association
between pro- and anti-inflammatory cytokine responses is difficult
to determine, however, numerous clinical studies have suggested
that SAP progression is closely associated with immune dysfunction
(4).
With the significance of immune function in the
pathophysiology of SAP being increasingly emphasized, immune
intervention has become an important aspect of SAP treatment. The
multifunctional cytokines, interferon α (IFNα) and thymosin α1
(TA1), have been used in the treatment of chronic cancer, immune
deficiencies and viral pancreatitis (6,7). TA1
is a polypeptide hormone with multiple bioactivities, including the
induction of T cell differentiation and maturation, promotion of
cytokine production and enhancement of the B cell antibody reaction
(6,8). IFNα is an endogenous immune regulator
and antiviral agent, which has an important regulatory role in T
cell activation and cytokine release (9). However, the effects of TA1 and IFNα
on SAP remain to be elucidated. The present study aimed to
investigate the effects of TA1 and IFNα on cellular immune
functions in a rat model of SAP, and to establish an experimental
basis for the further administration of TA1 and IFNα in SAP.
Materials and methods
Animals and treatment
All experiments were performed with the consent of
the University Animal Care and Usage Committee of the Experimental
Animals Center of Xi'an Jiaotong University (Xi'an, China). A total
of 144 Sprague-Dawley rats (aged 8–10 weeks, weighing 200–250 g)
were provided by the Medical Experimental Animal Center of Xi'an
Jiaotong University. The rats were fed and housed at 23±3°C, 40–50%
humidity, with a 12 h light/dark cycle and <60 dB interior
noise, were provided with free access to food and water.
The rats were randomly divided into four groups
(n=36/group). Animals were anesthetized by intraperitoneal
injection of and 10% chloral hydrate (320 mg/kg body weight). All
rats were celiotomized and, following pulling the pancreas out of
the body re-inserting it, the surgical incision was closed. The
control rats were administrated with an intravenous injection of
saline 0.5 h following the surgical procedure. The three other
groups of rats were administered with 5% 1 ml/kg sodium
taurocholate (Sigma-Aldrich, St. Louis, MO, USA) via the
cholangiopancreatic duct for 5 min, and the SAP group rats were
administered with saline by intravenous injection 0.5 h later. The
TA1 group rats received 26.7 µg/kg TA1 (American Science and
Engineering, Inc., Billerica, MA, USA) in the saline infusion. The
INFα group rats received 4.0×105 U/kg IFNα (Shanghai
Senxiong Biotech Industry Co., Ltd., Shanghai, China) in the saline
infusion. The rats were then anesthetized and blood samples (2 ml)
were collected from the inferior vena cava 3, 12 and 24 h following
surgery. Samples of the pancreatic and lung tissue were collected
at 2, 3, 12 and 24 h post-surgery by resection of the intact
pancreas and left middle lung tissue following celiotomy, and the
samples were stained with hematoxylin and eosin (HE; GefanBio Co.
Ltd, Shanghai, China). After 24 h, the mortality and survival rates
were recorded for a further 24 h. The general conditions of the
rats were also observed, including mental status, physical
activity, water consumption and hair smoothness.
The present study was approved by the ethics
committee of the First Affiliated Hospital of Medical School, Xi'an
Jiaotong University (Xi'an, China).
T cell subpopulation detection
The lymphocytes were separated from the heparinized
venous blood by density gradient centrifugation (500 x g for 20 min
at 4°C) using Ficoll-Hypaque (GE Healthcare Bio-Sciences,
Pittsburg, PA, USA), resuspended in phosphate-buffered saline (PBS)
and incubated with fluorescein isothiocyanate-conjugated anti-CD3
(cat no. sc-20047 monoclonal mouse anti-human; 1/1,000 dilution),
phycoerythrin-conjugated anti-CD4 (cat no. sc-19642; monoclonal rat
anti-mouse; 1/1,000 dilution) or allophycocyanin-conjugated
anti-CD8 (cat no. sc-18913; monoclonal rat anti-mouse; 1/1,000
dilution) (all from Santa Cruz Biotechnology, Inc., Dallas, TX,
USA) at 4°C for 15 min. Appropriately conjugated isotype-matched
antibodies were used as controls. Populations of fluorescent cells
(1×104/sample) were measured using a CyFlow®
ML flow cytometer (Sysmex Europe GmbH, Norderstedt, Germany)
following two washes with PBS.
Serum enzyme assay
Anticoagulant-free blood (5 ml) was centrifuged
(1,700 x g, 18°C, 4 min), and the serum was collected for the
measurement of the levels of aspartate transaminase (AST), lactate
dehydrogenase (LDH), α-amylase (AMY), lipase (LPS) and P-type
amylase (P-AMY) using an Olympus AU5400 automatic biochemical
analyzer (Olympus Corporation, Tokyo, Japan).
Cytokine and procalcitonin (PCT)
assay
The serum expression levels of tumor necrosis factor
α (TNFα), interleukin (IL)-4, IL-5, IL-6, IL-18 and PCT were
detected by ELISA using a commercial BD OptEIATM ELISA kit (BD
Biosciences, San Jose, CA, USA), according to the manufacturer's
instructions. The sensitivities for TNFα and the ILs were 15 and 5
pg/ml, respectively.
Histological examination
The tail of the pancreas and the left superior lobe
of the lung were fixed with 5% paraformaldehyde (Dingguo Changsheng
Biotechnology Co. Ltd, Beijing, China), dehydrated and embedded in
paraffin wax (GefanBio Co. Ltd). Sections (3 mm thick) were cut,
dewaxed and stained with HE for histological examination using a
BX-5D1TF microscope (Olympus, Tokyo, Japan). The pathological
scores of pancreatitis (10) and
lung tissue samples (11) were
evaluated. For the pancreatic tissue samples, a scale of 0–4 was
used for interstitial edema and hemorrhage, inflammatory cell
infiltration and acinar cell vacuolization and necrosis, consistent
with the improved scoring method, described by Sharif et al
(10). For the lung tissue
samples, a scale of 0–3 was used for interstitial edema and
hemorrhage, and inflammatory cell infiltration, consistent with a
method previously described by Chooklin (11). The assessment was performed by two
experienced pathologists in a blinded-manner. Disagreements in
scoring were resolved by discussion.
Statistical analysis
Statistical analysis was performed using SPSS 13.0
(SPSS, Inc., Chicago, IL, USA). The data are presented as the mean
± standard deviation. Statistical differences were evaluated using
one-way analysis of variance and a least significant difference
test. Spearman's linear correlation analysis was used for
correlation analysis. Survival rates were compared between groups
using Kaplan-Meier survival curves and a Log-rank test. P<0.05
was considered to indicate a statistically significant
difference.
Results
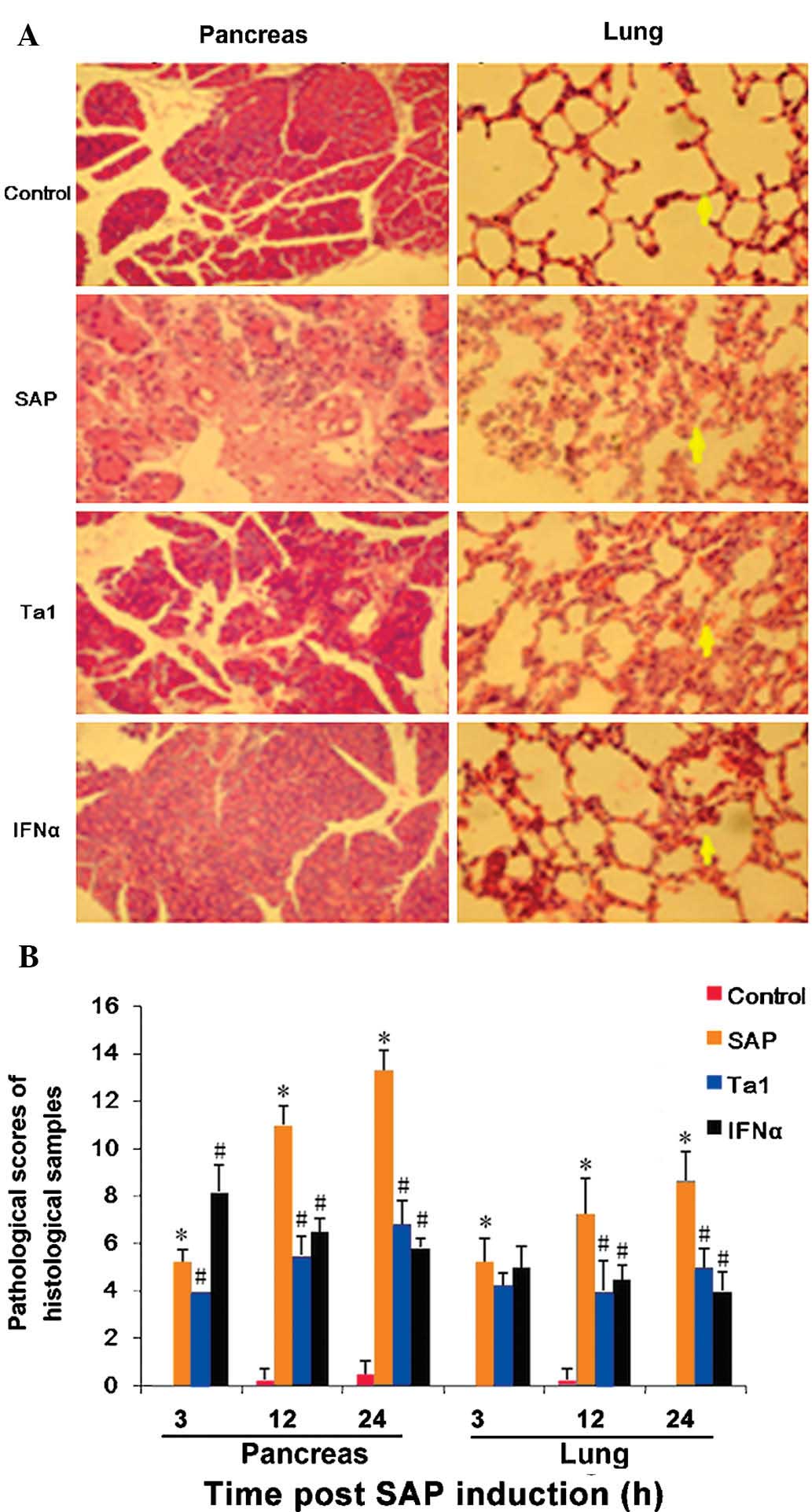
Expression levels of serum enzymes in the
different treatment groups
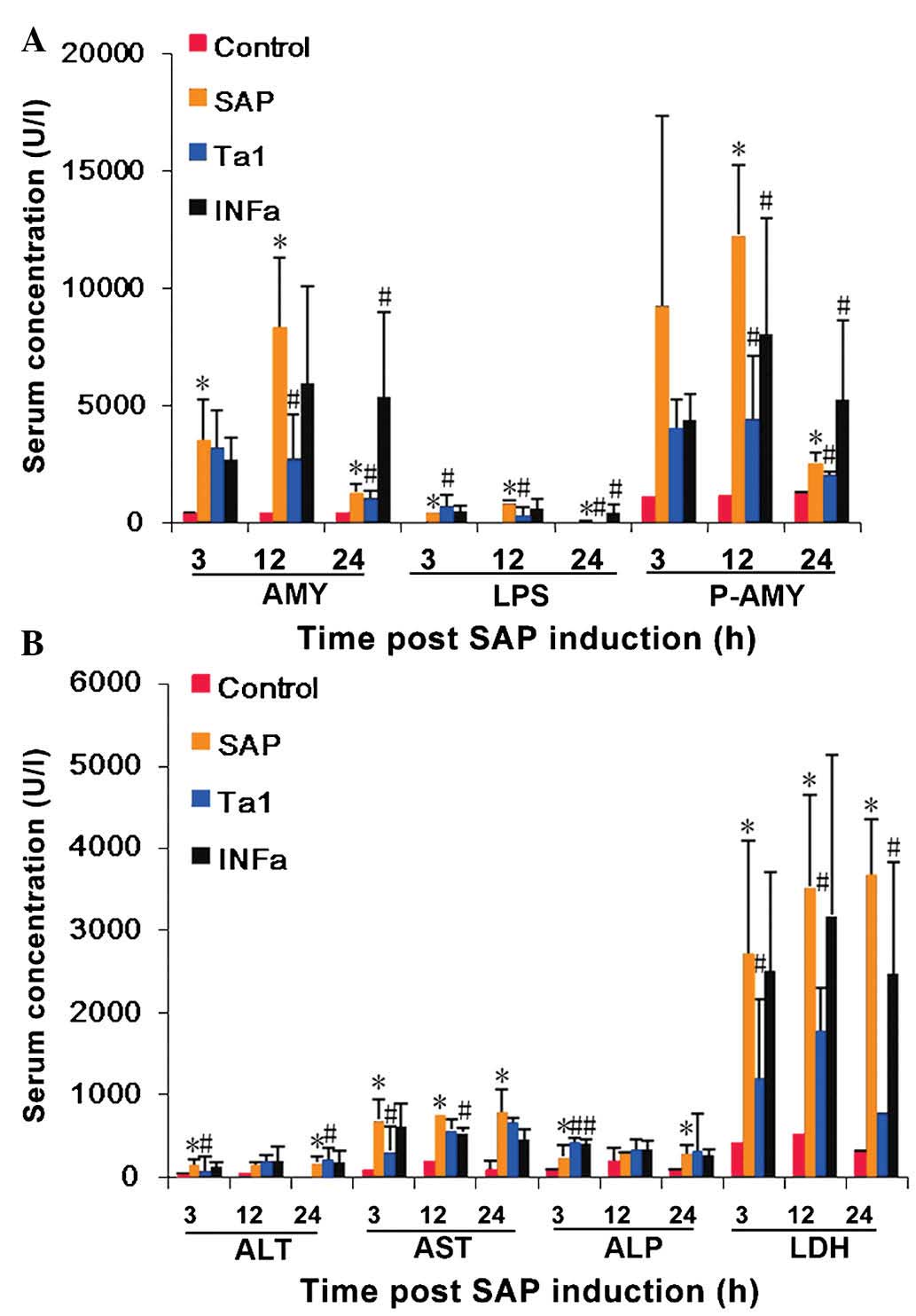
Circulating expression levels of AMY, LPS and P-AMY
were significantly higher in the rats in the SAP group, compared
with the rats in the control group. The highest expression levels
observed ~12 h following celiotomy and remained elevated for a
further 12 h (P<0.05, Fig. 1A)
indicating pancreatic damage. Elevated expression levels of AST and
LDH were also observed 3, 12 and 24 h following SAP induction
(P<0.05; Fig. 1B), These
results suggested that multiple organ damage was induced by
SAP.
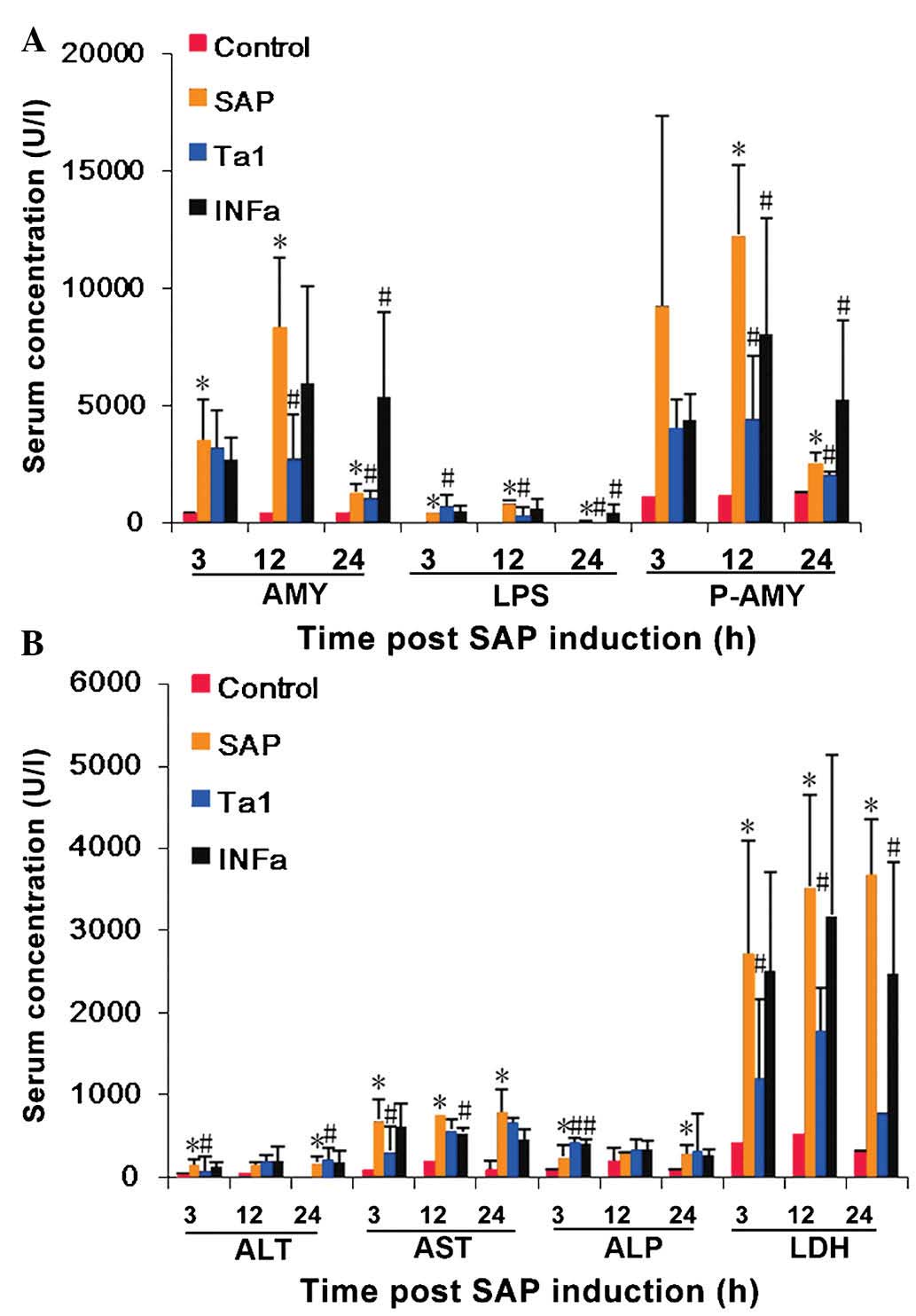 | Figure 1Detection of organ damage in rats
following SAP induction and TA1 or INFα treatment. A total of 144
Sprague-Dawley rats, randomly divided into four groups (n=36), were
celiotomized and three groups were administered with sodium
taurocholate to induce SAP. These rats were then administered
saline, TA1 or INFα, and blood samples were collected over the
following 24 h. (A) Serum levels of ALT, AST, ALP, and LHD were
measured using an automatic biochemical analyzer. (B) Serum levels
of LPS, AMY and P-AMY were analyzed using ELISA. The data are
presented as the mean ± standard deviation.*P<0.05,
vs. control group; #P<0.05, vs. SAP group. SAP,
severe acute pancreatitis; TA1, thymosin α1; IFNα, interferon α;
ALT, alanine aminotransferase; AST, aspartate transaminase; ALP,
alkaline phosphatase; LDH, lactate dehydrogenase; LPS, lipase; AMY,
α-amylase; P-AMY, P-type-amylase. |
Although the concentration levels of AMY, LPS and
P-AMY in the TA1 group rats were higher than those of the control
group rats, they were significantly lower, compared with those of
the SAP group 3, 12 and 24 h post-SAP induction (P<0.05;
Fig. 1A). The expression levels of
circulating AMY, LPS and P-AMY were also lower in the INFα group 12
h following SAP induction (P<0.05; Fig. 2).
Levels of serum cytokines following
celiotomy
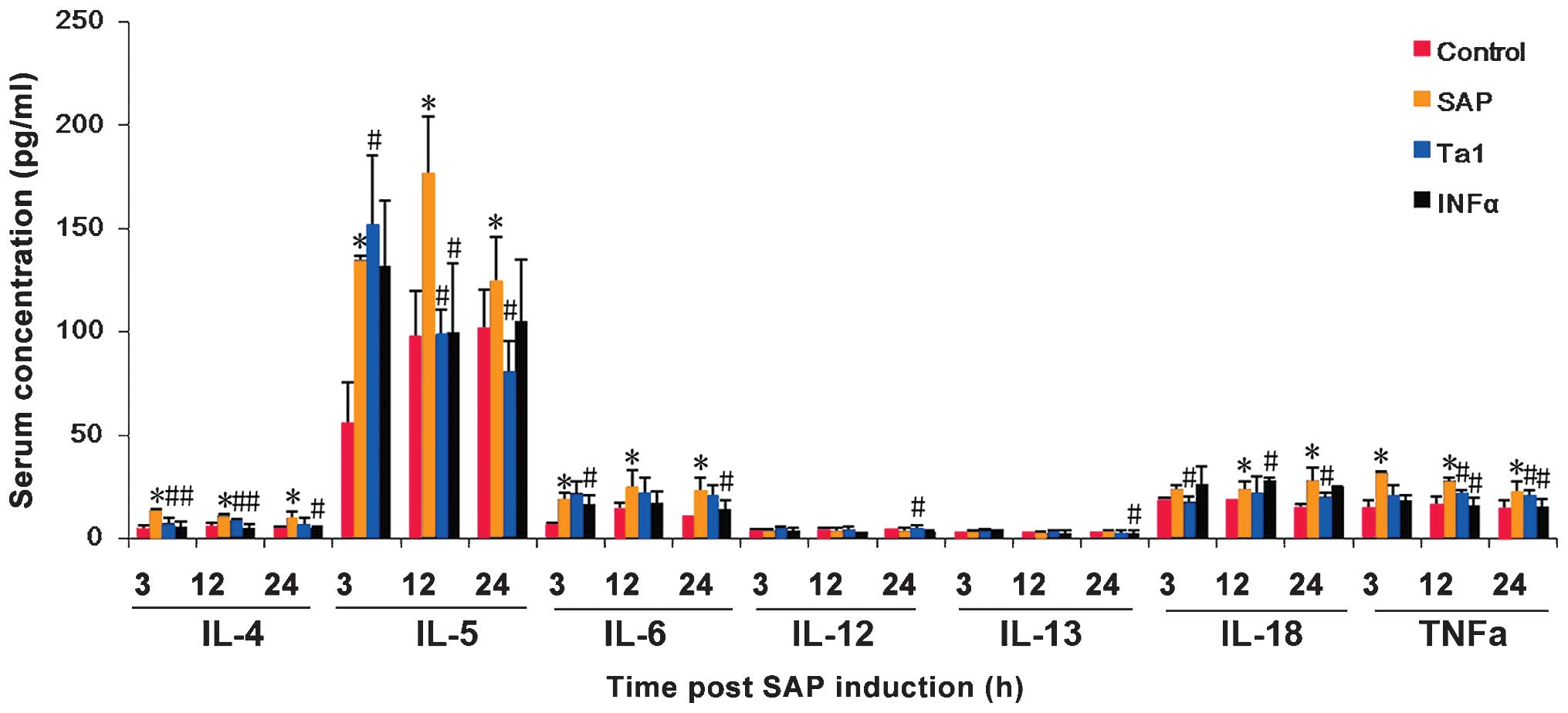
The circulating levels of TNFα, IL-4, IL-5, IL-6 and
IL-18 were significantly higher in the SAP group rats, compared
with the control group rats 3, 12 and 24 h following the indiction
of SAP (P<0.05; Fig. 3). In the
rats treated with TA1 or INFα, the levels of TNFα, IL-4, IL-5 and
IL-18 were significantly lower, compared with those in the SAP
group (P<0.05, Fig. 2).
Expression levels of serum PCT in the
different treatment groups
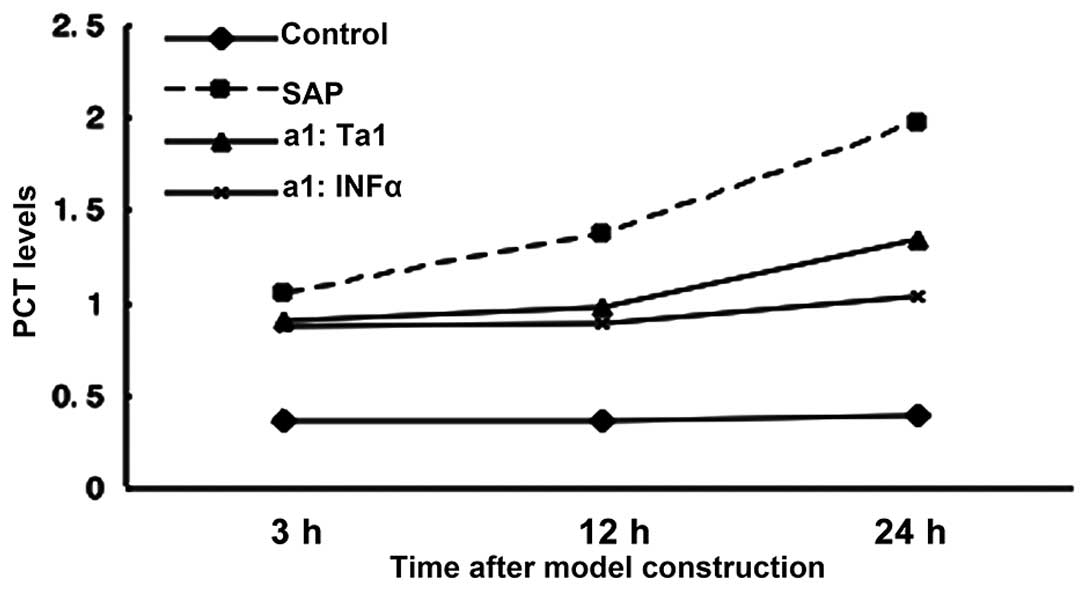
At 24 h post-SAP, the circulating levels of PCT
increased in the SAP group rats, whereas the expression levels of
PCT in the rats, which were not administered with sodium
taurocholate remained stable. Circulating levels of PCT were
significantly decreased in the rats treated with TA1 or IFNα at 12
and 24 h post celiotomy (P>0.05; Fig. 4).
Lymphocyte subsets in the peripheral
blood of the different treatment groups
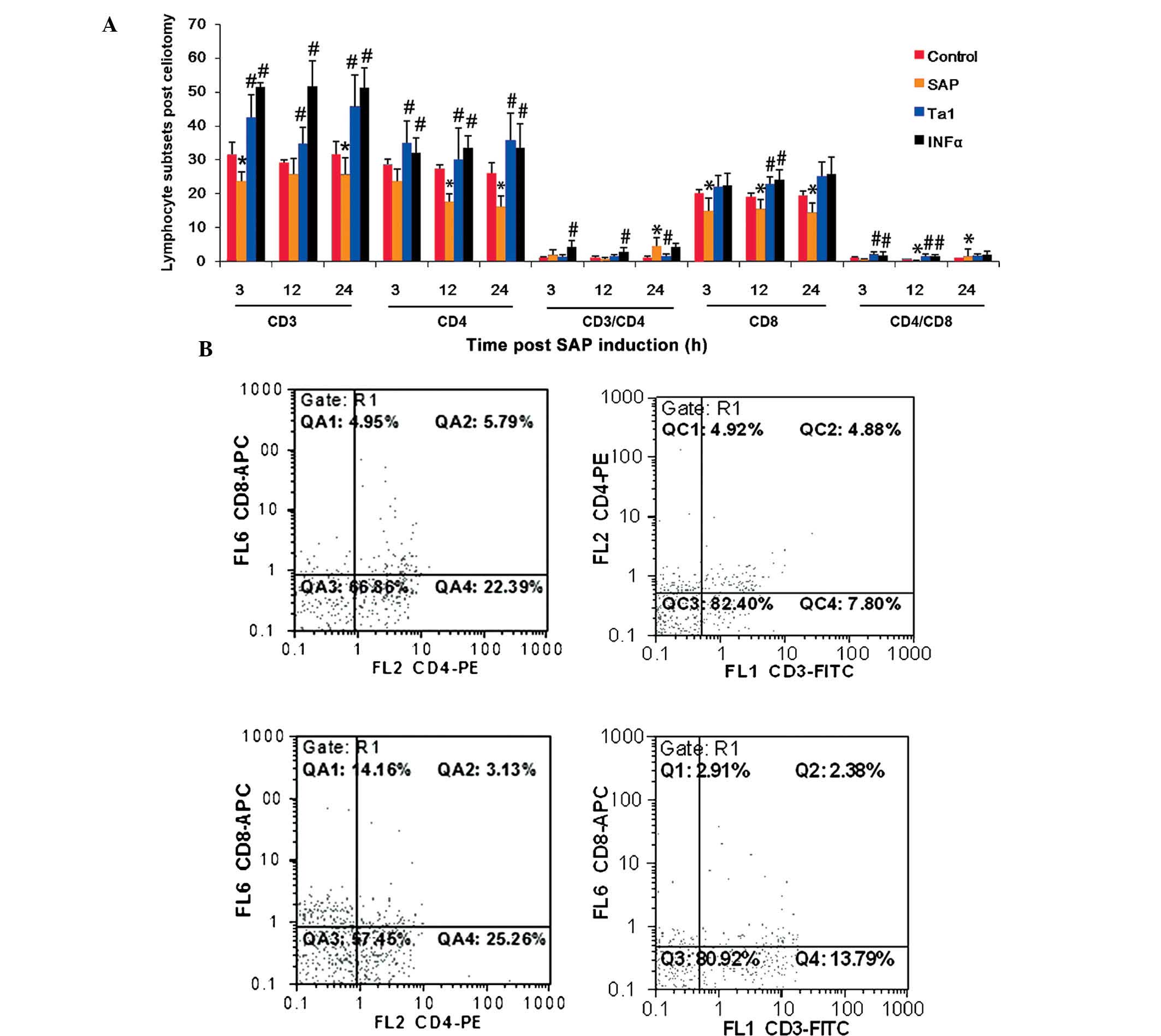
T cell subsets were significantly affected by the
establishment of SAP. Compared with the control animals, the
proportion of T lymphocytes expressing CD3 and CD8 decreased 3 h
post-celiotomy, the proportion of T lymphocytes expressing CD4 and
CD8 decreased 12 h post-celiotomy, and the proportion of T
lymphocytes expressing CD3, CD4 and CD8 decreased 24 h
post-celiotomy (Fig. 4). The
animals treated with TA1 exhibited higher levels of CD3+
and CD4+ (3, 12 and 24 h), CD8+ (12 h), and
CD4+/CD8+ (3 and 12 h) T lymphocytes
(Fig. 4). The animals administered
with INFα exhibited higher levels of CD3+ and
CD4+ (3 h, 12 h, 24 h), CD8+ (24 h) and
CD4+/CD8+ (3 h, 12 h) T lymphocytes (Fig. 4).
Histological observation of rat
pancreatic and lung tissue samples
Pancreatic and lung tissue samples were removed from
the experimental animals 3, 12 and 24 h post-SAP to evaluate tissue
damage. As shown in Fig. 5A, which
shows representative images of the tissue samples at 12 h, the
pancreatic samples removed from the control rats exhibited intact
pancreatic structure with normal alveoli, with no lobular necrosis,
hemorrhage or inflammatory cell infiltration. In the pancreatic
tissue samples of the SAP rats, marked pancreatic edema, lobular
damage, inflammatory cell infiltration, acinar necrosis and
hemorrhage were observed. Compared with the SAP group, the rats
administered with TA1 or INFα exhibited alleviated symptoms at the
corresponding time-points.
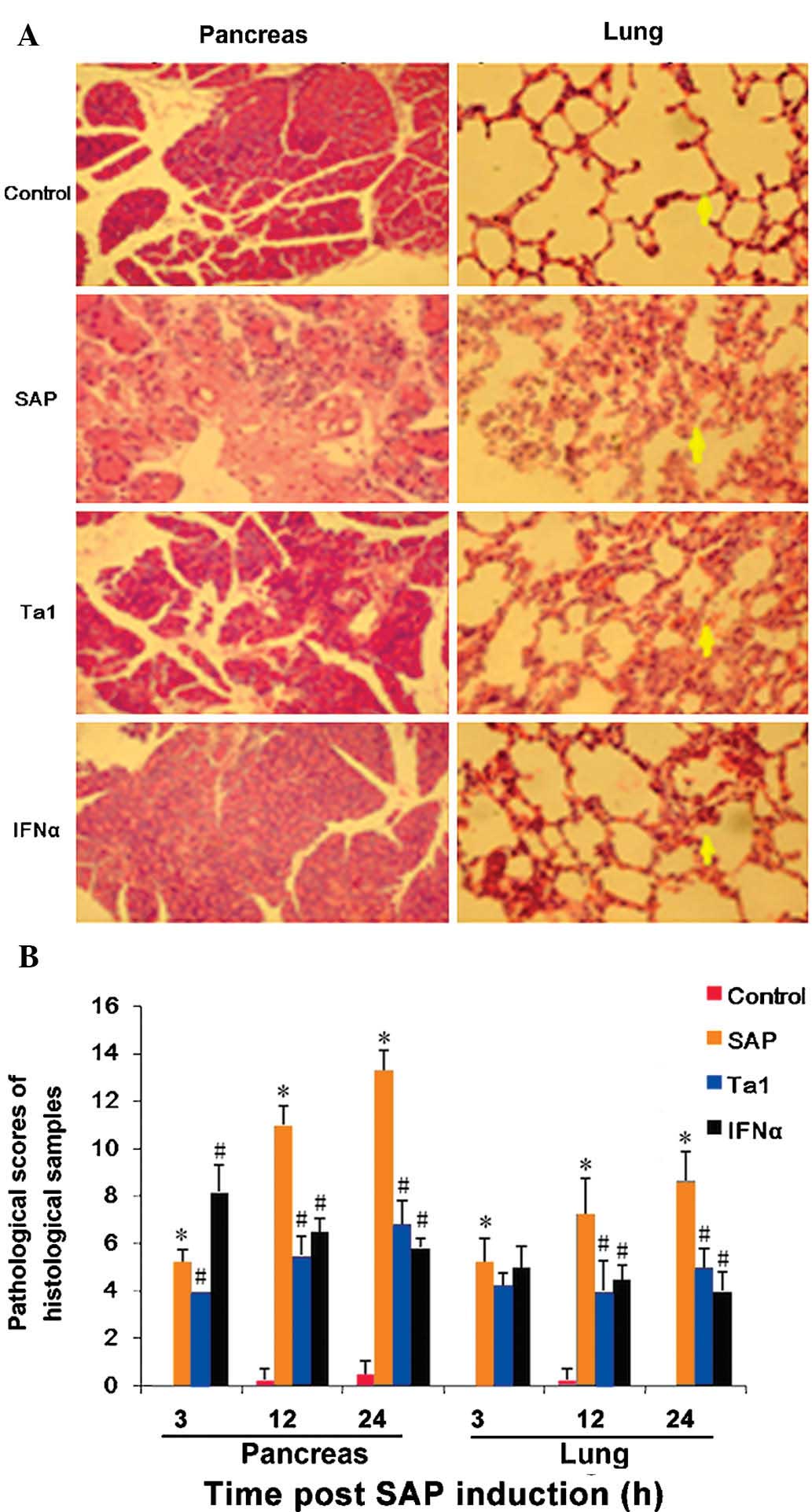 | Figure 5Pathological changes in the pancreas
and lung 12 h post-SAP and Ta1 or INFα treatment. Pancreatic and
lung tissue samples were harvested at different time-points
post-treatment and following hematoxylin and eosin staining, tissue
damage was evaluated. (A) Representative histological images of
tissues 12 h post-treatment. Marked pancreatic edema, lobular
damage, inflammatory cell infiltration, acinar necrosis and
hemorrhage were observed in the SAP group. TA1 or INFα-treated rat
tissue samples exhibited alleviated symptoms at the corresponding
time-points. SAP lung samples exhibited pulmonary edema, scattered
bleeding, alveolar wall rupture, marginal pleural effusion,
interstitial hyperemia and edema, with significant widening and
neutrophil infiltration in the alveolar and interstitial lung. TA1
and INFα-treated rats exhibited alleviated symptoms at the
corresponding time-points. (B) Damage was quantified and compared
between groups. Data are presented as the mean ± standard
deviation. *P<0.05, vs. control group;
#P<0.05, vs. SAP group. SAP, severe acute
pancreatitis; TA1, thymosin α1; IFNα, interferon α. |
Histological analysis of the lung tissue samples
obtained from the SAP rats revealed pulmonary edema, scattered
bleeding, alveolar wall rupture, marginal pleural effusion,
interstitial hyperemia and edema, and marked widening and
neutrophil infiltration of the alveoli and interstitial lung. The
TA1 and INFα-treated rats exhibited markedly alleviated symptoms at
the corresponding time-points (Fig.
5A).
Pathological scoring (Fig. 5B) revealed that damage to the
pancreas and lung had been induced 3 h following SAP induction, and
thes symptoms were aggravated with time. Tissue damage was
significantly ameliorated following the administration of TA1 and
INFα in the pancreas and lung 12 and 24 h post-model induction,
compared with the SAP group.
Correlation between pathological scores
and levels of cytokines and PCT
At 24 h post-model establishment, the histological
scoring of the pancreatic damage in the SAP rats was positively
correlated with the level of lung damage and the serum levels of
TNFα, IL-4, IL-5, IL-18 and IL-6 (coefficients of 0.879, 0.857,
0.803, 0.788, 0.696 and 0.574, respectively; P<0.05; Table I). The histological scoring of the
lung damage in the SAP rats was also positively correlated with the
serum levels of TNFα, IL-4 and IL-5, with correlation coefficients
of 0.763, 0.669 and 0.589, respectively (P<0.05; Table I). The circulating levels of PCT
were also positively correlated with the levels of lung (r=0.789;
P<0.05) and pancreatic damage (r=0.824, P<0.05; Table I).
 | Table ICorrelation between pathological score
and levels of cytokines and PCT at 24 h post-SAP establishment. |
Table I
Correlation between pathological score
and levels of cytokines and PCT at 24 h post-SAP establishment.
| Factor | Pancreatic damage
(r-value) | Lung damage
(r-value) | TNFα (r-value) | IL-4 (r-value) | IL-5 (r-value) | IL-18 (r-value) | IL-6 (r-value) |
|---|
| Pancreatic
damage | | 0.879a | 0.857a | 0.803a | 0.788a | 0.696a | 0.574a |
| Lung damage | 0.879a | 0.763a | 0.669a | 0.589a | | | |
| PCT | 0.789a | 0.824a | | | | | |
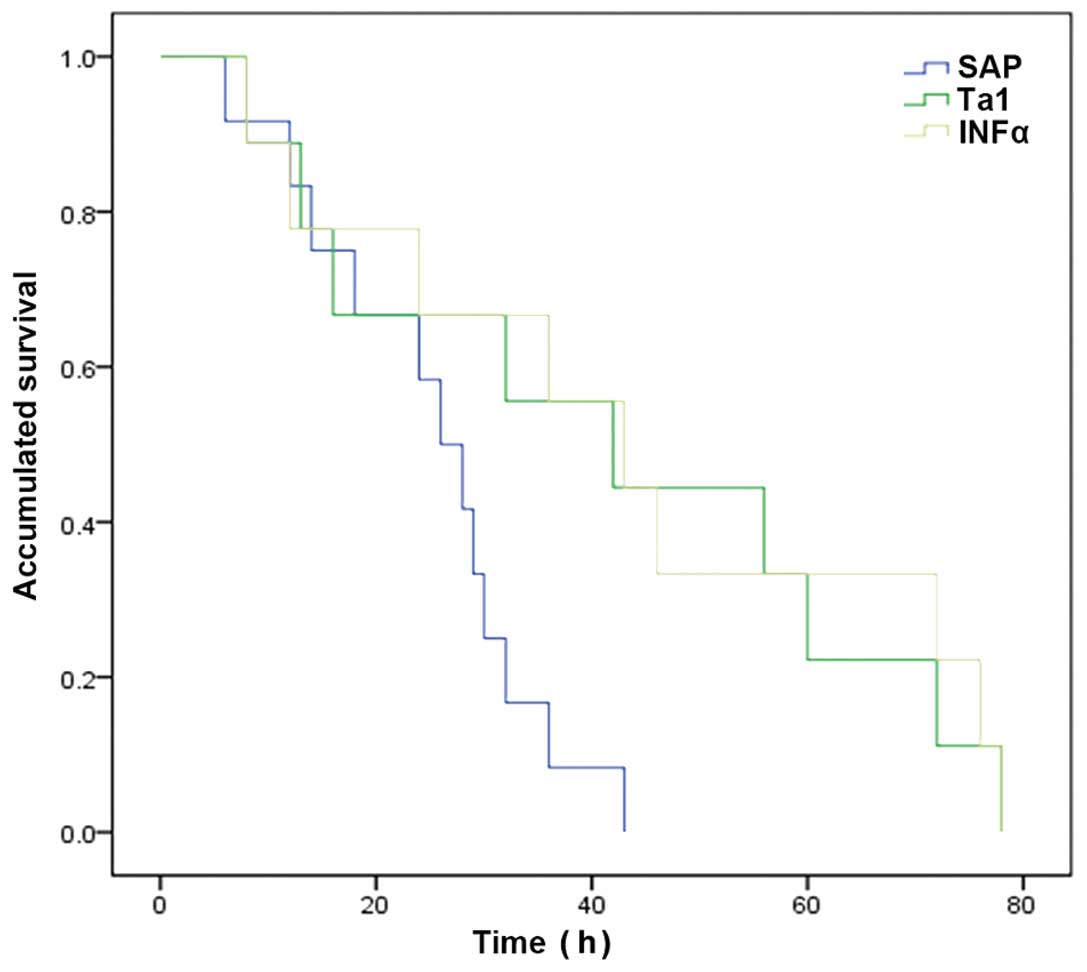
Mortality and survival following
celiotomy
Rats administered with TA1 or INFα survived for
significantly longer periods of time, compared with the rats in the
SAP group (P<0.05; Fig. 6).
Discussion
The present study aimed to investigate the effects
of TA1 and IFNα on cellular immune functions in a rat model of SAP,
and to establish an experimental basis for the administration of
TA1 and IFNα in the treatment of SAP. The results demonstrated that
administration of either TA1 or IFNα decreased the expression
levels of AST, LDH, AMY, p-AMY, LPS, PCT and inflammatory
cytokines, following the establishment of SAP. Administration of
either TA1 or IFNα also resulted in a significantly higher
proportion of CD3+, CD4+ and CD8+
T cells in the circulating blood, and histological examination of
the pancreas and lung revealed a reduction in damage.
Administration of either TA1 or IFNα also extended the survival
rates of the rats in this SAP model, suggesting that TA1 and IFNα
reduced the inflammatory reaction, decreased cell damage and
enhanced immune function in the SAP rats.
T helper (Th)1/Th2 cell-expressed cytokines and
tissue damage levels were used as indicators of immune function,
and thus the efficacy of TA1 and IFNα in the treatment of SAP. A
significant correlation was observed between serum levels of PCT
and lung damage in the SAP rats, with improvement in following TA1
and IFNα treatment. These findings indicated that TA1 and IFNα
enhanced T cell function by elevating the percentage of
CD3+ and CD4+ T cells, and the CD4+/CD8+
ratio, and by inhibiting the release of inflammatory cytokines.
The pancreatic enzyme activation-induced
self-digestion of pancreatic tissues can result in acute
pancreatitis (AP), however, the mechanisms underlying the
development of AP remain to be fully elucidated. A previous study
suggested that in the early phases of AP, macrophages, neutrophils
and the complement system activated by local lesions can trigger
the release of high levels of proinflammatory cytokines and
vasoactive substances, which then lead to a cascade reaction and
excessive systemic inflammatory responses, resulting in the
development of SAP (12).
Therefore, the release of proinflammatory cytokines is considered
to be a major contributor to the uncontrolled systemic inflammation
detected during AP progression. In the present study, the levels of
enzymatic indicators and inflammatory cytokines in SAP rats
increased with the severity of SAP, however, the rats treated with
TA1 and INFα exhibited significantly decreased enzyme levels,
suggesting reduced damage to the pancreas and other organs. The
association between cytokine levels and AP progression was first
suggested in the 1990s (13), and
subsequent experiments and clinical trials suggested the
involvement of TNFα and IL-18 in the activation of immune disorder
during SAP (14). Previous studies
also identified a correlation between circulating levels of IL-4,
TNFα, IL-8, IL-18 and IL-6, and the severity of SAP and the
development of complications (15–17).
These findings are consistent with the progression of SAP in the
rat model of the present study.
TNFα is predominantly produced by mononuclear
macrophages, and is the first inflammatory cytokine to increase in
the early phase of AP. TNFα induces the apoptosis of pancreatic
acinar cells (18); the activation
of cytokines, including IL-6 and IL-8; and the production of
vasoactive substances, including platelet-activating factors,
oxygen-free radicals and endothelial cell adhesion molecules
(19). Therefore, TNFα can induce
local and systemic tissue damage. The circulating levels of serum
IL-6 increase following the surge of TNFα, perhaps indicating IL-6
induction by TNFα (20). In the
present study, circulating levels of IL-6 were maintained at
relatively high levels in the acute phase of SAP. High levels of
IL-6 can directly damage endothelial cells, facilitate immune
adhesion and micro-thrombosis formation, inhibit endothelial
repair, and increase vascular permeability to cause tissue damage
(21).
IL-18 can induce the transcription of IFNγ in
primary human CD4+ T cells, and also independently
induces the secretion of IFNγ from natural killer cells (22). In synergy with mitogen or anti-CD3
monoclonal antibody, IL-18 induces the production of
granulocyte-macrophage colony-stimulating factor from human
peripheral blood mononuclear cells or enriched T cells, in a
dose-dependent manner (23). The
present study demonstrated that the serum expression levels of
TNFα, IL-6 and IL-8 in the SAP rats were significantly higher,
compared to those of the control, and this elevation was positively
correlated with the severity of pancreatic and lung damage,
indicating that TNFα, IL-6 and IL-18 are associated with AP
progression, and may represent important indicators of SAP
severity.
PCT functions to amplify inflammatory responses, and
to regulate the activation of various cytokines. Serum expression
levels of PCT have been demonstrated to increase more substantially
in infected pancreatic necrotic tissues than in aseptic necrotic
tissues (24), suggesting that
serum PCT may be a valuable indicator of AP development,
progression and infected pancreatic necrosis. In the present study,
no significant change in PCT levels were observed within the first
3 h of SAP establishment, however PCT levels gradually increased
over the following 24 h. The administration of TA1 and INFα reduced
circulating levels of PCT from 12 h post-SAP.
Previous studies have demonstrated that, when
abnormal immune function occurs in early SAP, the levels of
circulating T lymphocytes are also reduced, and T cell subset
abnormalities are observed. In the middle and late phases of SAP,
however, excessive immune responses precipitate immunosuppression
(25). In the present study, the
percentage of CD3+, CD4+ and CD8+
T cells, and the CD4+/CD8+, ratio were all
reduced following the establishment of SAP. The percentage of
CD4+ T cells and the CD4+/CD8+
ratio may partially reflect cell-mediated immune function in
patients with SAP (26).
CD4+ T cells secrete IL-2 to induce the secretion of
IL-1 from mononuclear macrophages, and CD4+ T cells also
stimulate stationary T lymphocytes to express IL-2 receptors, which
then bind to IL-2 to trigger various immune responses and to
enhance DNA synthesis in lymphocytes (27). Therefore, decreased CD4+
T cell counts impair immune function and increase susceptibility to
infection.
In the present study, as SAP progressed,
pathological changes were observed in the pancreas and lung.
Hemorrhage, necrosis and inflammatory cell infiltration were
observed in pancreatic lesions, whereas lung edema and neutrophil
infiltration were observed in the lungs. The present study
identified a direct correlation between lung damage and
inflammatory mediators, and cytokines were detected in the
pancreatic and extra-pancreatic tissue samples. This indicated that
inflammatory cytokines are only involved in the development of SAP,
but they are also key in the progression of SAP local lesions to
systemic disease, and may be directly involved in the development
of early multiple organ dysfunction syndrome during SAP.
The use of immune agents in the early treatment of
SAP may alleviate lymphocyte damage and protect immune function to
various extents. However, previous inflammatory mediators
intervention in clinical treatment of SAP achieved no significant
efficacy, suggesting that blunt suppression of inflammation may
instead aggravate immune disorders (28). Therefore, the use of
immunomodualatory agents, including TA1 and IFNα may contribute
significantly to alleviating inflammatory responses, reducing cell
damage, decreasing enzymatic abnormalities and improving immune
disorders, thus reducing secondary infections. Although the results
of immunomodulation in animal models do not directly translate to
clinical settings, the clinical application of immunomodulation
therapy in SAP treatment merits further investigation.
Acknowledgments
The present study was supported by the International
Science and Technology Cooperation and Exchange Program of Shaanxi
Province (grant no. 2015KW-045, XW).
References
|
1
|
Otsuki M, Takeda K, Matsuno S, Kihara Y,
Koizumi M, Hirota M, Ito T, Kataoka K, Kitagawa M, Inui K and
Takeyama Y: Criteria for the diagnosis and severity stratification
of acute pancreatitis. World J Gastroenterol. 19:5798–5805. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Schepers NJ, Besselink MG, van Santvoort
HC, Bakker OJ and Bruno MJ; Dutch Pancreatitis Study Group: Early
management of acute pancreatitis. Best Pract Res Clin
Gastroenterol. 27:727–743. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Panek J, Karcz D, Pieton R, Zasada J,
Tusinski M, Dolecki M and Winiarski M: Blood serum levels of
proinflammatory cytokines in patients with different degrees of
biliary pancreatitis. Can J Gastroenterol. 20:645–648.
2006.PubMed/NCBI
|
|
4
|
Kylanpaa ML, Repo H and Puolakkainen PA:
Inflammation and immunosuppression in severe acute pancreatitis.
World J Gastroenterol. 16:2867–2872. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Bone RC: Sir Isaac Newton, sepsis, SIRS
and CARS. Crit Care Med. 24:1125–1128. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Garaci E, Pica F, Sinibaldi-Vallebona P,
Pierimarchi P, Mastino A, Matteucci C and Rasi G: Thymosin alpha
(1) in combination with cytokines and chemotherapy for the
treatment of cancer. Int Immunopharmacol. 3:1145–1150. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Aman MJ, Tretter T, Eisenbeis I, Bug G,
Decker T, Aulitzky WE, Tilg H, Huber C and Peschel C:
Interferon-alpha stimulates production of interleukin-10 in
activated CD4+ T cells and monocytes. Blood. 87:4731–4736.
1996.PubMed/NCBI
|
|
8
|
Romani L, Bistoni F, Montagnoli C, Gaziano
R, Bozza S, Bonifazi P, Zelante T, Moretti S, Rasi G, Garaci E and
Puccetti P: Thymosin alpha1: An endogenous regulator of
inflammation, immunity and tolerance. Ann N Y Acad Sci.
1112:326–338. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Pestka S, Krause CD and Walter MR:
Interferons, interferon-like cytokines, and their receptors.
Immunol Rev. 202:8–32. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Sharif S, Broman M, Babcock T, Ong E, Jho
D, Rudnicki M, Helton WS and Espat NJ: A priori dietary omega-3
lipid supplementation results in local pancreatic macrophage and
pulmonary inflammatory response attenuation in a model of
experimental acute edematous pancreatitis (AEP). JPEN J Parenter
Enteral Nutr. 30:271–276. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Chooklin S: Pathogenic aspects of
pulmonary complications in acute pancreatitis patients.
Hepatobiliary Pancreat Dis Int. 8:186–192. 2009.PubMed/NCBI
|
|
12
|
de Beaux AC, Ross JA, Maingay JP, Fearon
KC and Carter DC: Proinflammatory cytokine release by peripheral
blood mono-nuclear cells from patients with acute pancreatitis. Br
J Surg. 83:1071–1075. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Curley PJ: Endotoxin, cellular immune
dysfunction and acute pancreatitis. Ann R Coll Surg Engl.
78:531–535. 1996.PubMed/NCBI
|
|
14
|
Ueda T, Takeyama Y, Yasuda T, Matsumura N,
Sawa H, Nakajima T, Ajiki T, Fujino Y, Suzuki Y and Kuroda Y:
Significant elevation of serum interleukin-18 levels in patients
with acute pancreatitis. J Gastroenterol. 41:158–165. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Kaya E, Dervisoglu A and Polat C:
Evaluation of diagnostic findings and scoring systems in outcome
prediction in acute pancreatitis. World J Gastroenterol.
13:3090–3094. 2007.PubMed/NCBI
|
|
16
|
Denham W, Fink G, Yang J, Ulrich P, Tracey
K and Norman J: Small molecule inhibition of tumor necrosis factor
gene processing during acute pancreatitis prevents cytokine cascade
progression and attenuates pancreatitis severity. Am Surg.
63:1045–1049; discussion 1049–1050. 1997.PubMed/NCBI
|
|
17
|
Stimac D, Fisić E, Milić S, Bilić-Zulle L
and Perić R: Prognostic values of IL-6, IL-8 and IL-10 in acute
pancreatitis. J Clin Gastroenterol. 40:209–212. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Karne S and Gorelick FS: Etiopathogenesis
of acute pancreatitis. Surg Clin North Am. 79:699–710. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Springer TA: Adhesion receptors of the
immune system. Nature. 346:425–434. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Jiang CF, Shiau YC, Ng KW and Tan SW:
Serum interleukin-6, tumor necrosis factor alpha and C-reactive
protein in early prediction of severity of acute pancreatitis. J
Chin Med Assoc. 67:442–446. 2004.PubMed/NCBI
|
|
21
|
Zhao X, Andersson R and Wang X, Dib M and
Wang X: Acute pancreatitis-associated lung injury:
Pathophysiological mechanisms and potential future therapies. Scand
J Gastroenterol. 37:1351–1358. 2002. View Article : Google Scholar
|
|
22
|
Barbulescu K, Becker C, Schlaak JF,
Schmitt E, Meyer zum Buschenfelde KH and Neurath MF: IL-12 and
IL-18 differentially regulate the transcriptional activity of the
human IFN-gamma promoter in primary CD4+ T lymphocytes. J Immunol.
160:3642–3647. 1998.PubMed/NCBI
|
|
23
|
Matsumoto S, Tsuji-Takayama K, Aizawa Y,
Koide K, Takeuchi M, Ohta T and Kurimoto M: Interleukin-18
activates NF-kappaB in murine T helper type 1 cells. Biochem
Biophys Res Commun. 234:454–457. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Rau BM, Kemppainen EA, Gumbs AA, Büchler
MW, Wegscheider K, Bassi C, Puolakkainen PA and Beger HG: Early
assessment of pancreatic infections and overall prognosis in severe
acute pancreatitis by procalcitonin (PCT): A prospective
international multicenter study. Ann Surg. 245:745–754. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Li J, Yang WJ, Huang LM and Tang CW:
Immunomodulatory therapies for acute pancreatitis. World J
Gastroenterol. 20:16935–16947. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Li XM, Chen JZ and Zhang NY: Association
of TCM-bionzheng with Tlymphrocyte subsets and thyroidism in
patients with diabetes mellitus. J Fourth Mil Med Univ. 2:223–234.
2000.In Chinese.
|
|
27
|
Watson J and Mochizuki D: Interleukin 2: A
class of T cell growth factors. Immunol Rev. 51:257–278. 1980.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Li J, Yang WJ, Huang LM and Tang CW:
Immunomodulatory therapies for acute pancreatitis. World J
Gastroenterol. 20:16935–16947. 2014. View Article : Google Scholar : PubMed/NCBI
|