Introduction
Gallbladder cancers (GBCs) are the fifth most common
type of gastrointestinal cancer and the most common biliary tract
malignancy in the USA (1,2). The prognosis of GBC is poor with a
high mortality. Early diagnosis is rare due to the lack of specific
signs or symptoms (3).
Consequently, over 90% of patients with GBC are diagnosed at an
inoperable stage with significant invasion and metastasis to other
organs (4). The majority of GBCs
are adenocarcinomas (AC; >90%) (5), whereas other histopathological
subtypes including mucinous, papillary, and squamous subtypes are
observed only rarely (2). Squamous
cell/adenosquamous carcinoma (SC/ASC) represents 1–12% of GBCs
(2,6). The clinicopathological
characteristics of SC/ASC remain to be well documented, due to the
fact that the majority of currently available data describe
individual case reports or the analysis of small case series.
Therefore, therapeutic interventions for SC/ASC remain to be fully
elucidated (7). Although
biomarkers for predicting the prognosis of AC have been
investigated, none of the proposed markers have yet reached
clinical application (8). Notably,
no biomarkers associated with the progression and prognosis of
SC/ASC have been reported. Therefore, it is important to document
the clinicopathological and biological characteristics of
SC/ASC.
Ki-67 and proliferating cell nuclear antigen (PCNA)
are two conventional proliferation markers used for routine
clinical diagnosis and/or prognostic prediction for several types
of cancer (9). However, these two
markers are associated with significant problems. For example,
Ki-67 serves a role in ribosome biosynthesis, and is not directly
responsible for cell proliferation (10). In addition, the labeling index of
Ki-67 immunostaining is usually affected by external factors such
as nutrient deprivation (11).
Notably, the precise function of Ki-67 remains unclear (12,13).
PCNA is a marker of DNA replication that is also required for DNA
repair. Therefore, it is a less specific marker (9,14).
Previously, geminin was identified as a novel tumor cell
proliferation marker. However, geminin expression was restricted to
S, G2 and early M phase of the cell cycle (9,14),
thus the labeling index of geminin identifies only the number of
actively proliferating cells that have passed G1 phase.
Therefore, there remains a requirement for the identification of
more specific and precise markers to facilitate patient diagnosis
and/or prognosis.
The minichromosome maintenance (MCM) complex
components 2–7 are essential for DNA replication in all eukaryotic
cells, and are expressed more frequently in cancer cells compared
with normal cells (15). Unlike
Ki-67 and PCNA, MCM proteins are required in cycling cells, however
are absent from quiescent cells. Immunostaining with antibodies
against MCM identified a greater number of cells in the cell cycle
than that of either PCNA or Ki-67 (16). This supports the potential clinical
applications of MCM proteins as specific markers of proliferation.
In addition, MCM proteins have demonstrated potential for
diagnostic and prognostic applications in several types of human
malignancies (9,14). For example, multivariate analysis
identified MCM expression as an independent negative predictor of
patient survival (9). in addition,
MCM expression could be expanded to population screening for
neoplasia at a range of organ sites at which cells could be
obtained for cytological analysis (17–19).
However, the expression of MCM in GBC remains to be assessed.
HIV-1 tat interactive protein 2 (TIP30) was
identified as a transcriptional cofactor that suppresses metastasis
by inhibiting tumor growth (20)
and angiogenesis (21,22), and induces apoptosis (23). Li et al (24) demonstrated that weak or negative
expression of TIP30 contributed to the development and progression
of gastric cancer. When TIP30 expression was silenced,
hepatocellular carcinoma and other tumors developed spontaneously
in mice (25). In contrast, the
ectopic expression of TIP30 increased the expression of a subset of
pro-apoptotic genes (23), and
subsequently inhibited tumorigenesis in liver and lung cells. The
direct involvement of MCM in DNA replication and TIP30 in cell
proliferation and apoptosis suggests that these molecules are
potential targets for gene therapy. Therefore, the identification
of proliferation-specific markers, including MCM and TIP30
expression, is important for the development of novel GBC
treatments.
In the current study, the expression of MCM2 and
TIP30 in surgically resected specimens, including AC and SC/ASC,
was examined using immunohistochemistry. The correlation between
MCM2 and TIP30 expression and the clinicopathological
characteristics and prognosis of AC and SC/ASC were evaluated and
compared.
Materials and methods
Case selection
The current study was pre-approved by The Ethics
Committee for Human Research, Central South University (Changsha).
A total of 46 SC/ASC samples that underwent surgical resection or
biopsy were diagnosed from a total of 1,060 GBC samples collected
between January 1995 and December 2009 from 7 hospitals. A total of
80 AC samples with available survival information were selected
randomly from 1060 GBC samples for comparison in the present study.
Among the 46 patients with SC/ASC, 27 were female and 19 were male
(F/M=1.42) aged 35–82 (mean, 55.8±9.6) years. Among the 80 patients
with AC, 54 were female and 26 were male (F/M=2.08), aged 33–80
(mean, 53.8±9.9) years. Surgery included radical resection for 14
SCs/ASCs and 26 ACs, palliative surgery for 18 SCs/ASCs and 28 ACs,
and no operation for 14 SCs/ASCs and 26 ACs with biopsy alone.
Survival information of all 46 SC/ASC and 80 AC patients was
obtained through letters and phone calls. The follow-up time of the
study was 2 years. Individuals whom survived longer than 2 years
were included in the analysis as censored cases.
Immunohistochemistry staining
Mouse anti-MCM2 (sc-373702), mouse anti-TIP30
(sc-55343) and horseradish peroxidase (HRP)-conjugated anti-mouse
secondary antibodies (sc-2010) were purchased from Santa Cruz
Biotechnology, Inc. (Santa Cruz, CA, USA). Staining was performed
using the peroxidase-based EnVision™ Detection kit (Dako North
America, Inc., Carpinteria, CA, USA) following the manufacturer's
instructions. Briefly, 4 µM sections were cut from routinely
paraffin-embedded AC and SC/ASC tissues. The sections were
deparaffinized and incubated with 3% H2O2 for
15 min, and soaked with phosphate-buffered saline (PBS) for 3×5
min. They were then incubated with mouse anti-MCM2 (1:100 dilution)
or mouse anti-TIP30 (1:100) antibodies for 1 h at room temperature.
Subsequent to rinsing the sections with PBS three times, solution A
(containing the HRP-conjugated secondary antibody) was added and
incubated for 30 min. DAB substrate was then added, followed by
hematoxylin counter-staining. The slides were subsequently
dehydrated and soaked in xylene for 3×5 min. Positive sections
purchased from Wuhan Boster Biological Technology, Ltd. (Wuhan,
China) were used as the positive control, whereas replacing the
primary antibody with 5% fetal bovine serum was used as the
negative control. The percentage of positive cells was calculated
from 500 cells in 10 random fields. Cases with ≥25% positive cells
were considered to be positive, whereas samples with <25%
positive cells were negative.
Statistical analysis
Data were analyzed using SPSS software, version 14.0
(SPSS, Inc., Chicago, IL, USA). The associations between MCM2 and
TIP30 expression with histological or clinical factors were
analyzed using χ2 or Fisher's exact test. Kaplan-Meier
and time series analyses were used for univariate survival
analysis. Cox proportional hazards model was used for multivariate
analysis, and to determine the 95% confidence interval. P<0.05
was considered to indicate a statistically significant
difference.
Results
Comparison of clinicopathological
characteristics with MCM2 and TIP30 expression in SC/ASC and
AC
As presented in Table
I, the percentage of cases in patients older than 45 years and
with a tumor mass >3 cm was significantly higher in the SC/ASC
group compared with the ACs (P<0.05). In contrast, the
percentage of poorly differentiated tumors was significantly
reduced in SC/ASC compared with AC. No significant differences in
other clinicopathological characteristics (including gender, TNM
stage, invasion, lymph node metastasis, history of gallstones,
operative procedure and average survival time) were observed
between the SC/ASC and AC groups. Immunohistochemistry identified
that MCM2-positive cells exhibited brown nuclear staining, whereas
TIP30-positive cells presented with a brown membrane and
cytoplasmic staining in the SC/ASC (Fig. 1) and AC (Fig. 2) tissues. In addition, no
significant differences in the percentage of positive MCM2 and
TIP30 expression was observed between patients with SC/ASC and AC
(Table I).
 | Table I.Comparison of gallbladder SC/ASC and
AC clinicopathological features and MCM2 and TIP30 expression
status. |
Table I.
Comparison of gallbladder SC/ASC and
AC clinicopathological features and MCM2 and TIP30 expression
status.
| Clinicopathological
characteristic | SC (n=46) | ASC (n=80) | χ2 | P-value |
|---|
| Sex |
|
|
|
|
|
Male | 19 (41.3) | 26 (32.5) | 0.986 | 0.352 |
|
Female | 27 (58.7) | 54 (67.5) |
|
|
| Age (year) |
|
|
|
|
|
≤45 | 3 (6.5) | 16 (20.0) | 4.143 | 0.042 |
|
>45 | 43 (93.5) | 64 (80.0) |
|
|
|
Differentiation |
|
|
|
|
|
Well-differentiated | 16 (34.8) | 27 (33.8) |
|
|
|
Moderately differentiated | 24 (52.2) | 25 (31.3) | 8.515 | 0.014 |
| Poorly
differentiated | 6 (13.0) | 28 (35.0) |
|
|
| Maximum diameter of
tumor (cm) |
|
|
|
|
| ≤3
cm | 20 (43.5) | 50 (62.5) | 4.280 | 0.039 |
| >3
cm | 26 (56.5) | 30 (37.5) |
|
|
|
Cholecystolithiasis |
|
|
|
|
|
(−) | 18 (39.1) | 42 (52.5) | 2.093 | 0.148 |
|
(+) | 28 (60.9) | 38 (47.5) |
|
|
| TNM stages |
|
|
|
|
|
I+II | 12 (26.1) | 21 (26.3) |
|
|
|
III | 20 (33.5) | 38 (47.5) | 0.287 | 0.866 |
| IV | 14 (30.4) | 21 (26.3) |
|
|
| Lymph node
metastasis |
|
|
|
|
|
(−) | 17 (37.0) | 30 (37.5) | 0.004 | 0.952 |
|
(+) | 29 (63.0) | 50 (62.5) |
|
|
| Locoregional
invasion |
|
|
|
|
|
(−) | 16 (34.8) | 31 (38.8) | 0.197 | 0.658 |
|
(+) | 30 (62.5) | 49 (61.3) |
|
|
| Operation
methods |
|
|
|
|
|
Radical | 14 (30.4) | 26 (32.5) |
|
|
|
Palliative | 18 (39.1) | 28 (35.0) | 0.215 | 0.898 |
| Without
resection | 14 (30.4) | 26 (32.5) |
|
|
| Mean
survival time | 10.07 (4–25) | 10.34 (3–27) | 0.014 | 0.906 |
| MCM2 |
|
|
|
|
|
(−) | 24 (52.2) | 38 (47.5) | 0.951 | 0.382 |
|
(+) | 22 (47.8) | 42 (52.5) |
|
|
| TIP30 |
|
|
|
|
|
(−) | 26 (56.5) | 38 (47.5) | 0.289 | 0.678 |
|
(+) | 20 (43.5) | 42 (52.5) |
|
|
The association of MCM2 and TIP30
expression with GBC clinicopathological characteristics
As presented in Table
II, the percentage of positive MCM2 and negative TIP30
expression in tumor tissues was significantly associated with large
tumor size, high TNM stage, invasion, lymph node metastasis and no
surgical curability of SC/ASC (P<0.05 or P<0.01). Positive
MCM2 expression was significantly associated with poor
differentiation in SC/ASC (P<0.05). There was no significant
association between MCM2 and TIP30 and pathological type, gender,
age and history of gallstones.
 | Table II.The association of MCM2 and TIP30
expression with the clinicopathological characteristics of
SC/ASC. |
Table II.
The association of MCM2 and TIP30
expression with the clinicopathological characteristics of
SC/ASC.
|
| MCM2 | TIP30 |
|---|
|
|
|
|
|---|
|
Clinicalpathological characteristics | Total no. | Pos no. (%) | χ2 | P-value | Pos no. (%) | χ2 | P-value |
|---|
| Sex |
|
| 0.090 | 0.765 |
| 1.565 | 0.211 |
|
Male | 19 | 9 (47.4) |
|
| 12 (63.2) |
|
|
|
Female | 27 | 14 (51.9) |
|
| 12 (44.6) |
|
|
| Age (years) |
|
| 0.357 | 0.550 |
| 0.270 | 0.603 |
|
≤45 | 3 | 1 (33.3) |
|
| 2 (66.7) |
|
|
|
>45 | 43 | 22 (51.2) |
|
| 22 (51.2) |
|
|
| Pathological
type |
|
| 0.354 | 0.552 |
| 2.333 | 0.127 |
| SC | 26 | 14 (53.8) |
|
| 11 (42.3) |
|
|
|
ASC | 20 | 9 (45.0) |
|
| 13 (65.0) |
|
|
|
Differentiation |
|
| 7.167 | 0.028 |
| 3.753 | 0.153 |
|
Well | 16 | 6 (37.5) |
|
| 10 (62.5) |
|
|
|
Moderately | 24 | 11 (45.8) |
|
| 13 (54.2) |
|
|
|
Poorly | 6 | 6 (100.0) |
|
| 1 (16.7) |
|
|
| Tumor mass
size |
|
| 5.662 | 0.017 |
| 7.389 | 0.007 |
| ≤3
cm | 20 | 6 (30.0) |
|
| 15 (75.0) |
|
|
| >3
cm | 26 | 167 (65.4) |
|
| 9 (34.6) |
|
|
| Gallstones |
|
| 0.365 | 0.546 |
| 0.708 | 0.400 |
| No | 18 | 10 (55.6) |
|
| 8 (44.4) |
|
|
|
Yes | 28 | 13 (46.4) |
|
| 16 (57.1) |
|
|
| TNM stage |
|
| 10.943 | 0.004 |
| 9.936 | 0.008 |
|
I+II | 12 | 3 (25.0) |
|
| 10 (83.3) |
|
|
|
III | 20 | 8 (40.0) |
|
| 11 (55.0) |
|
|
| IV | 14 | 12 (85.7) |
|
| 3 (21.4) |
|
|
| Lymph
metastasis |
|
| 4.572 | 0.032 |
| 6.379 | 0.012 |
| No | 17 | 5 (29.4) |
|
| 13 (76.5) |
|
|
|
Yes | 29 | 18 (62.1) |
|
| 11 (37.9) |
|
|
| Invasion |
|
| 6.133 | 0.013 |
| 12.270 | 0.000 |
| No | 16 | 4 (25.0) |
|
| 14 (87.5) |
|
|
|
Yes | 30 | 19 (63.3) |
|
| 10 (33.3) |
|
|
| Surgery |
|
| 7.365 | 0.025 |
| 9.296 | 0.00 |
|
Radical | 14 | 3 (21.4) |
|
| 11 (78.6) |
|
|
|
Palliative | 18 | 10 (55.6) |
|
| 10 (55.6) |
|
|
|
Biopsy | 14 | 10 (71.4) |
|
| 3 (21.4) |
|
|
As presented in Table
III, the percentage of positive MCM2 and negative TIP30
expression in AC tumors was significantly higher in cases with poor
differentiation, larger tumor mass, higher TMN stage with lymph
node metastasis, invasion to the tissues and organs surrounding the
gallbladder and lack of surgical curability when compared with
cases that were well differentiated, had a small tumor mass, lower
TMN stage, no lymph metastasis, no invasion and that were radically
resected (P<0.05, P<0.01). There was no association between
MCM2 and TIP30 and gender, age and history of gallstones.
 | Table III.The association of MCM2 and TIP30
expression with the clinicopathological characteristics of AC. |
Table III.
The association of MCM2 and TIP30
expression with the clinicopathological characteristics of AC.
|
|
| MCM2 | TIP30 |
|---|
|
|
|
|
|
|---|
| Clinicopathological
characteristics | Total no. | Pos no. (%) | χ2 | P-value | Pos no. (%) | χ2 | P-value |
|---|
| Sex |
|
| 0.000 | 0.990 |
| 0.024 | 0.877 |
|
Male | 26 | 14 (53.8) |
|
| 13 (50.0) |
|
|
|
Female | 54 | 29 (53.7) |
|
| 26 (48.1) |
|
|
| Age (years) |
|
| 2.124 | 0.145 |
| 3.202 | 0.074 |
|
≤45 | 16 | 6 (37.5) |
|
| 11 (68.8) |
|
|
|
>45 | 64 | 37 (57.8) |
|
| 28 (43.8) |
|
|
|
Differentiation |
|
| 7.880 | 0.019 |
| 10.784 | 0.004 |
|
Well | 27 | 11 (40.7) |
|
| 20 (74.1) |
|
|
|
Moderately | 25 | 11 (44.0) |
|
| 10 (40.0) |
|
|
|
Poorly | 28 | 21 (75.0) |
|
| 9 (32.1) |
|
|
| Tumor mass
size |
|
| 5.099 | 0.024 |
| 6.754 | 0.009 |
| ≤3
cm | 50 | 22 (44.0) |
|
| 30 (60.0) |
|
|
| >3 cm | 30 | 21 (70.0) |
|
| 9 (30.0) |
|
|
| Gallstones |
|
| 1.337 | 0.248 |
| 1.279 | 0.258 |
| No | 42 | 20 (47.6) |
|
| 23 (54.8) |
|
|
|
Yes | 38 | 23 (60.5) |
|
| 16 (42.1) |
|
|
| TNM stage |
|
| 11.943 | 0.003 |
| 7.328 | 0.026 |
|
I+II | 21 | 8 (38.1) |
|
| 13 (61.9) |
|
|
|
III | 38 | 17 (44.7) |
|
| 21 (55.3) |
|
|
| IV | 21 | 18 (85.7) |
|
| 5 (23.8) |
|
|
| Lymph
metastasis |
|
| 5.635 | 0.018 |
| 4.086 | 0.043 |
| No | 30 | 11 (36.7) |
|
| 19 (63.3) |
|
|
|
Yes | 50 | 32 (64.0) |
|
| 20 (40.0) |
|
|
| Invasion |
|
| 4.605 | 0.036 |
| 5.035 | 0.025 |
| No | 31 | 12 (38.7) |
|
| 20 (64.5) |
|
|
|
Yes | 49 | 31 (63.3) |
|
| 19 (38.8) |
|
|
| Surgery |
|
| 8.665 | 0.013 |
| 7.449 | 0.024 |
|
Radical | 26 | 10 (38.5) |
|
| 16 (61.5) |
|
|
|
Palliative | 28 | 13 (46.4) |
|
| 16 (57.1) |
|
|
|
Biopsy | 26 | 20 (76.9) |
|
| 7 (26.9) |
|
|
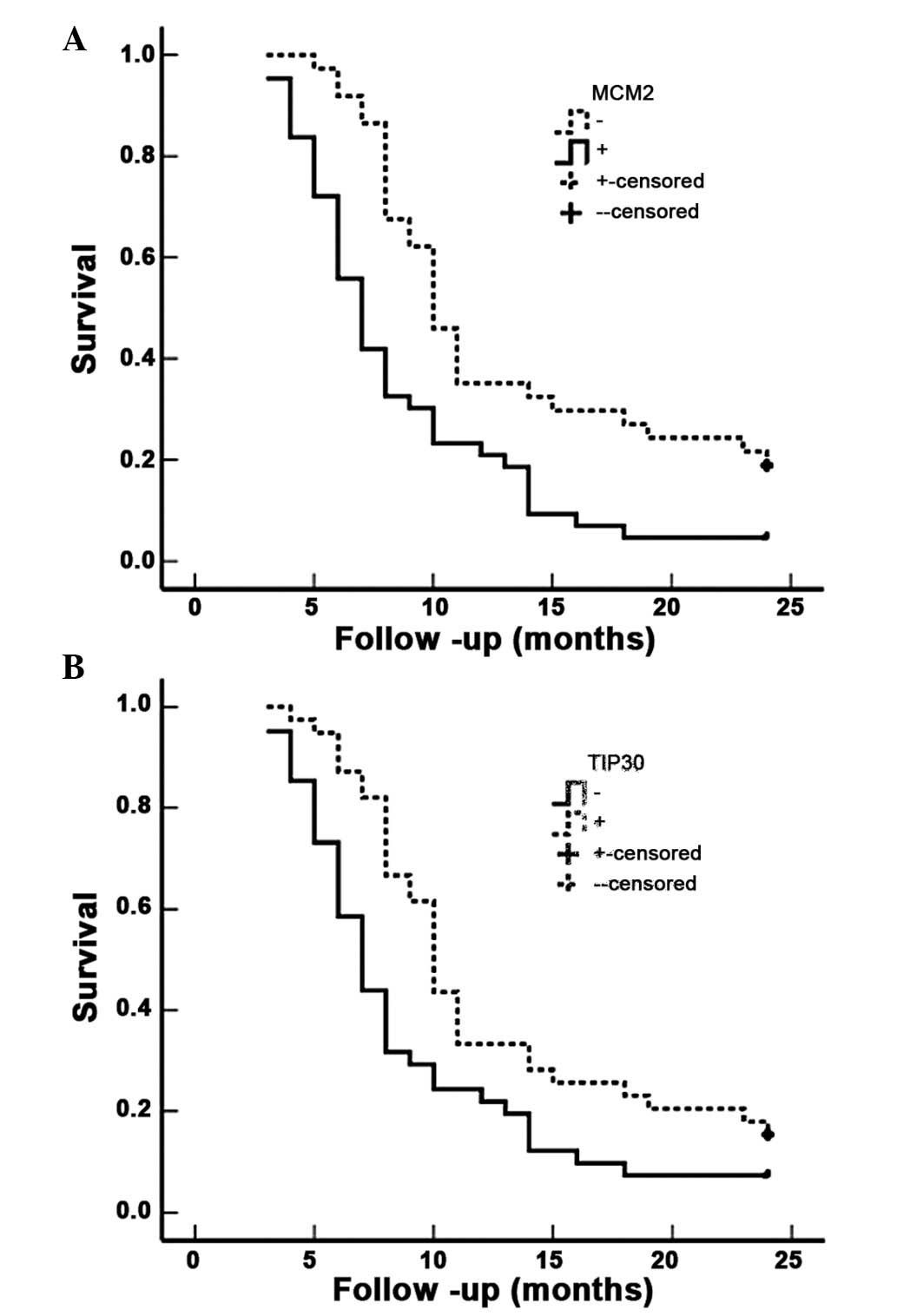
The correlation of MCM2 and/or TIP30
expression with survival in patients with SC/ASC and AC
Survival information for the 46 patients with SC/ASC
was obtained through letters and phone calls. The follow-up time
was 2 years, and patients who survived longer than 2 years were
included in the analysis as censored cases. A total of 13 patients
survived >1 year (of which 4 survived >2 years), and 33
patients survived <1 year, with a mean survival time of
10.07±0.78 months. Kaplan-Meier survival analysis demonstrated that
differentiation, tumor size, TNM stage, lymph node metastasis,
invasion and the operative procedure were significantly associated
(P<0.001) with mean survival time in SC/ASC patients (Table IV). The mean survival time of
MCM2-positive patients was significantly lower compared with
MCM2-negative patients (P<0.001). In contrast, the mean survival
time of TIP30-positive patients was significantly greater than
TIP30-negative patients (P<0.001) (Table IV; Fig. 3). Cox multivariate analysis
indicated that tumor size ≥3 cm, TMN stage, lymph node metastasis,
invasion, operative procedure and MCM2-positive expression or
TIP30-negative expression were negatively correlated with
post-operative survival, and positively correlated with mortality.
This suggests that MCM2 positivity is a risk factor, and that TIP30
is a prognostic indicator in SC/ASC (Table V).
 | Table IV.Association between MCM2 and TIP30
expression, clinicopathological characteristics and average
survival of SC/ASC patients. |
Table IV.
Association between MCM2 and TIP30
expression, clinicopathological characteristics and average
survival of SC/ASC patients.
| Clinicopathological
characteristics | Samples (n) | Average survival
(month) | Chi-square | P-value |
|---|
| Sex |
|
| 0.767 | 0.381 |
|
Male | 19 | 10.74 (6–24) |
|
|
|
Female | 27 | 9.85 (4–24) |
|
|
| Age (years) |
|
| 2.023 | 0.155 |
|
≤45 | 3 | 15.67 (8–24) |
|
|
|
>45 | 56 | 9.84 (4–25) |
|
|
| Pathological
type |
|
| 0.223 | 0.637 |
| SC | 26 | 10.19 (4–24) |
|
|
|
ASC | 20 | 10.25 (4–24) |
|
|
|
Differentiation |
|
| 19.125 | 0.000 |
|
Well | 16 | 13.81 (5–24) |
|
|
|
Moderately | 24 | 8.92 (4–18) |
|
|
|
Poorly | 6 | 5.83 (4–9) |
|
|
| Tumor mass
size |
|
| 31.337 | 0.000 |
| ≤3
cm | 20 | 14.35 (7–24) |
|
|
| >3
cm | 26 | 7.04 (4–11) |
|
|
| Gallstones |
|
| 3.730 | 0.053 |
| No | 18 | 8.22 (4–12) |
|
|
|
Yes | 28 | 11.50 (4–24) |
|
|
| TNM stage |
|
| 51.139 | 0.000 |
|
I+II | 12 | 17.00 (9–24) |
|
|
|
III | 20 | 9.20 (7–15) |
|
|
| IV | 14 | 5.86 (4–8) |
|
|
| Lymph node
metastasis |
|
| 16.219 | 0.000 |
| No | 17 | 14.24 (4–24) |
|
|
|
Yes | 29 | 7.86 (4–15) |
|
|
| Invasion |
|
| 32.271 | 0.000 |
| No | 16 | 15.75 (9–24) |
|
|
|
Yes | 30 | 7.27 (4–12) |
|
|
| Surgery |
|
| 50.165 | 0.000 |
|
Radical | 14 | 16.64 (10–24) |
|
|
|
Palliative | 18 | 8.50 (6–12) |
|
|
|
Biopsy | 14 | 6.00 (4–8) |
|
|
| MCM2 |
|
| 17.096 | 0.000 |
| − | 23 | 13.17 (6–24) |
|
|
| + | 23 | 7.26 (4–12) |
|
|
| TIP30 |
|
| 21.434 | 0.000 |
| − | 22 | 7.05 (4–12) |
|
|
| + | 24 | 13.13 (6–24) |
|
|
 | Table V.Multivariate Cox regression analysis
of survival rate in SC/ASC patients. |
Table V.
Multivariate Cox regression analysis
of survival rate in SC/ASC patients.
|
|
|
|
|
|
|
| 95% confidence
interval |
|---|
|
|
|
|
|
|
|
|
|
|---|
| Groups | Factors | RC | SE | Wald | P | RR | Lower | Upper |
|---|
| Pathological
types | SC/ASC | 0.108 | 0.360 | 0.090 | 0.764 | 1.114 | 0.550 | 2.256 |
| Differatiation |
Well/moderately/poorly | 1.100 | 0.399 | 7.600 | 0.006 | 3.004 | 1.374 | 6.567 |
| Tumor mass
size | ≤3/>3 cm | 2.351 | 0.791 | 8.834 | 0.003 | 10.496 | 2.227 | 49.470 |
| Gallstone | No/yes | 0.859 | 0.479 | 3.216 | 0.073 | 2.361 | 0.923 | 6.037 |
| TNM stage | I+II/III/IV | 1.252 | 0.518 | 5.842 | 0.016 | 3.497 | 1.267 | 9.653 |
| Lymph
metastasis | No/yes | 1.180 | 0.473 | 6.224 | 0.013 | 3.254 | 1.288 | 8.224 |
| Invasion | No/yes | 2.624 | 0.809 | 10.520 | 0.001 | 13.791 | 2.825 | 67.332 |
| Surgery |
Radical/palliative/biopsy | 1.084 | 0.467 | 5.388 | 0.020 | 2.956 | 1.184 | 7.384 |
| MCM2 | −/+ | 1.136 | 0.488 | 5.419 | 0.020 | 3.114 | 1.197 | 8.105 |
| TIP30 | −/+ | −0.981 | 0.470 | 4.357 | 0.037 | 0.375 | 0.149 | 0.942 |
The survival information of 80 patients with AC was
also obtained. A total of 23 patients survived >1 year (of which
9 survived >2 years), and 57 survived <1 year; the mean
survival time was 10.34±0.63 months. Kaplan-Meier survival analysis
indicated that differentiation, tumor size, TNM stage, lymph node
metastasis, invasion and operative procedure were significantly
associated (P<0.001) with the mean survival time of patients
with AC (Table VI). The mean
survival time of MCM2-positive patients with AC was significantly
lower than that of MCM2-negative patients with AC (P=0.001),
whereas the mean survival time of TIP30-positive patients was
significantly higher than TIP30-negative patients (P=0.009)
(Table VI; Fig. 4). Cox multivariate analysis
demonstrated that differentiation, tumor size ≥3 cm, TMN stage,
lymph node metastasis, invasion, operative procedure and
MCM2-positive or TIP30-negative expression were positively
correlated with poor survival in patients with AC (Table VII).
 | Table VI.Association between MCM2 and TIP30
expression, clinicopathological characteristics and average
survival of AC patients. |
Table VI.
Association between MCM2 and TIP30
expression, clinicopathological characteristics and average
survival of AC patients.
| Clinicopathological
characteristics | Samples (n) | Average survival
(month) | Chi-square | P-value |
|---|
| Sex |
|
| 2.567 | 0.109 |
|
Male | 26 | 9.58 (3–24) |
|
|
|
Female | 54 | 11.30 (3–24) |
|
|
| Age (years) |
|
| 0.003 | 0.956 |
|
≤45 | 16 | 10.81 (4–24) |
|
|
|
>45 | 64 | 10.72 (3–24) |
|
|
|
Differentiation |
|
| 32.501 | 0.000 |
|
Well | 27 | 15.07 (5–24) |
|
|
|
Moderately | 25 | 10.60 (4–24) |
|
|
|
Poorly | 28 | 6.68 (3–14) |
|
|
| Tumor mass
size |
|
| 68.283 | 0.000 |
| ≤3
cm | 50 | 13.70 (6–24) |
|
|
| >3
cm | 30 | 5.80 (3–10) |
|
|
| Gallstones |
|
| 0.246 | 0.620 |
| No | 42 | 10.19 (3–24) |
|
|
|
Yes | 38 | 11.34 (4–24) |
|
|
| TNM stage |
|
| 105.825 | 0.000 |
|
I+II | 21 | 18.96 (5–24) |
|
|
|
III | 38 | 9.29 (6–15) |
|
|
| IV | 21 | 5.14 (3–7) |
|
|
| Lymph node
metastasis |
|
| 42.372 | 0.000 |
| No | 30 | 16.27 (4–24) |
|
|
|
Yes | 50 | 7.42 (3–14) |
|
|
| Invasion |
|
| 55.535 | 0.000 |
| No | 31 | 16.68 (7–24) |
|
|
|
Yes | 49 | 6.98 (3–11) |
|
|
| Surgery |
|
| 113.141 | 0.000 |
|
Radical | 26 | 18.31 (10–24) |
|
|
|
Palliative | 28 | 8.64 (6–11) |
|
|
|
Biopsy | 26 | 5.42 (3–9) |
|
|
| MCM2 |
|
| 11.466 | 0.001 |
| − | 37 | 13.24 (5–24) |
|
|
| + | 43 | 8.58 (3–24) |
|
|
| TIP30 |
|
| 6.894 | 0.009 |
| − | 41 | 8.95 (3–24) |
|
|
| + | 39 | 12.62 (4–24) |
|
|
 | Table VII.Multivariate Cox regression analysis
of survival rate in patients with AC. |
Table VII.
Multivariate Cox regression analysis
of survival rate in patients with AC.
|
|
|
|
|
|
|
| 95% confidence
interval |
|---|
|
|
|
|
|
|
|
|
|
|---|
| Groups | Factors | RC | SE | Wald | P | RR | Lower | Upper |
|---|
| Differatiation |
Well/moderately/poorly | 1.364 | 0.514 | 7.042 | 0.008 | 3.912 | 1.428 | 10.713 |
| Tumor mass
size | ≤3/>3cm | 1.290 | 0.430 | 9.000 | 0.003 | 3.633 | 1.564 | 8.438 |
| Gallstone | No/yes | 0.151 | 0.270 | 0.313 | 0.576 | 1.163 | 0.685 | 1.974 |
| TNM stage | I+II/III/IV | 1.194 | 0.469 | 6.481 | 0.011 | 3.300 | 1.316 | 8.275 |
| Lymph
metastasis | No/yes | 1.059 | 0.446 | 5.638 | 0.018 | 2.883 | 1.203 | 6.911 |
| Invasion | No/yes | 1.386 | 0.506 | 7.503 | 0.006 | 3.999 | 1.483 | 10.781 |
| Surgery |
Radical/palliative/biopsy | 1.426 | 0.479 | 8.863 | 0.003 | 4.162 | 1.628 | 10.642 |
| MCM2 | −/+ | 0.995 | 0.393 | 6.410 | 0.011 | 2.705 | 1.252 | 5.843 |
| TIP30 | −/+ | −0.857 | 0.374 | 5.251 | 0.022 | 0.424 | 0.204 | 0.883 |
Discussion
Previous studies suggested that squamous carcinoma
proliferates at a higher rate than AC, however lymph node
metastasis is less common with squamous tumors (26,27).
The results of the current study observed no differences in
invasion and lymph node metastasis between AC and SC/ASC, however
an increased number of patients with SC/ASC had an increased tumor
size. There were also no significant differences in
differentiation, TNM stage, surgical curability and post-operative
survival time between patients with AC (10.34±0.63 months) and
SC/ASC (10.07±0.78 months). These observations suggest that
squamous differentiation is no more aggressive than glandular
differentiation in the gallbladder. In addition, it was observed
that radical resection was a good prognostic factor in patients
with AC and SC/ASC. However, 86% of patients with SC/ASC and 74%
with AC were diagnosed at an inoperable stage. Inconsistent with a
previous report concluding that SC/ASC occurs predominantly in
females (F/M=3.8) (6), no
difference in the prevalence of SC/ASC between females and males
(F/M ratio=1.4) was observed in the current study. However, the
prevalence of SC/ASC among older patients was increased compared
with AC. Consistent with previous reports (2,6), it
was observed that 4.34% of GBCs were SC/ASC. This suggests that the
clinicopathological presentation of SC/ASC was not significantly
different from AC. Current knowledge of the clinicopathological
characteristics of SC/ASC was obtained predominantly from
individual case reports or the analysis of small case series.
Therefore, the present study provided more accurate information
describing the differences between the rare SC/ASC subtype and the
more common AC.
Accumulating evidence has demonstrated that low
levels of expression of TIP30 and increased expression of MCM2
correspond with increased malignancy of tumors, high incidence of
metastasis, poor prognosis and high invasive potential (28–31).
In the present study, an extensive collection of human gallbladder
SC/ASC and AC samples was used to demonstrate that elevated MCM2 or
lowered TIP30 levels are important prognostic factors, independent
of other clinicopathological factors.
MCM2 is a key protein that regulates the transition
of a cell from G1 phase to S phase; its expression is
silenced in mature cells or those in G0. Therefore, MCM2
is a specific marker that indicates an active state of cell
proliferation (28,29). TIP30 is a serine/threonine kinase
that blocks cell function at G0/G1 phase,
which subsequently reduces the proportion of cells in S phase.
However, the clinicopathological characteristics of these proteins
in GBC remain to be fully elucidated. Previous studies reported
that MCM levels could reflect tumor carcinogenesis and progression
(9,14). Because of its high specificity and
sensitivity for determining cell proliferation, MCM2 may be a
malignant marker. MCM2 has been used for population screening for
neoplasms for a range of benign lesions using exfoliated cells
(32–34). Positive MCM2 and negative TIP30
expression were significantly associated with large tumor size,
high TNM stage, invasion, lymph node metastasis, and no surgical
curability (only biopsy) of SC/ASC and AC. Therefore, high
expression of MCM2 and low expression of TIP30 may be used as a
biological marker to identify subgroups of patients who may require
more aggressive treatment. Patients with high MCM2 and low TIP30
expression in their tumors are more likely to suffer from
metastatic recurrence. These patients may need to be monitored
closely for clinical signs of relapse to ensure that therapeutic
inventions are applied early enough for optimal outcomes. It is
reasonable to predict that the combination of MCM2(+) and TIP30(−)
may be a powerful predictor for malignant metastasis and a
biomarker for the early diagnosis and grading of GBC.
Previous studies demonstrated that MCM levels may
reflect clinical behavior and prognosis of cancer (9,14).
In the current study, Kaplan-Meier survival analysis indicated that
the survival time of patients with positive expression of MCM2 was
significantly shorter than that of patients with negative
expression; Cox multivariate analysis indicated that MCM2
expression was positively correlated with mortality. Conversely,
patients expressing TIP30 survived longer than those with negative
expression of TIP30; Cox multivariate analysis identified that
TIP30 expression was positively correlated with post-operative
survival. Therefore, MCM2 and TIP30 are proposed as two independent
prognostic factors.
The surgical removal of the gallbladder with
dissection of part of the liver and the lymph nodes is currently
the most common treatment for resectable GBC. However, the majority
of patients present with poor prognosis and will experience a
survival time of <1 year. Due to the fact that palliative
chemotherapy and radiation therapy offer little benefit in GBC
(2), there is an urgent
requirement for novel therapeutic approaches to improve patient
survival. Malignant tumors with high expression of MCM2 have an
increased rate of progression, are prone to metastasis and invasion
and have poor prognosis. TIP30 inhibits tumor growth and metastasis
by regulating the expression of cell proliferation-, apoptosis-,
and angiogenesis-associated genes (35,36).
High expression of MCM2 and low expression of TIP30 in gallbladder
tumor cells may allow them to be targeted for gene therapy. There
are several possible pathways for the development of novel
treatments for GBC based on the molecular targeting of MCM2 and
TIP30. For example, viral- or non viral-based delivery (such as the
nanoparticle-based delivery of small interfering RNA) could be used
to silence MCM2 expression alone or in combination with the
overexpression of TIP30. Notably, MCM proteins are specifically
required in cycling cells, however are absent from quiescent cells.
Therefore, using the MCM2 promoter to drive the expression of TIP30
or other apoptotic genes may provide tumor-specific targeting in
gallbladder AC or other tumor types that express MCM proteins.
In conclusion, reduced expression of TIP30 and
elevated expression of MCM2 are important markers for the
progression, clinical biological behavior, and prognosis of
gallbladder SC/ASC and AC. Measuring MCM2 and TIP30 expression may
be a tool for the early detection of GBC in benign lesions in
addition to in population screening. The observation that MCM
proteins are required only in cycling cells and are not expressed
in quiescent cells, in addition to the role of TIP30 in inhibiting
tumor growth, suggests that these two markers have potential to be
developed as targets for gene therapy by silencing MCM2 expression
and/or overexpressing TIP30.
Acknowledgements
The current study was supported by the Department of
Pathology, Basic School of Medicine (Changsha, China); Department
of Pathology, Second Xiangya Hospital (Changsha, China); Department
of Pathology, Third Xiangya Hospital (Changsha, China); Department
of Pathology, Loudi Central Hospital (Loudi, China); and the
Department of Pathology, Hunan Provincial Tumor Hospital (Changsha,
China). The present study was supported by a grant from the
National Natural Science Foundation of China (grant no.
81472738).
References
|
1
|
Jemal A, Siegel R, Ward E, Hao Y, Xu J,
Murray T and Thun MJ: Cancer statistics, 2008. CA Cancer J Clin.
58:71–96. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Jayaraman S and Jarnagin WR: Management of
gallbladder cancer. Gastroenterol Clin North Am. 39:331–342. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Reid KM, Ramos-De la Medina A and Donohue
JH: Diagnosis and surgical management of gallbladder cancer: A
review. J Gastrointest Surg. 11:671–681. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Hawkins WG, DeMatteo RP, Jarnagin WR,
Ben-Porat L, Blumgart LH and Fong Y: Jaundice predicts advanced
disease and early mortality in patients with gallbladder cancer.
Ann Surg Oncol. 11:310–315. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Ootani T, Shirai Y, Tsukada K and Muto T:
Relationship between gallbladder carcinoma and the segmental type
of adenomyomatosis of the gallbladder. Cancer. 69:2647–2652. 1992.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Roa JC, Tapia O, Cakir A, Basturk O,
Dursun N, Akdemir D, Saka B, Losada H, Bagci P and Adsay NV:
Squamous cell and adenosquamous carcinomas of the gallbladder:
Clinicopathological analysis of 34 cases identified in 606
carcinomas. Mod Pathol. 24:1069–1078. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Park SB, Kim YH, Rho HL, Chae GB and Hong
SK: Primary carcinosarcoma of the gallbladder. J Korean Surg Soc.
82:54–58. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Liu DC and Yang ZL: MTDH and EphA7 are
markers for metastasis and poor prognosis of gallbladder
adenocarcinoma. Diagn Cytopathol. 41:199–205. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Giaginis C, Vgenopoulou S, Vielh P and
Theocharis S: MCM proteins as diagnostic and prognostic tumor
markers in the clinical setting. Histol Histopathol. 25:351–370.
2010.PubMed/NCBI
|
|
10
|
MacCallum DE and Hall PA: The biochemical
characterization of the DNA binding activity of pKi67. J Pathol.
191:286–298. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Mehrotra P, Gonzalez MA, Johnson SJ,
Coleman N, Wilson JA, Davies BR and Lennard TW: Mcm-2 and Ki-67
have limited potential in preoperative diagnosis of thyroid
malignancy. Laryngoscope. 116:1434–1438. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Brown DC and Gatter KC: Ki67 protein: The
immaculate deception? Histopathology. 40:2–11. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Toschi L and Bravo R: Changes in
cyclin/proliferating cell nuclear antigen distribution during DNA
repair synthesis. J Cell Biol. 107:1623–1628. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Tachibana KE, Gonzalez MA and Coleman N:
Cell-cycle-dependent regulation of DNA replication and its
relevance to cancer pathology. J Pathol. 205:123–129. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Stoeber K, Tlsty TD, Happerfield L, Thomas
GA, Romanov S, Bobrow L, Williams ED and Williams GH: DNA
replication licensing and human cell proliferation. J Cell Sci.
114:2027–2041. 2001.PubMed/NCBI
|
|
16
|
Madine MA, Swietlik M, Pelizon C,
Romanowski P, Mills AD and Laskey RA: The roles of the MCM, ORC,
and Cdc6 proteins in determining the replication competence of
chromatin in quiescent cells. J Struct Biol. 129:198–210. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Chatrath P, Scott IS, Morris LS, Davies
RJ, Rushbrook SM, Bird K, Vowler SL, Grant JW, Saeed IT, Howard D,
et al: Aberrant expression of minichromosome maintenance protein-2
and Ki67 in laryngeal squamous epithelial lesions. Br J Cancer.
89:1048–1054. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Davies RJ, Freeman A, Morris LS, Bingham
S, Dilworth S, Scott I, Laskey RA, Miller R and Coleman N: Analysis
of minichromosome maintenance proteins as a novel method for
detection of colorectal cancer in stool. Lancet. 359:1917–1919.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Sirieix PS, O'Donovan M, Brown J, Save V,
Coleman N and Fitzgerald RC: Surface expression of minichromosome
maintenance proteins provides a novel method for detecting patients
at risk for developing adenocarcinoma in Barrett's esophagus. Clin
Cancer Res. 9:2560–2566. 2003.PubMed/NCBI
|
|
20
|
Zhao J, Zhang X, Shi M, Xu H, Jin J, Ni H,
Yang S, Dai J, Wu M and Guo Y: TIP30 inhibits growth of HCC cell
lines and inhibits HCC xenografts in mice in combination with 5-FU.
Hepatology. 44:205–215. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Shtivelman E: A link between metastasis
and resistance to apoptosis of variant small cell lung carcinoma.
Oncogene. 14:2167–2673. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
NicAmhlaoibh R and Shtivelman E:
Metastasis suppressor CC3 inhibits angiogenic properties of tumor
cells in vitro. Oncogene. 20:270–275. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Xiao H, Palhan V, Yang Y and Roeder RG:
TIP30 has an intrinsic kinase activity required for up-regulation
of a subset of apoptotic genes. EMBO J. 19:956–963. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Li X, Zhang Y, Cao S, Chen X, Lu Y, Jin H,
Sun S, Chen B, Liu J, Ding J, et al: Reduction of TIP30 correlates
with poor prognosis of gastric cancer patients and its restoration
drastically inhibits tumor growth and metastasis. Int J Cancer.
124:713–721. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Ito M, Jiang C, Krumm K, Zhang X, Pecha J,
Zhao J, Guo Y, Roeder RG and Xiao H: TIP30 deficiency increases
susceptibility to tumorigenesis. Cancer Res. 63:8763–8767.
2003.PubMed/NCBI
|
|
26
|
Nishihara K, Nagai E, Izumi Y, Yamaguchi K
and Tsuneyoshi M: Adenosquamous carcinoma of the gallbladder: A
clinicopathological, immunohistochemical and flow-cytometric study
of twenty cases. Jpn J Cancer Res. 85:389–399. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Kondo M, Dono K, Sakon M, Shimizu J,
Nagano H, Nakamori S, Umeshita K, Wakasa K and Monden M:
Adenosquamous carcinoma of the gallbladder. Hepatogastroenterology.
49:1230–1234. 2002.PubMed/NCBI
|
|
28
|
Tye BK: MCM proteins in DNA replication.
Annu Rev Biochem. 68:649–686. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Lei M and Tye BK: Initiating DNA synthesis
from recruiting to activating the MCM complex. J Cell Sci.
114:1447–1454. 2001.PubMed/NCBI
|
|
30
|
Zhang H, Zhang Y, Duan HO, Kirley SD, Lin
SX, McDougal WS, Xiao H and Wu CL: TIP30 is associated with
progression and metastasis of prostate cancer. Int J Cancer.
123:810–816. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Zhao J, Ni H, Ma Y, Dong L, Dai J, Zhao F,
Yan X, Lu B, Xu H and Guo Y: TIP30/cc3 expression in breast
carcinoma: Relation to metastasis, clinicopathologic parameters,
and P53 expression. Hum Pathol. 38:293–298. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Gakiopoulou H, Korkolopoulou P, Levidou G,
Thymara I, Saetta A, Piperi C, Givalos N, Vassilopoulos I, Ventouri
K, Tsenga A, et al: Minichromosome maintenance 2 and 5 in
non-benign epithelial ovarian tumours: Relationship with cell cycle
regulators and prognostic implications. Br J Cancer. 97:1124–1134.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Reena RM, Mastura M, Siti-Aishan AM,
Munirah MA, Norlia A, Naqiyah I, Rohaizak M and Sharifah NA:
Minichromosome maintenance 2 is a reliable proliferative marker in
breast carcinoma. Ann Diagn Pathol. 12:340–343. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Giaqinis C, Georgiadou M, Dimakopoulou K,
Tsourouflis G, Gatzidou E, Kouraklis G and Theocharis S: Clinical
significance of MCM-2, MCM-5 expression in colon cancer:
Association with clinicopathological parameters and tumor
proliferative capacity. Dig Dis Sci. 54:282–291. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Xiao H, Tao Y, Greenblatt J and Roeder RG:
A cofactor, TIP30, specifically enhances HIV-1 Tat-activated
transcription. Proc Natl Acad Sci USA. 95:2146–2151. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Shtivelman E: A link between metastasis
and resistance to apoptosis of variant small cell lung carcinoma.
Oncogene. 14:2167–2173. 1997. View Article : Google Scholar : PubMed/NCBI
|