Introduction
Identification of breast cancer stem cells (BCSCs)
from tumor samples or breast cancer cell lines has been based
primarily on cluster of differentiation (CD)
44+/CD24−/low or aldehyde
dehydrogenase (ALDH)+ phenotypes (1). Due to their invasiveness, resistance
to chemo- and radiotherapy, mesenchymal phenotype and hypothesized
role in seeding distant metastases, agents that specifically target
the population of breast cancer cells bearing the
CD44posCD24neg/low cell surface phenotype,
which was first described by Vazquez-Martin et al (2) as a cardinal feature of BCSCs, are
required. However, it is well-known that, in addition to CD44
expression, the expression of ALDH1 and Twist1 is involved in
breast cancer invasion, metastasis and relapse. ALDH1 is a marker
of normal and malignant human mammary stem cells and a predictor of
poor clinical outcome (3). A
previous study (4) reported that
the overexpression of Twist1 can promote upregulation of ALDH1. The
basic helix-loop-helix transcription factor Twist1 was previously
demonstrated (5) to be a potent
promoter of both cancer cell dissemination into circulation and
metastases, providing a promising therapeutic target for
intervention (6). Twist1 can
activate a latent process termed the epithelial-mesenchymal
transition (EMT), thus enabling carcinoma cells to dissociate from
each other and migrate (7). For
epithelial malignancies, EMT is a crucial event in the
dissemination of cancer cells (8).
Further understanding of the mechanisms by which Twist1 promotes
metastasis and the identification of Twist1 functional modulators
may hold promise for developing novel strategies to inhibit EMT and
cancer metastases (9). Currently,
lymph node metastases (LNM) are considered to be a manifestation of
widespread metastatic process and more useful markers of an
aggressive primary tumor (PT) compared with the ‘bridgeheads’ for
predicting further metastatic spread (10). LNM are enriched in cells with more
aggressive phenotypes, marked by elevated levels of EMT regulators
(11). Experimental models provide
further evidence that the development of LNM indicates the
increased potential of PT to disseminate aggressive cells and
produce metastasis-promoting growth factors (10). Thus, molecular profiling of LNM may
be used as a surrogate marker for the aggressiveness and metastatic
potential of PT (11). At present,
a variety of biological tumor markers are studied to diagnose these
early diseases, monitor recurrence or metastasis in treated
patients and to predict response or resistance to therapies
(7). Carcinoma antigen 15–3
(CA15-3) is a member of a polymorphous group of highly glycosylated
proteins (12,13) and is the most widely-applied serum
marker due to the fact that it is easy to use, cheap and quick to
use. CA15-3 is particularly useful for tracking treatment in those
patients who cannot be assessed by radiology. Due to the lack of
specificity, measurement of CA15-3 serum levels alone is not
suitable for the follow-up of patients with breast cancer. However,
at present, CA15-3, carcinoembryonic antigen (CEA) and others are
primarily utilized to monitor therapy in metastatic breast cancer
in combination with imaging, history and physical examination
(14).
Therefore, the present study assumed that targeting
LNM and a combination of Twist1and CA15-3 levels were significant
for prognosis of breast cancer because Twist1 served a vital role
in promoting tumor cell metastasis and recurrence.
Materials and methods
Reagents
Allophycocyanin (APC)-conjugated rabbit anti-human
CD24 (catalogue no. sc-11406 FL-80) and rabbit anti-human Twist1
(catalogue no. sc-15393 H-81) antibodies were obtained from Santa
Cruz Biotechnology, Inc. (Santa Cruz, CA, USA). Rabbit anti-human
CD44 (catalogue no. GTX 102111) was obtained from GeneTex, Inc.
(Irvine, CA, USA). ALDH1 (catalogue no. ab52492) was obtained from
Abcam, Shanghai, China. The donkey anti-rabbit IgG-fluorescein
isothiocyanate (FITC) antibodies (catalogue no: SA00003-8) and goat
anti-rabbit phycoerythin (PE) antibodies (catalogue no: SA00008-2)
were from Wuhan Sanying Biotechnology, Wuhan, China. The rabbit
anti-histone H3 antibody (catalogue no. ZDR-5105) was from Beijing
Zhongshan Jinqiao Biotechnology Co., Ltd (Beijing, China). Vimentin
(catalogue no: CST 5741P D21H3) and N-cadherin (catalogue no:
CST13116p) antibodies were from Cell Signaling Technologies, Inc.
(Danvers, MA, USA). The primer synthesis, reverse
transcription-quantitative polymerase chain reaction (RT-qPCR) kit
(catalogue no. RP1202) and western blotting kits were provided by
Takara Biotechnology Co., Ltd., (Dalian, China).
4′,6-diamidino-2-phenylindole (DAPI) was purchased from Molecular
Probes, Inc. (Thermo Fisher Scientific, Inc., Waltham, MA, USA).
The X-ray film for autoradiography was from Kodak (Rochester, NY,
USA). The chemiluminescence immunoassay kit was purchased from
Roche Diagnostics (Indianapolis, IN, USA). The hematoxylin and
eosin (H&E) staining kit was from Shanghai Shenggong Biology
Engineering Technology Service, Ltd. (Shanghai, China).
Ethics statement
Research specimens were collected from surgically
removed tumor tissues and the clinicopathological data were
obtained after the selected patients signed informed consent forms.
These forms allowed the use of the biological tissues for research
purposes. All protocols were approved by the Ethics Committee of
Affiliated Yong Chuan Hospital of Chongqing Medical University
(Chongqing, China).
Tissue specimens
A total of 102 patients with primary breast cancer
underwent definitive surgery from 2007 to 2014 at the Department of
Breast Gland Surgery in The Second Affiliated Hospital of Chongqing
Medical University (Chongqing, China). All patients were Chinese
females aged 38–69 years old. Availability of PT and matched LNM
was mandatory. Patients with no evidence of lymph node involvement
or earlier chemotherapy were deemed ineligible for the present
study. Non-cancer control breast tissue samples were acquired
during mastectomy. Patient survival data was collected at this
stage; information on patients included age, tumor size, nodal
status, tumor grade, histological tumor type, and ER, PR and human
epidermal growth factor receptor 2 (HER2) status, was obtained from
the Department of Breast Gland Surgery and Pathology of the
hospital. HER2 expression status was scored with MoAb clone CB11, a
monoclonal antibody (Novocastra; Leica Biosystems, Newcastle Ltd.,
Newcastle, UK). The data treated by immunohistochemistry were
collected from Department of Pathology, The Second Affiliated
Hospital of Chongqing Medical University. The tumor tissues were
immediately frozen following removal and stored at −80°C in liquid
nitrogen. Finally, total RNA and protein were isolated from frozen
tumor tissues using TRizol reagent or DAPI NP-40 lysis buffer,
respectively. All specimens were stored in a −80°C freezer
(Invitrogen; Thermo Fisher Scientific, Inc.).
Immunofluorescence and laser confocal
scanning analysis
Laser confocal scanning analysis was performed as
described previously (15).
Sections of human breast gland and ALN tissues were first
identified to be breast cancer and matched ALN metastases with
H&E staining. The sample slides were then treated by
immunofluorescence staining. After a wash in 0.01 M/l
phosphate-buffered saline (PBS; pH 7.4), the samples were incubated
with a blocking buffer (1% bovine serum albumin, 5% normal goat
serum and 0.1% Triton X-100-PBS) for 1 h at room temperature.
Samples were then incubated with primary rabbit anti-human
antibodies (CD44, CD24, Twist1 and ALDH1; 1:200 dilution) and
diluted in the blocking buffer at 4°C overnight in a humidified
chamber, followed by three washes in PBS for 15 min each. The
samples were then stained with secondary antibodies (donkey
anti-rabbit IgG-FITC antibodies for the CD44 and ALDH1 sections,
and goat anti-rabbit PE antibodies for the CD24 and Twist1
sections; 1:2,000 dilution) diluted in blocking buffer for 30 min,
followed by three washes in PBS. Coverslips were mounted on slides
with DAPI (ProLong® Gold antifade reagent; Molecular
Probes, Inc.; Thermo Fisher Scientific, Inc.). Positive control
slides were run simultaneously to assess the quality of
immunoreactivity. Normal ALN (30 mm away from the cancer tissue)
were used as negative controls. Finally, immunostained tissues were
visualized and imaged using an inverted optical microscope and an
inverted fluorescence confocal microscope.
Total RNA extraction from fresh-frozen
tissue
The tissue samples stored at −80°C were thawed and
immediately treated. Tissue sections of 20–30 mg were homogenized
with zircon beads in a MagNA Lyzer (Roche Diagnostics GmbH,
Mannheim, Germany) for 40 sec. Total RNA was isolated using the
RNeasy Mini kit (Takara Biotechnology Co., Ltd) according to the
manufacturer's protocol, including on-column DNase I treatment.
RNA analysis and reverse
transcription
To determine the gene expression of CD44, CD24,
ALDH1 and Twist1 in the specimens obtained from the surgery,
followed by the reverse transcription of RNA, sequences of the
human primers (provided by Takara Biotechnology Co., Ltd.) were
designed as follows: CD44, 5′GCC CAA TGC CTT TGA TGG ACC3′ (sense
primer), 3′GCA GGG ATT CTG TCT GTG CTG5′ (anti-sense primer); CD24,
5′-ATGGGCAGAGCAATGGTGGCCA-3′ (sense primer) and 3′TCA AGA GAA GCA
CCA GAG TGA GA5′ (anti-sense primer); Twist1, 5′CAA GAA GTC TGC GGG
CTG TG3′ (sense primer), 5′TCG TTC AGC GAC TGG GTGC3′ (anti-sense
primer); ALDH1, 5′CAA ACG ACC ATC TGC CGCT3′ (sense primer), 5′CAG
GTT GCC TCT CAC TCG GTT3′ (anti-sense primer). For all samples, the
RNA concentration and purity were determined using a Nano-Drop
ND-1000 spectrophotometer (Thermo Fisher Scientific, Inc.).
Qualitative analysis of the RNA was performed by microcapillary
electrophoresis using the Agilent 2100 Bioanalyzer with Expert
Software, version B.02.08 using an RNA Nano Chip (Agilent
Technologies, Inc., Santa Clara, CA, USA). For each sample,
whenever possible, 1 µg RNA was used as the template in the reverse
transcription reaction using the Transcriptor First Strand cDNA
Synthesis kit (Roche Diagnostics GmbH) in a 20 µl volume with
random hexamer primers according to the manufacturer's protocol.
Total PCR was processed for 35 cycles (95°C, 30 sec; 56°C, 30 sec;
72°C, 15 sec) with Taq DNA polymerase (Invitrogen; Thermo Fisher
Scientific, Inc.). Relative mRNA levels were quantified using SYBR
supermix (Bio-Rad Laboratories, Inc., Hercules, CA, USA) on an
iCycler iQ5 for 40 cycles (95°C, 30 sec; 54°C, 20 sec; 72°C, 15
sec) followed by default melting curve cycles, and IQ5 software for
PCR baseline subtraction (Bio-Rad laboratories, Inc.) was used for
analysis.
Fresh-frozen tissue for western blot
analysis
For western blot analysis, the tissue samples stored
at −80°C were quickly thawed and treated immediately. Whole cell
lysates were prepared from the frozen tissues. Briefly, following
centrifugation at 800–1000 × g, 4°C for 3 min, the samples were
collected by centrifugation and resuspended in 100 µM SDS sample
buffer [125 mM Tris-HCl, pH 6.8, 20% (v/v) glycerol, 2% (w/v) SDS,
0.2% (w/v) bromophenol blue] prior to boiling for 5 min.
Subsequently, 30 µg protein from each lysate was loaded onto 12%
SDS polyacrylamide gels, separated by electrophoresis and
transferred onto a nitrocellulose membrane prior to probing with
rabbit anti-vimentin and N-cadherin (1:2,000) at 4°C overnight. The
horseradish peroxidase-conjugated anti-rabbit secondary antibody
(1:1,000, catalogue no. ab6721, Abcam) was detected using the ECL
Advanced Western Blotting kit (Takara Biotechnology Co., Ltd.) and
visualized using the Molecular Imager ChemiDoc XRS System (Bio-Rad
Laboratories, Inc., Hercules, CA, USA). Lysates were probed with
rabbit anti-histone H3 antibody (1:2,500) as a loading control.
Tumor markers
In addition, 2 ml peripheral venous blood was
collected from each of the studied patients on the 4th day prior to
and the 3rd day following surgery respectively. This blood was used
to detect the serum CA15-3 levels, which are currently considered
useful tumor markers for breast cancer. Serum CA15-3 concentrations
were determined by chemiluminescence immunoassay using a
commercially available kit (Roche Diagnostics), and the cut-off
level recommended by the manufacturers was 30 U/ml. The within- and
between-assay coefficients of variation for CA15-3 were <9%.
Finally, the blood samples of the 102 patients were divided into
four groups: The stages I and II group, the stages III and IV
group, the pre-operative group and the post-operative group. The
increase in tumor markers was considered progressive when it was
>30% in the sample following the initial elevated value.
Statistical analysis
Statistical analyses of the results were performed
in Microsoft Excel 2007 (Microsoft Corporation, Redmond, WA, USA)
and SPSS software, version 15.0.1 (SPSS, Inc., Chicago, IL, USA)
and expressed as the mean ± standard deviation. Student's t-test
was used for paired comparisons between the data groups. A two-way
analysis of variance test was then conducted using the defining
factors comparison, among the multi-data groups and for
nonparametric tests. P<0.05 was considered to indicate a
statistically significant difference.
The patients were continuously followed-up for 6
years and 184 days after leaving the hospital. Progression-free
survival (PFS) was defined as the time from the first diagnosis of
breast cancer until the radiographical examination of progression.
Patient mortality without progressive evidence were treated as
events and the patients who were lost to follow-up were treated as
censored observations. The overall survival rate was defined as the
time from endocrine therapy until the mortality date or the most
recent follow-up. The median PFS and median survival time were
calculated using the Kaplan-Meier method, and marked statistical
differences in survival curves were examined using the log-rank
test.
Results
The clinicopathological data from the patients in
the current study are presented in Table I. A selected series of 102 primary
invasive breast carcinomas were included in the present study. All
histological sections of tumor specimens were re-evaluated by two
experienced pathologists. Each patient was staged according to the
International Union Against Cancer TNM classification (16). The tumor size was ≤2 cm in 35.7%
(n=45) of cases and >2 cm in 64.3% (n=57) of cases. Pathological
examination revealed that the status of all ALN was positive.
Histological grading was performed according to the Elston and
Ellis method (17) and 45.1%
(n=46) of tumors were histological grade 1–2 and 54.9% (n=56) were
grade 3. In addition, of all of the tumors 75 (73.8%) were invasive
ductal carcinoma not otherwise specified, with the remaining 27
(26.2%) consisting of other histological types, including medullary
and lobular tumors. The variables collected for the expression
analysis were estrogen receptor (ER) and progesterone receptor (PR)
status, human epidermal growth factor receptor 2 (HER2) status and
BCA225 antigen status. ER and PR were considered to be
overexpressed when >10% of the nuclei were positive. The HER2
status was scored as 0, 1+, 2+ or
3+. In accordance with the Dako HercepTest scoring
system; 0, no membranous immunoreactivity or <10% of cells
reactive; 1+, incomplete membranous reactivity in
>10% of cells; 2+, >0% of cells with weak to
moderate complete membranous reactivity; and 3+, strong
and complete membranous reactivity in >10% of cells. It was
noted that 32 of the 102 patients demonstrated the BCA225 antigen
>75 µg/l in their blood and the serum CEA level of 76.5%
(78/102) patients was >7 ng/l.
 | Table I.Clinicopathological data for the
patients in the present study; median (range) age 53.5 (41–71)
years old. |
Table I.
Clinicopathological data for the
patients in the present study; median (range) age 53.5 (41–71)
years old.
| Variable | Number of cases
(n=102) | % |
|---|
| Tumor stage |
|
|
|
T1–2 | 29 | 28.5 |
|
T3–4 | 73 | 71.5 |
| Nodes stage |
|
|
| N1 | 26 | 25.4 |
| N2 | 62 | 60.7 |
| N3 | 14 | 13.9 |
| ER status |
|
|
|
Negative | 36 | 35.3 |
|
Positive | 66 | 64.7 |
| PR status |
|
|
|
Negative | 72 | 70.5 |
|
Positive | 30 | 29.5 |
| HER2 status |
|
|
|
Negative | 77 | 75.5 |
|
Positive | 33 | 24.5 |
| Histological
type |
|
|
|
Ductal | 61 | 59.8 |
|
Lobular | 22 | 21.6 |
|
Other | 19 | 18.6 |
| Tumor grade |
|
|
|
G1–2 | 66 | 64.7 |
| G3 | 36 | 35.3 |
| BCA225 antigen |
|
|
| >75
µg/l | 69 | 67.6 |
| <75
µg/l | 63 | 32.4 |
| Serum CEA
level |
|
|
| >7
ng/l | 73 | 71.6 |
The median follow-up calculated by the Kaplan-Meier
method was 5 years and 224 days. The median follow-up of patients
who did not have an event (n=33) was 5 years and 317 days. Those
exhibiting local and regional relapse and died from tumors) were 3
years and 327 days (n=69). The average number of metastatic lymph
nodes was 4.8 (range 1–22).
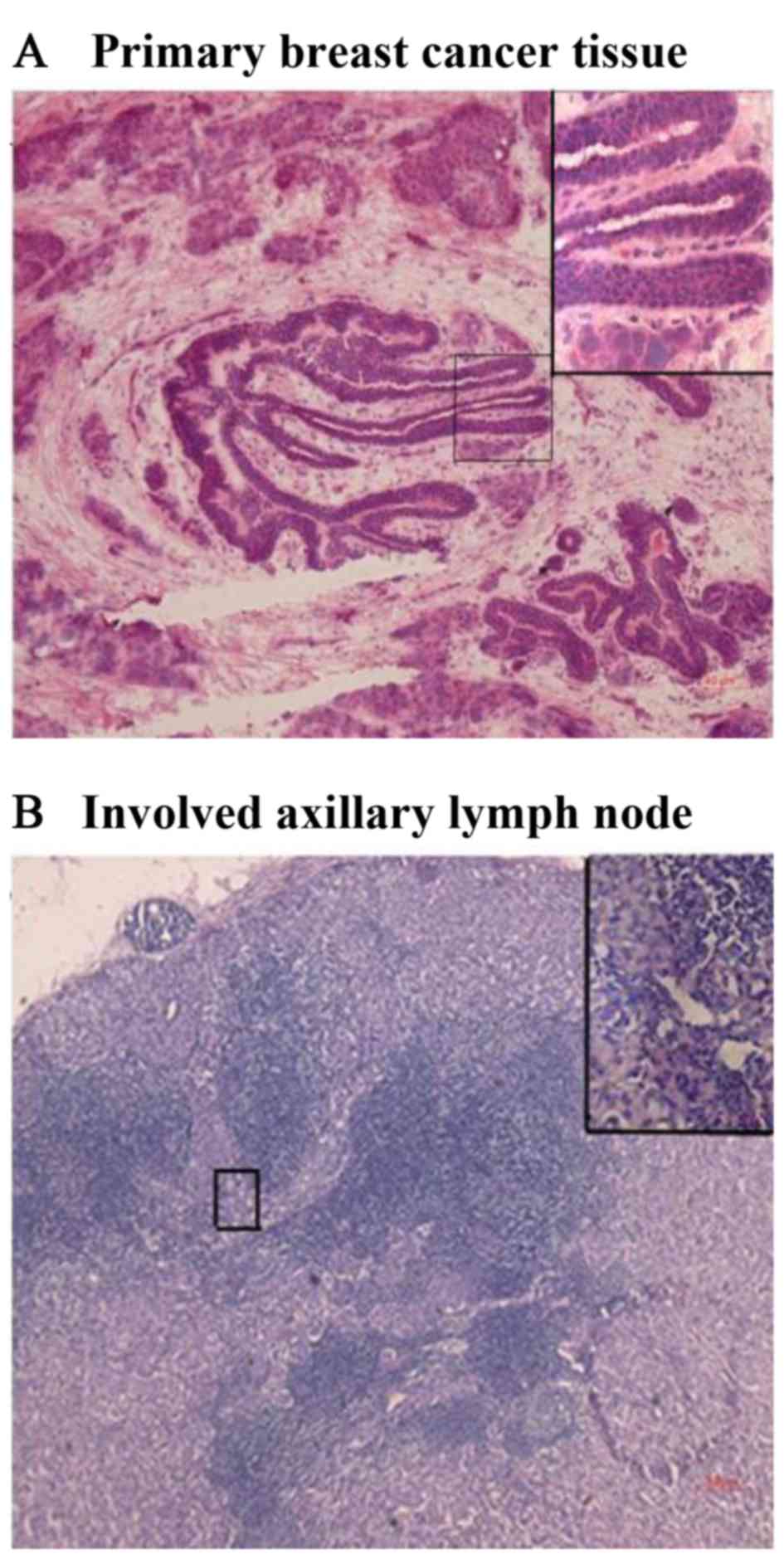
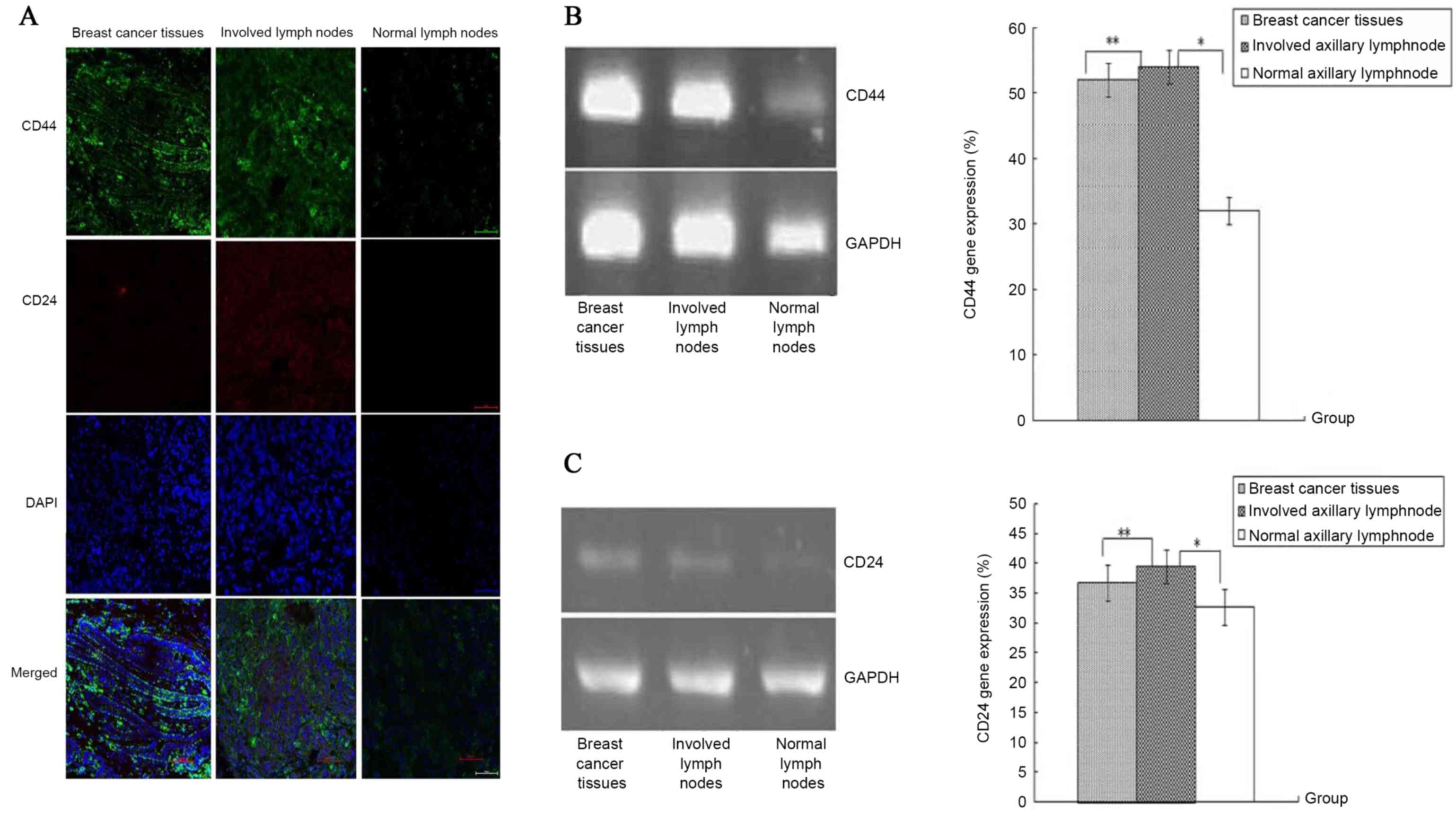
Expression of CD44 markedly increased
in PT and lymph node metastasis compared with normal lymph
nodes
To investigate whether BCSCs were present in the
collected specimens (the breast gland tissues, normal ALN and
involved ALN), the expression levels of CD44 and CD24 were
determined by immunofluorescence staining and laser confocal
microscope analysis with rabbit anti-human CD44 and CD24
antibodies, respectively. All slide sections, including breast
cancer tissues (Fig. 1A) and
involved ALN (Fig. 1B), were first
verified by H&E staining. The results of immunofluorescence
staining demonstrated that CD44 and CD24 were all expressed at low
levels in the normal ALN (Fig. 2A;
CD44 conjugated-FITC and CD24 conjugated-PE). However, CD44 was
strongly localized on the membranes of the tumor cells and existed
as an intercellular substance slightly distinct from the breast
cancer tissues and the involved ALN (Fig. 2A, CD44 conjugated-FITC and CD24
conjugated-PE). The results demonstrated that CD44 was more highly
expressed compared with CD24 in primary breast cancer tissues and
the involved ALN. RT-qPCR analysis for the three tissues
demonstrated that CD44 mRNA expression in the breast cancer tissue
and the involved ALN was significantly upregulated compared with
the normal ALN (Fig. 2B), and no
statistical difference was observed between the gene expression in
the breast cancer tissues and the metastatic ALN. Conversely, CD24
mRNA expression in the three samples was at low or not detectable
levels and no significant difference was observed (P>0.05;
Fig. 2C). The positive expression
of CD44 and CD24 is presented in Table II.
 | Table II.Overexpression of genes in the
primary breast cancer tissue and ALN. |
Table II.
Overexpression of genes in the
primary breast cancer tissue and ALN.
|
| Normal ALN-low
expression | Primary
tissue-overexpression | Involved
ALN-overexpression |
|---|
|
|
|
|
|
|---|
| Variable | n | % | n | % | P-value | n | % | P-value |
|---|
| CD44 | 75/102 | 73.5 | 89/102 | 87.3 | <0.05 | 84/102 | 82.4 | <0.05 |
| CD24 | 6/102 | 5.9 | 3/102 | 3.9 | >0.05 | 2/102 | 1.9 | >0.05 |
| ALDH1 | 52/102 | 51 | 78/102 | 76.5 | <0.05 | 87/102 | 85.3 | <0.05 |
| Twist1 | 54/102 | 52.9 | 82/102 | 80.4 | <0.05 | 71/102 | 69.6 | <0.05 |
ALDH1 overexpression in PT and
metastatic ALN
The status of ALDH1 expression in the samples was
detected with immunofluorescence staining and RT-qPCR analysis. The
immunofluorescence and laser confocal scanning staining (ALDH1
conjugated-FITC) demonstrated that ALDH1 was expressed in the
epithelial cytoplasm of the primary breast cancer tissues and the
involved ALN; at the same time, it was also weakly expressed in the
normal breast gland tissues (Fig.
3A). The positive expression of ALDH1 is presented in Table II. However, the observed densities
from the immunofluorescence staining were markedly brighter in the
primary breast cancer tissues and metastatic ALN (Fig. 3A) than in the normal ALN.
Furthermore, the results demonstrated that ALDH1 mRNA expression
was significantly higher in the breast cancer and involved ALN than
in the normal ALN (P<0.05; Fig.
3B). Furthermore, no statistical difference was observed
between the gene expression levels of the breast cancer tissues and
the metastatic ALN (P>0.05).
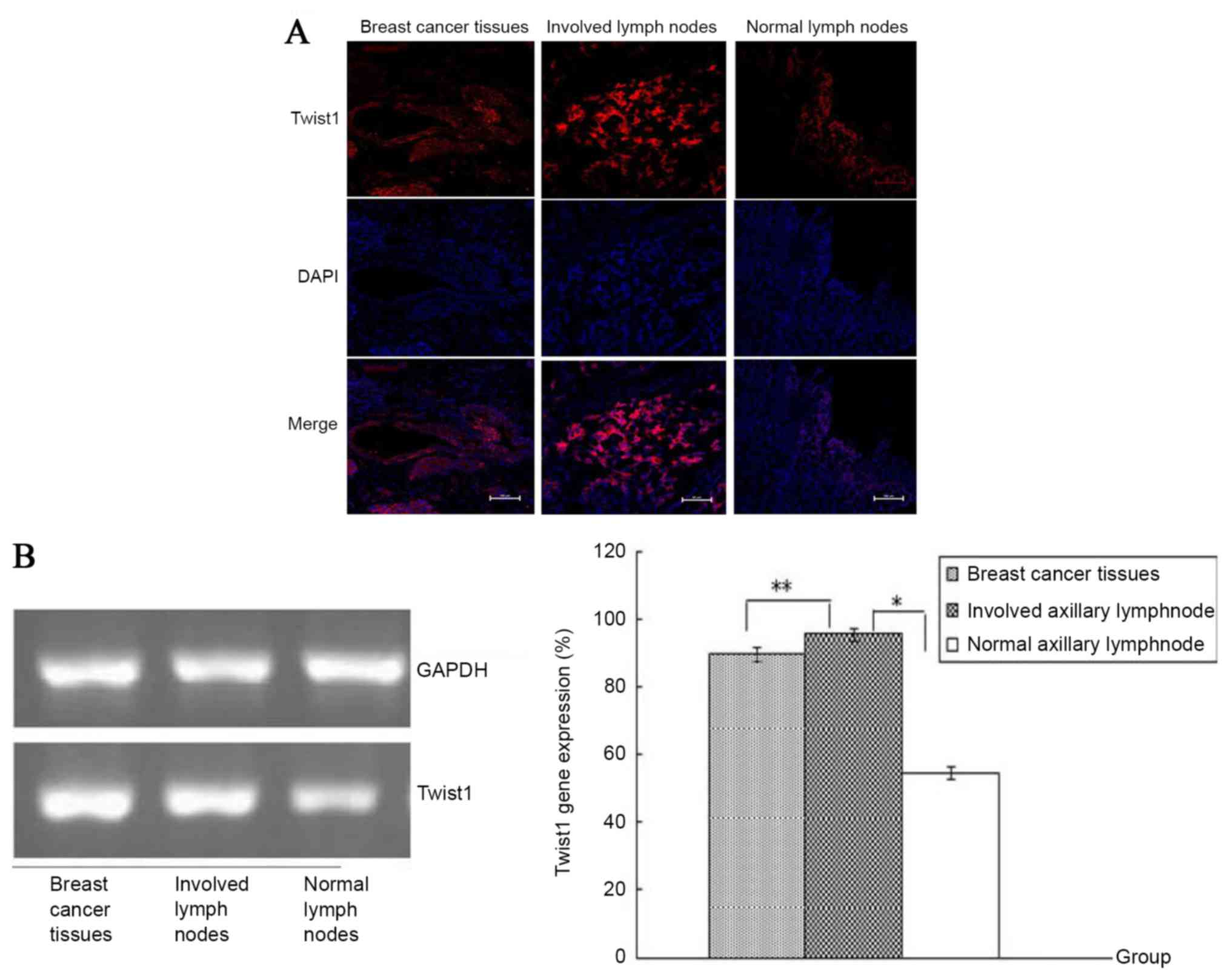
High expression of Twist1 in the PT
and metastatic ALN may contribute to the promotion of cancer cell
migration, invasion and metastasis
Following immunofluorescence staining and RT-qPCR
analysis, the results demonstrated that the Twist1 molecule was
predominantly localized in the nucleus and cytoplasm of tumor and
stromal cells whilst being additionally expressed in normal
tissues. However, the observed densities of immunofluorescence
staining were markedly weaker in the normal ALN than in the primary
breast cancer tissues and metastatic ALN (Fig. 4A; Twist1 conjugated-PE). The
positive expression of Twist1 is presented in Table II. In addition, Twist1 mRNA
expression was significantly higher in the breast cancer and
involved ALN compared with normal ALN (P<0.05; Fig. 4B). No statistical difference was
observed between the gene expression in the breast cancer tissues
and the metastatic ALN (P>0.05).
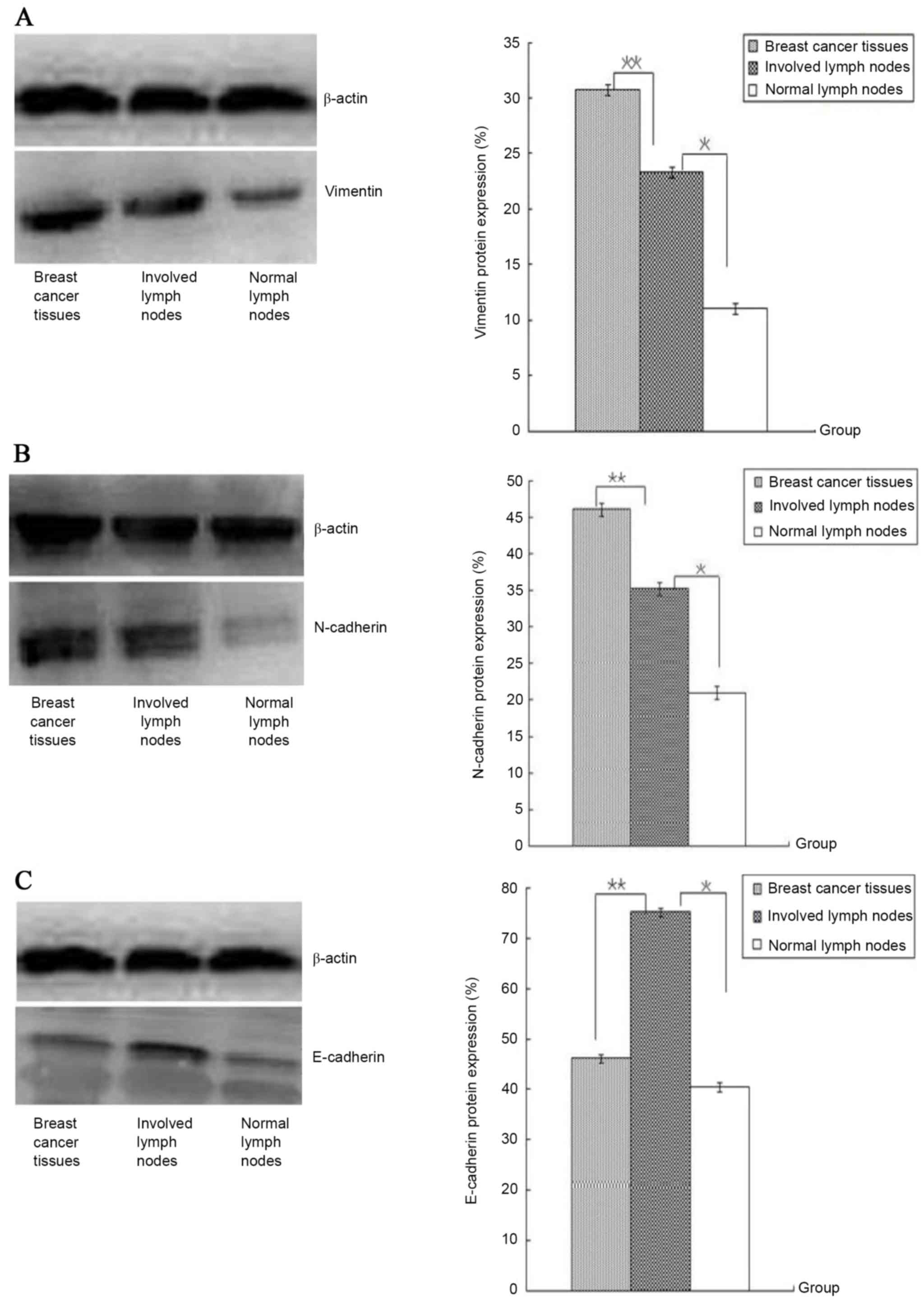
E-cadherin, instead of vimentin and
N-cadherin, was upregulated in metastatic ALN
Following western blotting analysis for primary
cancer tissues and the normal and metastatic ALN, the results
demonstrated that vimentin (Fig.
5A) expression in primary cancer tissues were significantly
higher in the normal and metastatic ALN, and the protein in
metastatic ALN was increased compared with normal ALN. N-cadherin
protein from primary cancer tissues was also highly expressed
compared with normal and metastatic ALN (Fig. 5B). Furthermore, the expression of
the two markers in primary cancer tissues appeared to be higher
compared with the metastatic ALN. This difference was statistically
significant (P<0.05). However, E-cadherin protein expression was
higher in metastasized ALN than in primary cancer tissues and in
normal ALN (P<0.05). The difference in E-cadherin expression
between the latter two tissues was not statistically significant
(P>0.05).
Although the four genes are all poorly expressed in
normal ALN, CD44, ALDH1 and Twist1 are also overexpressed in breast
cancer tissues and ALN with the exception of CD24. The expression
of the four genes in association with various clinicopathological
characteristics is presented in Table
II. Table III demonstrates
that there was no association between overexpression of these genes
(CD44, ALDH1 and Twist1) and tumor stage, nodes stage and family
history (P>0.05). A more significant association lay between the
overexpression of these genes and PR, ER, triple-receptor negative
and HER2/neu status. Patients whose receptors were positive were
more likely to have an overexpression of CD44, ALDH1 and Twist1
(P<0.05). The proportion of CD44, ALDH1, Twist1 and CA15-3
overexpression was also increased in the patients with
triple-receptor negative or pre-menopausal breast cancer.
 | Table III.Association between
clinicopathological characteristics and overexpression of CD44,
ALDH1, TWIST1 and CA15-3. |
Table III.
Association between
clinicopathological characteristics and overexpression of CD44,
ALDH1, TWIST1 and CA15-3.
|
| CD44
overexpression | ALDH1
overexpression | Twist1
overexpression | CA15-3
overexpression |
|---|
|
|
|
|
|
|
|---|
| Variable | Number of
cases | % | P-value | Number of
cases | % | P-value | Number of
cases | % | P-value | Number of
cases | % | P-value |
|---|
| Tumor stage |
|
|
|
|
|
|
|
|
|
|
|
|
|
T1–2 | 43/89 | 48.3 |
| 41/78 | 52.6 |
| 39/82 | 47.5 |
| 16/68 | 23.5 |
|
|
T3–4 | 46/89 | 51.7 | 0.327 | 37/78 | 47.4 | 0.342 | 42/82 | 52.5 | 0.168 | 52/68 | 76.5 | 0.031 |
| Node stage |
|
|
|
|
|
|
|
|
|
|
|
|
| N1 | 38/84 | 45.2 |
| 41/87 | 47.1 |
| 36/71 | 50.7 |
| 30/68 | 44.1 |
|
| N2-
N3 | 46/84 | 54.8 | 0.312 | 46/87 | 52.9 | 0.343 | 35/71 | 49.3 | 0.466 | 38/68 | 55.9 | 0.242 |
| PR status |
|
|
|
|
|
|
|
|
|
|
|
|
|
Negative | 35/79 | 44.3 |
| 24/76 | 31.5 |
| 32/84 | 38.1 |
| 27/68 | 39.7 |
|
|
Positive | 44/79 | 55.7 |
| 52/76 | 68.5 |
| 52/84 | 61.9 | 0.035 | 41/68 | 60.3 | 0.021 |
| ER status |
|
|
|
|
|
|
|
|
|
|
|
|
|
Negative | 21/79 | 26.5 |
| 30/81 | 37.0 |
| 32/86 | 37.2 |
| 21/68 | 30.9 |
|
|
Positive | 58/79 | 73.5 | 0.037 | 51/81 | 63.0 | 0.033 | 54/86 | 62.8 | 0.042 | 47/68 | 69.1 | 0.039 |
| HER2 status |
|
|
|
|
|
|
|
|
|
|
|
|
|
Negative | 63/79 | 79.7 |
| 58/81 | 71.6 |
| 64/86 | 74.4 |
| 48/68 | 70.6 |
|
|
Positive | 36/79 | 20.3 |
| 23/81 | 28.4 |
| 22/86 | 25.6 | 0.037 | 20/68 | 29.4 | 0.029 |
| Histological
type |
|
|
|
|
|
|
|
|
|
|
|
|
|
Ductal | 66/89 | 74.2 |
| 58/81 | 71.6 |
| 66/86 | 76.7 |
| 37/68 | 54.4 |
|
| Lobular
(others) | 23/89 | 25.8 | 0.040 | 23/81 | 28.4 | 0.029 | 20/86 | 23.3 | 0.037 | 31/68 | 45.6 | 0.144 |
| Family history |
|
|
|
|
|
|
|
|
|
|
|
|
|
Yes | 83/89 | 6.7 |
| 11/87 | 12.6 |
| 10/86 | 11.6 |
| 7/68 | 10.2 |
|
| No | 6/89 | 93.3 | 0.043 | 76/87 | 87.4 | 0.039 | 76/86 | 88.4 | 0.035 | 61/68 | 89.8 | 0.046 |
|
Triple-receptor negative | 32/89 | 35.9 |
| 19/87 | 21.8 |
| 31/86 | 36 |
| 20/68 | 29.4 |
|
|
Others | 57/89 | 64.1 | 0.041 | 68/87 | 78.2 | 0.045 | 55/86 | 64 | 0.042 | 48/68 | 70.6 | 0.059 |
| Menopausal
status |
|
|
|
|
|
|
|
|
|
|
|
|
|
Pre- | 69/89 | 77.5 |
| 52/87 | 59.8 |
| 58/86 | 67.4 |
| 49/68 | 72.1 |
|
|
Post- | 20/89 | 22.5 | 0.036 | 35/87 | 40.2 | 0.040 | 35/87 | 40.2 | 0.027 | 19/68 | 27.9 | 0.044 |
Serum CA15-3 levels can be used to
evaluate the clinical pathological stage of the tumor
The serum levels of the carbohydrate antigen CA15-3
in the patients' blood was tested on the fourth day prior to
surgery and the third day following surgery. The results
demonstrated that the serum CA15-3 levels of patients in stages I
and II (39.9±11.6) were significantly lower compared with stages
III and IV (78.4±18.1; P<0.05). However, no statistical
difference was observed between the pre-operative (65.8±21.6) and
the post-operative blood testing (67.9±17.3, P>0.05; Table IV).
 | Table IV.Serum levels of CA15-3 from the
enrolled patients with primary breast cancer in four groups. |
Table IV.
Serum levels of CA15-3 from the
enrolled patients with primary breast cancer in four groups.
|
| Serum CA15-3
(level>39 U/ml) |
|---|
|
|
|
|---|
| Variable | U (mean ± standard
deviation) | n | % |
|---|
| Pre-operation | 65.8±21.6 | 68/102 | 66.7 |
| Post-operation | 67.9±17.3 | 56/102 | 54.9 |
| Stage I–II | 39.9±11.6 | 21/102 | 20.5 |
| Stage III–IV | 78.4±18.1 | 47/102 | 79.5 |
Survival analysis
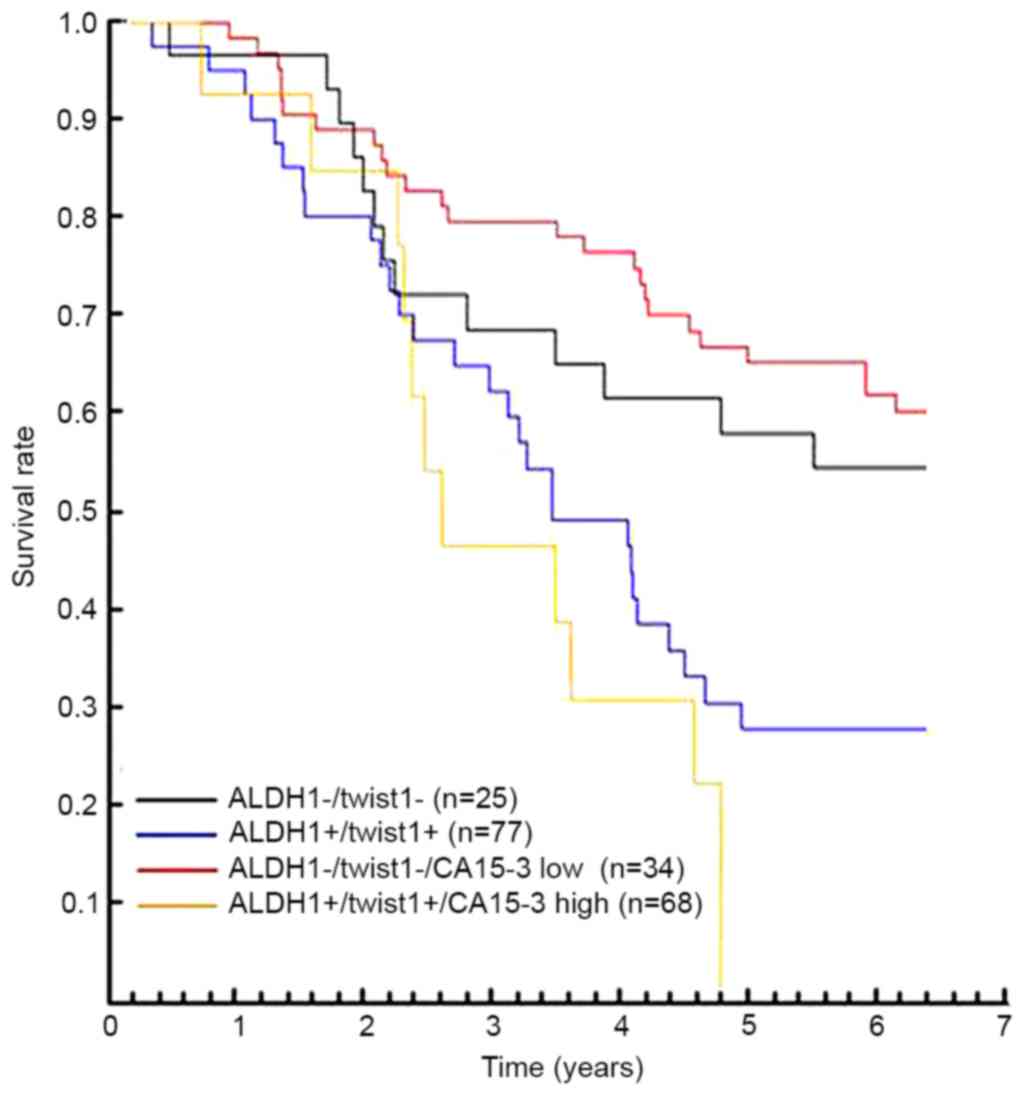
The median PFS for the patients was 4 years and 194
days, that for
CD44+CD24−/ALDH1−/Twist1−
was 5 years and 252 days and that for
CD44+CD24−/ALDH1+/Twist1+
was 4 years and 184 days.
CD44+CD24−/ALDH1+/Twist1+/CA153high
was 2 years and 263 days whereas
CD44+CD24−/ALDH1−/Twist1−
CA153low was 6 years and 169 days (P<0.05). No
significant difference in median survival was observed between
CD44+CD24− cancers and the other groups
(P<0.05). By analyzing the prognosis of the patients with
hormone receptor and HER2-negative tumors (n=52), statistically
significant differences were observed in hormone receptor tumors.
The median PFS of HER2-negative was shorter than HER2-positive
(P<0.05).
The univariate and binary logistic regression
analysis on 102 cases was used to assess the associations between
tumor markers and clinical characteristics. The combining status of
CD44+
CD24−/ALDH1+/Twist1+/CA15-3+
and triple-receptor negative were all significant factors strongly
associated with worse prognosis (P=0.018). Notably, only the
presence of membranous CD44+ CD24− or
CD44−
CD24−/ALDH1−/Twist1−
CA153low resulted in a favorable prognostic factor
(P=0.003 and P=0.021, respectively; Table V). Subsequent to an evaluation of
the prognostic relevance of the significant univariate parameters,
a multivariate logistic regression analysis also indicated that
poor prognosis correlated with the tumor markers demonstrated in
the Kaplan-Meier breast cancer survival curves, which illustrated
the decreasing survival associated with overexpression of genes
(Fig. 6).
 | Table V.Multivariate logistic regression
analysis for tumor markers predicting prognosis of 102 patients
with breast cancer. |
Table V.
Multivariate logistic regression
analysis for tumor markers predicting prognosis of 102 patients
with breast cancer.
| Variable | Hazard ratio 95%
CI | P-value |
|---|
|
CD44+CD24−/ALDH1−/TWIST1− | 2.923
7.010–9.246 | 0.022 |
|
CD44−CD24−/ALDH1+/TWIST1+ | 5.214
4.160–6.994 | 0.040 |
|
CD44+CD24−/TWIST1−/CA15-3− | 3.185
5.624–9.540 | 0.031 |
|
CD44+CD24−/TWIST1+/CA15-3+ | 7.153
6.122–9.532 | 0.038 |
|
HER2-negative/TWIST1−/CA15-3− | 1.831
4.152–9.334 | 0.033 |
|
HER2-positive/TWIST1+/CA15-3+ | 7.063
5.120–9.630 | 0.029 |
| Triple-receptor
negative/TWIST1−/CA15-3− | 4.028
6.187–9.925 | 0.048 |
| Triple-receptor
negative/TWIST1+/CA15-3+ | 8.064
4.112–8.530 | 0.021 |
Discussion
BCSCs expressing the
CD44+CD24−/low molecular phenotype
additionally possess numerous properties including self-renewal,
proliferation and the ability to promote the metastasis of tumor
cells (18). Hallmarks of these
tumors include a high enrichment for a
CD44+/CD24−/low tumor-initiating
cell signature, the downregulation of cell junction proteins
including cadherins and claudins, an enrichment of mesenchymal
markers, high lymphocyte infiltration and high phenotypic
resistance to chemotherapy (19,20).
ALDH1+ and CD44+/CD24− (BCSCs)
serve significant roles in metastasis (21). The results of the present study
confirmed that CD44 and ALDH1 were only poorly expressed in normal
breast tissues but highly expressed in tumor tissues and involved
ALN. However, CD24 expression was negative or low in the above
three tissues, consistent with previous studies. In addition, the
results indicated that CD44 and ALDH1 may serve a key role in
introducing tumorigenesis and then maintaining their expression
with no apparent changes. ALDH1 confers a tumorigenic character
when expressed at levels higher than the normal range. High
expression of ALDH1 has been associated with good overall survival
(P=0.021) (22), however, the
results of the present study demonstrated that high ALDH1
expression was involved in disease recurrence or poor survival
rates. The rate of ALDH1+ cells appears to be an
improved predictive marker of breast cancer metastasis than the
CD44+/CD24− phenotype (21). Twist1 overexpression in breast
cells can promote the generation of a BCSC phenotype characterized
by the high expression of CD44, little or no expression of CD24 and
increased ALDH1 activity, independent of the EMT (23,24).
The induction of EMT enables epithelial cells to acquire the
properties of mesenchymal lineages, including enhanced mobility and
invasiveness, which are closely correlated with cancer metastasis
(25,26). The well-defined features of EMT
include the loss of epithelial markers (E-cadherin and α- and
γ-catenin), the gain of mesenchymal cell markers (fibronectin,
vimentin and N-cadherin), and the acquisition of migratory and
invasive properties (27). The
results of the present study demonstrated that Twist1 mRNA was
significantly higher in breast cancer and involved ALN than in the
normal ALN. As EMT markers, N-cadherin and vimentin proteins of the
involved ALN were poorly expressed compared with breast cancer
tissues, but E-cadherin protein expression was higher in
metastasized and normal ALN compared with primary cancer tissues.
This may suggest that Twist1 overexpression is correlated with the
easy migration of tumors or a shorter PFS. The high expression of
Twist1 and SNAIL in LNM and the negative-to-positive conversion of
SNAIL confer worse prognosis, thus confirming the correlation of
EMT with aggressive disease behavior (11). The results of the present study
demonstrated that all Twist1-high samples, including the involved
ALN compared with the normal ALN, exhibited low ER and PR levels
and high HER2 levels, which may indicate that Twist1 and ER or PR
are inversely correlated in breast cancer patients. Chromatin
immunoprecipitation and promoter assays demonstrated that Twist
could directly bind to E-boxes in the ER promoter and significantly
downregulate ER promoter activity in vitro (28). The low expression of ER and high
expression of Twist1 in breast tumors correlated with increased
tumor recurrence and metastasis and poor progression-free survival.
CA15-3 has been considered a representative tumor marker for breast
cancer (7). The results of the
present study demonstrated that the serum levels of CA15-3 are not
statistically different in the pre-operative and post-operative
states. However, CA15-3 levels were significantly upregulated in
advanced cancer compared with early stage cancer, which suggested
that the change of CA15-3 levels was not associated with surgical
resection however with the stage of cancer. High serum levels of
tumor markers and high expression of Twist1 may suggest an
increased likelihood of relapse and a poor prognosis. The results
of the present study also demonstrated that
Twist1+/CA15-3+,
HER2-negative/Twist1+/CA15-3+ and
triple-receptor negative/Twist1+/CA15-3+
groups displayed a worse prognosis compared with the others,
suggesting that the assays can be widely used for monitoring
disease progression and response to therapy in some patients with
late stage breast cancer. CEA (6)
and BCA225 (29) are also
considered useful tumor markers, alone and in combination with
CA15-3, for detecting the recurrence of breast cancer. Although
they have some shortcomings, they are particularly valuable for
monitoring treatment in patients who have diseases that cannot be
evaluated by radiology (30).
In conclusion, the results of the present study
demonstrated that CD44, ALDH1 and Twist1 were significantly
overexpressed in primary cancer tissues and involved ALN while the
serum levels of CA15-3 of those patients were markedly increased
and survival rates fell, which suggests that patients, in
particular those with advanced cancer, may have a poor prognosis.
Note that the present study did not specifically engage in the
underlying mechanism of how the aforementioned genes are correlated
with poor prognosis or chemotherapy; that remains to be
elucidated.
Acknowledgements
The present study was supported by the Natural
Science Foundation of Chongqing, China (grant no. cstc2011jjA0058).
The authors would like to thank the staff of the Department of
Breast Gland Surgery and Department of Clinical Pathology, The
Second Affiliated Hospital of Chongqing Medical University for
their technical assistance, and the study participants for donating
the samples. The authors thank Professor Zhangxiong of Chongqing
Medical University (Chongqing, China) for critical technical
assistance.
References
|
1
|
Velasco-Velázquez MA, Homsi N, De La
Fuente M and Pestell RG: Breast cancer stem cells. Int J Biochem
Cell Biol. 44:573–577. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Vazquez-Martin A, Oliveras-Ferraros C,
Cufí S, Del Barco S, Martin-Castillo B and Menendez JA: Metformin
regulates breast cancer stem cell ontogeny by transcriptional
regulation of the epithelial-mesenchymal transition (EMT) status.
Cell Cycle. 9:3807–3814. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Ginestier C, Hur MH, Charafe-Jauffret E,
Monville F, Dutcher J, Brown M, Jacquemier J, Viens P, Kleer CG,
Liu S, et al: ALDH1 is a marker of normal and malignant human
mammary stem cells and a predictor of poor clinical outcome. Cell
Stem Cell. 1:555–567. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Li J and Zhou BP: Activation of β-catenin
and Akt pathways by Twist are critical for the maintenance of EMT
associated cancer stem cell-like characters. BMC Cancer. 11:492011.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Ru GQ, Wang HJ, Xu WJ and Zhao ZS:
Upregulation of twist in gastric carcinoma associated with tumor
invasion and poor prognosis. Pathol Oncol Res. 17:341–347. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Li S, Kendall SE, Raices R, Finlay J,
Covarrubias M, Liu Z, Lowe G, Lin YH, Teh YH, Leigh V, et al:
TWIST1 associates with NF-κB subunit RELA via carboxyl-terminal WR
domain to promote cell autonomous invasion through IL8 production.
BMC Biol. 10:732012. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Kong Y, Wang J, Liu W, Chen Q, Yang J, Wei
W, Wu M, Yang L, Xie X, Lv N, et al: Cytokeratin19-2g2, a novel
fragment of cytokeratin19 in serum, indicating a more invasive
behavior and worse prognosis in breast cancer patients. PLoS One.
8:e570922013. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Eckert MA, Lwin TM, Chang AT, Kim J, Danis
E, Ohno-Machado L and Yang J: Twist1-induced invadopodia formation
promotes tumor metastasis. Cancer Cell. 19:372–386. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Qin Q, Xu Y, He T, Qin C and Xu J: Normal
and disease-related biological functions of Twist1 and underlying
molecular mechanisms. Cell Res. 22:90–106. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Sleeman JP, Cady B and Pantel K: The
connectivity of lymphogenous and hematogenous tumor cell
dissemination: Biological insights and clinical implications. Clin
Exp Metastasis. 29:737–746. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Markiewicz A, Ahrends T,
Wełnicka-Jaśkiewicz M, Seroczyńska B, Skokowski J, Jaśkiewicz J,
Szade J, Biernat W and Zaczek AJ: Expression of epithelial to
mesenchymal transition-related markers in lymph node metastases as
a surrogate for primary tumor metastatic potential in breast
cancer. J Transl Med. 10:2262012. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Sell S: Cancer-associated carbohydrates
identified by monoclonal antibodies. Hum Pathol. 21:1003–1019.
1990. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Hilkens J, Buijs F, Hilgers J, Hageman P,
Calafat J, Sonnenberg A and van der Valk M: Monoclonal antibodies
against human milk-fat globule membranes detecting differentiation
antigens of the mammary gland and its tumors. Int J Cancer.
34:197–206. 1984. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Duffy MJ, Evoy D and McDermott EW: CA
15–3: Uses and limitation as a biomarker for breast cancer. Clin
Chim Acta. 411:1869–1874. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Zhou J, Zhang L, Gu Y, Li K, Nie Y, Fan D
and Feng Y: Dynamic expression of CEACAM7 in precursor lesions of
gastric carcinoma and its prognostic value in combination with CEA.
World J Surg Oncol. 9:1722011. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Sobin LH, Hermanek P and Hutter RV: TNM
classification of malignant tumors. A comparison between the new
(1987) and the old editions. Cancer. 61:2310–2314. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Elston CW and Ellis IO: Pathological
prognostic factors in breast cancer. I. The value of histological
grade in breast cancer: Experience from a large study with
long-term follow-up. Histopathology. 19:403–410. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Montgomery N, Hill A, McFarlane S, Neisen
J, O'Grady A, Conlon S, Jirstrom K, Kay EW and Waugh DJ: CD44
enhances invasion of basal-like breast cancer cells by upregulating
serine protease and collagen-degrading enzymatic expression and
activity. Breast Cancer Res. 14:R842012. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Prat A, Parker JS, Karginova O, Fan C,
Livasy C, Herschkowitz JI, He X and Perou CM: Phenotypic and
molecular characterization of the claudin-low intrinsic subtype of
breast cancer. Breast Cancer Res. 12:R682010. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Creighton CJ, Li X, Landis M, Dixon JM,
Neumeister VM, Sjolund A, Rimm DL, Wong H, Rodriguez A,
Herschkowitz JI, et al: Residual breast cancers after conventional
therapy display mesenchymal as well as tumor-initiating features.
Proc Natl Acad Sci USA. 106:13820–13825. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Zhong Y, Shen S, Zhou Y, Mao F, Guan J,
Lin Y, Xu Y and Sun Q: ALDH1 is a better clinical indicator for
relapse of invasive ductal breast cancer than the CD44+/CD24-
phenotype. Med Oncol. 31:8642014. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Sung WJ, Park KS, Kwak SG, Hyun DS, Jang
JS and Park KK: Epithelial-mesenchymal transition in patients of
pulmonary adenocarcinoma: Correlation with cancer stem cell markers
and prognosis. Int J Clin Exp Pathol. 8:8997–9009. 2015.PubMed/NCBI
|
|
23
|
Vesuna F, Lisok A, Kimble B and Raman V:
Twist modulates breast cancer stem cells by transcriptional.
Neoplasia. 11:1318–1328. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Li J and Zhou BP: Activation of β-catenin
and Akt pathways by Twist are critical for the maintenance of EMT
associated cancer stem cell-like characters. BMC Cancer. 11:492011.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Kalluri R: EMT: When epithelial cells
decide to become mesenchymal-like cells. J Clin Invest.
119:1417–1419. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Chaffer CL and Weinberg RA: A perspective
on cancer cell metastasis. Science. 331:1559–1564. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Huber MA, Kraut N and Beug H: Molecular
requirements for epithelial-mesenchymal transition during tumor
progression. Curr Opin Cell Biol. 17:548–558. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Vesuna F, Lisok A, Kimble B, Domek J, Kato
Y, Groep P vander, Artemov D, Kowalski J, Carraway H, van Diest P
and Raman V: Twist contributes to hormone resistance in breast
cancer by downregulating estrogen receptor-α. Oncogene.
31:3223–3234. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Ri G, Ohno S, Yamamoto T, Ito E, Furutani
M, Furutani Y, Umeda Y, Tsukahara T, Hagita N and Matsuoka R: Serum
levels of CA15-3, KL-6 and BCA225 are positively correlated with
each other in the general population. Anticancer Res. 29:4239–4242.
2009.PubMed/NCBI
|
|
30
|
Bidard FC, Hajage D, Bachelot T, Delaloge
S, Brain E, Campone M, Cottu P, Beuzeboc P, Rolland E, Mathiot C
and Pierga JY: Assessment of circulating tumor cells and serum
markers for progression-free survival prediction in metastatic
breast cancer: A prospective observational study. Breast Cancer
Res. 14:R292012. View Article : Google Scholar : PubMed/NCBI
|