|
1
|
Usluogullari CA, Balkan F, Caner S, Ucler
R, Kaya C, Ersoy R and Cakir B: The relationship between
microvascular complications and vitamin D deficiency in type 2
diabetes mellitus. BMC Endocr Disord. 15:332015. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Ghaderian SB, Hayati F, Shayanpour S and
Mousavi Beladi SS: Diabetes and end-stage renal disease; a review
article on new concepts. J Renal Inj Prev. 4:28–33. 2015.PubMed/NCBI
|
|
3
|
Palmer SC, Mavridis D, Navarese E, Craig
JC, Tonelli M, Salanti G, Wiebe N, Ruospo M, Wheeler DC and
Strippoli GF: Comparative efficacy and safety of blood
pressure-lowering agents in adults with diabetes and kidney
disease: A network meta-analysis. Lancet. 385:2047–2056. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Tanaka N, Babazono T, Takagi M, Yoshida N,
Toya K, Nyumura I, Hanai K and Uchigata Y: Albuminuria and reduced
glomerular filtration rate for predicting the renal outcomes in
type 2 diabetic patients. Nephrology (Carlton). 20:531–538. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Avogaro A and Fadini GP: The effects of
dipeptidyl peptidase-4 inhibition on microvascular diabetes
complications. Diabetes Care. 37:2884–2894. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Al-Mendalawi MD: Occurrence of
microalbuminuria among children and adolescents with
insulin-dependent diabetes mellitus. Saudi J Kidney Dis Transpl.
26:373–374. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Wang Y, Nie M, Lu Y, Wang R, Li J, Yang B,
Xia M, Zhang H and Li X: Fucoidan exerts protective effects against
diabetic nephropathy related to spontaneous diabetes through the
NF-κB signaling pathway in vivo and in vitro. Int J Mol Med.
35:1067–1073. 2015.PubMed/NCBI
|
|
8
|
Aggarwal J and Kumar M: Prevalence of
microalbuminuria among rural north indian population with diabetes
mellitus and its correlation with glycosylated haemoglobin and
smoking. J Clin Diagn Res. 8:CC11–CC13. 2014.PubMed/NCBI
|
|
9
|
Peng T, Hu Z, Wu L, Li D and Yang X:
Correlation between endothelial dysfunction and left ventricular
remodeling in patients with chronic kidney disease. Kidney Blood
Press Res. 39:420–426. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Yang X, Wang X, Nie F, Liu T, Yu X, Wang
H, Li Q, Peng R, Mao Z, Zhou Q and Li G: miR-135 family members
mediate podocyte injury through the activation of Wnt/β-catenin
signaling. Int J Mol Med. 36:669–677. 2015.PubMed/NCBI
|
|
11
|
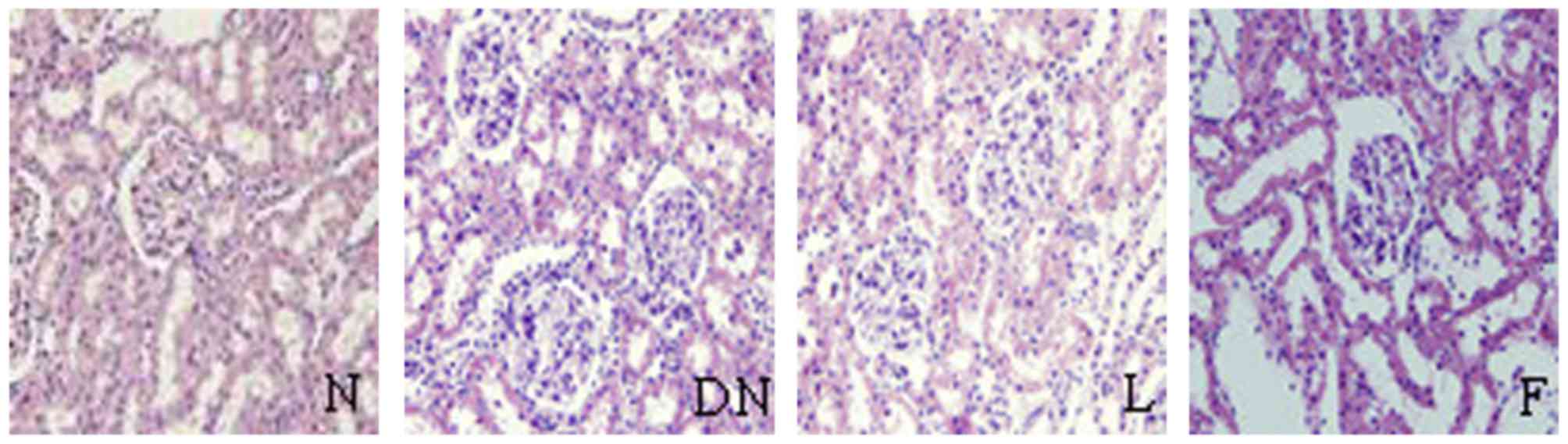
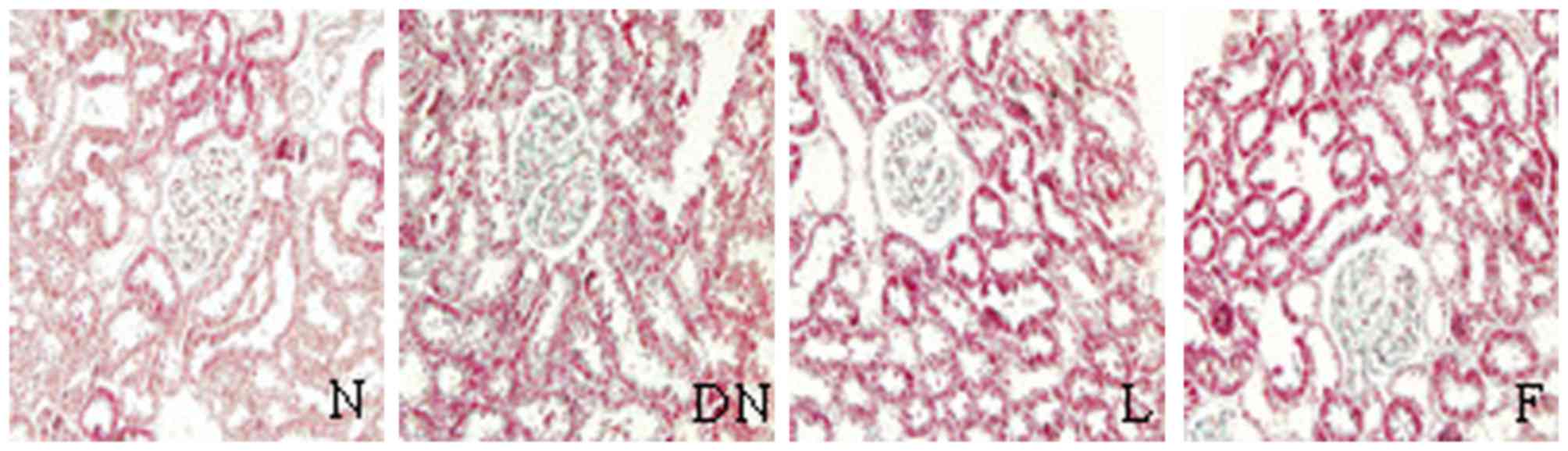
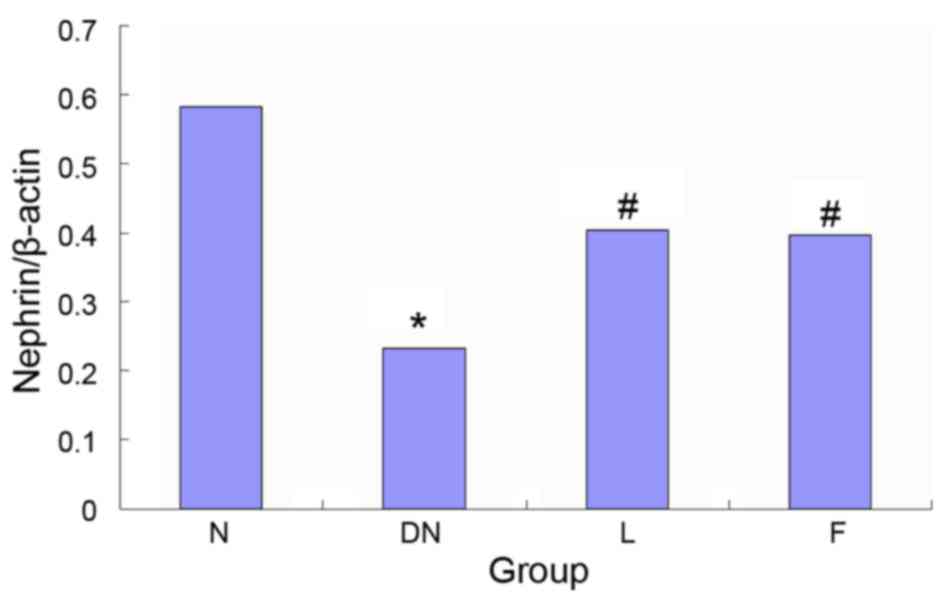
Wu Y, Dong J, Yuan L, Liang C, Ren K,
Zhang W, Fang F and Shen J: Nephrin and podocin loss is prevented
by mycophenolate mofetil in early experimental diabetic
nephropathy. Cytokine. 44:85–91. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Qi XM, Wu YG, Liang C, Zhang P, Dong J,
Ren KJ, Zhang W, Fang F and Shen JJ: FK506 ameliorates renal injury
in early experimental diabetic rats induced by streptozotocin. Int
Immunopharmacol. 11:1613–1619. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Álamo JM, Olivares C, Barrera L, Marín LM,
Suarez G, Bernal C, Serrano J, Muntané J, Padillo FJ and Gómez MA:
Conversion from calcineurin inhibitors to mTOR inhibitors
stabilizes diabetic and hypertensive nephropathy after liver
transplant. World J Transplant. 5:19–25. 2015.PubMed/NCBI
|
|
14
|
Brouwers O, Niessen PM, Miyata T,
Østergaard JA, Flyvbjerg A, Peutz-Kootstra CJ, Sieber J, Mundel PH,
Brownlee M, Janssen BJ, et al: Glyoxalase-1 overexpression reduces
endothelial dysfunction and attenuates early renal impairment in a
rat model of diabetes. Diabetologia. 57:224–225. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Liu XJ, Zhang YM, Wang SX and Liu G:
Ultrastructural changes of podocyte foot processes during the
remission phase of minimal change disease of human kidney.
Nephrology (Carlton). 19:392–397. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Bohman SO, Jaremko G, Bohlin AB and Berg
U: Foot process fusion and glomerular filtration rate in minimal
change nephrotic syndrome. Kidney Int. 25:696–700. 1984. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Wu HS and Dikman S: Segmentation and
thickness measurement of glomerular basement membranes from
electron microscopy images. J Electron Microsc (Tokyo). 59:409–418.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Maestroni S, Maestroni A, Dell'Antonio G,
Gabellini D, Terzi S, Spinello A, Meregalli G, Castoldi G and
Zerbini G: Viable podocyturia in healthy individuals: Implications
for podocytopathies. Am J Kidney Dis. 64:1003–1005. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Lin CL, Wang FS, Hsu YC, Chen CN, Tseng
MJ, Saleem MA, Chang PJ and Wang JY: Modulation of Notch-1
signaling alleviates VEGF-mediated diabetic nephropathy. Diabetes.
59:1915–1925. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Tryggvason K: Unraveling the mechanisms of
glomerular ultrafiltration: Nephrin, a key component of the slit
diaphragm. J Am Soc Nephrol. 10:2440–2445. 1999.PubMed/NCBI
|
|
21
|
Koop K, Eikmans M, Baelde HJ, Kawachi H,
De Heer E, Paul LC and Bruijn JA: Expression of podocyte-associated
molecules in acquired human kidney diseases. J Am Soc Nephrol.
14:2063–2071. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Langham RG, Kelly DJ, Cox AJ, Gow RM,
Holthofer H and Gilbert RE: Angiotensin II-induced proteinuria and
expression of the podocyte slit pore membrane protein, nephrin.
Nephrol Dial Transplant. 19:262–263. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Toyoda M, Suzuki D, Umezono T, Uehara G,
Maruyama M, Honma M, Sakai T and Sakai H: Expression of human
nephrin mRNA in diabetic nephropathy. Nephrol Dial Transplant.
19:380–385. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Wallemacq PE and Reding R: FK506
(tacrolimus), a novel immunosuppressant in organ transplantation:
Clinical, biomedical, and analytical aspects. Clin Chem.
39:2219–2228. 1993.PubMed/NCBI
|
|
25
|
Liu LS, Li J, Chen XT, Zhang HX, Fu Q,
Wang HY, Xiong YY, Liu S, Liu XM, Li JL, et al: Comparison of
tacrolimus and cyclosporin A in CYP3A5 expressing Chinese de novo
kidney transplant recipients: A 2-year prospective study. Int J
Clin Pract Suppl. 43–52. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Bechstein WO, Paczek L, Wramner L,
Squifflet JP and Zygmunt AJ: European Rapamune Tacrolimus Study
Group: A comparative, randomized trial of concentration-controlled
sirolimus combined with reduced-dose tacrolimus or standard-dose
tacrolimus in renal allograft recipients. Transplant Proc.
45:2133–2140. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Yap DY, Ma MK, Mok MM, Kwan LP, Chan GC
and Chan TM: Long-term data on tacrolimus treatment in lupus
nephritis. Rheumatology (Oxford). 53:2232–2237. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Bloch J, Hazzan M, Van der Hauwaert C,
Buob D, Savary G, Hertig A, Gnemmi V, Frimat M, Perrais M, Copin
MC, et al: Donor ABCB1 genetic polymorphisms influence
epithelial-to-mesenchyme transition in tacrolimus-treated kidney
recipients. Pharmacogenomics. 15:2011–2024. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Jiang S, Tang Q, Rong R, Tang L, Xu M, Lu
J, Jia Y, Ooi Y, Hou J, Guo J, et al: Mycophenolate mofetil
inhibits macrophage infiltration and kidney fibrosis in long-term
ischemia-reperfusion injury. Eur J Pharmacol. 688:56–61. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Gooch JL, Barnes JL, Garcia S and Abboud
HE: Calcineurin is activated in diabetes and is required for
glomerul hypertrophy and ECM accumulation. Am J Physiol Renal
Physiol. 284:F144–F154. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Qi XM, Wu YG, Liang C, Zhang P, Dong J,
Ren KJ, Zhang W, Fang F and Shen JJ: FK506 ameliorates renal injury
in early experimental diabetic rats induced by streptozotocin. Int
Immunopharmacol. 11:1613–1691. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Peng T, Hu Z, Xia Q, Jiang B, Li X and
Yang X: A comparative study of the renoprotective effects of
benidipine and valsartan in primary hypertensive patients with
proteinuria. Arzneimittelforschung. 59:647–650. 2009.PubMed/NCBI
|
|
33
|
Jin H, Piao SG, Jin JZ, Jin YS, Cui ZH,
Jin HF, Zheng HL, Li JJ, Jiang YJ, Yang CW and Li C: Synergistic
effects of leflunomide and benazepril in streptozotocin-induced
diabetic nephropathy. Nephron Exp Nephrol. 126:148–156. 2014.
View Article : Google Scholar : PubMed/NCBI
|