Introduction
Diabetes is one of the most common metabolic
disorders affecting individuals worldwide, and its incidence is
increasing each year. Currently, approximately 347 million people
are suffering from diabetes mellitus (DM) worldwide and the number
will continue to increase (1). The
prevalence of diabetes in China has risen significantly in past
decades. A large body of research has demonstrated that diabetes is
one of the major risk factors for dementia (2,3).
Diabetes is associated with alterations in the central nervous
system, including cognitive impairment and cerebrovascular disease
(4–6). Type 1 diabetes mellitus (T1DM) and
type 2 DM (T2DM) have been associated with reduced performance in
multiple domains of cognitive function. Previous studies have
demonstrated a stronger association between dementia and T2DM
compared with T1DM. Specifically, T2DM is associated with a 50%
increase in the risk for dementia, and has been associated with
impaired attention, processing and motor speed, executive
functioning, and verbal memory. Among the components of metabolic
syndrome, hyperglycemia demonstrates the strongest association with
the risk of developing cognitive impairment. Hyperglycemia leads to
oxidative stress and an inflammatory response, which are the risk
factors for Alzheimer's disease in DM. The increased level of
oxidative stress under diabetic conditions leads to morphological
and functional alterations in different regions of the brain,
including the hippocampus and the cerebral cortex (1). In addition, excessive malondialdehyde
(MDA) production and decreased efficiency of superoxide dismutase
(SOD) in various brain regions have been reported to lead to
morphological abnormalities and memory deficits during aging
(7). Inflammation is an additional
key factor in diabetes-associated cognitive decline. The increased
incidence of diabetes is associated with serious socioeconomic
problems (1). However, the precise
mechanisms underlying diabetes-associated cognitive deficits remain
to be elucidated. Therefore, an improved understanding of the
mechanisms underlying diabetes-associated cognitive impairment, and
the identification of effective treatments for patients with DM is
urgently required.
Butylphthalide, a promising drug for the treatment
of ischemic stroke, has been approved for clinical use by the State
Food and Drug Administration of China (8,9).
Preclinical and clinical studies have demonstrated that
butylphthalide is an effective neuroprotective agent for the
treatment of ischemic stroke (10). In addition, previous studies have
investigated the association between butylphthalide and cognition
(11,12), as well as the use of butylphthalide
in the treatment of diabetic rats (13,14).
However, the precise mechanisms remain to be elucidated. In the
present study, a streptozotocin (STZ)-induced rat model of diabetes
was employed to study the possible protective effects of
butylphthalide in diabetes-associated cognitive decline.
Materials and methods
Generation of a diabetic rat model and
butylphthalide administration
A total of 30 healthy male Sprague Dawley rats (age,
6 weeks; weight, 180–200 g) were obtained from the Animal Center of
Tianjin Huanhu Hospital (Tianjin, China). All experiments were
performed in compliance with the regulations approved by the Ethics
Committee of Tianjin Huanhu Hospital, and the current study
received ethical approval from this committee. Rats were housed in
a room at 21–25°C with 12-h light/dark cycles, one rat per cage,
and had access to food and water ad libitum. A total of 20
rats received 10% STZ (60 mg/kg dissolved in citrate buffer, pH
4.5; cat. no. ab142155; Abcam, Cambridge, MA, USA) by
intraperitoneal injection. At 72 h following injection, blood was
collected from caudal vein, and blood glucose levels were measured.
Diabetic models were considered successful if blood glucose levels
were >16.7 mmol/l. Blood glucose levels were measured weekly,
and rats with values <16.7 mmol/l were excluded from the study.
Diabetic rats were divided into the following 2 groups at random:
Diabetic model (DM) control (n=10) and butylphthalide-treated
groups (n=10). A total of 10 rats without STZ injection were used
as normal controls. Butylphthalide (CSPC NBP Pharmaceutical Co.,
Ltd., Shijiazhuang, China) was dissolved in vegetable oil. Rats in
the butylphthalide-treated group were administered with 80
mg/kg/day butylphthalide orally for 8 consecutive weeks. The
control and DM groups received the same volume of vegetable oil
orally.
Fasting plasma glucose (FPG)
measurements
FPG was measured in all rats once a week at 24 h
following drug treatment. Tail vein blood was collected for FPG
measurements with a blood glucose meter (Accu-Chek; Roche Applied
Science, Penzberg, Germany), reading the blood glucose measurement
results after 5 sec.
Food and water intake
measurements
The body weight and water intake of rats were
measured once every two weeks for 8 weeks (56 days) immediately
after the STZ injection.
Morris water maze (MWM) test
The MWM test (diameter, 50 cm; height, 50 cm; water
depth, 40 cm; temperature, 22±1°C) (14) included a hidden platform (diameter,
10 cm) submerged 1 cm below the surface of the water. On day 1
following the last treatment, all rats were subjected to the MWM
test to assess learning and memory abilities. Tests were performed
at a fixed time every day for 5 continuous days. A camera located
above the center of the maze, together with a tracking system were
used to record images and the time taken to locate the platform
(the escape latency). If a rat failed to reach the platform within
60 sec, it was guided onto the platform (where it remained for 20
sec), and the latency was recorded as 60 sec. A probe trial was
performed at day 6 following the final treatment. In this trial,
the platform was removed, and rats were allowed to search for the
missing platform for 60 sec. The frequency of platform crossings
was then recorded.
SOD and MDA measurements
The rats in all groups were sacrificed by
decapitation at 6 days following the final drug treatment.
Hippocampal tissue samples were prepared for SOD and MDA tests.
Hippocampal SOD and MDA activity were detected using the Superoxide
Dismutase Activity Colorimetric assay kit (ab65354; Abcam). SOD and
MDA levels were measured according to the manufacturer's protocol.
Absorbance of MDA and SOD was measured using spectrophotometer and
microplate reader.
Western blotting analysis of
brain-derived neurotrophic factor (BDNF) expression
Hippocampal tissue sections were homogenized with a
glass homogenizer in radioimmunoprecipitation assay lysis buffer.
The homogenate was centrifuged (4°C, 13,000 × g, 10 min) and the
supernatants were collected and stored at −80°C. The protein
concentration was determined using a Bradford protein assay kit
(cat. no. ab102535; Abcam). An equal quantity (100 µl) of protein
from each sample was separated by 12% SDS-PAGE, and transferred
onto a polyvinylidene difluoride membrane by electroblotting.
Membranes were blocked for 1 h at 37°C with 5% non-fat milk, and
then incubated overnight at 4°C with a rabbit anti-BDNF antibody
(1:1,000; Abcam; ab108319) and a rabbit anti-β-actin (1:2,000;
Abcam; ab8227). After several washes in TBST, the membranes were
incubated with the appropriate horseradish peroxidase
(HRP)-conjugated secondary antibodies (anti-Rabbit IgG H&L; cat
no. ab6271; 1:10,000; Abcam) for 45 min at 37°C. LuminataTM
Crescendo Western HRP substrate (EMD Millipore, Billerica, MA, USA)
was used to visualize the protein bands. Protein bands were
detected using the ChemiDoc XRS system (Bio-Rad Laboratories, Inc.,
Hercules, CA, USA) and Quantity One version 4.62 software (Bio-Rad
Laboratories, Inc.).
Enzyme-linked immunosorbent assay
(ELISA) analysis of hippocampal cytokine levels
Rat hippocampal tissues were washed and then
homogenized on ice with normal saline. Homogenates were centrifuged
at 3,000 × g for 10 min at 4°C, and the supernatants (100 ml) were
used for subsequent analysis. The levels of interleukin (IL)-1β,
IL-6, tumor necrosis factor-α (TNF-α) were measured using the Rat
TNF-α ELISA kit (cat. no. ab46070, Abcam), the Rat IL-1β ELISA kit
(cat. no. ab100768, Abcam) and the Rat IL-6 ELISA kit (cat. no.
ab100772; Abcam), respectively, according to manufacturer's
protocol. TNF-α, IL-1β and IL-6 levels were measured according to
the manufacturer's protocol. Absorbance was measured using a
microplate reader at a wavelength of 210 nm.
Statistical analysis
The results are presented as the mean ± standard
deviation. All statistical analyses were performed using SPSS
(version, 13.0; SPSS, Inc., Chicago, IL, USA). Data were analyzed
using repeated measures analysis of variance (ANOVA) followed by
least significant difference post hoc analysis. P<0.05 was
considered to indicate a statistically significant difference.
Results
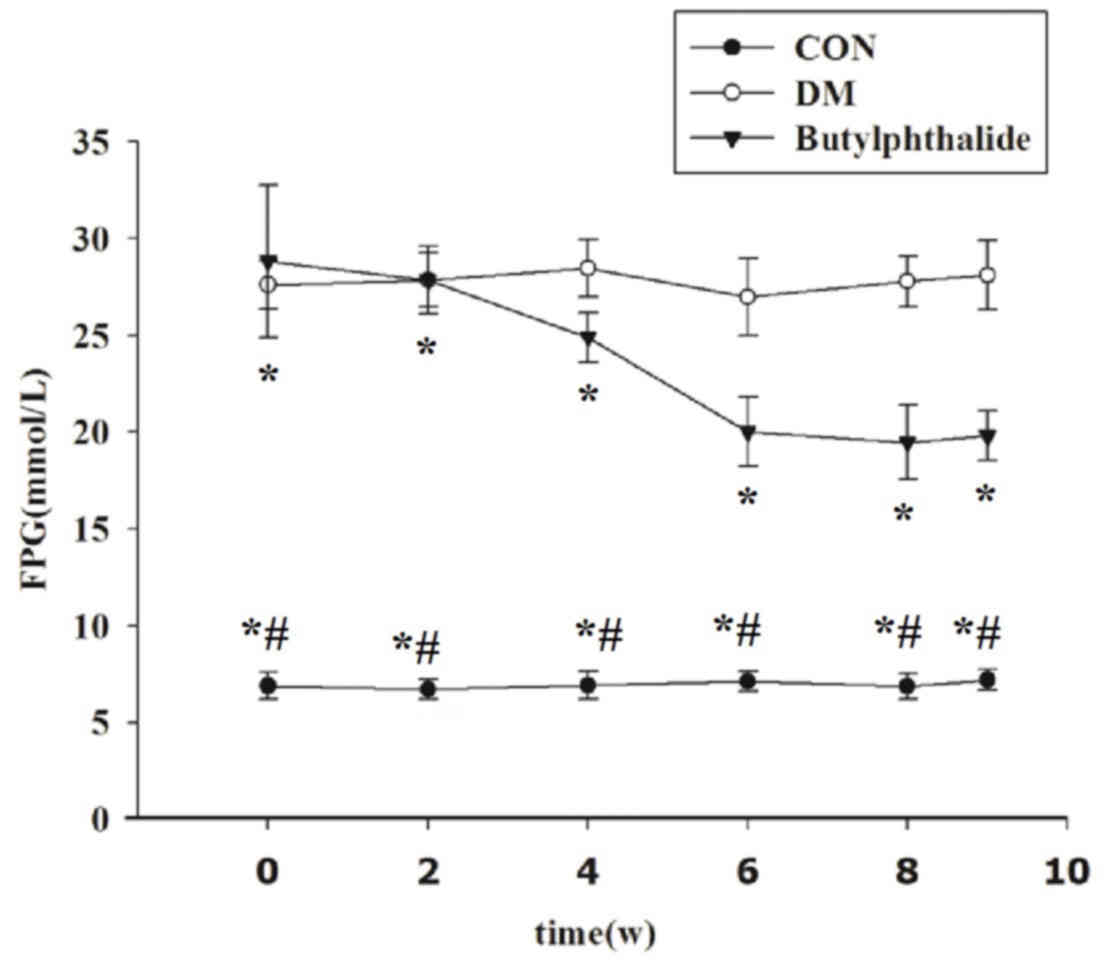
Butylphthalide decreases FPG levels in
diabetic rats
Blood glucose was tested dynamically over the course
of 8 weeks. The FPG levels of the DM and butylphthalide-treated
diabetic groups were significantly higher than the NC group at all
time points (P<0.001; Fig. 1).
However, following administration of butylphthalide for 8 weeks,
FPG levels were significantly decreased when compared with the DM
group (P<0.001; Fig. 1).
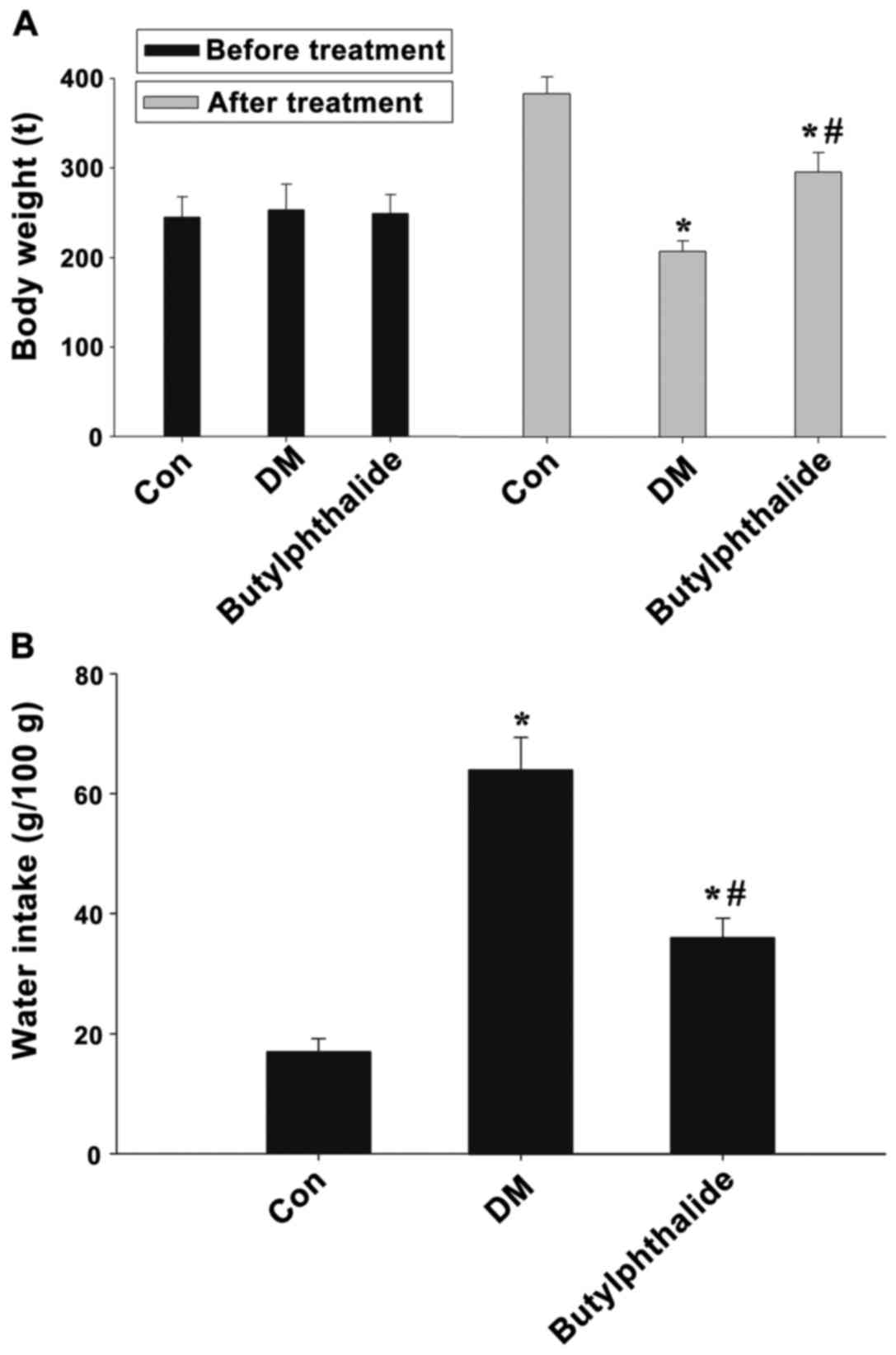
Butylphthalide influences body weight
and water intake in STZ-induced diabetic rats
A significant reduction in the body weight of
STZ-treated rats in the DM group was observed when compared with
untreated control rats (P<0.01; Fig. 2A). By contrast, butylphthalide
administration significantly reversed the body weight of diabetic
rats (P<0.05; Fig. 2A). The
water intake of rats over a 24-h period, which was measured at week
6 following the final drug treatment and when blood glucose levels
and body weight had reached a steady state, was increased ~3-fold
in the diabetic rats when compared with the control group, and
~2-fold compared with the control group (Fig. 2B).
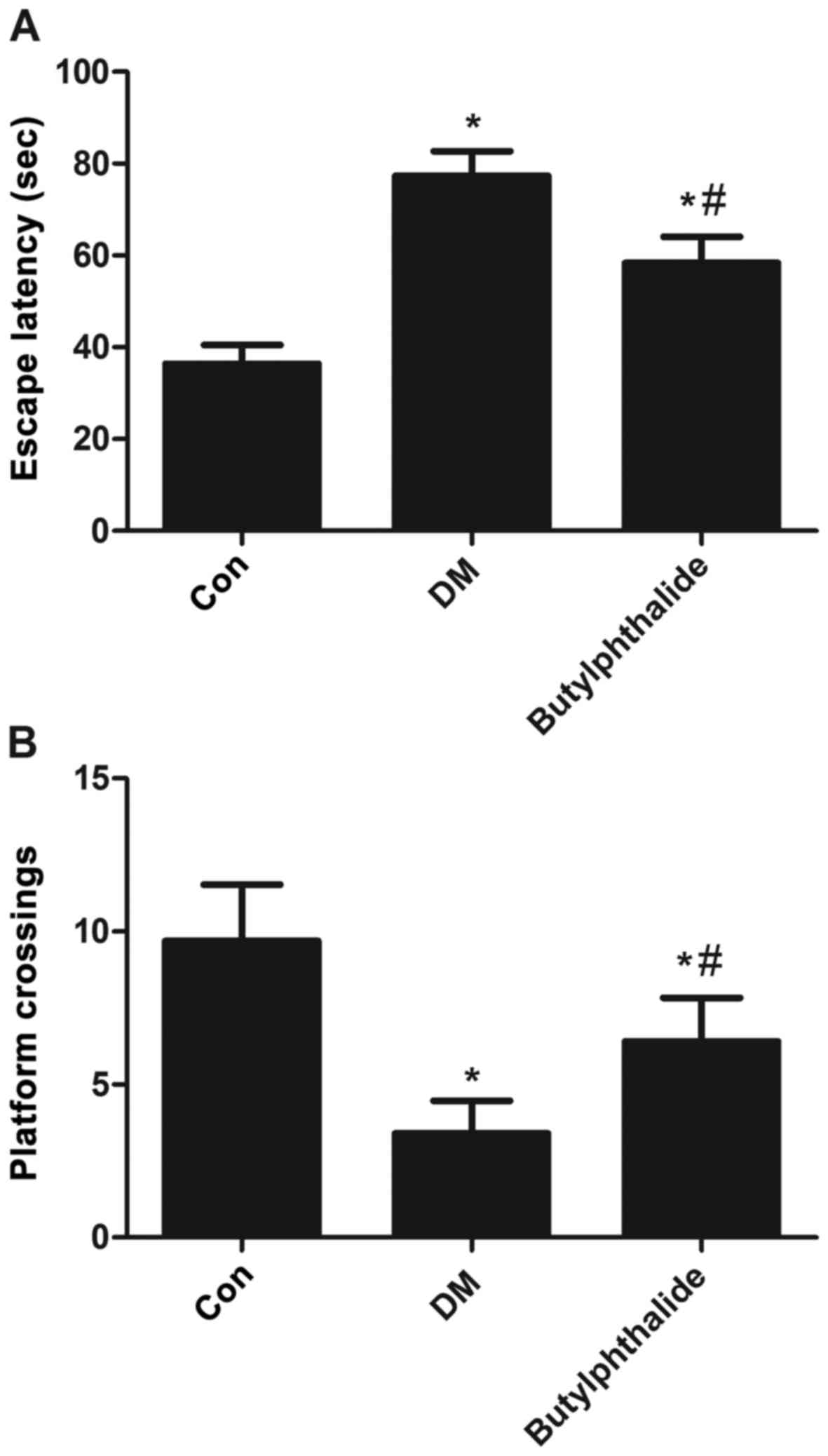
Effects of butylphthalide on cognitive
deficits in STZ-induced diabetic rats
The results presented in Fig. 3 demonstrate that butylphthalide
significantly ameliorated the cognitive deficits observed in
diabetic rats from the DM group. Compared with control group, the
escape latency of rats in the DM group was significantly increased
(P<0.001). However, treatment with butylphthalide significantly
decreased the escape latency when compared with the DM group
(P<0.001; Fig. 3A). In the
probe test, the number of platform crossings was significantly
decreased in DM group compared with the control group (P<0.001;
Fig. 3B). By contrast, treatment
with butylphthalide significantly increased the number of platform
crossings when compared with the DM group (P<0.001; Fig. 3B).
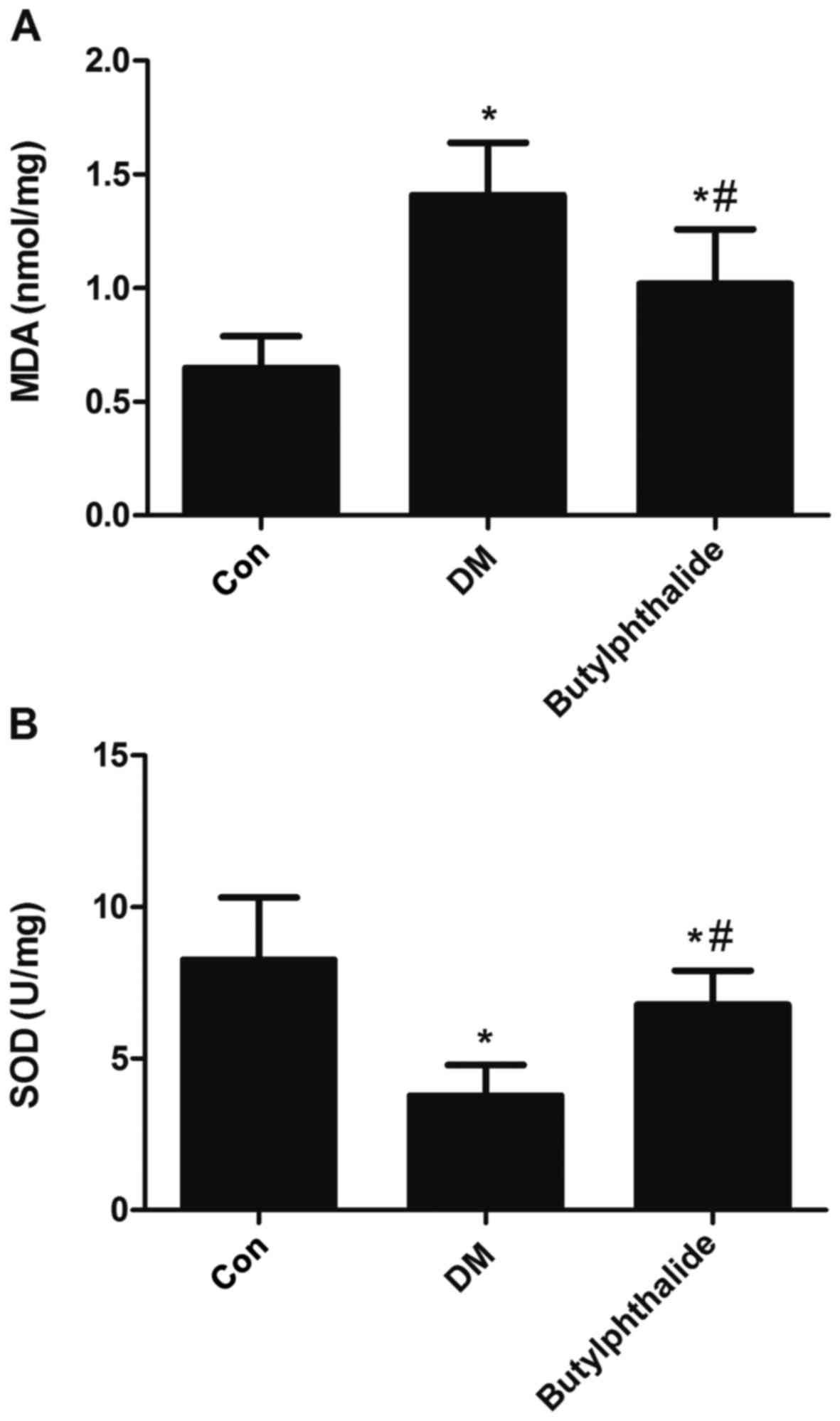
Effect of butylphthalide on
diabetes-induced alterations in oxidative stress
The production of MDA was significantly increased in
rats from the DM group when compared with the controls (P<0.05,
Fig. 4A). By contrast,
administration of butylphthalide significantly decreased
hippocampal MDA levels when compared with the DM group (P<0.05,
Fig. 4A). In addition, SOD levels
were significantly reduced in rat hippocampal tissues from the DM
group compared with the control group (P<0.05, Fig. 4B). However, treatment with
butylphthalide significantly reversed SOD levels in DM rats
(P<0.05, Fig. 4B).
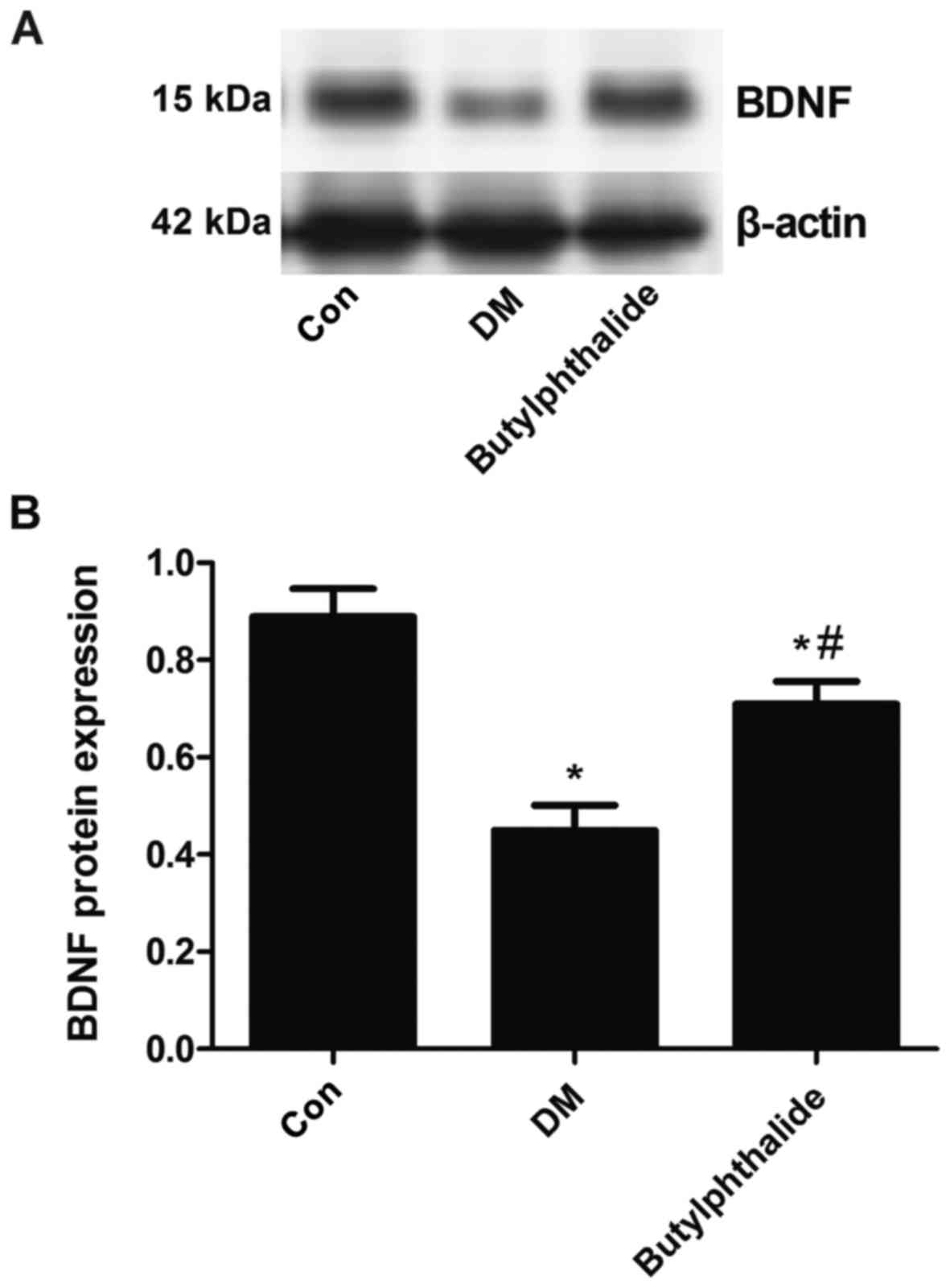
Effects of butylphthalide on the
protein expression levels of BDNF in the hippocampus of STZ-induced
diabetic rats
Following establishment of the STZ-induced rat model
of diabetes, a significant decrease in the protein expression
levels of BDNF were observed when compared with normal controls
(P<0.05, Fig. 5). However,
following the administration of butylphthalide for 8 weeks, the
protein expression of BDNF in the rat hippocampus was significantly
increased when compared to the DM group (P<0.05, Fig. 5).
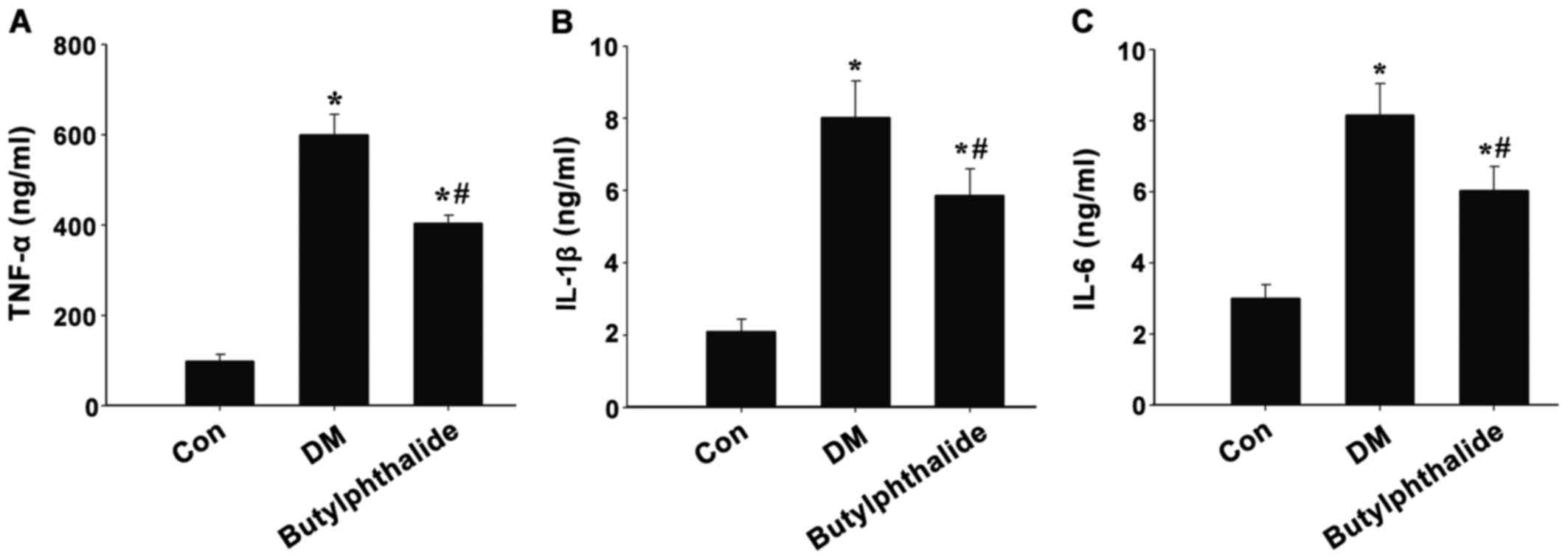
Effects of butylphthalide on the level
of inflammatory cytokines in the hippocampus of STZ-induced
diabetic rats
The effects of butylphthalide on the
diabetes-associated increase in inflammation were investigated in
the present study. As demonstrated in Fig. 6, the expression of inflammatory
factors, TNF-α, IL-1β and IL-6, were significantly increased in the
hippocampus of rats in the DM group when compared with normal
controls (P<0.01). By contrast, butylphthalide treatment
significantly reduced the level of these inflammatory factors in
the hippocampus of diabetic rats (Fig.
6).
Discussion
DM is characterized by dysfunctional insulin
secretion and/or insulin function, which leads to the development
of metabolic glucose disorders with secondary complications that
affect the kidneys, heart, eyes and brain. It has been reported
that DM is associated with subtle cognitive decline and an
increased risk for reduced cognitive flexibility in the form of
dementia. The mechanisms of diabetes-associated cognitive decline
include impaired neurogenesis, synaptic dysfunction and reduced
blood-brain barrier function (15–18),
hyperglycemia and hypoglycemia (19,20),
inflammatory and oxidative stress (15), microvascular and macrovascular
dysfunction (21,22), and alterations in the insulin
signaling pathway (23).
The association between obesity and T2DM has been
previously described in an in vivo study, where it was
demonstrated that adipose-derived TNF-α levels in rats were
elevated with increasing body weight (24). During obesity and metabolic
dysfunction, immune cells in adipose tissues secrete
proinflammatory cytokines that affect glucose and lipid metabolism
(25). The excessive migration of
macrophages to adipose tissues and their subsequent activation is a
key factor for TNF-α and IL-6 production and release, which
decreases the activity of the lipoprotein lipase enzyme and
increases blood lipid levels.
Oxidative stress has been demonstrated to be
involved in the generation of STZ-induced diabetic rats, and has
been associated with characteristics of memory decline (26). Due to individual differences, the
uptake of STZ is different among rats, therefore the rate of
successful generation of a diabetic rat model by oral
administration of STZ may be lower when compared with
intraperitoneal injection. These methods of model generation will
differ in the extent of hyperglycemia and inflammation induced, as
well as in the effects of different treatments (27). It is well known that oxidative
stress leads to the oxidative damage of biomacromolecules. An
increase in MDA is considered to be a specific marker of lipid
peroxidation during oxidative damage (28). In addition, oxidative injury may
lead to damage of the antioxidant defense system, involving factors
such as SOD. Notably, it was previously reported that oxidative
stress-induced brain injury contributed to the severe impairment of
learning and memory abilities in STZ-induced rats (29). The results of the present study
demonstrated that oxidative injury, as evidenced by increased MDA
content and decreased SOD activity, and cognitive impairment was
observed in a rat model of diabetes. However, these
diabetes-associated effects were significantly reversed by
butylphthalide treatment.
Butylphthalide is a promising agent for the
treatment of ischemic stroke (30). Its mechanisms of action include,
decreasing oxidative damage (31),
inhibiting platelet aggregation and inflammatory responses
(8,32,33),
improving mitochondrial function (34) and reducing neuronal apoptosis
(35,36). Taking the results of these previous
studies into account, there is a strong possibility that
butylphthalide may restore cognitive deficits in diabetic rats.
In the present study, diabetic rats underwent
continuous butylphthalide treatment for 8 weeks. The escape latency
of butylphthalide-treated rats was significantly reduced when
compared with untreated diabetic rats, which indicated that
STZ-induced cognitive deficits were ameliorated by butylphthalide
treatment. In addition, serum FPG levels were significantly
decreased in butylphthalide-treated rats, which suggests that
butylphthalide may alter glucose metabolism. Hippocampal SOD and
BDNF levels were then assessed. SOD is used as a marker of
oxidative stress during diabetes (37,38).
The results of the present study demonstrated that butylphthalide
significantly reversed the diabetes-associated decrease in SOD
levels, which suggests that butylphthalide may exhibit
antioxidative effects.
BDNF is a type of neurotrophin that serves an
important role in regulating the growth and survival of neurons
(39). BDNF enhances neuronal
plasticity in the hippocampus and improves learning and memory
abilities (40). The results of
the present study indicated that BDNF protein expression was
decreased in STZ-induced diabetic rats, and the expression was
upregulated by butylphthalide treatment. These results, together
with the known role of BDNF in enhancing neuronal plasticity,
suggest that the protective effects of butylphthalide in diabetic
rats may involve increased neurogenesis and neuronal
plasticity.
Butylphthalide is used for the clinical treatment of
acute ischemic stroke, which effectively ameliorates injury of the
central nervous system and promotes functional recovery (7). The results of the present study
demonstrated that butylphthalide improved diabetes-associated
cognitive deficits in rats. It is possible that this may have been
due to the antioxidative effects, which is similar to the
pharmacological effects of butylphthalide in the treatment of acute
ischemic stroke. This was verified by the follow-up experiments, in
which butylphthalide is currently used to treat chronic
neurodegenerative diseases and those associated with diabetes,
butylphthalide may be used to treat chronic neurodegenerative
diseases including cognitive impairment in diabetes.
In conclusion, the results of the current study
demonstrated that butylphthalide treatment ameliorated the
cognitive deficits in STZ-induced diabetic rats. In addition, the
protective effects of butylphthalide may be associated with
upregulation of BDNF expression and SOD levels in the hippocampus.
A single dose of 80 mg/kg butylphthalide was selected for the
purposes of the present study, therefore the effects of different
doses need to be investigated in future studies. In addition,
clinical studies will be required to validate the neuroprotective
effects of butylphthalide on cognitive function in diabetes.
Glossary
Abbreviations
Abbreviations:
|
DM
|
diabetes mellitus
|
|
BDNF
|
brain-derived neurotrophic factor
|
|
STZ
|
streptozotocin
|
|
MWM
|
Morris water maze
|
|
FPG
|
fasting plasma glucose
|
|
SOD
|
superoxide dismutase
|
|
MDA
|
malondialdehyde
|
|
TNF-α
|
tumor necrosis factor-α
|
|
IL-1β
|
interleukin-1β
|
|
IL-6
|
interleukin-6
|
References
|
1
|
Seto SW, Yang GY, Kiat H, Bensoussan A,
Kwan YW and Chang D: Diabetes mellitus, cognitive impairment, and
traditional Chinese medicine. Int J Ednocrinol.
2015:8104392015.
|
|
2
|
Hölscher C: Diabetes as a risk factor for
Alzheimer's disease: Insulin signalling impairment in the brain as
an alternative model of Alzheimer's disease. Biochem Soc Trans.
39:891–897. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Katon W, Lyles CR, Parker MM, Karter AJ,
Huang ES and Whitmer RA: Association of depression with increased
risk of dementia in patients with type 2 diabetes: The diabetes and
aging study. Arch Gen Psychiatry. 69:410–417. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Strachan MW, Reynolds RM, Frier BM,
Mitchell RJ and Price JF: The relationship between type 2 diabetes
and dementia. Br Med Bull. 88:131–146. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Messier C, Awad N and Gagnon M: The
relationships between atherosclerosis, heart disease, type 2
diabetes and dementia. Neurol Res. 26:567–572. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Scott AR: Diabetes and Cerebrovascular
DiseaseVascular Complications of Diabetes: Current Issues in
Pathogenesis and Treatment. Second Edition. Donnelly R and Horton
E: Blackwell Publishing. Inc; Malden, MA: pp. 45–50. 2007
|
|
7
|
Lan Z, Xu X, Xu W, Li J, Liang Z, Zhang X,
Lei M and Zhao C: Discovery of
3-n-butyl-2,3-dihydro-1H-isoindol-1-one as a potential
anti-ischemic stroke agent. Drug Des Devel Ther. 9:3377–3391.
2015.PubMed/NCBI
|
|
8
|
Peng Y, Xing C, Xu S, Lemere CA, Chen G,
Liu B, Wang L, Feng Y and Wang X: L-3-n-butylphthalide improves
cognitive impairment induced by intracerebroventricular infusion of
amyloid-beta peptide in rats. Eur J Pharmacol. 621:38–45. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Huai Y, Dong Y, Xu J, Meng N, Song C, Li W
and Lv P: L-3-n-butylphthalide protects against vascular dementia
via activation of the Akt kinase pathway. Neural Regen Res.
8:1733–1742. 2013.PubMed/NCBI
|
|
10
|
Xiao S, Kai H, Yang C, Wang X, Ji H, Xu J,
Huang Z and Zhang Y: Novel hybrids of 3-n-butylphthalide and
edaravone: Design, synthesis and evaluations as potential
anti-ischemic stroke agents. Bioorg Med Chem Lett. 25:3535–3540.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Peng Y, Xu S, Chen G, Wang L, Feng Y and
Wang X: l-3-n-Butylphthalide improves cognitive impairment induced
by chronic cerebral hypoperfusion in rats. J Pharmacol Exp Ther.
321:902–910. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Wang F, Chen H, Sun XJ and Ke ZJ:
Improvement of cognitive deficits in SAMP8 mice by
3-n-butylphthalide. Neurol Res. 36:224–233. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Wang F, Ma J, Han F, Guo X, Meng L, Sun Y,
Jin C, Duan H, Li H and Peng Y: DL-3-n-butylphthalide delays the
onset and progression of diabetic cataract by inhibiting oxidative
stress in rat diabetic model. Sci Rep. 6:193962016. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Zhang T, Jia W and Sun X:
3-n-Butylphthalide (NBP) reduces apoptosis and enhances vascular
endothelial growth factor (VEGF) up-regulation in diabetic rats.
Neurol Res. 32:390–396. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Barcia JM, Floresbellver M, Muriach M,
Sancho-Pelluz J, Lopez-Malo D, Urdaneta AC, Martinez-Gil N,
Atienzar-Aroca S and Romero FJ: Matching diabetes and alcoholism:
Oxidative stress, inflammation, and neurogenesis are commonly
involved. Mediators Inflamm. 2015:6242872015. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Wang J, Gong B, Zhao W, Tang C, Varghese
M, Nguyen T, Bi W, Bilski A, Begum S, Vempati P, et al: Epigenetic
mechanisms linking diabetes and synaptic impairments. Diabetes.
63:645–654. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Huang S, Wang Y, Gan X, Fang D, Zhong C,
Wu L, Hu G, Sosunov AA, McKhann GM, Yu H and Yan SS: Drp1-mediated
mitochondrial abnormalities link to synaptic injury in diabetes
model. Diabetes. 64:1728–1742. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Huber JD: Diabetes, cognitive function,
and the blood-brain barrier. Curr Pharm Des. 14:1594–1600. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
González-Reyes RE, Aliev G,
Ávila-Rodrigues M and Barreto GE: Alterations in glucose metabolism
on cognition: A possible link between diabetes and dementia. Curr
Pharm Des. 22:812–818. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Perantie DC, Lim A, Wu J, Weaver P, Warren
SL, Sadler M, White NH and Hershey T: Effects of prior hypoglycemia
and hyperglycemia on cognition in children with type 1 diabetes
mellitus. Pediatr Diabetes. 9:87–95. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Krentz AJ, Clough G and Byrne CD:
Interactions between microvascular and macrovascular disease in
diabetes: Pathophysiology and therapeutic implications. Diabetes
Obes Metab. 9:781–791. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Caballero AE, Arora S, Saouaf R, Lim SC,
Smakowski P, Park JY, King GL, LoGerfo FW, Horton ES and Veves A:
Microvascular and macrovascular reactivity is reduced in subjects
at risk for type 2 diabetes. Diabetes. 48:1856–1862. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Sebastião I, Candeias E, Santos MS, de
Oliveira CR, Moreira PI and Duarte AI: Insulin as a bridge between
type 2 diabetes and Alzheimer disease-how anti-diabetics could be a
solution for dementia. Front Endocrinol (Lausanne).
5:1102014.PubMed/NCBI
|
|
24
|
Hotamisligil GS, Shargill NS and
Spiegelman BM: Adipose expression of tumor necrosis factor-alpha:
Direct role in obesity-linked insulin resistance. Science.
259:87–91. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Tateya S, Kim F and Tamori Y: Recent
advances in obesity-induced inflammation and insulin resistance.
Front Endocrinol (Lausanne). 4:932013.PubMed/NCBI
|
|
26
|
Wu W, Wang X, Xiang Q, Meng X, Peng Y, Du
N, Liu Z, Sun Q, Wang C and Liu X: Astaxanthin alleviates brain
aging in rats by attenuating oxidative stress and increasing BDNF
levels. Food Funct. 5:158–166. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Singh R, Kaur N, Kishore L and Gupta GK:
Management of diabetic complications: A chemical constituents based
approach. J Ethnopharmacol. 150:51–70. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Zhong SZ, Ge QH, Qu R, Li Q and Ma SP:
Paeonol attenuates neurotoxicity and ameliorates cognitive
impairment induced by d-galactose in ICR mice. J Neurol Sci.
277:58–64. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Zhao CH, Liu HQ, Cao R, Ji AL, Zhang L,
Wang F and Yang RH: Effects of dietary fish oil on learning
function and apoptosis of hippocampal pyramidal neurons in
streptozotocin-diabetic rats. Brain Res. 1457:33–43. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Wang X, Wang L, Li T, Huang Z, Lai Y, Ji
H, Wan X, Xu J, Tian J and Zhang Y: Novel hybrids of optically
active ring-opened 3-n-butylphthalide derivative and isosorbide as
potential anti-ischemic stroke agents. J Med Chem. 56:3078–3089.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Huang JZ, Chen YZ, Su M, Zheng HF, Yang
YP, Chen J and Liu CF: dl-3-n-Butylphthalide prevents oxidative
damage and reduces mitochondrial dysfunction in an MPP(+)-induced
cellular model of Parkinson's disease. Neurosci Lett. 475:89–94.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Chen M, Qi L, Min T, Wen S, Pi R and Lin
D: Synthesis and biological evaluation of n-butylphthalide
derivatives as anti-platelet aggregation agents. Nat Prod Res. 1–4.
2016.(Epub ahead of print).
|
|
33
|
Wang HM, Zhang T, Huang JK and Sun XJ:
3-N-butylphthalide (NBP) attenuates the amyloid-β-induced
inflammatory responses in cultured astrocytes via the nuclear
factor-κB signaling pathway. Cell Physiol Biochem. 32:235–242.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Wang YG, Li Y, Wang CY, Ai JW, Dong XY,
Huang HY, Feng ZY, Pan YM, Lin Y, Wang BX and Yao LL:
L-3-n-butylphthalide protects rats' cardiomyocytes from
ischaemia/reperfusion-induced apoptosis by affecting the
mitochondrial apoptosis pathway. Acta Physiol (Oxf). 210:524–533.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Yin W, Lan L, Huang Z, Ji J, Fang J, Wang
X, Ji H, Peng S, Xu J and Zhang Y: Discovery of a ring-opened
derivative of 3-n-butylphthalide bearing NO/H2S-donating moieties
as a potential anti-ischemic stroke agent. Eur J Med Chem.
115:369–380. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Li J, Yin L, Ogle M, Xin Zhou, Minke Song,
Ping Yu Shan and Ling Wei: dl-3-n-Butylphthalide prevents neuronal
cell death after focal cerebral ischemia in mice via the JNK
pathway. Brain Res. 1359:216–226. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Tiwari BK, Pandey KB, Abidi AB and Rizvi
SI: Markers of oxidative stress during diabetes mellitus. J
Biomark. 2013:1–8. 2013. View Article : Google Scholar
|
|
38
|
Bandeira SM, Gda S Guedes, da Fonseca LJ,
Pires AS, Gelain DP, Moreira JC, Rabelo LA, Vasconcelos SM and
Goulart MO: Characterization of blood oxidative stress in type 2
diabetes mellitus patients: Increase in lipid peroxidation and SOD
activity. Oxid Med Cell Longev. 2012:8193102012. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Pencea V, Bingaman KD, Wiegand SJ and
Luskin MB: Infusion of brain-derived neurotrophic factor into the
lateral ventricle of the adult rat leads to new neurons in the
parenchyma of the striatum, septum, thalamus, and hypothalamus. J
Neurosci. 21:6706–6717. 2001.PubMed/NCBI
|
|
40
|
Mizuno M, Yamada K, Olariu A, Nawa H and
Nabeshima T: Involvement of brain-derived neurotrophic factor in
spatial memory formation and maintenance in a radial arm maze test
in rats. J Neurosci. 20:7116–7121. 2000.PubMed/NCBI
|