Introduction
The prevalence of diabetes mellitus is likely to
exceed 591.9 million by 2035, and is becoming a serious
international health crisis (1,2). The
hallmark of diabetes mellitus is chronic hyperglycemia, resulting
in vascular complications, including the impairment of
angiogenesis, eventually resulting in disorders of wound healing
and the development of refractory low extremity ulcerations
(3,4).
A previous study demonstrated that circulating
endothelial precursor cells (EPCs), a multifunctional population
derived from bone marrow, are important for the promotion of
angiogenesis and the maintenance of vascular homeostasis (5). An impairment in circulating EPCs may
contribute to the pathogenesis of diabetic vasculopathy (6–8).
Also, it has been observed that patients with type 1 and type 2
diabetes mellitus (T2DM) exhibited marked dysfunction in EPCs
(9,10). In addition, a marked reduction in
circulating EPCs was observed in diabetic patients (11–13).
Preclinical experiments have demonstrated impaired tube formation
in the EPCs of diabetic mice (14). These previous data indicated that
the dysfunction of EPCs may be association with a deterioration in
wound healing in diabetes (15,16).
Metformin, an oral antihyperglycaemic agent, is the
first-line drug in the clinic for patients with T2DM (17,18).
Studies have demonstrated that metformin is able to increase the
circulating EPC number in addition to improving the cellular
function of EPCs in patients with T2DM (8,19).
Thrombospondin-1 (TSP-1), a novel antiangiogenic adipokine, has
been reported to be expressed in animal models susceptible to
diabetes, including obesity and insulin resistance (20). Genetically, augmented mRNA
expression of TSP-1 has been observed in diabetes mellitus
(21,22). A previous study demonstrated an
apparent detrimental effect of TSP-1 on EPC function, which was
reported to be negatively-correlated with nitric oxide (NO)
regeneration in in vitro endothelial cells (23). Although metformin has been reported
to be a regulatory factor for TSP-1 in patients with polycystic
ovarian syndrome, little data are currently available in diabetes
(24).
Xie et al (25) reported that the function of EPCs is
associated with cellular oxidative stress. The study demonstrated
that a decrease in the NO level or excess generation of superoxide
(O2−) may result in a detrimental effect on
EPCs, as indicated by impaired angiogenesis and tube formation.
Little data is available concerning the role of metformin in
improving impaired wound closure in T2DM. The present study
hypothesized that metformin may be able to contribute to wound
healing in T2DM mice, and that this protective effect may be partly
attributed to an improvement in EPC function with the involvement
of TSP-1 and cellular oxidative stress.
Materials and methods
Animals
A total of 14 male C57BLKS/J db/db diabetic
mice (age, 6 weeks; weight, 32–36 g) were purchased from Shanghai
SLAC Laboratory Animal Co., Ltd. (Shanghai, China) and 7 male
C57BL/6J non-diabetic mice (age, 6 weeks; weight, 16–18 g) were
obtained from Sino-British SIPPR/BK Lab Animal Ltd. (Shanghai,
China). Mice were housed in a well-ventilated holding room with a
12-h light-dark cycle at an ambient temperature of 23±2°C and 70%
humidity, with free access to water and food. All studies were in
accordance with the Guide for the Care and Use of Laboratory
Animals published by the National Institutes of Health (Bethesda,
MD, USA). The present study was approved by the Animal Care and
Ethics Committee of Second Military Medical University (Shanghai,
China).
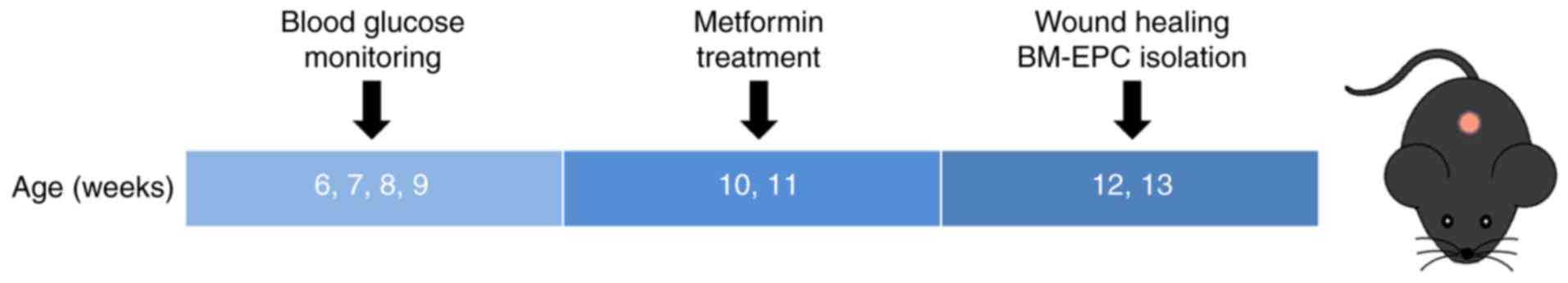
Experimental protocols
Male db/db mice with obesity and
hyperglycemia were used as a model of T2DM. Male age-matched
C57BL/6J mice were used as control non-diabetic mice and received
treatment with a vehicle. The db/db mice were randomly
divided into 2 groups, either receiving the vehicle [0.5%
carboxymethyl cellulose-Na; 10 ml/kg/day; intragastric (i.g.)] or
metformin (250 mg/kg/day; i.g.; Sigma-Aldrich; Merck KGaA,
Darmstadt, Germany) for 14 consecutive days. Whole blood samples
from the tail veins of the mice were used for detecting blood
glucose via a monitoring system (Maochang, Taipei, China). The mice
were used for wound healing experiments, or anesthetized for the
harvesting of bone marrow to isolate EPCs (BM-EPCs) (Fig. 1).
Analysis of wound closure
A 6-mm circular wound was produced by punch biopsy,
and digital images of the wound on the dorsum were captured every 2
days until the end of the experiment for all experimental mice. The
wound areas were analyzed by tracing the wound margins and
calculated using Image-Pro Plus software version 6.0 (Media
Cybernetics, Rockville, MD, USA). The closure was expressed as a
percentage area of the original wound area (26).
Wound angiogenesis
Wounds were harvested from mice on days 7 and 14
following the creation of the wound. Platelet endothelial cell
adhesion molecule (CD31) staining was used to evaluate
angiogenesis. Samples of skin at the wounded area and surrounding
tissue (~1 cm in diameter, ~2 mm in thickness) were excised,
bisected, and fixed in 10% formalin for 6 h at room temperature.
The samples were subsequently embedded in paraffin. Following
deparaffinization, rehydration with decreasing alcohol series,
antigen retrieval (0.5 h at 90°C in 10 mM citrate buffer) and 5%
serum blocking (3 h at room temperature; Chemicon International,
Inc., Temecula, CA, USA), the slides were incubated with an
anti-CD31 antibody (2 µg/ml; cat. no. 550274; BD Biosciences, San
Jose, CA, USA) for 1 h at room temperature and subsequently
incubated with a biotinylated secondary antibody (1:500; cat. no.
BA-9200; Vectastain Elite ABC kit; Vector Laboratories Ltd.,
Peterborough, UK) for 1 h at room temperature. The samples were
counterstained with hematoxylin for 2 min at room temperature
(27). CD31-positive tubular
structures were considered to be capillaries and the capillary
density in the wound healing area was quantified. One slide from
each mouse was examined and, for each slide, two high-power fields
(magnification, ×200) were examined using a light microscope. The
capillaries were then counted.
Quantification of circulating
EPCs
Circulating EPCs were determined according to a
previously-described technique (28). Peripheral blood was acquired by
removing the eyeballs from anesthetized mice. The samples were
dissolved in PBS (1:1), following which gradient centrifugation
liquid 1083 (Sigma-Aldrich; Merck KGaA) was used for the separation
of peripheral blood mononuclear cells at 400 × g for 30 min. The
mononuclear fraction was extracted and the erythrocytes were lysed
with red blood cell lysis buffer (Beyotime Institute of
Biotechnology, Haimen, China). Following washing, the samples were
suspended for incubation (0.5 h at room temperature) using a buffer
solution containing fluorescein isothiocyanate-ataxin-1 (Sca-1)
(1:100; cat. no. 557405; BD Biosciences) and phycoerythrin-vascular
endothelial growth factor receptor 2 (Flk-1) (1:100; cat. no.
555308; BD Biosciences) antibodies for flow cytometry detection and
analyzed using FlowJo software version 7.6 (Tree Star Inc.,
Ashland, OR, USA). Sca-1/Flk-1 double-positive cells were defined
as circulating EPCs.
Isolation of the BM-EPCs
The isolation and culturing of mouse BM-EPCs were in
accordance with a previous technique (25). BM-EPCs were obtained from mouse
tibias and femurs and seeded in 6-well plates coated with
vitronectin (Sigma-Aldrich; Merck KGaA). Cells were cultured in
endothelial growth medium-2 (Cambrex Corp., East Rutherford, NJ,
USA) supplemented with 10% fetal bovine serum (Gibco; Thermo Fisher
Scientific, Inc.) at 37°C, 5% CO2. A total of 4 days
subsequent to cultivation, the culture medium, including
nonadherent cells, was changed for fresh medium and adherent cells
were subjected to further culturing for 3 days. The supernatant was
collected for western blot quantification and the cells were used
for in vitro studies.
In vitro cell assays
Evaluation of the function of BM-EPCs
A tube formation assay, a previously described
method, was adopted to evaluate BM-EPC function (29). A total of 40,000 BM-EPCs were
seeded in 96-well plates which were precoated with 50 µl/well
growth factor-induced Matrigel (BD Biosciences). Following 8 h of
incubation at 37°C, images of tube morphology were captured using a
computer-assisted microscope (Leica Microsystems GmbH, Wetzlar,
Germany). Tube numbers were measured in five low power fields
(magnification, ×50) for each sample at random.
Measurement of intracellular NO and
O2−
The intracellular NO level was determined using
membrane-permeable 4-amino-5-methylamino-2′, 7′-difluorofluorescein
(DAF-FM) diacetate (Invitrogen; Thermo Fisher Scientific, Inc.). A
total of 7 days subsequent to BM-EPC culturing, the cells were
harvested and incubated with DAF-FM diacetate (10−6
mol/l) for 30 min at 37°C and an additional 30 min at room
temperature in dark. Following incubation, the DAF-FM fluorescence
intensity in cells was measured by flow cytometry (25).
The intracellular O2− level
was detected using the membrane-permeable dye dihydroethidium (DHE;
Invitrogen; Thermo Fisher Scientific, Inc.), which is oxidized to
ethidium bromide in the presence of O2−.
Following 7 days of culturing, BM-EPCs were harvested and incubated
with DHE (0.5×10−6 mol/l) for 30 min at room temperature
in dark. Following staining, the DHE fluorescence intensity in
cells was examined by flow cytometry (25).
Western blot analysis
Western blotting was performed as previously
described (30). TSP-1 secreted by
BM-EPCs was obtained by condensing the BM-EPC culture media using a
commercial filter device. The concentration of TSP-1 was determined
using a bicinchoninic acid assay (Thermo Fisher Scientific, Inc.).
For the western blotting experiments, ~30-µg samples were loaded
and run on an 8% SDS-PAGE gel. The proteins were
electrophoretically transferred to nitrocellulose membranes.
Subsequently, the membranes were blocked with 5% bovine serum
albumin (Sigma-Aldrich; Merck KGaA) in Tris-buffered saline
containing 0.1% Tween 20 (TBST) for 1 h at room temperature, washed
and incubated with the primary antibody for TSP-1 (1:500; cat. no.
ab85762; Abcam, Cambridge, UK) at 4°C overnight. IRDye
800-conjugated rabbit anti-mouse IgG was used as the secondary
antibody (1:5,000; cat. no. 925-32212; LI-COR Biosciences, Lincoln,
NE, USA) and incubated for 0.5 h at room temperature. The bands
were obtained using an Odyssey infrared imaging system (LI-COR
Biosciences), and the expression levels of TSP-1 protein were
quantified using Quantity One software version 4.2 (Bio-Rad
Laboratories, Inc., Hercules, CA, USA).
Statistical analysis
Data are expressed as the mean ± standard error of
the mean. Statistical significance was analyzed by one-way analysis
of variance followed by the Newman-Keuls multiple comparison test,
using GraphPad Prism Software version 5 (GraphPad Software, Inc.,
La Jolla, CA, USA). P<0.05 was considered to indicate a
statistically significant difference.
Results
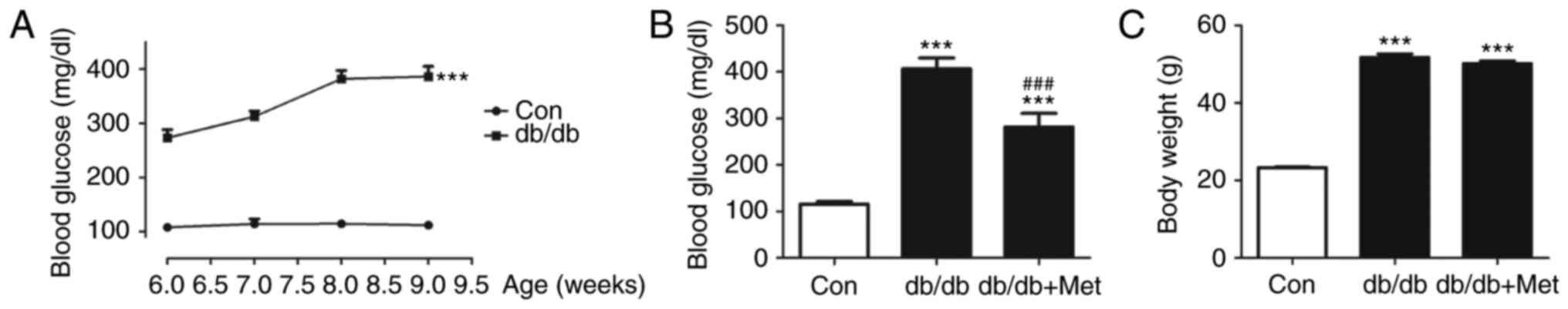
Effect of metformin on blood glucose
and body weight in db/db mice
A significant increase in blood glucose was observed
in db/db mice compared with the control (338.4±27.6 vs.
112.1±1.5 mg/dl; P<0.001; Fig.
2A). Pretreatment with metformin improved the blood glucose
level (Fig. 2B), although it did
not modify body weight in db/db mice (Fig. 2C).
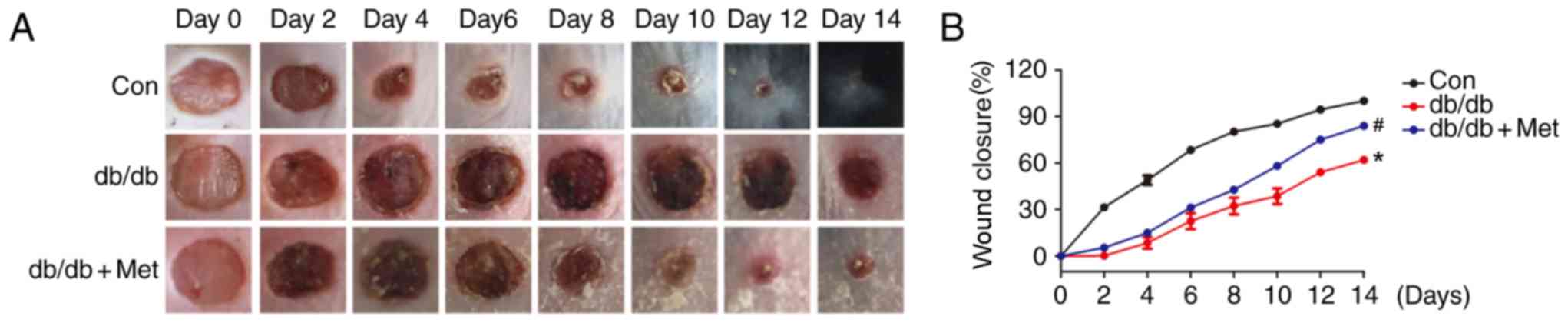
Metformin accelerates wound healing
and angiogenesis in db/db mice
In order to examine the effects of pretreatment with
metformin on wound closure in db/db mice, alterations in the
wounded skin were observed on alternate days until day 14. Fig. 3A exhibits the gross appearance of
the wounds during the 14 days following injury. Db/db mice
exhibited a marked delay in wound closure compared with the
control. By contrast, wounds in db/db mice pretreated with
metformin underwent gradual and progressive healing until reaching
complete closure (Fig. 3A).
Statistically, treatment with metformin significantly accelerated
wound closure in db/db mice when compared with the untreated
db/db mice (P<0.05; Fig.
3B).
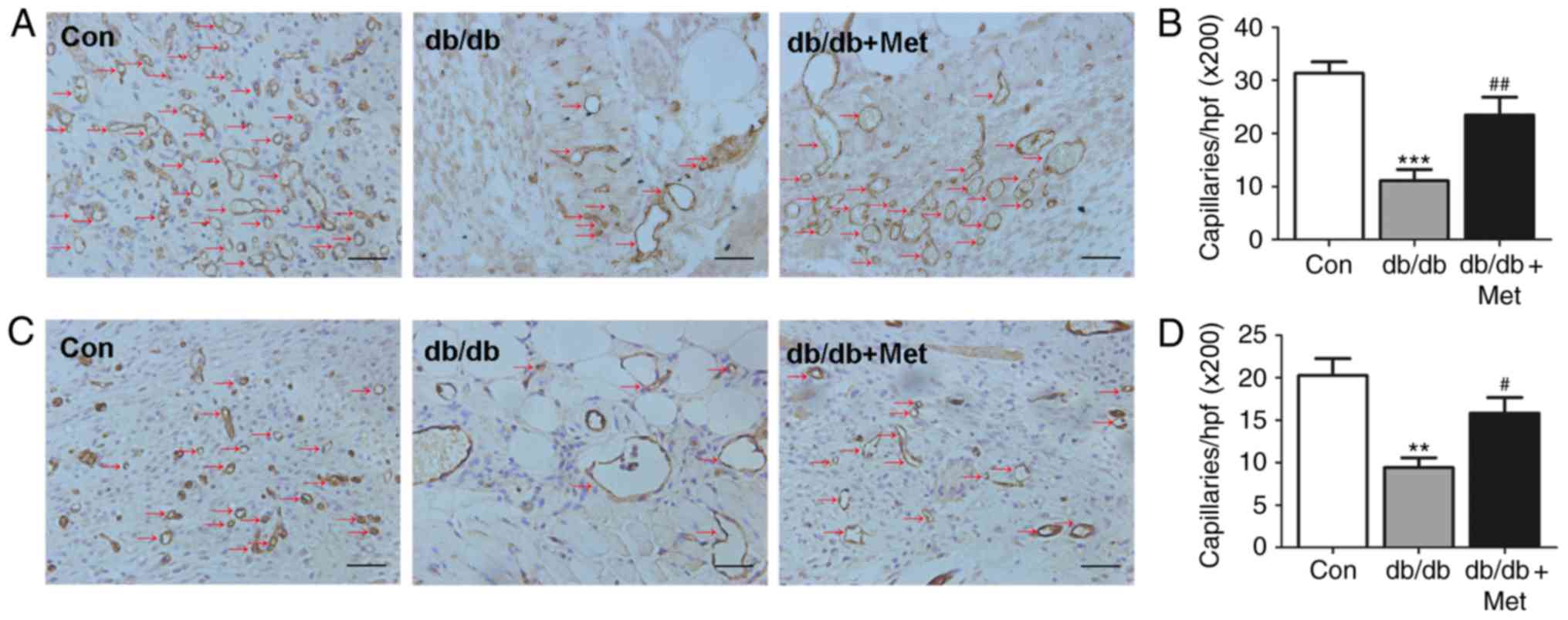
In order to further examine the role of metformin
treatment in skin neovascularization, the number of tubular
structures, indicated by CD31 staining of the skin tissue harvested
from the wound area, were calculated (Fig. 4). A significant decrease in
capillary formation was observed in db/db mice on days 7
(P<0.001; Fig. 4B) and 14
(P<0.01; Fig. 4D) compared with
the control. Capillary formation in db/db mice was
significantly improved on days 7 (P<0.01; Fig. 4B) and 14 (P<0.05; Fig. 4D) following pretreatment with
metformin.
Metformin improves BM-EPC function in
db/db mice
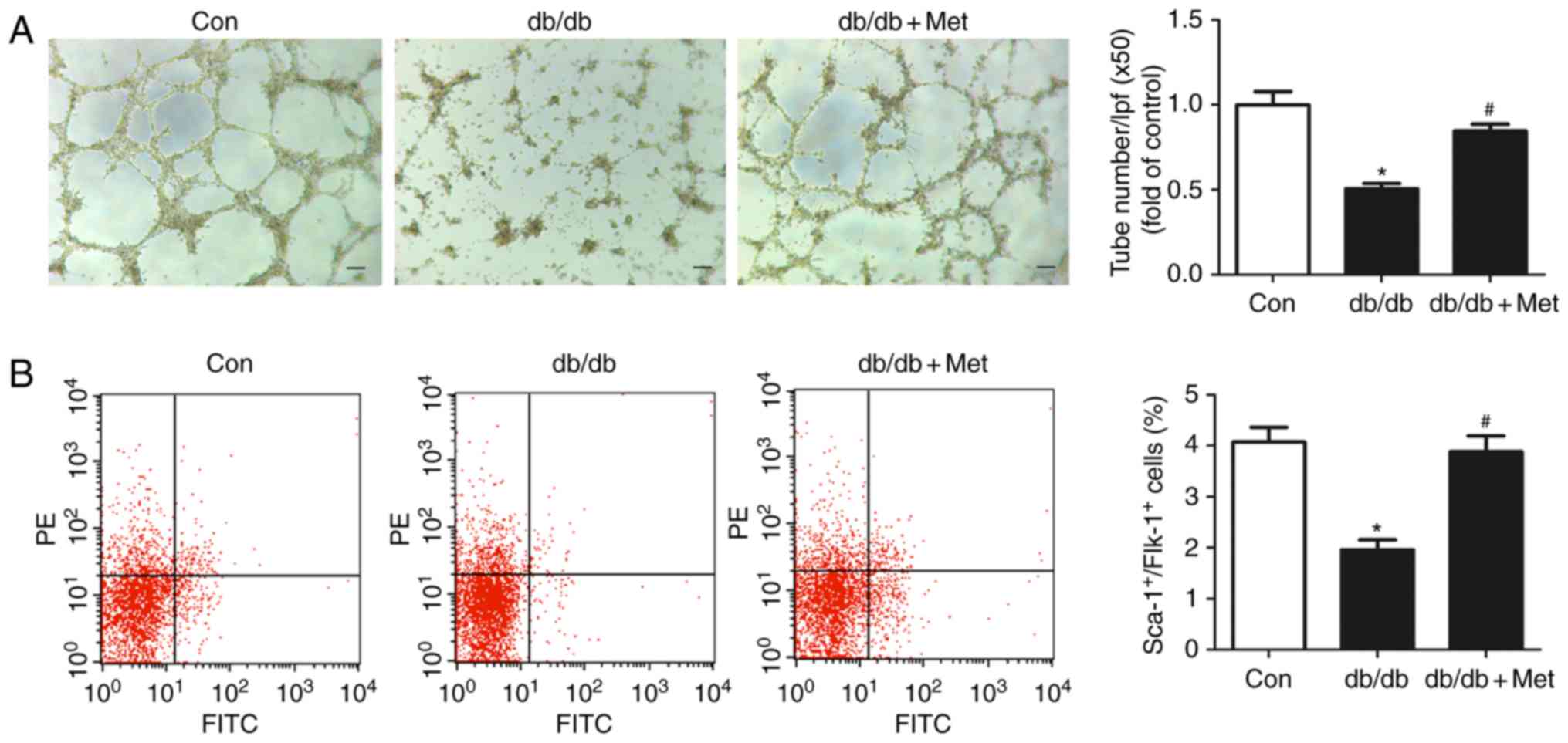
In order to further examine the mechanism underlying
the role of metformin in accelerating wound closure, the tube
formation capacity of EPCs from db/db mice was determined.
Impaired EPCs were observed in db/db mice compared with the
control. Pretreatment with metformin significantly improved tube
formation capacity in db/db mice (0.70±0.04 vs. 0.54±0.04;
P<0.05; Fig. 5A). A decrease in
the circulating EPC number was observed in db/db mice
compared with the control, which was partially reversed by
pretreatment with metformin (2.18±0.32% vs. 1.11±0.18%; P<0.05;
Fig. 5B).
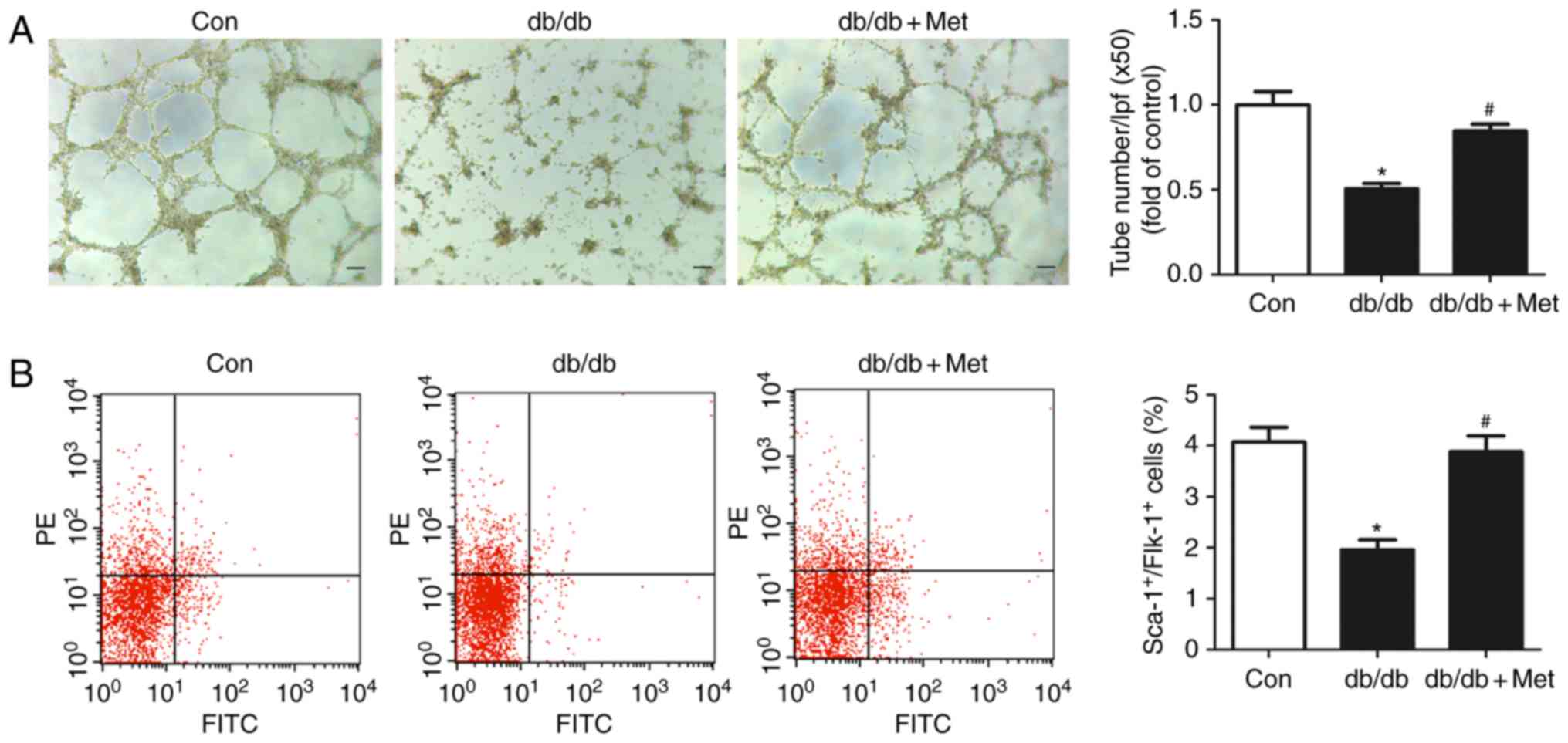 | Figure 5.Metformin therapy ameliorates BM-EPC
function in db/db mice. (A) Representative images of the
tube formation assay of BM-EPCs. The number of tubes in each sample
was calculated from 5 fields (magnification, ×50; scale bar, 100
µm) at random. Treatment with metformin ameliorated the tube
formation of BM-EPCs. (B) EPC numbers were detected by flow
cytometry and the percentage of Sca-1+/Flk-1+
cells was calculated. Metformin elevated the circulating EPC number
in db/db mice. *P<0.05 vs. Con; #P<0.05 vs.
db/db. Values are expressed as the mean ± standard error of
the mean (n=7 mice/group). Con, control; Met, metformin; BM-EPC,
bone marrow-endothelial precursor cell; PE, phycoerythrin; FITC,
fluorescein isothiocyanate; Sca-1, ataxin-1; Flk-1, vascular
endothelial growth factor receptor 2; lpf, low-power field. |
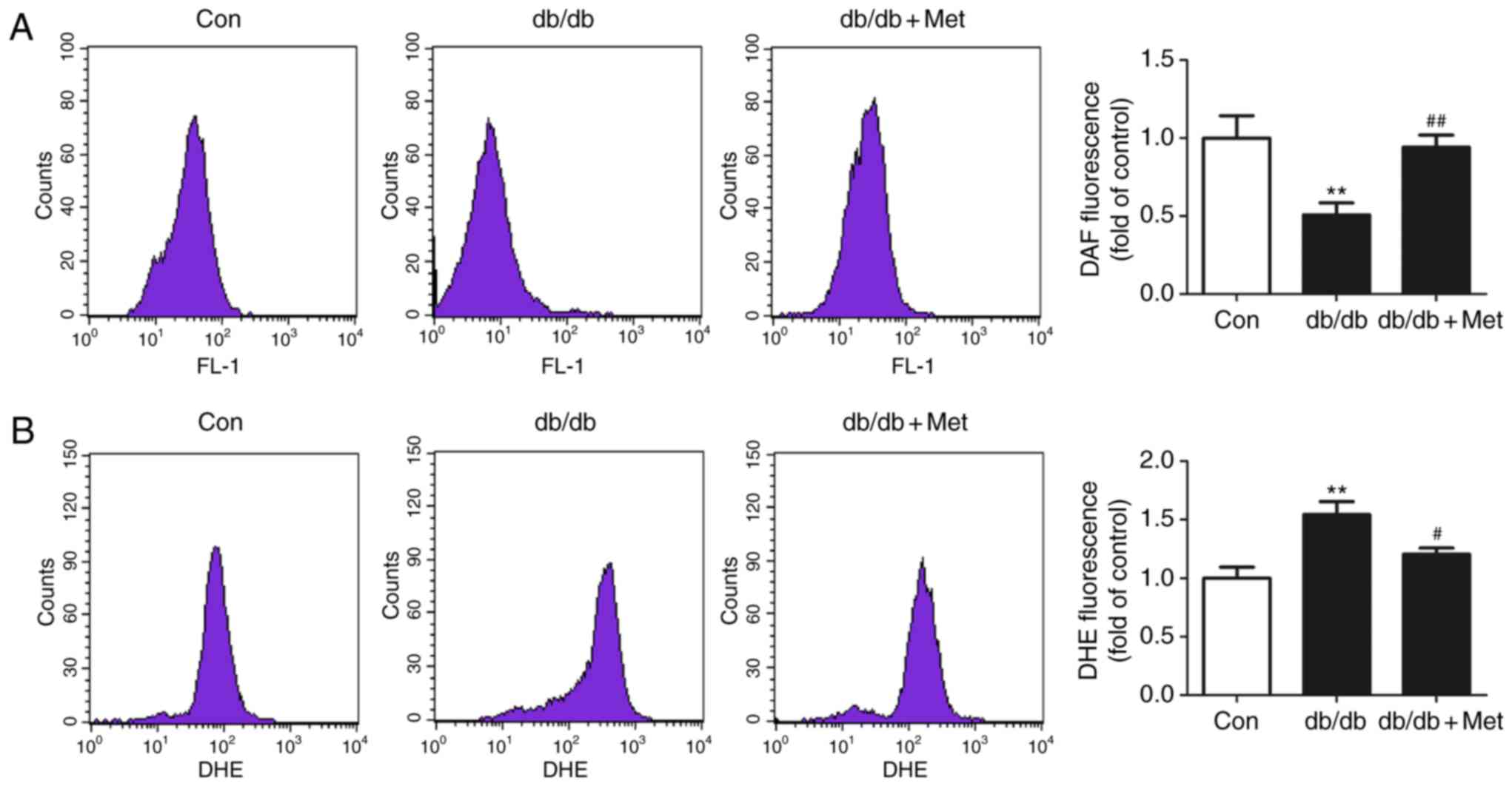
Metformin increases intracellular NO
production and decreases the intracellular
O2− level in BM-EPCs from db/db mice
There was significant decrease in intracellular NO
in BM-EPCs from db/db mice compared with the control
(P<0.01; Fig. 6A), and
pretreatment with metformin significantly increased the
intracellular NO level of BM-EPCs in db/db mice (P<0.01;
Fig. 6A). By contrast, the
intracellular O2− level in BM-EPCs from
db/db mice was significantly elevated compared with the
control (P<0.01; Fig. 6B).
However, pretreatment with metformin significantly decreased the
levels of intracellular O2− in BM-EPCs from
db/db mice (P<0.05; Fig.
6B).
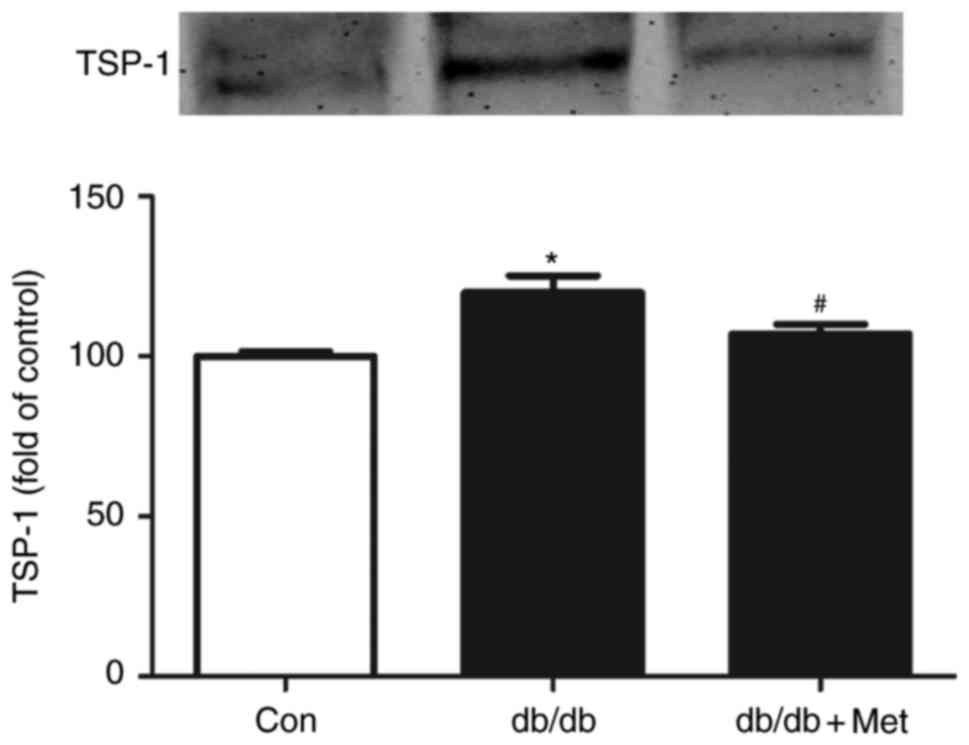
Metformin inhibits TSP-1 secretion in
BM-EPCs from db/db mice
Elevated TSP-1 secretion was observed in BM-EPCs
from db/db mice, as indicated by western blot analysis of
the supernatant from the cell culture medium, when compared with
the control (P<0.05; Fig. 7).
By contrast, a significant decrease in TSP-1 was detected in the
culture medium of BM-EPCs from metformin-pretreated db/db
mice (P<0.05; Fig. 7).
Discussion
The principal findings of the present study were as
follows: i) Metformin accelerated wound closure and improved
angiogenesis in db/db mice; ii) metformin improved BM-EPC
function in db/db mice; iii) metformin augmented the
decreased NO level and reduced the increased
O2− production in the BM-EPCs of db/db
mice; and iv) metformin decreased the serum TSP-1 level secreted
from the BM-EPCs of db/db mice.
In the present study, db/db mice, with
genetic hyperglycemia akin to adult-onset T2DM as a consequence of
an inactive gene mutation affecting leptin receptors, were
specifically selected as the T2DM model (31–33);
this model has been widely recognized to be well-established animal
model for investigating the association between hyperglycemia, EPC
function and wound closure (34).
Wound healing following tissue damage is a sophisticated
pathophysiological process which requires comprehensive
interactions between cells and a variety of signaling molecules
(35). However, diabetes may cause
disorders in the tissue microenvironment, in addition to
impairments in cellular function and wound healing. Angiogenesis is
important for promoting vessel formation which, in turn, provides
regenerating tissue with the required oxygen and nutrients
(35,36). CD31 is a typical marker for tracing
vascular and endothelial cells (37). It was observed in the present study
that healing capacity was decreased in genetically diabetic
db/db mice, as indicated by staining of CD31, when compared
with non-diabetic mice. These data were consistent with a previous
report (38).
Currently, regarding the role of metformin on EPC
function and wound healing, the published literature is subjected
to a degree of controversy. For example, previous studies have
indicated that metformin contributed to accelerated wound healing
and an enhanced quantity of circulating EPCs and BM-EPC function in
diabetes (39,40). Another study held the opposite
opinion, that metformin treatment did not result in any alterations
in the circulating EPC number, and even caused delayed wound
healing in diabetes (41). The
results of the present study demonstrated that treatment with
metformin accelerated wound healing and improved angiogenesis.
EPCs, as precursors of endothelial cells, can
mobilize from the bone marrow into the circulation and have been
implicated in neovascularization following tissue injury (5,23,42).
Reduced EPC numbers and impaired EPC function have been observed in
diabetic patients (43).
Metformin, a biguanide family member, is a commonly applied
therapeutic drug for T2DM (44,45).
Studies have demonstrated that metformin contributed substantially
to increasing the circulating EPC number and maintaining
endothelial cell function in patients with T2DM (19), while the associated mechanisms
remain largely unclear. In the present study, db/db mice
pretreated with metformin (250 mg/kg/day) for 2 weeks exhibited an
increased EPC number and improved EPC function.
Gao et al (46) demonstrated that NO serves an
important role in regulating tube formation in EPCs. Gallagher
et al (16) demonstrated
that induced expression of NO in bone marrow was highly correlated
with increased mobilization of EPCs to the circulation. In the
present study, metformin contributed to the elevation of NO levels
in EPCs from db/db mice, in addition to a significantly
increased circulating EPC number and improved EPC function. It has
been demonstrated that a decreased intracellular
O2− level may be accompanied by an
improvement in EPC dysfunction and an enhanced NO level in EPCs
(25,26). In the present study, it was
observed that the generation of O2− was
increased, and treatment with metformin was able to inhibit the
production of O2− in EPCs from db/db
mice.
TSP-1, an endogenous anti-angiogenic mediator, has
been demonstrated to be involved in vascular complications in
diabetes (47). In a T2DM animal
model, TSP-1 in the vessel walls was elevated at the mRNA and
protein levels (22). In addition,
preclinical studies suggested that the proangiogenic factor NO was
a biological antagonist of TSP-1 (48,49).
Ridnour et al (49)
observed that the protective effect of NO on endothelial cells was
accompanied by TSP-1 downregulation. Xu et al (50) reported that the TSP-1 level was
upregulated in impaired retinal capillaries provoked by nitrative
stress in diabetic rats. The results of the present study
identified that TSP-1 was increased and NO was decreased in
db/db mice, accompanied by wound healing delay, angiogenesis
impairment and EPC dysfunction. Treatment with metformin was able
to significantly alleviate disorders in wound healing, stimulate
angiogenesis and improve EPC function, with TSP-1 levels inhibited
and NO levels upregulated in BM-EPCs from db/db mice.
In conclusion, the results of the present study
demonstrated that wound healing, angiogenesis and EPC function were
impaired in db/db mice. Treatment with metformin was able to
accelerate wound healing, which was possibly associated with an
improvement in EPC function via a TSP-1/NO pathway.
Acknowledgements
The present study was supported by grants from the
Natural Science Foundation of Hangzhou (grant nos. 20131813A20,
20130733Q41 and 20150633B58) and the Natural Science Foundation of
Zhejiang (grant no. 2013RCB014). The abstract was presented at the
American Association of Pharmaceutical Scientists Annual Meeting
and Exposition, 13th-17th November 2016, in Denver, CO, USA.
Glossary
Abbreviations
Abbreviations:
|
T2DM
|
type 2 diabetes mellitus
|
|
BM-EPCs
|
bone marrow-endothelial precursor
cells
|
|
NO
|
nitric oxide
|
|
O2-
|
superoxide
|
|
TSP-1
|
thrombospondin-1
|
|
CD31
|
platelet endothelial cell adhesion
molecule
|
|
DAF-FM
|
4-amino-5-methylamino-2′,
7′-difluorofluorescein
|
|
DHE
|
dihydroethidium
|
|
i.g.
|
intragastric
|
|
Sca-1
|
ataxin-1
|
|
Flk-1
|
vascular endothelial growth factor
receptor 2
|
References
|
1
|
Chan JC, Cho NH, Tajima N and Shaw J:
Diabetes in the Western Pacific Region-past, present and future.
Diabetes Res Clin Pract. 103:244–255. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Thandavarayan RA, Garikipati VN,
Joladarashi D, Babu S Suresh, Jeyabal P, Verma SK, Mackie AR, Khan
M, Arumugam S, Watanabe K, et al: Sirtuin-6 deficiency exacerbates
diabetes-induced impairment of wound healing. Exp Dermatol.
24:773–778. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Papanas N, Demetzos C, Pippa N, Maltezos E
and Tentolouris N: Efficacy of a new heparan sulfate mimetic
dressing in the healing of foot and lower extremity ulcerations in
type 2 diabetes: A case series. Int J Low Extrem Wounds. 15:63–67.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Zgheib C and Liechty KW: Shedding light on
miR-26a: Another key regulator of angiogenesis in diabetic wound
healing. J Mol Cell Cardiol. 92:203–205. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Li DW, Liu ZQ, Wei J, Liu Y and Hu LS:
Contribution of endothelial progenitor cells to neovascularization
(Review). Int J Mol Med. 30:1000–1006. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Fadini GP, Sartore S, Albiero M, Baesso I,
Murphy E, Menegolo M, Grego F, de Kreutzenberg S Vigili, Tiengo A,
Agostini C and Avogaro A: Number and function of endothelial
progenitor cells as a marker of severity for diabetic vasculopathy.
Arterioscler Thromb Vasc Biol. 26:2140–2146. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Kovacic JC, Moore J, Herbert A, Ma D,
Boehm M and Graham RM: Endothelial progenitor cells, angioblasts,
and angiogenesis-old terms reconsidered from a current perspective.
Trends Cardiovasc Med. 18:45–51. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Liao YF, Chen LL, Zeng TS, Li YM, Fan Yu,
Hu LJ and Ling Yue: Number of circulating endothelial progenitor
cells as a marker of vascular endothelial function for type 2
diabetes. Vasc Med. 15:279–285. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Tepper OM: Human endothelial progenitor
cells from type II diabetics exhibit impaired proliferation,
adhesion, and incorporation into vascular structures. Circulation.
106:2781–2786. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Wang CH, Ting MK, Verma S, Kuo LT, Yang
NI, Hsieh IC, Wang SY, Hung A and Cherng WJ: Pioglitazone increases
the numbers and improves the functional capacity of endothelial
progenitor cells in patients with diabetes mellitus. Am Heart J.
152:1051.e1–8. 2006. View Article : Google Scholar
|
|
11
|
Fadini GP, Miorin M, Facco M, Bonamico S,
Baesso I, Grego F, Menegolo M, de Kreutzenberg SV, Tiengo A,
Agostini C and Avogaro A: Circulating endothelial progenitor cells
are reduced in peripheral vascular complications of type 2 diabetes
mellitus. J Am Coll Cardiol. 45:1449–1457. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Nakamura K, Oe H, Kihara H, Shimada K,
Fukuda S, Watanabe K, Takagi T, Yunoki K, Miyoshi T, Hirata K, et
al: DPP-4 inhibitor and alpha-glucosidase inhibitor equally improve
endothelial function in patients with type 2 diabetes: EDGE study.
Cardiovasc Diabetol. 13:1102014. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Yue WS, Lau KK, Siu CW, Wang M, Yan GH,
Yiu KH and Tse HF: Impact of glycemic control on circulating
endothelial progenitor cells and arterial stiffness in patients
with type 2 diabetes mellitus. Cardiovasc Diabetol. 10:1132011.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Badr G, Hozzein WN, Badr BM, Al Ghamdi A,
Eldien HM Saad and Garraud O: Bee venom accelerates wound healing
in diabetic mice by suppressing activating transcription factor-3
(ATF-3) and inducible nitric oxide synthase (iNOS)-mediated
oxidative stress and recruiting bone marrow-derived endothelial
progenitor cells. J Cell Physiol. 231:2159–2171. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Gallagher KA, Goldstein LJ, Thom SR and
Velazquez OC: Hyperbaric oxygen and bone marrow-derived endothelial
progenitor cells in diabetic wound healing. Vascular. 14:328–337.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Gallagher KA, Liu ZJ, Xiao M, Chen H,
Goldstein LJ, Buerk DG, Nedeau A, Thom SR and Velazquez OC:
Diabetic impairments in NO-mediated endothelial progenitor cell
mobilization and homing are reversed by hyperoxia and SDF-1 alpha.
J Clin Invest. 117:1249–1259. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Hattori Y, Hattori K and Hayashi T:
Pleiotropic benefits of metformin: Macrophage targeting its
anti-inflammatory mechanisms. Diabetes. 64:1907–1909. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Li DJ, Huang F, Lu WJ, Jiang GJ, Deng YP
and Shen FM: Metformin promotes irisin release from murine skeletal
muscle independently of AMP-activated protein kinase activation.
Acta Physiol (Oxf). 213:711–721. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Chen LL, Liao YF, Zeng TS, Yu F, Li HQ and
Feng Y: Effects of metformin plus gliclazide compared with
metformin alone on circulating endothelial progenitor cell in type
2 diabetic patients. Endocrine. 38:266–275. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Varma V, Yao-Borengasser A, Bodles AM,
Rasouli N, Phanavanh B, Nolen GT, Kern EM, Nagarajan R, Spencer HJ
III, Lee MJ, et al: Thrombospondin-1 is an adipokine associated
with obesity, adipose inflammation, and insulin resistance.
Diabetes. 57:432–439. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Dabir P, Marinic TE, Krukovets I and
Stenina OI: Aryl hydrocarbon receptor is activated by glucose and
regulates the thrombospondin-1 gene promoter in endothelial cells.
Circ Res. 102:1558–1565. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Stenina OI, Krukovets I, Wang K, Zhou Z,
Forudi F, Penn MS, Topol EJ and Plow EF: Increased expression of
thrombospondin-1 in vessel wall of diabetic Zucker rat.
Circulation. 107:3209–3215. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Tie L, Chen LY, Chen DD, Xie HH, Channon
KM and Chen AF: GTP cyclohydrolase I prevents diabetic-impaired
endothelial progenitor cells and wound healing by suppressing
oxidative stress/thrombospondin-1. Am J Physiol Endocrinol Metab.
306:E1120–E1131. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Tan BK, Adya R, Chen J, Farhatullah S,
Heutling D, Mitchell D, Lehnert H and Randeva HS: Metformin
decreases angiogenesis via NF-kappaB and Erk1/2/Erk5 pathways by
increasing the antiangiogenic thrombospondin-1. Cardiovasc Res.
83:566–574. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Xie HH, Zhou S, Chen DD, Channon KM, Su DF
and Chen AF: GTP cyclohydrolase I/BH4 pathway protects EPCs via
suppressing oxidative stress and thrombospondin-1 in salt-sensitive
hypertension. Hypertension. 56:1137–1144. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Li ZP, Xin RJ, Yang H, Jiang GJ, Deng YP,
Li DJ and Shen FM: Diazoxide accelerates wound healing by improving
EPC function. Front Biosci (Landmark Ed). 21:1039–1051. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Cai J, Lu S, Yao Z, Deng YP, Zhang LD, Yu
JW, Ren GF, Shen FM and Jiang GJ: Glibenclamide attenuates
myocardial injury by lipopolysaccharides in streptozotocin-induced
diabetic mice. Cardiovasc Diabetol. 13:1062014. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Marrotte EJ, Chen DD, Hakim JS and Chen
AF: Manganese superoxide dismutase expression in endothelial
progenitor cells accelerates wound healing in diabetic mice. J Clin
Invest. 120:4207–4219. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Chen JK, Deng YP, Jiang GJ, Liu YZ, Zhao T
and Shen FM: Establishment of tube formation assay of bone
marrow-derived endothelial progenitor cells. CNS Neurosci Ther.
19:533–535. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Lee MH, Choi EN, Jeon YJ and Jung SC:
Possible role of transforming growth factor-β1 and vascular
endothelial growth factor in Fabry disease nephropathy. Int J Mol
Med. 30:1275–1280. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Aoyama H, Daitoku H and Fukamizu A:
Nutrient control of phosphorylation and translocation of Foxo1 in
C57BL/6 and db/db mice. Int J Mol Med. 18:433–439. 2006.PubMed/NCBI
|
|
32
|
Bao Q, Shen X, Qian L, Gong C, Nie M and
Dong Y: Anti-diabetic activities of catalpol in db/db mice. Korean
J Physiol Pharmacol. 20:153–160. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Tamura Y, Murayama T, Minami M, Yokode M
and Arai H: Differential effect of statins on diabetic nephropathy
in db/db mice. Int J Mol Med. 28:683–687. 2011.PubMed/NCBI
|
|
34
|
Galiano RD, Tepper OM, Pelo CR, Bhatt KA,
Callaghan M, Bastidas N, Bunting S, Steinmetz HG and Gurtner GC:
Topical vascular endothelial growth factor accelerates diabetic
wound healing through increased angiogenesis and by mobilizing and
recruiting bone marrow-derived cells. Am J Pathol. 164:1935–1947.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Galeano M, Altavilla D, Cucinotta D, Russo
GT, Calò M, Bitto A, Marini H, Marini R, Adamo EB, Seminara P, et
al: Recombinant human erythropoietin stimulates angiogenesis and
wound healing in the genetically diabetic mouse. Diabetes.
53:2509–2517. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Zhang XN, Ma ZJ, Wang Y, Li YZ, Sun B, Guo
X, Pan CQ and Chen LM: The four-herb Chinese medicine formula
Tuo-Li-Xiao-Du-San accelerates cutaneous wound healing in
streptozotocin-induced diabetic rats through reducing inflammation
and increasing angiogenesis. J Diabetes Res. 2016:56391292016.
View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Caligiuri G, Groyer E, Khallou-Laschet J,
Al Haj Zen A, Sainz J, Urbain D, Gaston AT, Lemitre M, Nicoletti A
and Lafont A: Reduced immunoregulatory CD31+ T cells in the blood
of atherosclerotic mice with plaque thrombosis. Arterioscler Thromb
Vasc Biol. 25:1659–1664. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Tellechea A, Kafanas A, Leal EC,
Tecilazich F, Kuchibhotla S, Auster ME, Kontoes I, Paolino J,
Carvalho E, Nabzdyk LP and Veves A: Increased skin inflammation and
blood vessel density in human and experimental diabetes. Int J Low
Extrem Wounds. 12:4–11. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Desouza CV: Does drug therapy reverse
endothelial progenitor cell dysfunction in diabetes? J Diabetes
Complications. 27:519–525. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Lin JT, Chen HM, Chiu CH and Liang YJ:
AMP-activated protein kinase activators in diabetic ulcers: From
animal studies to Phase II drugs under investigation. Expert Opin
Investig Drugs. 23:1253–1265. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Ochoa-Gonzalez F, Cervantes-Villagrana AR,
Fernandez-Ruiz JC, Nava-Ramirez HS, Hernandez-Correa AC,
Enciso-Moreno JA and Castañeda-Delgado JE: Metformin induces cell
cycle arrest, reduced proliferation, wound healing impairment in
vivo and is associated to clinical outcomes in diabetic foot ulcer
patients. PLoS One. 11:e01509002016. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Mao L, Huang M, Chen SC, Li YN, Xia YP, He
QW, Wang MD, Huang Y, Zheng L and Hu B: Endogenous endothelial
progenitor cells participate in neovascularization via CXCR4/SDF-1
axis and improve outcome after stroke. CNS Neurosci Ther.
20:460–468. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Kim KA, Shin YJ, Kim JH, Lee H, Noh SY,
Jang SH and Bae ON: Dysfunction of endothelial progenitor cells
under diabetic conditions and its underlying mechanisms. Arch Pharm
Res. 35:223–234. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Ghosh S, Lakshmanan AP, Hwang MJ, Kubba H,
Mushannen A, Triggle CR and Ding H: Metformin improves endothelial
function in aortic tissue and microvascular endothelial cells
subjected to diabetic hyperglycaemic conditions. Biochem Pharmacol.
98:412–421. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Shi Y, He Z, Jia Z and Xu C: Inhibitory
effect of metformin combined with gemcitabine on pancreatic cancer
cells in vitro and in vivo. Mol Med Rep. 14:2921–2928. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Gao L, Li P, Zhang J, Hagiwara M, Shen B,
Bledsoe G, Chang E, Chao L and Chao J: Novel role of kallistatin in
vascular repair by promoting mobility, viability, and function of
endothelial progenitor cells. J Am Heart Assoc. 3:e0011942014.
View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Bhattacharyya S, Marinic TE, Krukovets I,
Hoppe G and Stenina OI: Cell type-specific post-transcriptional
regulation of production of the potent antiangiogenic and
proatherogenic protein thrombospondin-1 by high glucose. J Biol
Chem. 283:5699–5707. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Isenberg JS, Wink DA and Roberts DD:
Thrombospondin-1 antagonizes nitric oxide-stimulated vascular
smooth muscle cell responses. Cardiovasc Res. 71:785–793. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Ridnour LA, Isenberg JS, Espey MG, Thomas
DD, Roberts DD and Wink DA: Nitric oxide regulates angiogenesis
through a functional switch involving thrombospondin-1. Proc Natl
Acad Sci USA. 102:pp. 13147–13152. 2005; View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Xu L, Xun G, Yao Z, Liu Y, Qiu Y, Liu K,
Zhu D, Gu Q, Xu X and Ho PC: Effects of generated trans-arachidonic
acids on retinal capillary during nitrative stress in diabetic
rats. Ophthalmologica. 222:37–41. 2008. View Article : Google Scholar : PubMed/NCBI
|