|
1
|
Komotar RJ, Schmidt JM, Starke RM,
Claassen J, Wartenberg KE, Lee K, Badjatia N, Connolly ES Jr and
Mayer SA: Resuscitation and critical care of poor-grade
subarachnoid hemorrhage. Neurosurgery. 64:397–411. 2009. View Article : Google Scholar
|
|
2
|
Rosengart AJ, Schultheiss KE, Tolentino J
and Macdonald RL: Prognostic factors for outcome in patients with
aneurysmal subarachnoid hemorrhage. Stroke. 38:2315–2321. 2007.
View Article : Google Scholar
|
|
3
|
Steiner T, Juvela S, Unterberg A, Jung C,
Forsting M and Rinkel G: European Stroke Organization: European
Stroke Organization guidelines for the management of intracranial
aneurysms and subarachnoid haemorrhage. Cerebrovasc Dis. 35:93–112.
2013. View Article : Google Scholar
|
|
4
|
Budohoski KP, Czosnyka M, Kirkpatrick PJ,
Smirlewski P, Steiner LA and Pickard JD: Clinical relevance of
cerebral autoregulation following subarachnoid haemorrhage. Nat Rev
Neurol. 9:152–163. 2013. View Article : Google Scholar
|
|
5
|
Laskowitz DT and Kolls BJ: Neuroprotection
in subarachnoid hemorrhage. Stroke. 41 10 Suppl:S79–S84. 2010.
View Article : Google Scholar :
|
|
6
|
Macdonald RL, Higashida RT, Keller E,
Mayer SA, Molyneux A, Raabe A, Vajkoczy P, Wangke I, Bach D, Frey
A, et al: Clazosentan, an endothelin receptor antagonist, in
patients with aneurysmal subarachnoid haemorrhage undergoing
surgical clipping: A randomised, double-blind, placebo-controlled
phase 3 trail (CONSCIOUS-2). Lancet Neurol. 10:618–625. 2011.
View Article : Google Scholar
|
|
7
|
Kontos HA, Wei EP, Navari RM, Levasseur
JE, Rosenblum WI and Patterson JL Jr: Responses of cerebral
arteries and arterioles to acute hypotension and hypertension. Am J
Physiol. 234:H371–H383. 1978.
|
|
8
|
Sehba FA, Pluta RM and Zhang JH:
Metamorphosis of subarachnoid hemorrhage research: From delayed
vasospasm to early brain injury. Mol Neurobiol. 43:27–40. 2011.
View Article : Google Scholar
|
|
9
|
Tousoulis D, Antoniades C, Katsi V,
Bosinakou E, Kotsopoulou M, Tsioufis C and Stefanadis C: The impact
of early administration of low-dose atorvastatin treatment on
inflammatory process, in patients with unstable angina and low
cholesterol level. Int J Cardiol. 109:48–52. 2006. View Article : Google Scholar
|
|
10
|
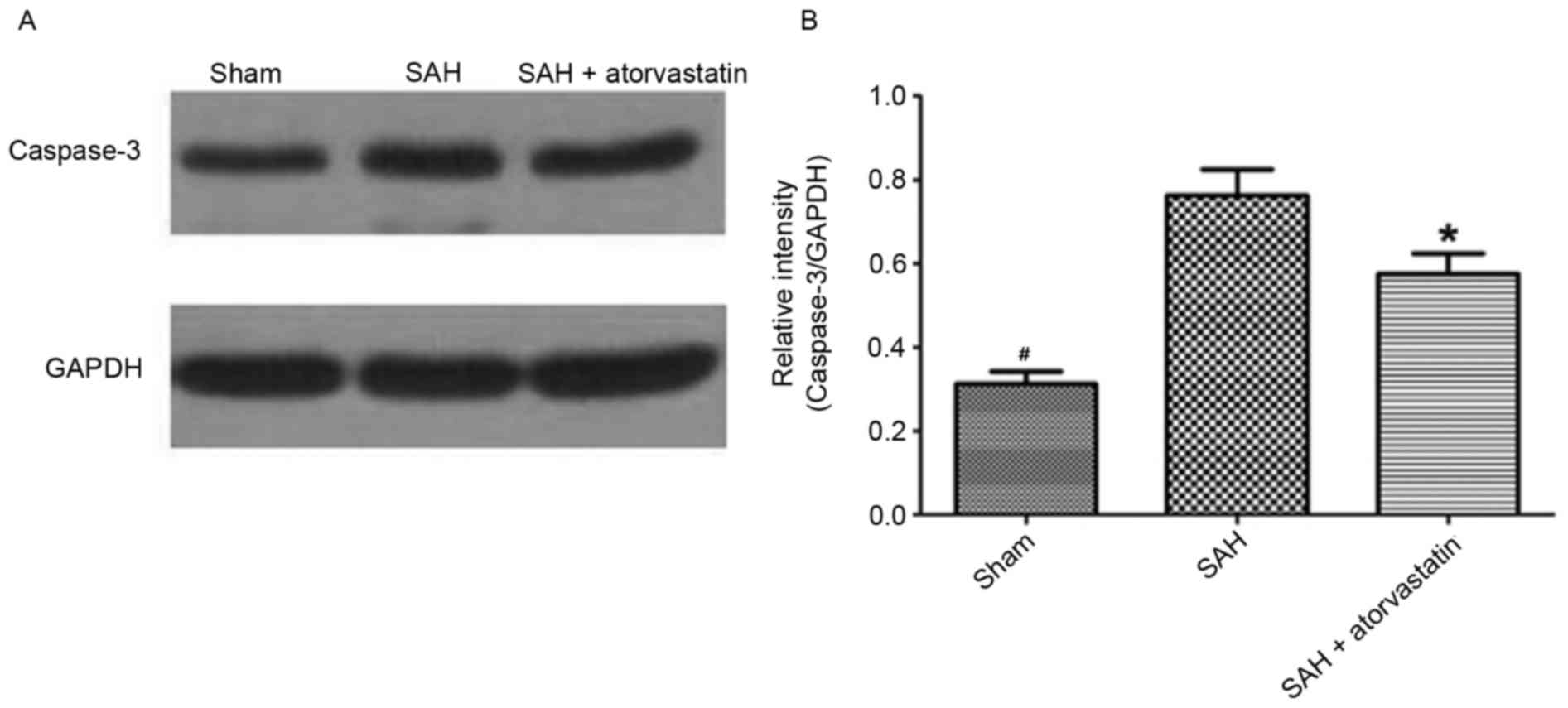
Cheng G, Wei L, Zhi-Dan S, Shi-Guang Z and
Xiang-Zhen L: Atorvastatin ameliorates cerebral vasospasm and early
brain injury after subarachnoid hemorrhage and inhibits
caspase-dependent apoptosis pathway. BMC Neurosci. 10:72009.
View Article : Google Scholar :
|
|
11
|
Tseng MY, Czonsnyka M, Richards H, Pickard
JD and Kirkpatrick PJ: Effects of acute treatment with pravastatin
on cerebral vasospasm, autoregulation and delayed ischemic deficits
after aneurismal subarachnoid hemorrhage: A phase 2 randomized
placebo-controlled trial. Stroke. 36:1627–1632. 2005. View Article : Google Scholar
|
|
12
|
Lee YM, Chen WF, Chou DS, Jayakumar T, Hou
SY, Lee JJ, Hsiao G and Sheu JR: Cyclic nucleotides and
mitogen-activated protein kinase: Regulation of simvastatin in
platelet. J Biomed Sci. 17:452010. View Article : Google Scholar :
|
|
13
|
Luzak B, Boncler M, Rywaniak J, Wilk R,
Stanczyk L, Czyz M, Rysz J and Watala C: The effect of a platelet
cholesterol modulation on the acetylsalicylic acid-mediated blood
platelet inhibition in hypercholesterolemic patients. Eur J
Pharmacol. 658:91–97. 2011. View Article : Google Scholar
|
|
14
|
Chen JH, Yang LK, Chen L, Wang YH, Wu Y,
Jiang BJ, Zhu J and Li PP: Atorvastatin ameliorates early brain
injury after subarachnoid hemorrhage via inhibition of AQP4
expression in rabbits. Int J Mol Med. 37:1059–1066. 2016.
View Article : Google Scholar
|
|
15
|
Zhou C, Yamaguchi M, Kusaka G, Schonholz
C, Nanda A and Zhang JH: Caspase inhibitors prevent endothelial
apoptosis and cerebral vasospasm in dog model of experimental
subarachnoid hemorrhage. J Cerebral Blood Flow Metab. 24:419–431.
2004. View Article : Google Scholar
|
|
16
|
Hu N, Wu Y, Chen BZ, Han JF and Zhou MT:
Protective effect of stellate ganglion block on delayed cerebral
vasospasm in an experimental rat model of subarachnoid hemorrhage.
Brain Res. 1585:63–71. 2014. View Article : Google Scholar
|
|
17
|
Seo JH, Guo S, Lok J, Navaratna D, Whalen
MJ, Kim KW and Lo EH: Neurovascular matrix metalloproteinases and
the blood-brain barrier. Curr Pharm Des. 18:3645–3648. 2012.
View Article : Google Scholar :
|
|
18
|
Zhu MX, Lu C, Xia CM, Qiao ZW and Zhu DN:
Simvastatin pretreatment protects cerebrum from neuronal injury by
decreasing the expressions of phosphor-CaMK II and AQP4 in ischemic
stroke rats. J Mol Neurosci. 54:591–601. 2014. View Article : Google Scholar
|
|
19
|
Koyama Y, Maebara Y, Hayashi M, Nagae R,
Tokuyama S and Michinaga S: Endothelins reciprocally regulate
VEGF-A and angiopoietin-1 production in cultured rat astrocytes:
Implications on astrocytic proliferation. Glia. 60:1954–1963. 2012.
View Article : Google Scholar
|
|
20
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(-Delta Delta C(T)) method. Methods. 25:402–408. 2001.
View Article : Google Scholar
|
|
21
|
Rosenberg GA and Navratil M:
Metalloproteinase inhibition blocks edema in intracerebral
hemorrhage in the rat. Neurolgy. 48:921–926. 1997. View Article : Google Scholar
|
|
22
|
Chang CZ, Wu SC, Kwan AL and Lin CL:
Preconditioning with pitavastatin, an HMG-CoA reductase inhibitor,
attenuates C-Jun N-terminal kinase activation in experimental
subarachnoid hemorrhage-induced apoptosis. Acta Neurochir (Wien).
157:1031–1041. 2015. View Article : Google Scholar
|
|
23
|
Chou SH, Smith EE, Badjatia N, Nogueira
RG, Sims JR II, Ogilvy CS, Rordorf GA and Ayata C: A randomized,
double-blind, placebo-controlled pilot study of simvastatin in
aneurysmal subarachnoid hemorrhage. Stroke. 39:2891–2893. 2008.
View Article : Google Scholar
|
|
24
|
Wong GK, Chan DY, Siu DY, Zee BC, Poon WS,
Chan MT, Gin T and Leung M: HDS-SAH Investigators: High-dose
simvastatin for aneurysmal subarachnoid hemorrhage: Multicenter
randomized controlled double-blinded clinical trial. Stroke.
46:382–388. 2015. View Article : Google Scholar
|
|
25
|
Kirkpatrick PJ, Turner CL, Smith C,
Hutchinson PJ and Murray GD: STASH Collaborators: Simvastatin in
aneurysmal subarachnoid haemorrhage (STASH): A multicentre
randomised phase 3 trial. Lancet Neurol. 13:666–675. 2014.
View Article : Google Scholar
|
|
26
|
Chang CZ, Wu SC, Lin CL, Hwang SL, Howng
SL and Kwan AL: Atorvastatin preconditioning attenuates the
production of endothelin-1 and prevents experimental vasospasm in
rats. Acta Neurochir (Wien). 152:1399–1406. 2010. View Article : Google Scholar
|
|
27
|
Blann AD and Tabemer DA: A reliable marker
of endothelial cell dysfunction: Does it exist. Br J Haemataol.
90:224–228. 1995.
|
|
28
|
Chow M, Dumont AS and Kasselletal NF:
Endothelin receptor antagonists and cerebral vasospasm: An update.
Neurosurgery. 51:1333–1342. 2002. View Article : Google Scholar
|
|
29
|
Califano F, Giovanniello T, Pantone P,
Campana E, Parlapiano C, Alegiani F, Vincentelli GM and Turchetti
P: Clinical importance of thrombomodulin serum levels. Eur RevMed
Pharmacol Sci. 4:59–66. 2000.
|
|
30
|
Kästner S, Oertel MF, Scharbrodt W, Krause
M, Böker DK and Deinsberger W: Endothelin-1 in plasma, cisternal
CSF and microdialysate following aneurysmal SAH. Acta Neurochir
(Wien). 147:1271–1279. 2005. View Article : Google Scholar
|
|
31
|
Juvela S: Plasma endothelin concentrations
after aneurysmal subarachnoid hemorrhage. J Neurosurg. 92:390–400.
2000. View Article : Google Scholar
|
|
32
|
Tang QF, Lu SQ, Zhao YM and Qian JX: The
changes of von willebrand factor/a disintegrin-like and
metalloprotease with thrombospondin type I repeats-13 balance in
aneurysmal subarachnoid hemorrhage. Int J Clin Exp Med.
8:1342–1348. 2015.
|
|
33
|
Xu T, Zhang WG, Sun J, Zhang Y, Lu JF, Han
HB, Zhou CM and Yan JH: Protective effects of thrombomodulin on
microvascular permeability after subarachnoid hemorrhage in mouse
model. Neuroscience. 299:18–27. 2015. View Article : Google Scholar
|
|
34
|
Su EJ, Geyer M, Wahl M, Mann K, Ginsburg
D, Brohmann H, Petersen KU and Lawrence DA: The thrombomodulin
analog Solulin promotes reperfusion and reduces infarct volume in a
thrombotic stroke model. J Thromb Haemost. 9:1174–1182. 2011.
View Article : Google Scholar :
|
|
35
|
Cahill J, Calvert JW, Marcantonio S and
Zhang JH: p53 may play an orchestrating role in apoptotic cell
death after experimental subarachnoid hemorrhage. Neurosurgery.
60:531–545. 2007. View Article : Google Scholar
|
|
36
|
Alnemri ES, Livingston DJ, Nicholson DW,
Salvesen G, Thomberry NA, Wong WW and Yuan J: Human ICE/CED-3
protease nomenclature. Cell. 87:1711996. View Article : Google Scholar
|